Abstract
The scourge of antibiotic resistance threatens modern healthcare delivery. A contributing factor to this significant issue may be antibiotic dosing, whereby standard antibiotic regimens are unable to suppress the emergence of antibiotic resistance. This article aims to review the role of pharmacokinetic and pharmacodynamic (PK/PD) measures for optimising antibiotic therapy to minimise resistance emergence. It also seeks to describe the utility of combination antibiotic therapy for suppression of resistance and summarise the role of biomarkers in individualising antibiotic therapy. Scientific journals indexed in PubMed and Web of Science were searched to identify relevant articles and summarise existing evidence. Studies suggest that optimising antibiotic dosing to attain defined PK/PD ratios may limit the emergence of resistance. A maximum aminoglycoside concentration to minimum inhibitory concentration (MIC) ratio of > 20, a fluoroquinolone area under the concentration–time curve to MIC ratio of > 285 and a β-lactam trough concentration of > 6 × MIC are likely required for resistance suppression. In vitro studies demonstrate a clear advantage for some antibiotic combinations. However, clinical evidence is limited, suggesting that the use of combination regimens should be assessed on an individual patient basis. Biomarkers, such as procalcitonin, may help to individualise and reduce the duration of antibiotic treatment, which may minimise antibiotic resistance emergence during therapy. Future studies should translate laboratory-based studies into clinical trials and validate the appropriate clinical PK/PD predictors required for resistance suppression in vivo. Other adjunct strategies, such as biomarker-guided therapy or the use of antibiotic combinations require further investigation.
Similar content being viewed by others
Antibiotic doses for suppression of emergence of resistance are likely to exceed doses approved for treatment. |
Antibiotic combination therapy may be one method to minimise resistance emergence. |
The role of biomarkers to reduce resistance emergence is yet to be determined. |
1 Introduction
Antibiotic resistance is a significant global health issue, particularly considering the association of increased mortality and length of hospital admission for patients with multi-drug-resistant (MDR) bacterial infections [1, 2]. The global spread of bacterial resistance to last-line antibiotics such as carbapenems and colistin threatens the return of a pre-antibiotic era [3, 4]. This issue is likely to further escalate given the lack of novel antibacterial drug classes that have been developed in recent decades that can treat infections caused by MDR pathogens [5]. Given that the drug development process may take decades, optimising the use of currently available antibiotics should be considered an essential tool to minimise antibiotic resistance emergence.
Methods to maximise the utility of currently available antibiotics include the optimisation of the dose and duration of treatment, along with the use of combination therapies, which may limit resistance emergence and potentially treat MDR or extensively drug-resistant bacterial infections [6, 7]. Optimisation of antibiotic dosing can by guided by pharmacokinetic and pharmacodynamic (PK/PD) ratios that relate the antibiotic exposure to improved clinical outcomes. Dosing that aims to suppress resistance may also be potentially guided by PK/PD ratios. In vitro and pre-clinical in vivo studies have described PK/PD ratios required to prevent antibiotic resistance emergence. However, exposures required for suppression of emergence of resistance are generally higher than that needed for clinical cure, suggesting that current dosing practices are unlikely to ensure the prevention of antibiotic resistance emergence [8]. A further measure to prevent resistance emergence may include minimising the duration of therapy. As clinical signs and symptoms of infection may persist for some time after bacterial eradication has occurred, biomarkers may enable the distinction between those who remain ill due to persistent bacterial infection and those who remain symptomatic after bacterial eradication [9]. Thus, biomarkers may permit reduced antibiotic use and limit antibiotic selective pressure [10].
This article aims to describe the use of PK/PD measures for the optimisation of antibiotic therapy with the goal of minimising resistance emergence. It also aims to summarise existing evidence regarding the role of combination antibiotic therapy for suppression of resistance. The use of biomarkers to guide clinical decision making with respect to limiting the duration of antibiotic therapy and its role in minimising resistance emergence is also discussed.
2 Methods
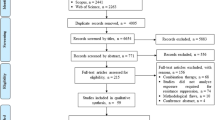
Published studies from 1946 until August 2017 were identified by searching the PubMed and Web of Science databases. Additional references were obtained by a bibliography and citation search of previously identified articles. Combinations of the following search terms were used: antibiotic, sepsis, septic shock, pharmacokinetic, pharmacodynamic, biomarker, resistant, bacteria and combination. Only studies written in English were reviewed. Any study describing antibiotic PK/PD ratios, the use of biomarkers to individualise therapy and antibiotic combination therapy, focussing on the emergence of resistance, were included.
3 Pharmacokinetic/Pharmacodynamic (PK/PD) Measures for Individualisation of Antibiotic Dosing
No objective and easily assessable clinical endpoint is available to guide antibiotic dose titration in a timely manner. The lack of an easily assessable and available clinical endpoint to ensure treatment adequacy and infection resolution (the ultimate goal of therapy) has led to the use of surrogate PK/PD ratios to guide both the design and the individualisation of antibiotic dosing. PK/PD ratios relate antibiotic exposure, usually relative to the minimum inhibitory concentration (MIC) of the pathogen with either bacterial killing or patient clinical outcomes [11]. Adjusting antibiotic dosing regimens to achieve these ratios can increase the likelihood that a patient will achieve desired outcomes [12].
The appropriate dosing adjustment strategy depends on the type of PK/PD ratio that best describes the clinical efficacy and bacterial kill characteristics of the antibiotic [13]. For concentration-dependent antibiotics, such as aminoglycosides, the preferred PK/PD ratio relates the free-drug maximum concentration (fCmax) to the MIC (fCmax/MIC) [14]. For time-dependent antibiotics such as β-lactam antibiotics, antibacterial effect is best described by the percentage of time the free drug concentration remains above the MIC throughout the dosing interval (fT>MIC) [15, 16]. On the other hand, the best PK/PD ratio for drugs with a more mixed concentration and time dependence, such as vancomycin, relate the area under the free-drug concentration–time curve, typically over a 24 h period, to the MIC (fAUC0–24/MIC) (Fig. 1 and Table 1) [8, 17]. These conventional PK/PD ratios have also been related to suppression of emergence of resistance (Fig. 1) although, as for clinical efficacy, the relationships are largely based on pre-clinical studies with a limited number of bacterial isolates. Prospective clinical trials are required to validate the PK/PD targets derived from in vitro studies.
Pharmacokinetic and pharmacodynamic parameters that define pharmacokinetic/pharmacodynamic ratios. AUC area under the concentration–time curve, C max maximum (peak) concentration, MIC minimum inhibitory concentration, T >MIC percentage of time the free drug concentration remains above the MIC throughout the dosing interval
In addition to the use of conventional PK/PD ratios that are based on the MIC of the pathogen, previous works have suggested that dosing aiming to suppress the emergence of resistance should preferentially be based on the mutant prevention concentration (MPC) [48, 49]. The MPC is derived from in vitro observation that the growth of resistant organisms can occur at a concentration above the MIC, but is inhibited at a threshold concentration defined as the MPC [34, 35]. Per the MPC definition, at least one mutation is needed for an isolate to grow in the presence of an antibiotic at a concentration above the MIC; however, two or more mutations conferring antibiotic resistance are required to grow at a concentration exceeding the MPC [34, 35]. Therefore, PK/PD ratios based on the MPC may be an appealing antibiotic dosing target as the probability of an organism attaining two or more mutations conferring antibiotic resistance is unlikely [34, 35]. Thus, when compared against increasing antibiotic concentrations, the emergence of resistance is typically described by an inverted ‘U’ shape (Fig. 2), where concentrations between the MIC and the MPC, known as the mutant selection window (MSW), promote the growth of a resistant bacterial subpopulation. This suggests the dosing regimen required for suppressing the emergence of antibiotic resistance is greater than that required for clinical cure. The MPC has been extensively described for fluoroquinolones [34,35,36, 49, 50] and to some extent for β-lactams [48, 51], aminoglycosides [52] and macrolides [53]. However, routine measurement of the MPC for use as a dosing target is not yet warranted as PK/PD ratios incorporating the MPC are uncommon and present a number of additional issues that require consideration. First, antibiotic exposure within the MSW is likely adequate for clinical cure in immunocompetent patients as the remaining bacterial burden is eradicated by the immune response [54, 55]. Second, the MPC reflects activity of the antibiotic against existing resistant subpopulations in vitro and not necessarily against acquired resistance mechanisms in vivo [56], although limited evidence suggests that the MPC may be independent of the resistance mechanism [57]. Third, the PK/PD ratios based on the MPC required to suppress resistance are not yet well described. Finally, the MPC requires additional culturing time of up to 72 h compared with up to 20 h for a standard MIC test [58] or between 5 and 19 h for Vitek2 MIC methods [59]. Nonetheless, the potential utility of the MPC as a guide for dose individualisation to minimise resistance deserves further investigation. One practical challenge is the relatively high MPC values that may be encountered for some antibiotics with narrow therapeutic windows, such as the aminoglycosides [52] and vancomycin [60]. Given that the MPC is not routinely used clinically, PK/PD ratios based on the MPC are difficult to derive from clinical studies. In this regard, translational in vitro studies, such as the dynamic hollow fiber infection model (HFIM), which enables the simulation of a human pharmacokinetic (PK) profile, thus potentially allowing extrapolation into clinical use, provides a useful guide for dosing that ensures suppression of resistance emergence [61, 62].
The effect of exposure to increasing antibiotic concentrations on the burden of resistant and susceptible bacterial populations. The susceptible (grey) bacterial burden is rapidly reduced against an antibiotic concentration equivalent to the minimum inhibitory concentration, which has little impact on the resistant (black) bacterial subpopulation. The resistant bacterial subpopulation killing curve is represented by the ‘inverted U-shape’, where the resistant population is eventually killed at the antibiotic mutant prevention concentration. CFU colony-forming units, MIC minimum inhibitory concentration, MPC mutant prevention concentration, MSW mutation selection window
4 What Information is Needed to Individualise Therapy?
4.1 Bacterial Minimum Inhibitory Concentration
PK/PD ratios that guide dose individualisation are currently based on the bacteria MIC. Microbiology laboratories routinely report whether bacteria are susceptible or resistant if the bacteria MIC is below or above the clinical breakpoint cut-off, respectively, but not necessarily the specific pathogen MIC, which may involve a separate assay than that used to determine susceptibility [63]. It has been well established that a ‘susceptible’ pathogen does not equate to the adequacy of antibiotic exposure, particularly for isolates with MICs near the clinical breakpoint (Table 1). This is exemplified by the decrease in estimated probability of attaining a target Cmax/MIC of ≥ 10 for amikacin by nearly 60% when the pathogen MIC increases from 4 to 8 mg/l, the European Committee on Antimicrobial Susceptibility Testing (EUCAST) susceptibility breakpoint for amikacin, even when administered at a dose of 30 mg/kg in patients with ventilator-associated pneumonia (VAP) [64]. Similar trends of reduced probability of target attainment within the susceptibility range have been described for meropenem [65], ciprofloxacin [66] and piperacillin–tazobactam [67].
The reduced probability of target attainment when using conventional doses against susceptible isolates with increased MICs for current clinical PK/PD indices suggests that doses need to be adjusted based on the measured MIC to achieve optimal PK/PD ratios. However, the utility of the MIC is questionable. The MIC is determined in optimal bacterial growth conditions in the presence of static serial twofold increasing antibiotic concentrations, which do not represent the in vivo environment in a patient receiving antibiotics therapeutically [68]. Moreover, the MIC is the observed minimum antibiotic concentration to inhibit bacterial growth. Given that a bacterial suspension is visibly turbid at an inoculum of ~ 1 × 107 colony-forming units (CFU)/ml, the MIC may also be interpreted as the concentration of antibiotic that inhibits growth below this bacterial burden [68]. The implication is that the MIC of a bacterial inoculum likely reflects the predominant bacterial population and does not consider a potentially ‘resistant’ or ‘less-susceptible’ bacterial subpopulation. Therefore, targets based on the MIC for suppression of resistance emergence, although commonly expressed as such, are of uncertain value in determining the actual antibiotic exposure required to suppress resistance emergence as the MIC does not reflect the antibiotic exposure to prevent growth of the ‘resistant’ bacterial subpopulation in a defined inoculum. Pursuant to this concept is the use of a high starting bacterial inoculum (~ 1 × 108 CFU/ml) in many studies that investigate bacterial resistance emergence, which exceeds that required for MIC testing (~ 1 × 105.5 CFU/ml) [58]. It would be expected that as the total bacterial population increases, so too does the probability of a ‘resistant’ bacterial subpopulation as can be demonstrated by the growth of bacteria in the presence of an antibiotic, typically at concentrations equivalent to a few multiples of the MIC, known as the mutation frequency [69,70,71]. For example, if we consider a reported fluoroquinolone mutation frequency of ~ 1 × 10−8 for Gram-negative pathogens, this would mean that a resistant subpopulation would be unlikely for a standard MIC test but may result in the emergence of resistance for some patients with high inoculum infections such as VAP [72,73,74,75,76].
To make use of the MIC that describes the antibiotic–pathogen PD, a clinician must also understand how to adjust the antibiotic dosing regimen to optimise PK/PD ratios to ensure optimal clinical efficacy.
4.2 Therapeutic Drug Monitoring and pharmacokinetic Models
Knowledge of the drug PK profile within the patient at the bedside is necessary to enable precise dose individualisation, guided by PK/PD ratios. The PK information in a patient is obtained from antibiotic concentration measurement with the use of therapeutic drug monitoring (TDM) [77]. Critically ill patients in the intensive care unit (ICU) have well documented altered PK related to enhanced or impaired elimination, or increased volume of distribution due to increased vascular permeability because of sepsis [14, 78, 79]. These result in PK fluctuations that may necessitate TDM-guided dose adjustment to maximise the likelihood of achieving therapeutic concentrations. For example, in one study, 74.2% of patients receiving β-lactam antibiotic therapy required a dose increase to meet a minimum plasma concentration (Cmin)/MIC ratio > 4 [80]. Similarly, amikacin dose adjustment was required in 83% of patients with sepsis, with approximately equivalent rates of dose increases and decreases [81]. The use of TDM to guide therapy has also been described for other antibiotics, including the glycopeptides [82], fluoroquinolones [12], linezolid [83] and daptomycin [84].
TDM with dose adjustment to meet key PK/PD targets has been shown to reduce mortality in patients with nosocomial pneumonia receiving aminoglycosides, β-lactam antibiotics and/or fluoroquinolones [12]. Dose adjustment with PK/PD target attainment of the prescribed antibiotics within 3 days of treatment initiation resulted in a lower mortality rate of 10.2% for the TDM cohort compared with 23.6% for the control cohort, highlighting the importance of dosing adjustment to attain PK/PD measures [12]. Moreover, patients with severe sepsis or septic shock achieving a target amikacin Cmax of between 60 and 80 mg/l (corresponding to a Cmax/MIC ratio of ~ 8) had reduced mortality compared with those who did not; which has also been shown in the treatment of nosocomial pneumonia [19, 85]. However, when interpreting the MIC result, the clinician should consider the impact of potential MIC assay error, which may be within one dilution of the determined value and thus affect the target drug exposure [68]. The lack of prospective randomised controlled trials supporting PK/PD targeted therapy, timely availability of MIC data, and limited TDM resources for many antibiotics have prevented widespread adoption of PK/PD-guided therapy [86].
A plethora of software packages have been developed to perform Bayesian dose adaptation at the bedside, whereby a single well-timed TDM concentration can be incorporated into a population PK model together with patient-specific clinical covariates to provide a recommended dose that may meet key PK/PD ratios. Several packages have been reviewed [13]. When clearly defined PK/PD ratios associated with resistance suppression are available, dosing software may be adjusted accordingly to predict patient-specific dosing regimens that minimise emergence of resistance.
5 PK/PD Measures to Minimise Resistance Emergence and Importance of Antibiotic PK at the Site of Infection
5.1 Aminoglycosides
PK/PD ratios of aminoglycosides required for suppression of resistance emergence have not been well established. When conventional PK/PD targets are used to guide aminoglycoside dosing, resistance emergence may occur within 12 h of the first dose [87]. Thus, it is generally expected that higher PK/PD ratios than required for clinical effect may be required to suppress resistance. This was demonstrated by Tam et al. [20], who showed, using one-compartment dynamic in vitro studies whereby bacteria were exposed to a humanised drug concentration–time profile, that a twice daily dosing regimen of gentamicin with both doses targeting a Cmax/MIC > 30 against Pseudomonas aeruginosa resulted in sustained resistance suppression. In contrast, single daily doses targeting a Cmax/MIC > 36 did not reduce resistance emergence. This discrepancy is likely a function of the increased AUC/MIC ratio in the twice daily dosing regimens, which is not surprising given both the AUC/MIC [88] and the Cmax/MIC [18] ratio have been correlated with clinical efficacy (Table 1). Therefore, it is important for treatment efficacy and minimisation of toxicity that the shape of the AUC reflects the contribution of the concentration-dependent bacterial killing property of aminoglycosides [88]. However, a once daily dose of amikacin with a Cmax/MIC > 20 against Acinetobacter baumannii suppressed the emergence of resistance [20]. This inter-isolate and inter-species differences in the required aminoglycoside target concentration for suppressing resistance emergence likely relates to non-specific outer membrane changes given that amikacin resistance against A. baumannii was stable with serial passaging; however, P. aeruginosa gentamicin resistance was transient [20]. Therefore, the dose required to suppress resistance emergence likely varies with specific drug within an antibiotic class and with the bacterial species or specific isolate. In any case, these results highlight that dosing targets at least twice that required for clinical efficacy may be necessary to ensure an exposure that minimises resistance; however, the risk of significant nephrotoxicity with such regimens likely precludes the implementation into routine practice until the risk–benefit ratio of such dosing regimens have been established [89]. Layeux et al. [90] demonstrated that one potential approach could be the use of high-dose aminoglycoside therapy in combination with dialysis to enable attainment of high Cmax and AUC values but to minimise drug accumulation and toxicity through increased extracorporeal clearance.
The ability to meet target PK/PD ratios depends on the patient’s site of infection and mode of drug administration. Serum concentrations achieved with intravenous high-dose regimens of gentamicin and tobramycin (7 mg/kg), and amikacin (30 mg/kg) are unlikely to meet the proposed PK/PD ratios for resistance suppression [91, 92]. Even current clinical PK/PD indices for efficacy, which are at least half that required for resistance suppression (Table 1), may not be met in up to 41% of patients [91, 92].
For respiratory infections, nebulised aminoglycoside administration can attain concentrations in the epithelial lining fluid, the proposed site of bacterial deposition in pneumonia, up to 46-fold that of intravenous therapy [93]. This may be one method to minimise resistance emergence while improving treatment outcomes as has been shown in a recent meta-analysis [94]. Aminoglycosides are also commonly used in the management of complicated urinary tract infections (UTIs). Gentamicin achieves peak urinary concentrations approximately 26-fold that in serum [95], which may achieve proposed PK/PD targets for resistance suppression; however, the impact of this on bacterial eradication and resistance emergence has yet to be determined experimentally. Taken together, these data suggest that the AUC/MIC and the Cmax/MIC ratio are likely key PK/PD ratios to consider for resistance suppression, which may be attainable in the urine with modest aminoglycoside doses or through nebulisation for the treatment of respiratory infections.
5.2 Fosfomycin
Fosfomycin has been extensively used as an oral antibiotic for treating UTIs in Europe and is now also being increasingly used intravenously in the management of invasive infections caused by MDR bacteria [96]. Little is known regarding the optimal dosing strategy for clinical cure or resistance suppression; however, murine thigh infection models suggest an AUC/MIC ratio of > 8.5 h−1 is the minimum exposure required for bacteriostatic activity and mice survival, but this varies between species and bacterial isolate [46]. The AUC/MIC ratio has been linked with the suppression of emergence of resistance. In a dynamic in vitro HFIM simulating an intravenous fosfomycin total daily dose of 24 g, either as a single dose or administered in divided doses against an Escherichia coli isolate with a fosfomycin MIC of 1 mg/l suppressed resistance emergence (AUC0–24/MIC of 3136 h−1) [47]. It has also been postulated that the time above the MIC of any resistant subpopulation(s) is important for fosfomycin efficacy and reduction in resistance emergence [97]. When the fosfomycin concentration is above the MIC of the resistant subpopulation for 33% of the dosing interval, the bacterial concentration is reduced by 2-logs; however, the time above the MIC of the resistant subpopulation was not able to be quantified.
Fosfomycin is concentrated in the urine with AUC0–∞ of 31,995 mg/l.h following a single oral dose of 3 g, which is likely to exceed the AUC/MIC ratio potentially required for resistance suppression for isolates with an MIC of less than 8 mg/l [98]. Similar findings in a novel in vitro dynamic simulation of bladder fosfomycin concentrations following oral dosing show that a single oral dose of fosfomycin 3 g against E. coli and Enterobacter cloacae isolates with an MIC ≤ 4 mg/l is likely sufficient to suppress resistance emergence [99]. However, resistance emergence occurred with all Klebsiella pneumoniae isolates tested (MIC range 2–8 mg/l) [99].
High urinary tract concentrations, for some isolates, may partly explain the lack of resistance emergence when used for UTIs [100]. These exposures are unlikely to be attained in plasma or interstitial fluid with approved/safe high-dose oral or intravenous therapy, which may partly explain the rates of resistance emergence during the treatment of systemic infections with monotherapy, which may occur in up to 20% of patients with infections other than a UTI [100,101,102]. Nebulised fosfomycin for the treatment of pneumonia may be one alternate administration potentially resulting in the required concentrations to minimise resistance emergence [103].
5.3 β-Lactam Antibiotics
β-Lactam antibiotics demonstrate time-dependent bactericidal activity, and the plasma (% fT>MIC) correlates well with clinical outcomes and bactericidal activity [17]. The traditional fT>MIC values recommended for optimal effect are 40, 50 and 60–70% for carbapenems, penicillins and cephalosporins, respectively [17, 23]. However, these proposed ratios are likely insufficient for optimal patient outcomes, and higher PK/PD targets of as much as 100% fT>2–5×MIC have been proposed to be required for maximising clinical efficacy [79, 104,105,106,107]. Evidence for resistance suppression in clinical trials is scarce. A study in patients with VAP could not identify a statistically significant PK/PD index for carbapenems, based on either the MIC (fT>MIC) or the MPC (fT>MPC) [108]. However, resistance emergence was greatest (26%) in patients with an fT>MIC of < 40% [108].
In vitro dynamic infection models and in vivo animal model studies have described PK/PD ratios that may suppress resistance emergence. Meropenem Cmin/MIC ratios of > 6.2 have been shown in vitro with the dynamic in vitro HFIM as suppressing resistance emergence against P. aeruginosa [28]. Interestingly, this ratio was reduced to < 1.7 when meropenem was used in combination with tobramycin [28]. With the dynamic in vitro HFIM, Cmin/MIC ratios of > 3.8 have also been proposed for cefepime and ceftazidime against P. aeruginosa and K. pneumoniae isolates [27]. Moreover, should the concentration of meropenem remain within the MSW for > 80% of the dosing interval, resistance appears to be amplified, which is consistent with the MSW hypothesis [29]. Indeed, attainment of the accepted fT>MIC of 40% for meropenem, the traditional PK/PD ratio recommended for optimal clinical outcomes, was associated with P. aeruginosa resistance amplification in a murine pneumonia model, despite providing a 100% mice survival rate compared with 0% for untreated controls [109]. Similar results have been described by Zinner et al. [110] using the dynamic in vitro HFIM with doripenem against P. aeruginosa.
Results appear to be similar for the penicillins against Gram-negative bacterial pathogens. Felton et al. [25] described that a piperacillin–tazobactam Cmin/MIC ratio of 4.6 would be required for resistance suppression with intermittent bolus dosing against a relatively low bacterial inoculum (4 × 105 CFU/ml) in the dynamic in vitro HFIM. Interestingly, the target Cmin/MIC ratio is increased with continuous infusion regimens, with a ratio of 10.4 required for resistance suppression [25]. However, with intermittent regimens achieving Cmin/MIC ratios of 4.6, the plasma concentration to MIC ratio is likely to be greater than 10.4 for a substantial proportion of the dosing interval. Thus, prolonged exposure to concentrations higher than the Cmin of intermittent dosing may be required for resistance suppression. Practically, compared with continuous infusions, higher doses are required with intermittent regimens to achieve the respective ratios. Furthermore, in the same dynamic in vitro HFIM study, simulated high-dose piperacillin regimens of up to 17 g thrice daily administered as a bolus or extended infusion did not result in significant bacterial killing and was unable to suppress the emergence of resistance against a large P. aeruginosa bacterial density (~ 8 × 108 CFU/ml) [25]. Therefore, combination antibiotic therapy may be necessary to treat and suppress the emergence of resistance against infections with a high bacterial burden, such as VAP [72,73,74,75,76]; however, this requires further investigation.
For the newly available β-lactam antibiotic and β-lactamase inhibitor combinations, including ceftolozane–tazobactam and ceftazidime–avibactam, the PK/PD indices for resistance suppression are not yet well described. In the dynamic in vitro HFIM, simulated doses of ceftolozane–tazobactam 2–1 g administered every 8 h (achieving 100% fT>MIC) did not result in growth of resistant P. aeruginosa, but doses between 125–62.5 mg (achieving 12.5% fT>MIC) and 1–0.5 g (achieving 100% fT>MIC) were associated with resistance amplification [111]. This discrepancy is likely due to the different ceftolozane AUC between the 2–1 g (AUC0–24 1032.6 mg/l.h) and 1–0.5 g (AUC0–24 456.2 mg/l.h), which would likely result in an elevated Cmin/MIC ratio that has been associated with suppression of emergence of resistance [27, 111]. In a similar study using E. coli, a lower dose threshold of 750–375 mg administered every 8 h (100% fT>MIC) resulted in resistance suppression [112]. The difference between these studies is the lower MIC of E. coli (0.25 mg/l) against ceftolozane–tazobactam compared with P. aeruginosa (4 mg/l). The exposures required of the β-lactamase inhibitor in combination products is currently unknown, but the minimum concentration required for enzyme inhibition is likely important, as shown by the inhibition of AmpC that mediated cefepime resistance emergence in an HFIM study [87]. This concept is further supported by the suppression of bacterial regrowth when exposed to avibactam concentrations > 0.28 mg/l when combined with ceftazidime [113, 114]. Currently used ceftazidime–avibactam doses of up to 2–0.5 g administered intravenously thrice daily in a cohort of 37 patients with carbapenem-resistant Enterobacteriaceae infections have been associated with microbiological failures in up to 27% of patients, with 30% of these failures likely related to the emergence of ceftazidime–avibactam-resistant isolates [115]. Given that treatment was more likely to fail in patients with renal replacement therapy and lung infections, dosing consideration for target site antibiotic penetration [116] and extracorporeal elimination [117] are likely key factors influencing treatment outcomes [115]. This would suggest that dose optimisation must be considered to prevent resistance emergence to newly developed antibiotics.
PK/PD ratios for β-lactams against Gram-positive organisms are lacking, but a fT>MIC of 100% may be sufficient against susceptible Streptococcus pneumoniae [26, 118].
Given the lack of data describing significant toxicity with supratherapeutic concentrations of penicillins [119, 120] and potential impact on clinical outcomes, we would advocate the use of an initial loading dose followed by continuous infusions of high-dose β-lactam antibiotics for the treatment of patients with sepsis or septic shock requiring ICU admission [16]. However, up to 45% of patients may not achieve a serum fT>MIC of 100% when conventional total daily doses (e.g. piperacillin–tazobactam 16-2 g) are administered as a continuous infusion, potentially due to augmented renal clearance [121,122,123]. The site of infection exposure could be even lower. Currently licensed daily doses of β-lactam antibiotics (piperacillin–tazobactam 16-2 g, ceftazidime 8 g, meropenem 6 g) administered via prolonged or continuous infusions for the treatment of respiratory infections may be insufficient in up to 40% of patients to achieve a fT>MIC of 100% at the site of infection, in part due to highly variable lung tissue penetration (mean/median exposure 20–40% of serum concentrations) [65, 116, 124, 125]. Cefepime achieves approximately equivalent concentrations in serum and the lungs when administered as a continuous infusion, and may be one agent where resistance suppression indices may be met in the lung using continuous infusions of 8 g per day [126]. However, given the wide inter-individual heterogeneity in β-lactam antibiotic pharmacokinetics, TDM may enable individual dose optimisation to facilitate dosing that minimises resistance emergence [122].
5.4 Colistin
Given the use of colistin, administered as the prodrug colistin methanesulfonate (CMS), as a treatment for MDR Gram-negative bacterial infections, the risk of resistance emergence to this agent is likely very high [39]. Plasma concentrations of colistin achieved by commonly used doses may be far below those required for resistance suppression. For instance, data from a murine thigh and lung infection model suggest that A. baumannii resistance to colistin may occur at steady-state concentrations of > 10 mg/l, greatly exceeding the steady-state Cmax of 2–3 mg/l attainable in critically ill patients by administering 3 million international units (MIU) of CMS thrice daily [45, 127, 128]. However, against P. aeruginosa, smaller doses of colistin (~ 3 MIU, resulting in a Cmax of 3 mg/l) given thrice daily may be adequate to limit the emergence of high-level colistin resistance [128, 129]. Taken together, these data suggest that conventional colistin dosing regimens for clinical efficacy are insufficient to prevent resistance emergence.
Given the pathogen-specific variations in dosing requirements, it may be prudent to consider the highest possible dose that can be safely administered, although what this dose is in different patients is unclear. In a study of 28 critically ill patients, initial loading doses of 9 MIU of CMS followed by twice daily doses of 4.5 MIU did not result in resistance emergence of the initial pathogen, potentially suggesting that the immune response is central to minimisation of resistance emergence [54, 127, 130]. Another approach to achieve high target site exposures for respiratory infections is nebulised dose administration. In one study, nebulised CMS administered at a dose of 1 MIU thrice daily resulted in a median epithelial lining fluid concentration of 6.7 mg/l (interquartile range 4.8–10.1 mg/l) 1 h post-dose, with the respective plasma concentration being fivefold lower [131]. Thus, doses higher than 1 MIU should be administered to achieve adequate concentrations in the lung, whilst limiting systemic exposure. In addition, given the apparent lack of colistin penetration into lung tissue following intravenous CMS administration, concomitant nebulised dosing appears reasonable [132]. The poor lung penetration following intravenous CMS administration would also suggest that intravenous dose optimisation for suppression of resistance against pathogens causing pneumonia is likely to be challenging. At exposures achieved by an intravenous dose, a synergistic combination with other antibiotics may be necessary to suppress emergence of resistance [133]. Alternatively, use of other polymyxins with more predictable pharmacokinetics, like polymyxin B, may prove to be more valuable agents for the treatment of MDR infections. Evidence for this is suggested by a one-compartment dynamic in vitro study that simulated the gradual rise of active colistin concentrations following administration of a loading dose of CMS 12 MIU and 4.5 MIU twice daily thereafter [134]. This was compared with polymyxin B administered as a loading dose of 2 and 1.25 mg/kg daily thereafter against A. baumannii [134]. Colistin, administered as CMS, did not result in appreciable bacterial killing, compared with a 6-log reduction in bacteria following polymyxin B administration; however, this was not sustained, with bacterial regrowth exceeding the baseline within 12 h [134]. No dose of CMS or polymyxin B suppressed resistance emergence [134]. Further increasing the polymyxin B dose has been investigated as one strategy to prevent resistance emergence. In a separate HFIM study, a simulated polymyxin B loading dose of 3.33 mg/kg followed by 1.43 mg/kg twice daily thereafter increased the proportion of the bacterial population able to grow in the presence of 10 mg/l of polymyxin B compared with a loading dose of 2.22 and 1.43 mg/kg thereafter [135]. Indeed, the proportion of the resistant bacterial population was further increased when loading doses of up to 18.3 mg/kg without further maintenance doses were employed [135]. Taken together, these data suggest that polymyxin B should be used in combination with another active antibiotic to minimise resistance emergence.
5.5 Daptomycin
Daptomycin has a spectrum of activity that includes methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant Enterococci (VRE) [136].
In one study, the total AUC/MIC ratio of 200 (fAUC/MIC ~ 20 h−1) [123], achievable with licensed doses of 6 mg/kg/day, was predicted to suppress S. aureus daptomycin resistance emergence in a dynamic one-compartment in vitro infection model [137, 138]. However, another in vitro study of S. aureus endocarditis vegetations showed threefold increases in daptomycin MICs after use of 6 mg/kg/day, which may be related to reduced daptomycin penetration into the vegetation [139]. Similarly, doses of 6 mg/kg/day have resulted in resistance emergence in a clinical case report [140], potentially due to enhanced daptomycin clearance, which can be seen in critically ill patients [141]. At a simulated dose of 10 mg/kg/day, no decrease in susceptibility to daptomycin was observed in vitro for the S. aureus isolates that showed a threefold reduction in susceptibility at a dose of 6 mg/kg/day [139].
5.6 Fluoroquinolones
One-compartment dynamic in vitro studies simulating humanised PK profiles indicate a ciprofloxacin AUC0–24/MIC ratio of > 285 h−1 or a Cmax/MIC ratio of > 24 may be required to suppress P. aeruginosa resistance [32]. Exposures required for suppression of emergence of resistance are approximately twofold greater than that generally required for clinical cure (AUC0–24 of ≥ 125 mg/l.h) in critically ill patients with predominantly respiratory tract infections or Gram-negative bacterial infections [30, 31]. The importance of a Cmax/MIC ratio for fluoroquinolone efficacy has also been shown in a murine neutropenic model where a Cmax/MIC ratio of > 20 correlated with mice survival, potentially by reducing the probability of resistance emergence [142]. However, the AUC/MIC ratio has also been shown to be an important PK/PD ratio for suppression of emergence of resistance. Tam et al. [143], used the dynamic in vitro HFIM and showed that a garenoxacin AUC0–24/MIC ratio of 201 h−1 suppressed P. aeruginosa resistance emergence. This target may be reduced for K. pneumoniae where an AUC0–24/MIC of 67 h−1 inhibited resistance emergence, which was also identified in a separate HFIM study [34]. Furthermore, the percentage of the dosing interval spent within the MSW may also be an important PK/PD ratio for emergence of fluoroquinolone resistance. A fluoroquinolone fTMSW of < 20% is associated with suppression of emergence of resistance [35]. Using this PD target, clinically used intravenous doses of ciprofloxacin 400 mg every 12 h that achieve the clinical target PK/PD exposure for a pathogen with an MIC of 0.125 mg/l is unlikely to prevent suppression of emergence of resistance for isolates with an MIC of ≥ 0.125 mg/l [66, 144, 145]. Increasing the intravenous ciprofloxacin dose from 400 mg twice daily to 400 mg thrice daily in critically ill patients may be sufficient to suppress the emergence of resistance for isolates with an MIC of < 0.25 mg/l [146]. At least one small clinical trial [146] has shown this dosing regimen to be effective and well tolerated.
Other fluoroquinolones with increased Gram-positive antibacterial activity are available, such as levofloxacin and moxifloxacin. It has been shown in dynamic in vitro infection models that fluoroquinolone AUC/MIC ratios between 143 and 431 h−1 may suppress MRSA resistance emergence [34, 35]. Simulated clinically used moxifloxacin regimens of 400 mg once daily were sufficient to attain these target PK/PD ratios [35]. In contrast, dose increases of 90, 120 and 540% above currently used clinical doses of 400, 500 and 400 mg twice daily would be required to suppress S. aureus resistance emergence for gatifloxacin, levofloxacin and ciprofloxacin, respectively [35]. Lower AUC/MIC ratios of 100 h−1 have been shown to minimise resistance emergence of S. pneumoniae exposed to moxifloxacin [147]. Importantly, this may be sufficient to minimise the emergence of S. pneumoniae resistance in patients without severe sepsis or septic shock, who may require moxifloxacin 400 mg twice daily, depending on the MIC of the pathogen [148, 149].
An important factor regarding fluoroquinolone use is collateral resistance [150]. Commensal organisms, such as faecal E. coli and pharyngeal streptococcal species, may become resistant to fluoroquinolones following systemic therapy in up to 33% of patients, possibly related to potential horizontal gene transfer that may propagate the spread of resistance [151,152,153]. Moreover, the use of fluoroquinolones increases not only the risk of subsequent fluoroquinolone resistance but also resistance to third-generation cephalosporins, such as ceftriaxone, because of the emergence of extended-spectrum β–lactamase (ESBL)-producing organisms; thus, the judicial use of fluoroquinolones is warranted. Given that further dose increases are unlikely to suppress the emergence of bacterial resistance in the large bacterial inoculum of the faecal flora [152], the fluoroquinolone dose should be targeted to suppress the emergence of antibiotic resistance in the infecting pathogen. Furthermore, consideration should be given to the potential risks of high-dose therapy (e.g. intravenous ciprofloxacin > 400 mg every 8 h), which may include cardiac dysrhythmias and confusion [14].
5.7 Glycopeptides
Vancomycin and teicoplanin are the glycopeptides currently commonly used for MRSA infections. Firsov et al. [38] identified that a vancomycin AUC/MIC > 200 h−1 was sufficient to suppress resistance emergence against MRSA and methicillin-susceptible S. aureus (MSSA) in the dynamic one-compartment in vitro infection model, an exposure equivalent to intravenous vancomycin 1 g administered twice daily. These results are consistent with those of Nicasio et al. [154], whereby similar doses against an MRSA isolate resulted in resistance suppression in a dynamic HFIM. These results would suggest that current dosing regimens targeting an AUC/MIC > 400 h−1, which is associated with improved clinical outcomes, is sufficient for suppression of resistance emergence [37]. However, contrasting with these results, Lenhard et al. [39] showed that an AUC/MIC of 1800 h−1 (equivalent to 4 g administered twice daily) was required to suppress vancomycin resistance against two MRSA isolates. The initial inoculum differed between the studies conducted by Lenhard et al. [39] (~ 1 × 1010 CFU/ml) and Nicasio et al. [154] (~ 1 × 106 CFU/ml), suggesting that the exposure required to suppress resistance emergence depends not only on the specific isolate but also on the bacterial inoculum [155].
Charles et al. [156] described clinical data supporting these in vitro findings; they associated initial trough vancomycin concentrations of < 10 mg/l and high bacterial load infections (infective endocarditis, undrained collections or infected prosthetic material) with emergence of heterogenous vancomycin-intermediate S. aureus (hVISA) emergence in MRSA bacteraemia. This is supported by the lack of vancomycin resistance in a patient receiving long-term suppressive vancomycin therapy when trough concentrations were maintained at > 10 mg/l [157].
Taken together, these data suggest high-dose vancomycin therapy is required to mitigate resistance emergence. A loading dose of 30 mg/kg results in higher trough concentrations than standard doses of 15 mg/kg in the first dosing interval, as shown by Rosini et al. [158], where 34% of patients compared with 3%, respectively, achieved a trough concentration ≥ 15 mg/l. Following a loading dose, a continuous infusion with a steady-state target concentration of 20 mg/l may be sufficient for resistance suppression [159], depending on the pathogen MIC, without an increased risk of nephrotoxicity [160]. Another method to limit glycopeptide resistance emergence may be to reduce the infective inoculum with synergistic combinations. Combinations of vancomycin and cefazolin [161] or piperacillin–tazobactam [162] or nafcillin [163] have shown rapid reductions and a trend towards shorter clearance times of MRSA and MSSA with high initial inoculums of ~ 1 × 108 CFU/ml. The effectiveness of vancomycin and β-lactam combination therapy on clinical outcomes and resistance emergence have yet to be determined in clinical trials [164].
5.8 Linezolid
Little evidence exists regarding PK/PD ratios required for the suppression of resistance emergence. Tsuji et al. [43], in a dynamic HFIM, showed that simulated exposures of 600 mg twice daily dosing (AUC0–24 of 124 mg/l.h; AUC/MIC of 112 h−1) suppressed resistance emergence against clinical MRSA isolates, which approximates the AUC/MIC ratio of > 80–120 h−1 associated with improved microbiological eradication [40]. In a separate one-compartment in vitro model, lower linezolid doses of 120 mg twice daily, 120 mg as a continuous infusion over 24 h and 30 mg as a continuous infusion over 24 h were tested against MRSA, hVISA, VISA and VRE isolates [165]. Linezolid resistance emergence, as determined by an increase in MIC, was observed only for the 120 mg continuous infusion regimen, whereby the linezolid concentration approximated the baseline MIC of 2 mg/l for all isolates [165]. This suggests that doses achieving a steady-state linezolid concentration approximately equivalent to the pathogen MIC may promote resistance emergence. In a dynamic one compartment in vitro study investigating vancomycin-resistant Enterococcus faecalis, Tsuji et al. [42] showed a variable trend in the linezolid exposure required for resistance suppression. Exposures at an AUC/MIC ratio of > 31 h−1 prevented resistance emergence in all isolates without baseline resistance alleles; however, resistance emergence could not be prevented at any exposure (up to an AUC/MIC of 495 h−1) in a previously susceptible isolate with baseline resistance alleles [42]. Taken together, these data suggest that low linezolid exposures in isolates without baseline resistance mechanisms may result in resistance emergence.
Clinical data regarding linezolid resistance emergence are limited to case reports. In 2010, a linezolid-resistant S. aureus outbreak was identified in 12 patients in an ICU in Spain, 11 of whom had previously received linezolid [166]. Similarly, two children receiving suppressive low-dose linezolid therapy were also colonised with linezolid-resistant S. aureus [167]. These, in part, may be related to variable linezolid exposures. In critically ill patients receiving linezolid 600 mg twice daily as a 15 to 60 min infusion, only 30% of patients achieved an AUC within the therapeutic range (AUC0–24 200–400 mg/l.h) for a presumed pathogen MIC of 2 mg/l at any point during the study, and only 17% of patients met this target over the 4-day PK study [168]. Of concern is the potential for adverse events, such as haematological toxicity, with a linezolid Cmin > 10 mg/l [169]. Given the variability in linezolid exposures following a standard dosing regimen of 600 mg twice daily and the potential for both poor treatment efficacy and toxicity, TDM has been proposed as one method to improve linezolid dosing practices [170].
6 Impact of the Antimicrobial Regimen and Development of Antimicrobial Resistance
6.1 Combination Therapy
The role of combination therapy has been disputed. Several aspects of patient management intuitively support the use of combination therapy, including extending the spectrum of activity and synergism and minimising resistance emergence. These concepts may not be mutually exclusive. Mathematical models describe the amplification of resistance when a baseline resistant subpopulation is present, which may be present in a seemingly susceptible isolate based on the MIC [50, 171]. Thus, combination therapy may extend the spectrum of activity to the bacterial subpopulation, which may have resistance to one of the antibiotics in the combination regimen [172, 173]. Furthermore, the probability of an organism acquiring a mutation conferring resistance to both antibiotics is significantly less than with monotherapy [74, 174, 175], although developing resistance to two antibiotics would be highly problematic for drug choices. Other potentially beneficial mechanisms relate to the specific antibiotic combination used.
β-Lactams and aminoglycosides often have high rates of synergistic activity against Gram-negative and Gram-positive bacterial pathogens [172, 173, 176]. However, synergistic activity has not been correlated with the suppression of emergence of β-lactam antibiotic resistance against P. aeruginosa in vivo [177]. These results are consistent with a meta-analysis that did not identify a reduced risk of resistance emergence with β-lactam and aminoglycoside combination therapy [178]. In vitro evidence contrasts with clinical trials, whereby low doses of tobramycin and cefepime (3 mg/kg and 563 mg given every 8 h, respectively) suppressed resistance emergence of P. aeruginosa in a dynamic HFIM [87]. This discrepancy between clinical studies and in vitro methods may be related to the different dosing regimens used between the meta-analysis, which primarily included studies using multiple daily dosing regimens that may not meet key PK/PD ratios, and the once daily dosing regimens used by in vitro studies. Furthermore, the importance of combination therapy, as demonstrated in vitro studies, may not extend to clinical practice because of the immune system response, the ideal growth conditions provided in vitro that may enhance bacterial growth and the limited bacterial isolates studied in vitro [26]. Further work is needed to characterise the importance of β-lactam antibiotic and aminoglycoside combination therapy to minimise the emergence of resistance [179, 180].
Despite potential β-lactam antibiotic and fluoroquinolone synergistic activity [181, 182], there is an increased risk of emergence of ESBL-producing Enterobacteriaceae following fluoroquinolone therapy, which is not seen with aminoglycoside administration, potentially due to mutagenesis mediated by fluoroquinolone exposure [183,184,185]. Following treatment with a β-lactam antibiotic and fluoroquinolone, 15% of patients subsequently acquired an MDR pathogen compared with 4% of patients who received a β-lactam and macrolide combination in the management of community-acquired pneumonia [186]. This collateral resistance suggests fluoroquinolone use should be restricted to patients unable to tolerate β-lactams and/or aminoglycosides.
Given the increasing emergence of resistant Gram-negative bacteria, fosfomycin has been revived for clinical use; however, concerns exist regarding resistance emergence with monotherapy, and therefore combination regimens have been tested [100]. In an HFIM study, simulating airway exposure from nebulised doses, fosfomycin and amikacin combination therapy reduced the resistance emergence against P. aeruginosa that was observed with fosfomycin monotherapy [175]. In another in vitro study, meropenem and fosfomycin combinations following simulated intravenous dosing resulted in bacterial eradication and associated lack of resistance emergence [47]. Clinical studies of fosfomycin contrast with in vitro results, whereby limited resistance emergence has been identified with monotherapy [100]. Until further evidence is available, it may be prudent to use fosfomycin in combination with high-dose aminoglycosides or a carbapenem to prevent resistance emergence.
Given concerns regarding colistin hetero-resistance associated with monotherapy, use of colistin in combination therapy with another agent may reduce the emergence of colistin resistance [187, 188]. Combination therapy with a carbapenem, even if the isolate is resistant to the carbapenem, may prevent colistin resistance emergence [189, 190] and may lead to reduced mortality rates in MDR A. baumannii or P. aeruginosa infections [191]. Colistin in combination with tigecycline prevented tigecycline resistance emergence but not colistin resistance in vitro with simulated serum concentrations of both agents [192]. Polymyxin B has also been used in combination studies against MDR pathogens. Polymyxin B in combination with fosfomycin in an HFIM suppressed the emergence of two carbapenemase-producing K. pneumoniae isolates when a loading dose of polymyxin B 2.5 mg/kg was administered and followed by 1.5 mg/kg twice daily and fosfomycin 6 g as a 1 h infusion four times daily [193]. Interestingly, the same fosfomycin dose administered as a 3 h infusion did not prevent resistance emergence, evident by an MIC increase of sixfold for fosfomycin and 128-fold for polymyxin B [193]. This discrepancy in effect based on the infusion duration may suggest a concentration effect, whereby high peak fosfomycin concentrations are important to have an effect against less-susceptible bacterial subpopulations. Fosfomycin and polymyxin B combination therapy results may not extend to P. aeruginosa, with time-kill studies at clinically achievable concentrations resulting in bacterial regrowth [194]. Polymyxin B has also been used in combination with carbapenems. An HFIM study investigating a combination of polymyxin B and doripenem showed that a front-loaded continuous infusion polymyxin B regimen achieving a steady-state concentration of 5 mg/l in combination with doripenem suppressed the emergence of polymyxin B resistance over a 10-day course against a dense 1 × 109 CFU/ml starting inoculum of two polymyxin B heteroresistant strains of A. baumannii [195]. In contrast to these results, tigecycline in combination with polymyxin B has not shown consistent suppression of emergence of resistance against A. baumannii at clinically achievable concentrations in time-kill in vitro experiments [196]. Taken together, these results suggest that polymyxin B or colistin should be used in combination with a carbapenem, even if the identified bacteria are resistant to the carbapenem. Fosfomycin may suppress resistance emergence against Enterobacteriaceae but may not have consistent benefit against P. aeruginosa.
Little evidence exists regarding combination therapy against Gram-positive bacterial infections with regards to suppression of emergence of resistance. Some data exists with daptomycin and β-lactam antibiotic combinations. In vitro data suggest that daptomycin and low (0.25 × MIC) concentrations of ampicillin may prolong the time to emergence of daptomycin resistance in MRSA and VRE isolates [197].
6.2 Emergence of Resistance is Correlated with Duration of Treatment
Current evidence suggests that antimicrobial resistance emergence correlates with the duration of treatment.
Children with respiratory tract infections receiving high-dose (90 vs. 40 mg/kg/day, both in two divided doses) and short-duration (5 vs. 10 days) amoxycillin therapy have reduced subsequent carriage (24 vs. 32% for high-dose and low-dose course, respectively) 28 days after treatment of penicillin-resistant S. pneumoniae isolates [198]. Guillemot et al. [199] and Ruhe and Hasbun [200] found similar effects, where previous use of an anti-streptococcal antibiotic at low doses for prolonged durations resulted in subsequent resistance emergence for colonising and bacteraemia S. pneumoniae isolates, respectively.
Similar trends appear evident for Gram-negative bacterial infections. For susceptible E. coli isolates causing UTIs, a treatment duration of > 7 days was associated with resistance emergence for amoxicillin/ampicillin [odds ratio (OR) 1.79; 95% confidence interval (CI) 1.24–2.58] and trimethoprim (OR 4.62; 95% CI 2.73–7.82) [201]. This effect has also been seen in the treatment of VAP. In patients receiving 8 versus 15 days of treatment, subsequent infection recurrence was less likely to be due to an MDR bacteria (42.1 vs. 62.3%; p = 0.04) [202]. For patients requiring ICU admission with P. aeruginosa infections, a duration of therapy > 15 days of meropenem (OR 10; 95% CI 19.8–551), piperacillin–tazobactam (OR 4.7; 95% CI 1.8–12.4), ciprofloxacin (OR 14.5; 95% CI 2.8–75) or ceftazidime (OR 2.6; 95% CI 1.1–6) was associated with resistance emergence, but not for amikacin [203]. However, unlike the other agents investigated, meropenem resistance emergence may occur within 8 days of treatment initiation (OR 6.3; 95% CI 2.4–16.8). Importantly, resistance emergence following therapy may not occur with therapy durations < 4 days [203]. These data suggest that therapy should involve a high dose with the shortest possible duration of therapy, particularly with the carbapenems. Evidence for the treatment of intra-abdominal sepsis is similar to findings stated previously. Sawyer et al. [204] did not find a reduction in the rate of resistant organisms identified in subsequent infections, intra-abdominal or otherwise, between patients receiving 4 ± 1 or up to 10 days of antibiotic therapy. In contrast, patients with anastomotic leakage after colorectal cancer surgery who received > 5 days of antibiotics before the leakage event were twice as likely (OR 2.48; 95% CI 1.18–5.2) to acquire an MDR pathogen in either blood or peritoneal fluid, suggesting the importance of the inoculum effect for resistance emergence [205].
6.3 Biomarkers for Reducing Antibiotic Exposure
Biomarkers may assist in determining whether antibiotic therapy is indicated and in guiding the duration of antibiotic treatment.
An important distinction that may reduce the use of antibiotics is between sepsis, defined as a systemic inflammatory response syndrome (SIRS) with a presumed or documented infection, and SIRS secondary to a non-infectious cause. This can be difficult based on clinical observations alone. Many biomarkers have been reported in both animal and human trials to diagnose sepsis, but only procalcitonin and C-reactive protein (CRP) are currently available for widespread clinical use, albeit with potentially limited diagnostic value [206,207,208].
A meta-analysis conducted by Wacker et al. [209] showed that procalcitonin is sufficiently sensitive and specific to distinguish between infectious and non-infectious SIRS in a heterogeneous patient population in the emergency department and the ICU. Significant heterogeneity existed between studies, potentially reflecting differences in patient populations and procalcitonin cut-off values for infection diagnosis. Uzzan et al. [210] identified similar results in post-operative or trauma patients to distinguish SIRS from infection, evident with an area under the receiver operator curve of 0.85. In contrast, in a separate systematic review and meta-analysis [211], procalcitonin was unable to distinguish sepsis from SIRS with an area under the receiver operator curve of 0.79. Although these meta-analyses appear similar, differences in the included articles and the different procalcitonin cut-off points within the included articles in the respective meta-analyses likely limit a direct comparison of the area under the receiver operator curve values. Like any diagnostic test, the clinician must integrate the pre-test probability, involving the background prevalence and the clinical presentation of the patient when deciding on the diagnosis and treatment course.
These decisions regarding treatment initiation are often encountered in the emergency department. van der Does et al. [212] conducted a systemic review and observed that procalcitonin-guided decision making reduced antibiotic use in adults with respiratory complaints but not in paediatric patients. The impact of procalcitonin-guided antibiotic initiation is likely underestimated given the high rates of physician non-adherence in the included studies, which ranged from 6 to 20% [212]. As antibiotic use is clearly correlated with resistance emergence, at both the individual patient [213] and the national level [214], the use of biomarkers to guide antibiotic commencement would be valuable.
The use of procalcitonin-based clinical algorithms has been shown to reduce antibiotic duration in patients with sepsis or septic shock of varying aetiologies without increasing mortality [215,216,217,218,219]. Antibiotic duration reductions with use of procalcitonin vary but can be reduced by approximately 1 to 4 days. Despite reductions in antibiotic durations, the effect on resistance emergence remains largely unknown. The PRORATA trial is the only procalcitonin trial thus far to investigate the rates of emerging MDR bacteria taken from routine microbiological specimens. Despite a 23% relative reduction in days of antibiotic exposure in the procalcitonin group, no difference in the detection of MDR bacteria was observed [10]. It may be that either this reduction in duration of antibiotic therapy is insufficient to minimise resistance emergence or a more sensitive study design is required. Few other sepsis biomarkers are currently available for routine clinical use.
CRP is another currently available, clinically validated biomarker that may be useful in guiding antibiotic therapy [220]. The sensitivity (75 vs. 88%) and specificity (67 vs. 81%) of CRP is lower than procalcitonin in the diagnosis of bacterial infections; however, trends over time may provide information regarding infection resolution and prognosis [221, 222]. Despite being less specific and sensitive for diagnosing bacterial infections, no difference in antibiotic discontinuation rates in patients with severe sepsis have been identified between CRP and procalcitonin [223]. No studies have yet been conducted examining a reduction in antibiotic use based on CRP concentrations.
Further research is required to identify any reduction in resistance emergence with shorter antibiotic durations, particularly for resistance mechanism carriage in the gastrointestinal tract and in infection recurrence with resistant pathogens.
7 Conclusion
Current antibiotic dosing regimens that are presumably sufficient for clinical resolution of infections are potentially insufficient to prevent resistance emergence. However, current PK/PD ratios that predict resistance suppression are largely derived from in vitro studies that do not consider immune system involvement. Future studies are required to define antibiotic exposures required for suppression of emergence of resistance in vivo. For a few relatively well-studied antibiotics, the in vitro PK/PD ratios required for suppression of emergence of resistance are consistently high, necessitating doses that may be difficult to achieve with conventional dosing regimens, which may result in an unacceptable risk of toxicity. TDM-guided antibiotic dose individualisation is one strategy to attain these PK/PD ratios, minimise bacterial multi-drug resistance and minimise potential antibiotic toxicity. Alternative dosing strategies, such as β-lactam antibiotic continuous infusions, should be considered to minimise total daily doses required for attaining the higher PK/PD ratios. When possible, target site administration, such as nebulised aminoglycoside therapy, is useful to achieve high exposures with minimal risk of systemic toxicity. The use of combination regimens to prevent resistance emergence is supported by in vitro experiments but not yet by clinical evidence. Biomarkers such as procalcitonin and CRP are helpful to guide individualisation of the duration of antibiotic therapy, although evidence for minimising resistance is lacking. Overall, current knowledge on antibiotic strategies that prevent resistance emergence is meagre. Future studies should describe appropriate PK/PD predictors or clinical biomarkers associated with resistance suppression and validate their utility for individualising therapy at the bedside.
References
Satlin MJ, Cohen N, Ma KC, Gedrimaite Z, Soave R, Askin G, et al. Bacteremia due to carbapenem-resistant Enterobacteriaceae in neutropenic patients with hematologic malignancies. J Infect. 2016;73:336–45.
Ben-David D, Kordevani R, Keller N, Tal I, Marzel A, Gal-Mor O, et al. Outcome of carbapenem resistant Klebsiella pneumoniae bloodstream infections. Clin Microbiol Infect. 2012;18:54–60.
Looke DFM, Gottlieb T, Jones CA, Paterson DL. Gram-negative resistance: can we combat the coming of a new “Red Plague”? MJA. 2013;198:243–4.
Walsh TR, Weeks J, Livermore DM, Toleman MA. Dissemination of NDM-1 positive bacteria in the New Delhi environment and its implications for human health: an environmental point prevalence study. Lancet Infect Dis. 2011;11:355–62.
Deak D, Outterson K, Powers JH, Kesselheim AS. Progress in the fight against multidrug-resistant bacteria? A review of US Food and Drug Administration-Approved Antibiotics, 2010–2015. Ann Intern Med. 2016;165:363–72.
Combes A, Luyt CE, Fagon JY, Wolff M, Trouillet JL, Chastre J, et al. Early predictors for infection recurrence and death in patients with ventilator-associated pneumonia. Crit Care Med. 2007;35:146–54.
Fernandez-Cuenca F, Gomez-Sanchez M, Rodriguez-Bano J, Martinez-Martinez L, Vila J, Bou G, et al. Epidemiological and clinical features associated with colonisation/infection by Acinetobacter baumannii with phenotypic heterogeneous resistance to carbapenems. Int J Antimicrob Agents. 2012;40:235–8.
Abdul-Aziz MH, Lipman J, Mouton JW, Hope WW, Roberts JA. Applying pharmacokinetic/pharmacodynamic principles in critically ill patients: optimizing efficacy and reducing resistance development. Semin Respir Crit Care Med. 2015;36:136–53.
Sager R, Kutz A, Mueller B, Schuetz P. Procalcitonin-guided diagnosis and antibiotic stewardship revisited. BMC Med. 2017;15:11.
Bouadma L, Luyt C-E, Tubach F, Cracco C, Alvarez A, Schwebel C, et al. Use of procalcitonin to reduce patients’ exposure to antibiotics in intensive care units (PRORATA trial): a multicentre randomised controlled trial. Lancet. 2010;375:463–74.
Tsai D, Lipman J, Roberts JA. Pharmacokinetic/pharmacodynamic considerations for the optimization of antimicrobial delivery in the critically ill. Curr Opin Crit Care. 2015;21:412–20.
Scaglione F, Esposito S, Leone S, Lucini V, Pannacci M, Ma L, et al. Feedback dose alteration significantly affects probability of pathogen eradication in nosocomial pneumonia. Eur Resp J. 2009;34:394–400.
Roberts JA, Abdul-Aziz MH, Lipman J, Mouton JW, Vinks AA, Felton TW, et al. Individualised antibiotic dosing for patients who are critically ill: challenges and potential solutions. Lancet Infect Dis. 2014;14:498–509.
Roberts JA, Lipman J. Pharmacokinetic issues for antibiotics in the critically ill patient. Crit Care Med. 2009;37:840–51.
Lodise TP Jr, Lomaestro B, Drusano GL. Piperacillin-tazobactam for Pseudomonas aeruginosa infection: clinical implications of an extended-infusion dosing strategy. Clin Infect Dis. 2007;44:357–63.
Roberts JA, Abdul-Aziz MH, Davis JS, Dulhunty JM, Cotta MO, Myburgh J, et al. Continuous versus intermittent beta-lactam infusion in severe sepsis. A meta-analysis of individual patient data from randomized trials. Am J Respir Crit Care Med. 2016;194:681–91.
Craig WA. Pharmacokinetic/pharmacodynamic parameters: rationale for antibacterial dosing of mice and men. Clin Infect Dis. 1998;26:1–10.
Moore RD, Lietman PS, Smith CR. Clinical response to aminoglycoside therapy: importance of the ratio of peak concentration to minimal inhibitory concentration. J Infect Dis. 1987;155:93–9.
Pajot O, Burdet C, Couffignal C, Massias L, Armand-Lefevre L, Foucrier A, et al. Impact of imipenem and amikacin pharmacokinetic/pharmacodynamic parameters on microbiological outcome of Gram-negative bacilli ventilator-associated pneumonia. J Antimicrob Chemother. 2015;70:1487–94.
Tam VH, Ledesma KR, Vo G, Kabbara S, Lim TP, Nikolaou M. Pharmacodynamic modeling of aminoglycosides against Pseudomonas aeruginosa and Acinetobacter baumannii: identifying dosing regimens to suppress resistance development. Antimicrob Agents Chemother. 2008;52:3987–93.
Zelenitsky SA, Harding GK, Sun S, Ubhi K, Ariano RE. Treatment and outcome of Pseudomonas aeruginosa bacteraemia: an antibiotic pharmacodynamic analysis. J Antimicrob Chemother. 2003;52:668–74.
Smith PF, Ballow CH, Booker BM, Forrest A, Schentag JJ. Pharmacokinetics and pharmacodynamics of aztreonam and tobramycin in hospitalized patients. Clin Ther. 2001;23:1231–44.
Sinnollareddy MG, Roberts MS, Lipman J, Roberts JA. β-Lactam pharmacokinetics and pharmacodynamics in critically ill patients and strategies for dose optimization: a structured review. Clin Exp Pharmacol Physiol. 2012;39:489–96.
Craig WA. Basic pharmacodynamics of antibacterials with clinical applications to the use of beta-lactams, glycopeptides, and linezolid. Infect Dis Clin North Am. 2003;17:479–501.
Felton TW, Goodwin J, O’Connor L, Sharp A, Gregson L, Livermore J, et al. Impact of bolus dosing versus continuous infusion of piperacillin and tazobactam on the development of antimicrobial resistance in Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2013;57:5811–9.
Cafini F, Aguilar L, Sevillano D, Gimenez MJ, Alou L, Fenoll A, et al. Decrease in bacterial load versus resistance selection of pneumococcal subpopulations by beta-lactam physiological concentrations over time: an in vitro pharmacodynamic simulation. Microb Drug Resist. 2008;14:13–21.
Tam VH, Chang KT, Zhou J, Ledesma KR, Phe K, Gao S, et al. Determining beta-lactam exposure threshold to suppress resistance development in Gram-negative bacteria. J Antimicrob Chemother. 2017;72:1421–8.
Tam VH, Schilling AN, Neshat S, Poole K, Melnick DA, Coyle EA. Optimization of meropenem minimum concentration/MIC ratio to suppress in vitro resistance of Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2005;49:4920–7.
Li X, Wang L, Zhang XJ, Yang Y, Gong WT, Xu B, et al. Evaluation of meropenem regimens suppressing emergence of resistance in Acinetobacter baumannii with human simulated exposure in an in vitro intravenous-infusion hollow-fiber infection model. Antimicrob Agents Chemother. 2014;58:6773–81.
Zelenitsky SA, Ariano RE. Support for higher ciprofloxacin AUC(24)/MIC targets in treating Enterobacteriaceae bloodstream infection. J Antimicrob Chemother. 2010;65:1725–32.
Forrest A, Nix DE, Ballow CH, Goss TF, Birmingham MC, Schentag JJ. Pharmacodynamics of intravenous ciprofloxacin in seriously ill patients. Antimicrob Agents Chemother. 1993;37:1073–81.
Madaras-Kelly KJ, Ostergaard BE, Hovde LB, Rotschafer JC. Twenty-four-hour area under the concentration-time curve MIC ratio as a generic predictor of fluoroquinolone antimicrobial effect by using three strains of Pseudomonas aeruginosa and an in vitro pharmacodynamic model. Antimicrob Agents Chemother. 1996;40:627–32.
Ambrose PG, Grasela DM, Grasela TH, Passarell J, Mayer HB, Pierce PF. Pharmacodynamics of fluoroquinolones against Streptococcus pneumoniae in patients with community-acquired respiratory tract infections. Antimicrob Agents Chemother. 2001;45:2793–7.
Tam VH, Louie A, Deziel MR, Liu WG, Drusano GL. The relationship between quinolone exposures and resistance amplification is characterized by an inverted U: a new paradigm for optimizing pharmacodynamics to counterselect resistance. Antimicrob Agents Chemother. 2007;51:744–7.
Firsov AA, Vostrov SN, Lubenko IY, Drlica K, Portnoy YA, Zinner SH. In vitro pharmacodynamic evaluation of the mutant selection window hypothesis using four fluoroquinolones against Staphylococcus aureus. Antimicrob Agents Chemother. 2003;47:1604–13.
Olofsson SK, Marcusson LL, Lindgren PK, Hughes D, Cars O. Selection of ciprofloxacin resistance in Escherichia coli in an in vitro kinetic model: relation between drug exposure and mutant prevention concentration. J Antimicrob Chemother. 2006;57:1116–21.
Holmes NE, Turnidge JD, Munckhof WJ, Robinson JO, Korman TM, O’Sullivan MV, et al. Vancomycin AUC/MIC ratio and 30-day mortality in patients with Staphylococcus aureus bacteremia. Antimicrob Agents Chemother. 2013;57:1654–63.
Firsov AA, Smirnova MV, Lubenko IY, Vostrov SN, Portnoy YA, Zinner SH. Testing the mutant selection window hypothesis with Staphylococcus aureus exposed to daptomycin and vancomycin in an in vitro dynamic model. J Antimicrob Chemother. 2006;58:1185–92.
Lenhard JR, Brown T, Rybak MJ, Meaney CJ, Norgard NB, Bulman ZP, et al. Sequential evolution of vancomycin-intermediate resistance alters virulence in Staphylococcus aureus: pharmacokinetic/pharmacodynamic targets for vancomycin exposure. Antimicrob Agents Chemother. 2016;60:1584–91.
Rayner CR, Forrest A, Meagher AK, Birmingham MC, Schentag JJ. Clinical pharmacodynamics of linezolid in seriously ill patients treated in a compassionate use programme. Clin Pharmacokinet. 2003;42:1411–23.
Dong HY, Wang X, Dong YL, Lei JE, Li H, You HS, et al. Clinical pharmacokinetic/pharmacodynamic profile of linezolid in severely ill intensive care unit patients. Int J Antimicrob Agents. 2011;38:296–300.
Tsuji BT, Bulitta JB, Brown T, Forrest A, Kelchlin PA, Holden PN, et al. Pharmacodynamics of early, high-dose linezolid against vancomycin-resistant enterococci with elevated MICs and pre-existing genetic mutations. J Antimicrob Chemother. 2012;67:2182–90.
Tsuji BT, Brown T, Parasrampuria R, Brazeau DA, Forrest A, Kelchlin PA, et al. Front-loaded linezolid regimens result in increased killing and suppression of the accessory gene regulator system of Staphylococcus aureus. Antimicrob Agents Chemother. 2012;56:3712–9.
Safdar N, Andes D, Craig WA. In vivo pharmacodynamic activity of daptomycin. Antimicrob Agents Chemother. 2004;48:63–8.
Dudhani RV, Turnidge JD, Nation RL, Li J. fAUC/MIC is the most predictive pharmacokinetic/pharmacodynamic index of colistin against Acinetobacter baumannii in murine thigh and lung infection models. J Antimicrob Chemother. 2010;65:1984–90.
Lepak AJ, Zhao M, VanScoy B, Taylor DS, Ellis-Grosse E, Ambrose PG, et al. In vivo pharmacokinetics and pharmacodynamics of ZTI-01 (fosfomycin for injection) in the neutropenic murine thigh infection model against Escherichia coli, Klebsiella pneumoniae, and Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2017. https://doi.org/10.1128/AAC.00476-17.
Docobo-Perez F, Drusano GL, Johnson A, Goodwin J, Whalley S, Ramos-Martin V, et al. Pharmacodynamics of fosfomycin: insights into clinical use for antimicrobial resistance. Antimicrob Agents Chemother. 2015;59:5602–10.
Gugel J, dos Santos Pereira A, Pignatari ACC, Gales AC. β-Lactam MICs correlate poorly with mutant prevention concentrations for clinical isolates of Acinetobacter spp. and Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2006;50:2276–7.
Hansen GT, Zhao XL, Drlica K, Blondeau JM. Mutant prevention concentration for ciprofloxacin and levofloxacin with Pseudomonas aeruginosa. Int J Antimicrob Agents. 2006;27:120–4.
Jumbe N. Application of a mathematical model to prevent in vivo amplification of antibiotic-resistant bacterial populations during therapy. J Clin Invest. 2003;112:275–85.
Credito K, Kosowska-Shick K, Appelbaum PC. Mutant prevention concentrations of four carbapenems against gram-negative rods. Antimicrob Agents Chemother. 2010;54:2692–5.
Diez-Aguilar M, Morosini MI, Tedim AP, Rodriguez I, Aktas Z, Canton R. Antimicrobial activity of fosfomycin–tobramycin combination against Pseudomonas aeruginosa isolates assessed by time-kill assays and mutant prevention concentrations. Antimicrob Agents Chemother. 2015;59:6039–45.
Blondeau JM, Shebelski SD, Hesje CK. Killing of Streptococcus pneumoniae by azithromycin, clarithromycin, erythromycin, telithromycin and gemifloxacin using drug minimum inhibitory concentrations and mutant prevention concentrations. Int J Antimicrob Agents. 2015;45:594–9.
Drusano GL, Liu W, Fikes S, Cirz R, Robbins N, Kurhanewicz S, et al. Interaction of drug- and granulocyte-mediated killing of Pseudomonas aeruginosa in a murine pneumonia model. J Infect Dis. 2014;210:1319–24.
Hesje CK, Tillotson GS, Blondeau JM. MICs, MPCs and PK/PDs: a match (sometimes) made in hosts. Expert Rev Respir Med. 2007;1:7–16.
Drlica K, Zhao X. Mutant selection window hypothesis updated. Clin Infect Dis. 2007;44:681–8.
Dahdouh E, Shoucair SH, Salem SE, Daoud Z. Mutant prevention concentrations of imipenem and meropenem against Pseudomonas aeruginosa and Acinetobacter baumannii. Sci World J. 2014;2014:979648.
Wiegand I, Hilpert K, Hancock RE. Agar and broth dilution methods to determine the minimal inhibitory concentration (MIC) of antimicrobial substances. Nat Protoc. 2008;3:163–75.
Bruins MJ, Bloembergen P, Ruijs G, Wolfhagen M. Identification and susceptibility testing of Enterobacteriaceae and Pseudomonas aeruginosa by direct inoculation from positive BACTEC blood culture bottles into Vitek 2. J Clin Microbiol. 2004;42:7–11.
Liu LG, Zhu YL, Hu LF, Cheng J, Ye Y, Li JB. Comparative study of the mutant prevention concentrations of vancomycin alone and in combination with levofloxacin, rifampicin and fosfomycin against methicillin-resistant Staphylococcus epidermidis. J Antibiot. 2013;66:709–12.
Allen GP, Kaatz GW, Rybak MJ. Activities of mutant prevention concentration-targeted moxifloxacin and levofloxacin against Streptococcus pneumoniae in an in vitro pharmacodynamic model. Antimicrob Agents Chemother. 2003;47:2606–14.
Olofsson SK, Marcusson LL, Stromback A, Hughes D, Cars O. Dose-related selection of fluoroquinolone-resistant Escherichia coli. J Antimicrob Chemother. 2007;60:795–801.
Breakpoint tables for interpretation of MICs and zone diameters: The European Committee on Antimicrobial Susceptibility Testing; 2017. http://eucast.org. Accessed 24 Jan 2017.
Burdet C, Pajot O, Couffignal C, Armand-Lefevre L, Foucrier A, Laouenan C, et al. Population pharmacokinetics of single-dose amikacin in critically ill patients with suspected ventilator-associated pneumonia. Eur J Clin Pharmacol. 2015;71:75–83.
Frippiat F, Musuamba FT, Seidel L, Albert A, Denooz R, Charlier C, et al. Modelled target attainment after meropenem infusion in patients with severe nosocomial pneumonia: the PROMESSE study. J Antimicrob Chemother. 2015;70:207–16.
Haeseker M, Stolk L, Nieman F, Hoebe C, Neef C, Bruggeman C, et al. The ciprofloxacin target AUC:MIC ratio is not reached in hospitalized patients with the recommended dosing regimens. Br J Clin Pharmacol. 2013;75:180–5.
Alobaid AS, Wallis SC, Jarrett P, Starr T, Stuart J, Lassig-Smith M, et al. Population pharmacokinetics of piperacillin in nonobese, obese, and morbidly obese critically ill patients. Antimicrob Agents Chemother. 2017. https://doi.org/10.1128/AAC.01276-16.
Mouton JW, Muller AE, Canton R, Giske CG, Kahlmeter G, Turnidge J. MIC-based dose adjustment: facts and fables. J Antimicrob Chemother. 2017. https://doi.org/10.1093/jac/dkx427.
Tankovic J, Perichon B, Duval J, Courvalin P. Contribution of mutations in gyrA and parC genes to fluoroquinolone resistance of mutants of Streptococcus pneumoniae obtained in vivo and in vitro. Antimicrob Agents Chemother. 1996;40:2505–10.
Ince D, Aras R, Hooper DC. Mechanisms and frequency of resistance to gatifloxacin in comparison with ciprofloxacin in Staphylococcus aureus. Drugs. 1999;58:134–5.
Ince D, Aras R, Hooper DC. Mechanisms and frequency of resistance to moxifloxacin in comparison with ciprofloxacin in Staphylococcus aureus. Drugs. 1999;58:132–3.
Riesenfeld C, Everett M, Piddock LJV, Hall BG. Adaptive mutations produce resistance to ciprofloxacin. Antimicrob Agents Chemother. 1997;41:2059–60.
Morero NR, Monti MR, Argarana CE. Effect of ciprofloxacin concentration on the frequency and nature of resistant mutants selected from Pseudomonas aeruginosa mutS and mutT hypermutators. Antimicrob Agents Chemother. 2011;55:3668–76.
Drago L, De Vecchi E, Nicola L, Tocalli L, Gismondo MR. In vitro selection of resistance in Pseudomonas aeruginosa and Acinetobacter spp. by levofloxacin and ciprofloxacin alone and in combination with beta-lactams and amikacin. J Antimicrob Chemother. 2005;56:353–9.
Schedletzky H, Wiedemann B, Heisig P. The effect of moxifloxacin on its target topoisomerases from Escherichia coli and Staphylococcus aureus. J Antimicrob Chemother. 1999;43:31–7.
Baldesi O, Michel F, Guervilly C, Embriaco N, Granfond A, La Scola B, et al. Bacterial ventilator-associated pneumonia: bronchoalveolar lavage results are not influenced by dilution. Intensive Care Med. 2009;35:1210–5.
Jager NGL, van Hest RM, Lipman J, Taccone FS, Roberts JA. Therapeutic drug monitoring of anti-infective agents in critically ill patients. Expert Rev Clin Pharmacol. 2016;9:961–79.
Felton TW, Hope WW, Roberts JA. How severe is antibiotic pharmacokinetic variability in critically ill patients and what can be done about it? Diagn Microbiol Infect Dis. 2014;79:441–7.
Roberts JA, Paul SK, Akova M, Bassetti M, De Waele JJ, Dimopoulos G, et al. DALI: defining antibiotic levels in intensive care unit patients: are current beta-lactam antibiotic doses sufficient for critically ill patients? Clin Infect Dis. 2014;58:1072–83.
Roberts JA, Ulldemolins M, Roberts MS, McWhinney B, Ungerer J, Paterson DL, et al. Therapeutic drug monitoring of beta-lactams in critically ill patients: proof of concept. Int J Antimicrob Agents. 2010;36:332–9.
Duszynska W, Taccone FS, Hurkacz M, Kowalska-Krochmal B, Wiela-Hojenska A, Kubler A. Therapeutic drug monitoring of amikacin in septic patients. Crit Care. 2013;17:10.
Pea F, Furlanut M, Negri C, Pavan F, Crapis M, Cristini F, et al. Prospectively validated dosing nomograms for maximizing the pharmacodynamics of vancomycin administered by continuous infusion in critically ill patients. Antimicrob Agents Chemother. 2009;53:1863–7.
Galar A, Valerio M, Munoz P, Alcala L, Garcia-Gonzalez X, Burillo A, et al. Systematic therapeutic drug monitoring for linezolid: variability and clinical impact. Antimicrob Agents Chemother. 2017. https://doi.org/10.1128/AAC.00687-17.
Pea F, Cojutti P, Sbrojavacca R, Cadeo B, Cristini F, Bulfoni A, et al. TDM-guided therapy with daptomycin and meropenem in a morbidly obese, critically ill patient. Ann Pharmacother. 2011. https://doi.org/10.1345/aph.1P745.
Allou N, Bouteau A, Allyn J, Snauwaert A, Valance D, Jabot J, et al. Impact of a high loading dose of amikacin in patients with severe sepsis or septic shock. Ann Intensive Care. 2016. https://doi.org/10.1186/s13613-016-0211-z.
Abdul-Aziz MH, Sulaiman H, Mat-Nor MB, Rai V, Wong KK, Hasan MS, et al. Beta-lactam infusion in severe sepsis (BLISS): a prospective, two-centre, open-labelled randomised controlled trial of continuous versus intermittent beta-lactam infusion in critically ill patients with severe sepsis. Intensive Care Med. 2016;42:1535–45.
Drusano GL, Bonomo RA, Bahniuk N, Bulitta JB, VanScoy B, DeFiglio H, et al. Resistance emergence mechanism and mechanism of resistance suppression by tobramycin for cefepime for Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2012;56:231–42.
Kashuba ADM, Nafziger AN, Drusano GL, Bertino JS. Optimizing aminoglycoside therapy for nosocomial pneumonia caused by Gram-negative bacteria. Antimicrob Agents Chemother. 1999;43:623–9.
Drusano GL, Louie A. Optimization of aminoglycoside therapy. Antimicrob Agents Chemother. 2011;55:2528–31.
Layeux B, Taccone FS, Fagnoul D, Vincent JL, Jacobs F. Amikacin monotherapy for sepsis caused by pan resistant Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2010;54:4939–41.
Roger C, Nucci B, Molinari N, Bastide S, Saissi G, Pradel G, et al. Standard dosing of amikacin and gentamicin in critically ill patients results in variable and subtherapeutic concentrations. Int J Antimicrob Agents. 2015;46:21–7.
Roger C, Nucci B, Louart B, Friggeri A, Knani H, Evrard A, et al. Impact of 30 mg/kg amikacin and 8 mg/kg gentamicin on serum concentrations in critically ill patients with severe sepsis. J Antimicrob Chemother. 2016;71:208–12.
Luyt CE, Clavel M, Guntupalli K, Johannigman J, Kennedy JI, Wood C, et al. Pharmacokinetics and lung delivery of PDDS-aerosolized amikacin (NKTR-061) in intubated and mechanically ventilated patients with nosocomial pneumonia. Crit Care. 2009. https://doi.org/10.1186/cc8206.
Sole-Lleonart C, Rouby JJ, Blot S, Poulakou G, Chastre J, Palmer LB, et al. Nebulization of antiinfective agents in invasively mechanically ventilated adults: a systematic review and meta-analysis. Anesthesiology. 2017;126:890–908.
Labovitz E, Levison ME, Kaye D. Single-dose daily gentamicin therapy in urinary tract infection. Antimicrob Agents Chemother. 1974;6:465–70.
Michalopoulos AS, Livaditis IG, Gougoutas V. The revival of fosfomycin. Int J Infect Dis. 2011;15:E732–9.
VanScoy BD, McCauley J, Ellis-Grosse EJ, Okusanya OO, Bhavnani SM, Forrest A, et al. Exploration of the pharmacokinetic-pharmacodynamic relationships for fosfomycin efficacy using an in vitro infection model. Antimicrob Agents Chemother. 2015;59:7170–7.
Mazzei T, Cassetta MI, Fallani S, Arrigucci S, Novelli A. Pharmacokinetic and pharmacodynamic aspects of antimicrobial agents for the treatment of uncomplicated urinary tract infections. Int J Antimicrob Agents. 2006;28:S35–41.
Abbott IJ, Meletiadis J, Belghanch I, Wijma RA, Kanioura L, Roberts JA, et al. Fosfomycin efficacy and emergence of resistance among Enterobacteriaceae in an in vitro dynamic bladder infection model. J Antimicrob Chemother. 2017. https://doi.org/10.1093/jac/dkx441.
Karageorgopoulos DE, Wang R, Yu XH, Falagas ME. Fosfomycin: evaluation of the published evidence on the emergence of antimicrobial resistance in Gram-negative pathogens. J Antimicrob Chemother. 2012;67:255-68.
Parker SL, Frantzeskaki F, Wallis SC, Diakaki C, Giamarellou H, Koulenti D, et al. Population pharmacokinetics of fosfomycin in critically ill patients. Antimicrob Agents Chemother. 2015;59:6471–6.
Matzi V, Lindenmann J, Porubsky C, Kugler SA, Maier A, Dittrich P, et al. Extracellular concentrations of fosfomycin in lung tissue of septic patients. J Antimicrob Chemother. 2010;65:995–8.
Montgomery AB, Vallance S, Abuan T, Tservistas M, Davies A. A randomized double-blind placebo-controlled dose-escalation phase 1 study of aerosolized amikacin and fosfomycin delivered via the PARI investigational eflow (R) inline nebulizer system in mechanically ventilated patients. J Aerosol Med Pulm Drug Deliv. 2014;27:441–8.
McKinnon PS, Paladino JA, Schentag JJ. Evaluation of area under the inhibitory curve (AUIC) and time above the minimum inhibitory concentration (T > MIC) as predictors of outcome for cefepime and ceftazidime in serious bacterial infections. Int J Antimicrob Agents. 2008;31:345–51.
Tam VH, McKinnon PS, Akins RL, Rybak MJ, Drusano GL. Pharmacodynamics of cefepime in patients with Gram-negative infections. J Antimicrob Chemother. 2002;50:425–8.
Rhodes NJ, Kuti JL, Nicolau DP, Van Wart S, Nicasio AM, Liu JJ, et al. Defining Clinical Exposures of Cefepime for Gram-Negative Bloodstream Infections That Are Associated with Improved Survival. Antimicrob Agents Chemother. 2016;60:1401–10.
Aitken SL, Altshuler J, Guervil DJ, Hirsch EB, Ostrosky-Zeichner LL, Ericsson CD, et al. Cefepime free minimum concentration to minimum inhibitory concentration (fC(min)/MIC) ratio predicts clinical failure in patients with Gram-negative bacterial pneumonia. Int J Antimicrob Agents. 2015;45:541–4.
Crandon JL, Luyt C-E, Aubry A, Chastre J, Nicolau DP. Pharmacodynamics of carbapenems for the treatment of Pseudomonas aeruginosa ventilator-associated pneumonia: associations with clinical outcome and recurrence. J Antimicrob Chemother. 2016;71:2534.
Tam VH, Ledesma KR, Schilling AN, Lim T-P, Yuan Z, Ghose R, et al. In vivo dynamics of carbapenem-resistant Pseudomonas aeruginosa selection after suboptimal dosing. Diagn Microbiol Infect Dis. 2009;64:427–33.
Zinner SH, Gilbert D, Greer K, Portnoy YA, Firsov AA. Concentration–Resistance relationships with Pseudomonas aeruginosa exposed to doripenem and ciprofloxacin in an in vitro model. J Antimicrob Chemother. 2013;68:881–7.
VanScoy BD, Mendes RE, Castanheira M, McCauley J, Bhavnani SM, Jones RN, et al. Relationship between ceftolozane-tazobactam exposure and selection for Pseudomonas aeruginosa resistance in a hollow-fiber infection model. Antimicrob Agents Chemother. 2014;58:6024–31.
Vanscoy B, Mendes RE, Castanheira M, McCauley J, Bhavnani SM, Forrest A, et al. Relationship between ceftolozane-tazobactam exposure and drug resistance amplification in a hollow-fiber infection model. Antimicrob Agents Chemother. 2013;57:4134–8.
Coleman K, Levasseur P, Girard AM, Borgonovi M, Miossec C, Merdjan H, et al. Activities of ceftazidime and avibactam against β-lactamase-producing enterobacteriaceae in a hollow-fiber pharmacodynamic model. Antimicrob Agents Chemother. 2014;58:3366–72.
Crandon JL, Schuck VJ, Banevicius MA, Beaudoin ME, Nichols WW, Tanudra MA, et al. Comparative In vitro and in vivo efficacies of human simulated doses of ceftazidime and ceftazidime-avibactam against Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2012;56:6137–46.
Shields RK, Potoski BA, Haidar G, Hao B, Doi Y, Chen L, et al. Clinical outcomes, drug toxicity, and emergence of ceftazidime–avibactam resistance among patients treated for carbapenem-resistant enterobacteriaceae infections. Clin Infect Dis. 2016;63:1615–8.
Boselli E, Breilh D, Rimmele T, Poupelin JC, Saux MC, Chassard D, et al. Plasma and lung concentrations of ceftazidime administered in continuous infusion to critically ill patients with severe nosocomial pneumonia. Intensive Care Med. 2004;30:989–91.
Roberts DM, Liu X, Roberts JA, Nair P, Cole L, Roberts MS, et al. A multicenter study on the effect of continuous hemodiafiltration intensity on antibiotic pharmacokinetics. Crit Care. 2015;19:84.
Linder KE, Nicolau DP, Nailor MD. Predicting and preventing antimicrobial resistance utilizing pharmacodynamics: Part I gram positive bacteria. Exp Opin Drug Metab Toxicol. 2016;12:267–80.
May F, El-Helali N, Timsit JF, Misset B. Absence of obvious link between supratherapeutic serum levels of beta lactams and clinical toxicity in ICU patients with acute renal failure treated with intermittent hemodialysis. Crit Care. 2016. https://doi.org/10.1186/s13054-016-1394-2.
McDonald C, Cotta MO, Little PJ, McWhinney B, Ungerer JPJ, Lipman J, et al. Is high-dose beta-lactam therapy associated with excessive drug toxicity in critically ill patients? Miner Anestesiol. 2016;82:957–65.
Carlier M, Carrette S, Roberts JA, Stove V, Verstraete A, Hoste E, et al. Meropenem and piperacillin/tazobactam prescribing in critically ill patients: does augmented renal clearance affect pharmacokinetic/pharmacodynamic target attainment when extended infusions are used? Crit Care. 2013. https://doi.org/10.1186/cc12705.
Sime FB, Roberts MS, Peake SL, Lipman J, Roberts JA. Does beta-lactam pharmacokinetic variability in critically ill patients justify therapeutic drug monitoring? a systematic review. Ann Intensive Care. 2012. https://doi.org/10.1186/2110-5820-2-35.
Cotta MO, Gowen B, Truloff N, Bursle E, McWhinney B, Ungerer JPJ, et al. Even high-dose extended infusions may not yield desired concentrations of beta-lactams: the value of therapeutic drug monitoring. Infect Dis. 2015;47:739–42.
Boselli E, Breilh D, Rimmele T, Guillaume C, Xuereb F, Saux MC, et al. Alveolar concentrations of pipeyacillin/tazobactam administered in continuous infusion to patients with ventilatoy-associated pneumonia. Crit Care Med. 2008;36:1500–6.
Rodvold KA, George JM, Yoo L. Penetration of anti-infective agents into pulmonary epithelial lining fluid: focus on antibacterial agents. Clin Pharmacokinet. 2011;50:637–64.
Boselli E, Breilh D, Duflo F, Saux MC, Debon R, Chassard D, et al. Steady-state plasma and intrapulmonary concentrations of cefepime administered in continuous infusion in critically ill patients with severe nosocomial pneumonia. Crit Care Med. 2003;31:2102–6.
Plachouras D, Karvanen M, Friberg LE, Papadomichelakis E, Antoniadou A, Tsangaris I, et al. Population pharmacokinetic analysis of colistin methanesulfonate and colistin after intravenous administration in critically ill patients with infections caused by Gram-negative bacteria. Antimicrob Agents Chemother. 2009;53:3430–6.
Garonzik SM, Li J, Thamlikitkul V, Paterson DL, Shoham S, Jacob J, et al. Population pharmacokinetics of colistin methanesulfonate and formed colistin in critically ill patients from a multicenter study provide dosing suggestions for various categories of patients. Antimicrob Agents Chemother. 2011;55:3284–94.
Bergen PJ, Li J, Nation RL, Turnidge JD, Coulthard K, Milne RW. Comparison of once-, twice- and thrice-daily dosing of colistin on antibacterial effect and emergence of resistance: studies with Pseudomonas aeruginosa in an in vitro pharmacodynamic model. J Antimicrob Chemother. 2008;61:636–42.
Dalfino L, Puntillo F, Mosca A, Monno R, Spada ML, Coppolecchia S, et al. High-dose, extended-interval colistin administration in critically ill patients: is this the right dosing strategy? a preliminary study. Clin Infect Dis. 2012;54:1720–6.
Athanassa ZE, Markantonis SL, Fousteri MZF, Myrianthefs PM, Boutzouka EG, Tsakris A, et al. Pharmacokinetics of inhaled colistimethate sodium (CMS) in mechanically ventilated critically ill patients. Intensive Care Med. 2012;38:1779–86.
Imberti R, Cusato M, Villani P, Carnevale L, Iotti GA, Langer M, et al. Steady-state pharmacokinetics and BAL concentration of colistin in critically ill patients after IV colistin methanesulfonate administration. Chest. 2010;138:1333–9.
Nordqvist H, Nilsson LE, Claesson C. Mutant prevention concentration of colistin alone and in combination with rifampicin for multidrug-resistant Acinetobacter baumannii. Eur J Clin Microbiol Infect Dis. 2016;35:1845–50.
Cheah SE, Li J, Tsuji BT, Forrest A, Bulitta JB, Nation RL. Colistin and polymyxin b dosage regimens against Acinetobacter baumannii: differences in activity and the emergence of resistance. Antimicrob Agents Chemother. 2016;60:3921–33.
Tsuji BT, Landersdorfer CB, Lenhard JR, Cheah SE, Thamlikitkul V, Rao GG, et al. Paradoxical effect of polymyxin b: high drug exposure amplifies resistance in Acinetobacter baumannii. Antimicrob Agents Chemother. 2016;60:3913–20.
Sauermann R, Rothenburger M, Graninger W, Joukhadar C. Daptomycin: a review 4 years after first approval. Pharmacology. 2008;81:79–91.
Benvenuto M, Benziger DP, Yankelev S, Vigliani G. Pharmacokinetics and tolerability of daptomycin at doses up to 12 milligrams per kilogram of body weight once daily in healthy volunteers. Antimicrob Agents Chemother. 2006;50:3245–9.
D’Avolio A, Pensi D, Baietto L, Pacini G, Di Perri G, De Rosa FG. Daptomycin pharmacokinetics and pharmacodynamics in septic and critically ill patients. Drugs. 2016;76:1161–74.
Rose WE, Leonard SN, Rybak MJ. Evaluation of daptomycin pharmacodynamics and resistance at various dosage regimens against Staphylococcus aureus isolates with reduced susceptibilities to daptomycin in an in vitro pharmacodynamic model with simulated endocardial vegetations. Antimicrob Agents Chemother 2008;52:3061–7.
Sabol K, Patterson JE, Lewis Ii JS, Owens A, Cadena J, Jorgensen JH. Emergence of daptomycin resistance in Enterococcus faecium during daptomycin therapy. Antimicrob Agents Chemother. 2005;49:1664–5.
Falcone M, Russo A, Venditti M, Novelli A, Pai MP. Considerations for higher doses of daptomycin in critically ill patients with methicillin-resistant Staphylococcus aureus bacteremia. Clin Infect Dis. 2013;57:1568–76.
Drusano GL, Johnson DE, Rosen M, Standiford HC. Pharmacodynamics of a fluoroquinolone antimicrobial agent in a neutropenic rat model of Pseudomonas sepsis. Antimicrob Agents Chemother. 1993;37:483–90.
Tam VH, Louie A, Deziel MR, Liu WG, Leary R, Drusano GL. Bacterial-population responses to drug-selective pressure: Examination of garenoxacin's effect on Pseudomonas aeruginosa. J Infect Dis. 2005;192:420–8.
van Zanten ARH, Polderman KH, van Geijlswijk IM, van der Meer GYG, Schouten MA, Girbes ARJ. Ciprofloxacin pharmacokinetics in critically ill patients: a prospective cohort study. J Crit Care. 2008;23:422–30.
Cazaubon Y, Bourguignon L, Goutelle S, Martin O, Maire P, Ducher M. Are ciprofloxacin dosage regimens adequate for antimicrobial efficacy and prevention of resistance? Pseudomonas aeruginosa bloodstream infection in elderly patients as a simulation case study. Fundam Clin Pharmacol. 2015;29:615–24.
Lipman J, Scribante J, Gous AGS, Hon H, Tshukutsoane S, The Baragwanath Ciprofloxacin Study G. Pharmacokinetic profiles of high-dose intravenous ciprofloxacin in severe sepsis. Antimicrob Agents Chemother. 1998;42:2235–9.
Zinner SH, Lubenko IY, Gilbert D, Simmons K, Zhao XL, Drlica K, et al. Emergence of resistant Streptococcus pneumoniae in an in vitro dynamic model that simulates moxifloxacin concentrations inside and outside the mutant selection window: related changes in susceptibility, resistance frequency and bacterial killing. J Antimicrob Chemother. 2003;52:616–22.
Pletz MW, Bloos F, Burkhardt O, Brunkhorst FM, Bode-Boger SM, Martens-Lobenhoffer J, et al. Pharmacokinetics of moxifloxacin in patients with severe sepsis or septic shock. Intensive Care Med. 2010;36:979–83.
MacGowan AP, Rogers CA, Holt HA, Bowker KE. Activities of moxifloxacin against, and emergence of resistance in, Streptococcus pneumoniae and Pseudomonas aeruginosa in an in vitro pharmacokinetic model. Antimicrob Agents Chemother. 2003;47:1088–95.
Paterson DL. “Collateral damage” from cephalosporin or quinolone antibiotic therapy. Clin Infect Dis. 2004;38 Suppl 4:S341–5.
de Lastours V, Chau F, Roy C, Larroque B, Fantin B. Emergence of quinolone resistance in the microbiota of hospitalized patients treated or not with a fluoroquinolone. J Antimicrob Chemother. 2014;69:3393–400.
Fantin B, Duval X, Massias L, Alavoine L, Chau F, Retout S, et al. Ciprofloxacin dosage and emergence of resistance in human commensal bacteria. J Infect Dis. 2009;200:390–8.
Janoir C, Podglajen I, Kitzis MD, Poyart C, Gutmann L. In vitro exchange of fluoroquinolone resistance determinants between Streptococcus pneumoniae and Viridans streptococci and genomic organization of the parE-parC region in S-mitis. J Infect Dis. 1999;180:555–8.
Nicasio AM, Bulitta JB, Lodise TP, D’Hondt RE, Kulawy R, Louie A, et al. Evaluation of once-daily vancomycin against methicillin-resistant Staphylococcus aureus in a hollow-fiber infection model. Antimicrob Agents Chemother. 2012;56:682–6.
Lee DG, Murakami Y, Andes DR, Craig WA. Inoculum effects of ceftobiprole, daptomycin, linezolid, and vancomycin with Staphylococcus aureus and Streptococcus pneumoniae at inocula of 10(5) and 10(7) cfu injected into opposite thighs of neutropenic mice. Antimicrob Agents Chemother. 2013;57:1434–41.
Charles PGP, Ward PB, Johnson PDR, Howden BP, Grayson ML. Clinical features associated with bacteremia due to heterogeneous vancomycin-intermediate Staphylococcus aureus. Clin Infect Dis. 2004;38:448–51.
Sakoulas G, Gold HS, Cohen RA, Venkataraman L, Moellering RC, Eliopoulos GM. Effects of prolonged vancomycin administration on methicillin-resistant Staphylococcus aureus (MRSA) in a patient with recurrent bacteraemia. J Antimicrob Chemother. 2006;57:699–704.
Rosini JM, Laughner J, Levine BJ, Papas MA, Reinhardt JF, Jasani NB. A randomized trial of loading vancomycin in the emergency department. Ann Pharmacother. 2015;49:6–13.
Zelenitsky S, Alkurdi N, Weber Z, Ariano R, Zhanel G. Preferential emergence of reduced vancomycin susceptibility in health care-associated methicillin-resistant Staphylococcus aureus isolates during continuous-infusion vancomycin therapy in an in vitro dynamic model. Antimicrob Agents Chemother. 2011;55:3627–30.
Hanrahan T, Whitehouse T, Lipman J, Roberts JA. Vancomycin-associated nephrotoxicity: a meta-analysis of administration by continuous versus intermittent infusion. Int J Antimicrob Agents. 2015;46:249–53.
Hagihara M, Wiskirchen DE, Kuti JL, Nicolau DP. In Vitro Pharmacodynamics of Vancomycin and Cefazolin Alone and in Combination against Methicillin-Resistant Staphylococcus aureus. Antimicrob Agents Chemother. 2012;56:202–7.
Dilworth TJ, Leonard SN, Vilay AM, Mercier RC. Vancomycin and piperacillin-tazobactam against methicillin-resistant Staphylococcus aureus and vancomycin-intermediate Staphylococcus aureus in an in vitro pharmacokinetic/pharmacodynamic model. Clin Ther 2014;36:1334–44.
Climo MW, Patron RL, Archer GL. Combinations of vancomycin and beta-lactams are synergistic against staphylococci with reduced susceptibilities to vancomycin. Antimicrob Agents Chemother. 1999;43:1747–53.
Davis JS, Sud A, O’Sullivan MVN, Robinson JO, Ferguson PE, Foo H, et al. Combination of vancomycin and beta-lactam therapy for methicillin-resistant Staphylococcus aureus bacteremia: a pilot multicenter randomized controlled trial. Clin Infect Dis. 2016;62:173–80.
Boak LML, Rayner CR, Nation RL. Pharmacokinetic/Pharmacodynamic factors influencing emergence of resistance to linezolid in an in vitro model. Antimicrob Agents Chemother. 2007;51:1287–92.
Garcia MS, De la Torre MA, Morales G, Pelaez B, Tolon MJ, Domingo S, et al. Clinical outbreak of linezolid-resistant Staphylococcus aureus in an intensive care unit. JAMA. 2010;303:2260–4.
Roberts SM, Freeman AF, Harrington SM, Holland SM, Murray PR, Zelazny AM. Linezolid-resistant Staphylococcus aureus in two pediatric patients receiving low-dose linezolid therapy. Pediatr Infect Dis J. 2006;25:562–4.
Zoller M, Maier B, Hornuss C, Neugebauer C, Dobbeler G, Nagel D, et al. Variability of linezolid concentrations after standard dosing in critically ill patients: a prospective observational study. Crit Care. 2014;18:11.
Cattaneo D, Orlando G, Cozzi V, Cordier L, Baldelli S, Merli S, et al. Linezolid plasma concentrations and occurrence of drug-related haematological toxicity in patients with gram-positive infections. Int J Antimicrob Agents. 2013;41:586–9.
Pea F, Cojutti PG, Baraldo M. A 10-year experience of therapeutic drug monitoring (TDM) of linezolid in a hospital-wide population of patients receiving conventional dosing: is there enough evidence for suggesting TDM in the majority of patients? Basic Clin Pharmacol Toxicol. 2017;121:303–8.
Day T, Read AF. Does high-dose antimicrobial chemotherapy prevent the evolution of resistance? PLoS Comput Biol. 2016;12:20.
Yadav R, Bulitta JB, Nation RL, Landersdorfer CB. Optimization of synergistic combination regimens against carbapenem- and aminoglycoside-resistant clinical Pseudomonas aeruginosa isolates via mechanism-based pharmacokinetic/pharmacodynamic modeling. Antimicrob Agents Chemother. 2017. https://doi.org/10.1128/AAC.01011-16.
Yadav R, Landersdorfer CB, Nation RL, Boyce JD, Bulitta JB. Novel Approach To Optimize Synergistic Carbapenem-Aminoglycoside Combinations against Carbapenem-Resistant Acinetobacter baumannii. Antimicrob Agents Chemother. 2015;59:2286–98.
Drusano GL, Liu WG, Fregeau C, Kulawy R, Louie A. Differing effects of combination chemotherapy with meropenem and tobramycin on cell kill and suppression of resistance of wild-type Pseudomonas aeruginosa PAO1 and its isogenic MexAB efflux pump-overexpressed mutant. Antimicrob Agents Chemother. 2009;53:2266–73.
Sime FB, Johnson A, Whalley S, Santoyo-Castelazo A, Montgomery AB, Walters KA, et al. Pharmacodynamics of aerosolized fosfomycin and amikacin against resistant clinical isolates of Pseudomonas aeruginosa and Klebsiella pneumoniae in a hollow-fiber infection model: experimental basis for combination therapy. Antimicrob Agents Chemother. 2016. https://doi.org/10.1128/AAC.01763-16.
Burgess DS, Hastings RW. Activity of piperacillin/tazobactam in combination with amikacin, ciprofloxacin, and trovafloxacin against Pseudomonas aeruginosa by time-kill. Diagn Microbiol Infect Dis. 2000;38:37–41.
Chandrasekar PH, Crane LR, Bailey EJ. Comparison of the activity of antibiotic combinations in vitro with clinical outcome and resistance emergence in serious infection by Pseudomonas aeruginosa in non-neutropenic patients. J Antimicrob Chemother. 1987;19:321–9.
Bliziotis IA, Samonis G, Vardakas KZ, Chrysanthopoulou S, Falagas ME. Effect of aminoglycoside and beta-lactam combination therapy versus beta-lactam monotherapy on the emergence of antimicrobial resistance: a meta-analysis of randomized, controlled trials. Clin Infect Dis. 2005;41:149–58.
Ong DSY, van Werkhoven CH, Cremer OL, Thwaites GE, Bonten MJM. Is a randomized trial of a short course of aminoglycoside added to beta-lactam antibiotics for empirical treatment in critically ill patients with sepsis justified? Clin Microbiol Infect. 2017. https://doi.org/10.1016/j.cmi.2017.09.020.
Heffernan A, Lipman J, Roberts J. Is a randomized trial of a short course of aminoglycoside added to beta lactam antibiotics for empirical treatment in critically ill patients with sepsis justified? Clin Microbiol Infect. 2018. https://doi.org/10.1016/j.cmi.2017.12.019.
Dawis MA, Isenberg HD, France KA, Jenkins SG. In vitro activity of gatifloxacin alone and in combination with cefepime, meropenem, piperacillin and gentamicin against multidrug-resistant organisms. J Antimicrob Chemother. 2003;51:1203-–1.
Burgess DS, Nathisuwan S. Cefepime, piperacillin/tazobactam, gentamicin, ciprofloxacin, and levofloxacin alone and in combination against Pseudomonas aeruginosa. Diagn Microbiol Infect Dis. 2002;44:35–41.
Kohanski MA, DePristo MA, Collins JJ. Sublethal Antibiotic Treatment Leads to Multidrug Resistance via Radical-Induced Mutagenesis. Molecular Cell. 2010;37:311–20.
Wener KM, Schechner V, Gold HS, Wright SB, Carmeli Y. Treatment with fluoroquinolones or with beta-lactam-beta-lactamase inhibitor combinations is a risk factor for isolation of extended-spectrum-beta-lactamase-producing Klebsiella Species in hospitalized patients. Antimicrob Agents Chemother. 2010;54:2010–6.
Cassier P, Lallechere S, Aho S, Astruc K, Neuwirth C, Piroth L, et al. Cephalosporin and fluoroquinolone combinations are highly associated with CTX-M beta-lactamase-producing Escherichia coli: a case–control study in a French teaching hospital. Clin Microbiol Infect. 2011;17:1746–51.
Goldstein RC, Husk G, Jodlowski T, Mildvan D, Perlman DC, Ruhe JJ. Fluoroquinolone- and ceftriaxone-based therapy of community-acquired pneumonia in hospitalized patients: The risk of subsequent isolation of multidrug-resistant organisms. Am J Infect Control. 2014;42:539–41.
Li J, Rayner CR, Nation RL, Owen RJ, Spelman D, Tan KE, et al. Heteroresistance to colistin in multidrug-resistant Acinetobacter baumannii. Antimicrob Agents Chemother. 2006;50:2946–50.
Lenhard JR, Gall JS, Bulitta JB, Thamlikitkul V, Landersdorfer CB, Forrest A, et al. Comparative pharmacodynamics of four different carbapenems in combination with polymyxin B against carbapenem-resistant Acinetobacter baumannii. Int J Antimicrob Agents. 2016;48:719–24.
Bergen PJ, Forrest A, Bulitta JB, Tsuji BT, Sidjabat HE, Paterson DL, et al. Clinically Relevant Plasma Concentrations of Colistin in Combination with Imipenem Enhance Pharmacodynamic Activity against Multidrug-Resistant Pseudomonas aeruginosa at Multiple Inocula. Antimicrob Agents Chemother. 2011;55:5134–42.
Ly NS, Bulman ZP, Bulitta JB, Baron C, Rao GG, Holden PN, et al. Optimization of Polymyxin B in Combination with Doripenem To Combat Mutator Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2016;60:2870–80.
Rigatto MH, Vieira FJ, Antochevis LC, Behle TF, Lopes NT, Zavascki AP. Polymyxin B in Combination with Antimicrobials Lacking In Vitro Activity versus Polymyxin B in Monotherapy in Critically Ill Patients with Acinetobacter baumannii or Pseudomonas aeruginosa Infections. Antimicrob Agents Chemother. 2015;59:6575–80.
Cai XJ, Yang Z, Dai JQ, Chen K, Zhang LD, Ni WT, et al. Pharmacodynamics of tigecycline alone and in combination with colistin against clinical isolates of multidrug-resistant Acinetobacter baumannii in an in vitro pharmacodynamic model. Int J Antimicrob Agents. 2017;49:609–16.
Diep JK, Sharma R, Ellis-Grosse EJ, Abboud CS, Rao GG. Polymyxin B and ZTI-01 (fosfomycin for injection) against KPC-producing Klebsiella pneumoniae: evaluation of activity and emergence of resistance. Antimicrob Agents Chemother. 2017. https://doi.org/10.1128/AAC.01815-17.
Walsh CC, Landersdorfer CB, McIntosh MP, Peleg AY, Hirsch EB, Kirkpatrick CM, et al. Clinically relevant concentrations of fosfomycin combined with polymyxin B, tobramycin or ciprofloxacin enhance bacterial killing of Pseudomonas aeruginosa, but do not suppress the emergence of fosfomycin resistance. J Antimicrob Chemother. 2016;71:2218–29.
Rao GG, Ly NS, Bulitta JB, Soon RL, San Roman MD, Holden PN, et al. Polymyxin B in combination with doripenem against heteroresistant Acinetobacter baumannii: pharmacodynamics of new dosing strategies. J Antimicrob Chemother. 2016;71:3148-–56.
Rao GG, Ly NS, Diep J, Forrest A, Bulitta JB, Holden PN, et al. Combinatorial pharmacodynamics of polymyxin B and tigecycline against heteroresistant Acinetobacter baumannii. Int J Antimicrob Agents. 2016;48:331–6.
Entenza JM, Giddey M, Vouillamoz J, Moreillon P. In vitro prevention of the emergence of daptomycin resistance in Staphylococcus aureus and enterococci following combination with amoxicillin/clavulanic acid or ampicillin. Int J Antimicrob Agents. 2010;35:451–6.
Schrag SJ, Pena C, Fernandez J, Sanchez J, Gomez V, Perez E, et al. Effect of short-course, high-dose amoxicillin therapy on resistant pneumococcal carriage: a randomized trial. JAMA. 2001;286:49–56.
Guillemot D, Carbon C, Balkau B, Geslin P, Lecoeur H, Vauzelle-Kervroedan F, et al. Low dosage and long treatment duration of beta-lactam—risk factors for carriage of penicillin-resistant Streptococcus pneumoniae. JAMA. 1998;279:365–70.
Ruhe JJ, Hasbun R. Streptococcus pneumoniae bacteremia: duration of previous antibiotic use and association with penicillin resistance. Clin Infect Dis. 2003;36:1132-–8.
Hillier S, Roberts Z, Dunstan F, Butler C, Howard A, Palmer S. Prior antibiotics and risk of antibiotic-resistant community-acquired urinary tract infection: a case-control study. J Antimicrob Chemother. 2007;60:92–9.
Chastre J, Wolff M, Fagon JY, Chevret S, Thomas F, Wermert D, et al. Comparison of 8 vs 15 days of antibiotic therapy for ventilator-associated pneumonia in adults: a randomized trial. JAMA. 2003;290:2588–98.
Yusuf E, Van Herendael B, Verbrugghe W, Ieven M, Goovaerts E, Bergs K, et al. Emergence of antimicrobial resistance to Pseudomonas aeruginosa in the intensive care unit: association with the duration of antibiotic exposure and mode of administration. Ann Intensive Care. 2017. https://doi.org/10.1186/s13613-017-0296-z.
Sawyer RG, Claridge JA, Nathens AB, Rotstein OD, Duane TM, Evans HL, et al. Trial of Short-Course Antimicrobial Therapy for Intraabdominal Infection. N Engl J Med. 2015;372:1996–2005.
Lee DS, Ryu JA, Chung CR, Yang J, Jeon K, Suh GY, et al. Risk factors for acquisition of multidrug-resistant bacteria in patients with anastomotic leakage after colorectal cancer surgery. Int J Colorectal Dis. 2015;30:497–504.
Pierrakos C, Vincent JL. Sepsis biomarkers: a review. Crit Care. 2010. https://doi.org/10.1186/cc8872.
Sandquist M, Wong HR. Biomarkers of sepsis and their potential value in diagnosis, prognosis and treatment. Exp Rev Clin Immunol. 2014;10:1349–56.
Dupuy A-M, Philippart F, Péan Y, Lasocki S, Charles P-E, Chalumeau M, et al. Role of biomarkers in the management of antibiotic therapy: an expert panel review: I – currently available biomarkers for clinical use in acute infections. Ann Intensive Care. 2013;3:1–8.
Wacker C, Prkno A, Brunkhorst FM, Schlattmann P. Procalcitonin as a diagnostic marker for sepsis: a systematic review and meta-analysis. Lancet Infect Dis. 2013;13:426–35.
Uzzan B, Cohen R, Nicolas P, Cucherat M, Perret GY. Procalcitonin as a diagnostic test for sepsis in critically ill adults and after surgery or trauma: a systematic review and meta-analysis. Crit Care Med. 2006;34:1996–2003.
Tang BMP, Eslick GD, Craig JC, McLean AS. Accuracy of procalcitonin for sepsis diagnosis in critically ill patients: systematic review and meta-analysis. Lancet Infect Dis. 2007;7:210–7.
van der Does Y, Rood PPM, Haagsma JA, Patka P, van Gorp ECM, Limper M. Procalcitonin-guided therapy for the initiation of antibiotics in the ED: a systematic review. Am J Emerg Med. 2016;34:1286–93.
Costelloe C, Metcalfe C, Lovering A, Mant D, Hay AD. Effect of antibiotic prescribing in primary care on antimicrobial resistance in individual patients: systematic review and meta-analysis. BMJ. 2010. https://doi.org/10.1136/bmj.c2096.
Goossens H, Ferech M, Stichele RV, Elseviers M, Grp EP. Outpatient antibiotic use in Europe and association with resistance: a cross-national database study. Lancet. 2005;365:579–87.
de Jong E, van Oers JA, Beishuizen A, Vos P, Vermeijden WJ, Haas LE, et al. Efficacy and safety of procalcitonin guidance in reducing the duration of antibiotic treatment in critically ill patients: a randomised, controlled, open-label trial. Lancet Infect Dis. 2016;16:819–27.
Kopterides P. Procalcitonin-guided algorithms of antibiotic therapy in the intensive care unit: a systematic review and meta-analysis of randomized controlled trials. Crit Care Med. 2010;38:2229–41.
Prkno A, Wacker C, Brunkhorst FM, Schlattmann P. Procalcitonin-guided therapy in intensive care unit patients with severe sepsis and septic shock—a systematic review and meta-analysis. Crit Care. 2013. https://doi.org/10.1186/cc13157.
Schuetz P, Chiappa V, Briel M, Greenwald JL. Procalcitonin algorithms for antibiotic therapy decisions: a systematic review of randomized controlled trials and recommendations for clinical algorithms. Arch Intern Med. 2011;171:1322–31.
Schuetz P, Müller B, Christ-Crain M, Stolz D, Tamm M, Bouadma L, et al. Procalcitonin to initiate or discontinue antibiotics in acute respiratory tract infections. Cochrane Database Syst Rev. 2012;10:CD007498.
Nora D, Salluh J, Martin-Loeches I, Póvoa P. Biomarker-guided antibiotic therapy—strengths and limitations. Ann Transl Med. 2017. https://doi.org/10.21037/atm.2017.04.04.
Simon L, Gauvin F, Amre DK, Saint-Louis P, Lacroix J. Serum procalcitonin and C-reactive protein levels as markers of bacterial infection: a systematic review and meta-analysis. Clin Infec Dis. 2004;39:206–17.
Lobo SM, Lobo FR, Bota DP, Lopes-Ferreira F, Soliman HM, Melot C, et al. C-reactive protein levels correlate with mortality and organ failure in critically ill patients. Chest. 2003;123:2043–9.
Oliveira CF, Botoni FA, Oliveira CR, Silva CB, Pereira HA, Serufo JC, et al. Procalcitonin versus C-reactive protein for guiding antibiotic therapy in sepsis: a randomized trial. Crit Care Med. 2013;41:2336–43.
Acknowledgements
Aaron Heffernan would like to acknowledge funding from a Griffith School of Medicine Research Higher degree scholarship. Fekade Sime would like to acknowledge funding from a University of Queensland Post Doctoral Fellowship. Jason Roberts would like to recognise funding from the Australian National Health and Medical Research Council for a Centre of Research Excellence (APP1099452) and a Practitioner Fellowship (APP1117065).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Jason Roberts would like to declare collaborations with MSD, Bayer, Astellas, Pfizer, bioMerieux and Accelerate Diagnostics but none of which are considered relevant to the content of this paper. Aaron Heffernan, Fekade Sime and Jeffrey Lipman have no conflicts of interest to declare.
Rights and permissions
About this article
Cite this article
Heffernan, A.J., Sime, F.B., Lipman, J. et al. Individualising Therapy to Minimize Bacterial Multidrug Resistance. Drugs 78, 621–641 (2018). https://doi.org/10.1007/s40265-018-0891-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-018-0891-9