Abstract
The respective driving abilities of three patients having a right hemisphere infarct and mild unilateral spatial neglect (USN) were examined. Neuropsychological examinations included the Behavioral Inattention Test Japanese version (BIT-J) and the Japanese version of the Wechsler Adults Intelligence Scale – Third edition. Their driving ability was assessed with a driving simulator test and on-road evaluation. Patients had no neglect based on the BIT-J, but showed some slight signs of USN on a driving simulator test and on-road evaluation. This study assessed risks of mild USN patient driving and explored possibilities of improving it using Advanced Driving Assistance Systems.
You have full access to this open access chapter, Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
For many people, driving is an important activity of daily living. Previous reports have described that 30 %–66 % of stroke patients resume driving [1, 2]. Resuming car driving is an important concern for many stroke survivors and their families. Nevertheless, driving a car, a complex task, requires the integration of visual-perceptual stimuli, good judgment, decision making, and appropriate motor responses. These functional abilities might be affected by stroke, traumatic brain injury and other brain disorders. Above all, the unilateral spatial neglect (USN) is an extraordinary clinical phenomenon whereby patients appear to be unable to respond to objects and people located on the contralateral side to a cerebral lesion. It is one of many manifestations that can occur in people in the aftermath of a stroke. The incidence of USN has been reported to be as high as 82 % in right hemispheric stroke patients when assessed in the acute stage [3]. Although USN can be associated with damage to left or right hemispheres of the brain, it occurs more frequently and with greater severity following damage to the right hemisphere. The USN severity can vary from mild to severe. Mild USN has been assessed in several earlier studies.
Clinically, moderate or severe USN is regarded as severely affecting activities of daily living (ADL; Fig. 1, e.g., they frequently collide into surroundings during walking or wheelchair driving, ignore food on one side of the plate, and attend to only one side of the body). Therefore, moderate or severe USN is likely to pose a daunting obstacle to driving. However, the evaluation of driving ability in patients with mild USN is a multi-faceted matter that clinicians often encounter in their work. This report presents assessed driving ability and considers the possibility of advanced driver-assistance systems facilitating patients’ resumption of safe driving.
2 Patients and Methods
Three patients were selected from a larger group of recovering stroke patients who had been referred for specialized driving ability evaluation. All were patients affected by visual neglect without hemianopia in the acute phase because of a right hemisphere infarction. In all three cases, the acute neurological diagnosis was supported by computerized tomography of the brain. None had any prior neurological disorder. All the patients possessed a valid driving license immediately before their stroke. Then they were active, non-professional drivers.
3 Methods
Some neuropsychological examination and the Driving-simulator test were performed for each patient before the on-road driving assessment. Detailed results are reported for the Behavioral Inattention Test Japanese version (BIT-J; Fig. 2) and the Japanese version of the Wechsler Adults Intelligence Scale third edition (JWAIS-3rd; Fig. 3). These tests are used widely in Japan.
BIT-J is a representative screening battery of tests used to assess the presence of USN. BIT is divided into two subtests. The Conventional subtest consists of six items. Its Cut-Off score is 131. The Behavioral Subtest consists of nine items. Its Cut-Off score is 68. The Conventional subtest is paper-and-pencil based. If the patient’s BIT-J score is less than the Cut-Off Score, then it is regarded as indicating the presence of USN. The inclusion criterion of this study was normal performance (score >131) on the BIT at the time of Driving evaluation, which indicated the recovery of USN. Actually, BIT takes about 40 min to administer, including the test instructions.
Clinically, JWAIS-3rd is a useful test for measuring intelligence in adults and older adolescents. It provided scores for Verbal IQ, Performance IQ, and Full Scale IQ, along with four secondary indices (Verbal comprehension, Working memory, Perceptual organization, and Processing speed). Particularly according to previous studies, Processing Speed (PS) is lower for elderly drivers who have had accidents. JWAIS-3rd takes about 3 h to administer, including the test instructions.
In the Driving-simulator test, the subject’s task is Lane Tracking. Subjects must maintain the course continuously during driving on a road with random curves. The ratio of straying from the course is measured and calculated as the “error ratio.” The Driving-simulator test takes about 10 min to administer, including the test instructions. The simulator has high precision (Fig. 4, DS-20; Mitsubishi Inc.).
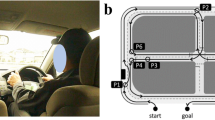
The on-road driving assessment was conducted after the neuropsychological examination and the Driving-simulator test were administered by a licensed driving instructor, who was not informed of the results of the neurological or neuropsychological examinations. The one-hour driving test took place during the daytime on a closed course at a driving school.
The main domains assessed in the driving instructor’s evaluation in the on-road driving test are presented in connection with the case descriptions.
4 Results
Three patients possessed a valid driving license immediately before experiencing a stroke. All the patients had a statutory duty to undergo the Extraordinary Aptitude Test after recovering from the stroke.
4.1 Case 1
The patient was a right-handed man in his 30s who had undergone right putamen hemorrhage (Fig. 5-A). In the acute phase, the man had severe hemiparesis and moderate USN. Two and a half months after onset, he had no hemiparesis. No sign of neglect was detected by the BIT-J (Conventional subtest 145/146, Behavioral subtest 79/81).
His ADL and gait were independent: without assistance. Nevertheless, the man had hit obstacles in the left hemispace and showed low processing speed (PS of 86 by WAIS-3rd). In the Driving simulator test, his “error ratio” was biased strongly toward the left side (Fig. 6-A).
In the Driving evaluation, during a closed course test, the man showed left-sided visual inattention and poor lane position (e.g., the man’s car was stopped too close to traffic while overtaking stopped traffic. The man’s car was spaced too widely on the left side. He scraped the right rear while parking left and rearward.) (Fig. 7-A). The man’s comments showed poor self-awareness of his driving performance (e.g., “It was not too bad.”). From these results, we inferred that the man would have difficulty resuming safe driving. At a later re-evaluation (7 months later), the man’s PS and self-awareness had improved (e.g., His PS was 102 by WAIS-3rd. He commented “I must drive carefully because I was terrible at driving.”). He was conscious that his vehicle was too close to stopped traffic. He resumed car driving because he had become capable of safe driving. Subsequently, this man has had no accident for two years.
4.2 Case 2
The patient was a right-handed man in his 50s with right putamen hemorrhage (Fig. 5-B). In the early recovery phase, the man hit obstacles on his left side when using his wheelchair. However, in the chronic recovery phase, no sign of neglect was detected according to the Behavioral Inattention Test – Japanese version (BIT-J: Conventional subtest 133/146, Behavioral subtest 74/81). Furthermore, his ADL and gait were independent.
In the Driving simulator test, his “error ratio” was strongly biased toward the left side, as in Case 1 (Fig. 6-B).
During the Driving evaluation, the man showed left-sided visual inattention and poor lane position (e.g., The man’s car scraped the left side while parking left and rearward. Overall, the man’s car showed a tendency for exceeding speed limits.) (Fig. 7-B). The man’s subsequent comments demonstrated poor awareness of his personal driving performance (e.g., “It was nice to be able to drive.”).
We inferred that the man would have difficulty resuming safe driving. At re-evaluation (9 months later), the man’s BIT-J score had improved (BIT-J: Conventional subtest 141/146, Behavioral subtest 81/81). In a closed course test, he was unable to continue modifying his own behavior after he was cautioned. His comments still showed poor self-awareness (“How slowly this car is moving!!”). We inferred that the man would have difficulty resuming safe driving because he was not able to reflect upon and modify his own driving performance. He has not resumed car driving following our recommendation to stop driving.
4.3 Case 3
The patient was a right-handed woman in her 50s with right putamen hemorrhage (Fig. 5-C). In the recovery phase, the woman hit obstacles on her left side when using a wheelchair. Furthermore, in the chronic phase, she hit obstacles on her left side during walking. However, no sign of neglect was detected according to BIT-J (Conventional subtest 142/146, Behavioral subtest 78/81).
In the Driving simulator test, her “error ratio” was biased strongly toward the left side, similarly to Cases 1 and 2 (Fig. 6-C).
In Driving evaluation, the woman showed left-sided visual inattention and poor lane position (e.g., The woman’s car ran off to the left side while running an S-curve course. The woman’s car ran the wrong way on right lane in left-hand traffic following running on an L-curve course.) (Fig. 7-C). Overall, the speed was too slow. The woman’s comments included reports of poor self-awareness of her driving performance (e.g., “I feel quite safe when driving slowly.”). We inferred that the woman would have difficulty resuming safe driving. She has not resumed car driving.
5 Discussion
This study presented three patients who were affected of mild USN on driving. All patients had USN between acute phase and recovery phase. At the time of neuropsychological test, the patients had no signs of USN according to the BIT-J. However, they showed signs of USN in the Driving simulator test and Driving evaluation. In fact, mild USN might impair safe driving by causing difficulties in maintaining driving lines and optimum speed, or by narrowing and slowing the perception of the whole environment.
One interesting finding was that of a non-detectable type of USN using BIT-J, as mild USN. According to several previous studies, BIT-J were shown to be reliable and valid in patients with moderate or severe USN [5, 6]. Conversely, BIT-J has insufficient reliability and validity for patients with mild USN. For example, mild USN patients might learn to compensate by voluntarily directing their attention to the contralateral side of the lesion. Furthermore, mild USN patients might compensate by looking carefully again because BIT-J is a paper–pencil based test.
In addition, some reports of previous studies have described subtypes of USN [7, 8]. Regarding specific details, they might include personal neglect (inability to attend to either side of the person’s body), peripersonal neglect (inability to attend to either side of the space within reaching distance), extrapersonal neglect (inability to attend to either side of the space beyond reaching distance). From a cognitive perspective, BIT-J corresponds to peripersonal neglect test because BIT-J is a desk test. Problems of peripersonal and extrapersonal space might be related to car driving.
Moreover, in this study, a non-detectable type of USN using BIT-J might be obvious only under certain circumstances as On Road Driving and using Driving Simulator. Taylor has pointed out that mild USN patients might show signs of USN in complex visual tasks but not in simple tasks [9]. This indication is in line with our findings that mild visual neglect patients might be affected by processing speed and complex tasks.
In this study, patients with poor self-awareness were unable to reflect and modify the driving performance. Ishiai pointed out that USN is linked inextricably to poor self-awareness [7]. Self-awareness is virtually synonymous with metacognition. In addition to problems of mild USN, a patient’s poor self-awareness might influence resuming car driving.
In recent years, Advanced Driving Assistance Systems (ADAS) are rapidly developing: field and assistance systems of various types are developed. Particularly, ADAS might improve USN patients’ driving performance. In this instantiation, ADAS (e.g., lane-keeping assist system, collision avoidance system, parking assist system) might decrease driving risks and assist the safe driving of USN patients.
6 Conclusion
USN patients’ driving performance might reveal problems of one sided visual attention and show a lack of self-awareness of their driving performance. For their resumption of safe driving in addition to providing rehabilitation training, it is necessary to compensate for their deficits using ADAS.
References
Fisk, G.D., Owsley, C., Pulley, L.V.: Driving after stroke: driving exposure, advice, and evaluations. Arch. Phys. Med. Rehabil. 78, 1338–1345 (1997)
Heikkilä, V.M., Korpelainen, J., Turkka, J., Kallanranta, T., Summala, H.: Clinical evaluation of the driving ability in stroke patients. Acta Neurol. Scand. 99, 349–355 (1999)
Stone, S.P., Halligan, P.W., Greenwood, R.J.: The incidence of neglect phenomena and related disorders in patients with an acute right or left hemisphere stroke. Age Ageing 22, 46–52 (1993)
Labo-Information, Tokyo Metropolitan University Liaison Office. http://www.tokyo-sangaku.jp/labo/%E7%B6%B2%E6%9C%AC-%E5%92%8C/
Halligan, P.W., Cockburn, J., Wilson, B.A.: The behavioural assessment of visual neglect. Neuropsychol. Rehabil. 1, 5–32 (1991)
Hannaford, S., Gower, G., Potter, J.M., Guest, R.M., Fairhurst, M.C.: Assessing visual inattention: study of interrater reliability. Brit. J. Ther. Rehabil. 10, 72–75 (2003)
Ishiai, S.: Behavioral Inattention Test Japanese Version. Sinko Igaku Syuppan, Japan (1999)
Mizuno, K.: Rehabilitation of unilateral spatial neglect. Medical Rehabilitation. MB Med Rehab, ZEN·NIHONBYOUIN·SYUPPANKAI, vol. 129 (2011)
Taylor, D.: Measuring mild visual neglect: do complex visual tests activate rightward attentional bias? N. Z. J. Physiotherapy 31, 67–72 (2003)
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this paper
Cite this paper
Sotokawa, T., Murayama, T., Noguchi, J., Sakimura, Y., Itoh, M. (2015). Driving Evaluation of Mild Unilateral Spatial Neglect Patients–Three High-Risk Cases Undetected by BIT After Recovery. In: Yamamoto, S. (eds) Human Interface and the Management of Information. Information and Knowledge in Context. HIMI 2015. Lecture Notes in Computer Science(), vol 9173. Springer, Cham. https://doi.org/10.1007/978-3-319-20618-9_25
Download citation
DOI: https://doi.org/10.1007/978-3-319-20618-9_25
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-20617-2
Online ISBN: 978-3-319-20618-9
eBook Packages: Computer ScienceComputer Science (R0)