Abstract
Upper respiratory tract infections (URTIs) are responsible for a large amount of community antibacterial use worldwide. Recent systematic reviews have demonstrated that most URTIs resolve naturally, even when bacteria are the cause. The high consumer expectation for antibacterials in URTIs requires intervention by the general practitioner and a number of useful strategies have been developed.
Generic strategies, including eliciting patient expectations, avoiding the term ‘just a virus’, providing a value-for-money consultation, providing verbal and written information, empowering patients, conditional prescribing, directed education campaigns, and emphasis on symptomatic treatments, should be used as well as discussion of alternative medicines when relevant.
The various conditions have differing rates of bacterial infection and require different approaches. For acute rhinitis, laryngitis and tracheitis, viruses are the only cause and, therefore, antibacterials are never required. In acute sore throat (pharyngitis) Streptococcus pyogenes is the only important bacterial cause. A scoring system can help to increase the likelihood of distinguishing a streptococcal as opposed to viral infection, or alternatively patients should be given antibacterials only if certain conditions are fulfilled. Strategies for treating acute otitis media vary in different countries. Most favour the strategy of prescribing antibacterials only when certain criteria are fulfilled, delaying antibacterial prescribing for at least 24 hours. In otitis media with effusion, on the other hand, there is no primary role for antibacterials, as the condition resolves naturally in almost all patients aged >3 months. Detailed strategies for acute sinusitis have not been worked out but restricting antibacterial prescribing to certain clinical complexes is currently recommended by several authorities because of the high natural resolution rate.
Similar content being viewed by others
Respiratory tract infections are the most common reasons for prescribing antibacterial agents in developed countries, representing about 75% of all prescriptions in community practice. Of these, upper respiratory tract infections (URTIs) constitute more than half of all general practice attendances, and it is common for antibacterials to be prescribed for 50% or more of these.[1,2] Furthermore, there has been a trend in some countries to the use of broader spectrum and more expensive agents.[3] As viruses are the most frequent cause of URTIs, high levels of antibacterial prescribing for URTIs suggest that there is considerable unnecessary prescribing.
Resistance to antibacterials has recently been targeted by the World Health Organization for major international action,[4] and reducing unnecessary prescribing is an essential component of this strategy. Tackling prescribing/consuming for respiratory tract infection is likely to lead to the greatest reduction. Given that resistance to antibacterials in the common bacterial respiratory pathogens, especially Streptococcus pneumoniae, is increasing worldwide,[5] it is time to critically review prescribing practices in patients with URTI and find methods for not prescribing antibacterials to patients who are unlikely to benefit.[6]
1. Natural Resolution of Upper Respiratory Tract Infections (URTIs)
The most important feature of URTIs is that most resolve naturally and rapidly, whether the infection is viral or bacterial. It cannot be stressed enough that even bacterial URTIs have a high rate of spontaneous resolution. This has two important implications: antibacterials will help only a small proportion of patients, even when the infection is known to be bacterial, and levels of resistance must be very high before there will be a noticeable effect on outcomes.[7] This explains the apparently paradoxical recommendations by many authorities that the antibacterial of choice − when required − is a narrow spectrum drug, even if resistant bacteria are known to be common.
Estimated natural resolution rates without complications are as follows: acute otitis media 81 to 86%;[8] streptococcal pharyngitis >90%;[9] and acute sinusitis about 69%.[10]
2. Generic Interventions
Because of high natural resolution rates, the default position for the treatment of URTIs is not to prescribe an antibacterial. This is not the expectation of many patients who present to the general practitioner. Indeed, many patients visit their doctor only because they or a relative believe they need an antibacterial, and in most developed countries antibacterials are not available over the counter. However, the combination of ‘routine’ antibacterial prescribing and belief that the patient expects to be prescribed an antibacterial has created a positive feedback loop whereby the prescriber may feel reluctant to discuss not using antibacterials with many patients. This feedback loop must be broken, and it requires the application of a general practitioner’s professional integrity to take this step with each new consultation.
The most important reason for inappropriate prescribing is fear of losing the patient’s confidence. If the doctor has prescribed unnecessary antibacterials for the patient in the past for the same condition, it takes courage and finesse to tackle the patient with the ‘new’ idea that antibacterials are not needed. Some general suggestions about how this might be done follow.
Make expectations explicit: A recent study of patients presenting with sore throats has shown that patients’ expectations are not usually explicit.[11] To make matters worse, doctors’ ideas about what the patient expects are often incorrect for the simple reason that they make an assumption and do not expressly ask what the patient expected. A direct question to the patient will determine what the patient expects and whether they really expect to be given an antibacterial. If the patient does not expect an antibacterial and you do not feel they require one, the consultation can conclude to everyone’s satisfaction. If the patient expects an antibacterial and you believe they do not need one, you have an opportunity to discuss with them why they don’t need one. Even if they insist, you have sown the seed of doubt for their next URTI.
Avoid the term ‘just a virus’: The term ‘just a virus’ is widespread in community practice. When this term is used medically it implies that the infection resolves relatively quickly and without complications. However, in the lay mind the term is often interpreted as ‘this is a trivial infection; why did you bother to consult me?’. As anyone knows who has had a ‘streaming head cold’ or influenza, viral infections can be quite debilitating. A sympathetic tone and an expression that viruses are just as troublesome as bacteria will make all the difference.
Provide value for money: Another finding from the sore throat study[11] was the importance placed by the patient on the doctor taking an active interest in their problem and giving them ‘value for money’. Value for money means different things to different people, but simple ingredients such as time, sympathy, being taken seriously and physical examination can make a significant difference.
Provide verbal information: Each consultation is an opportunity for education. If the practitioner knows that the information they will be giving will be new, the opportunity should not be squandered. In this context, it is better to give information that is personalised (‘we know now that antibiotics will not help you’) than to quote from studies and meta-analyses and systematic reviews. One part of achieving this personalisation is to emphasise the personal risks of taking antibacterials: adverse reactions such as rash, and the risk of becoming colonised with a resistant bacterium that will be harder to treat when they really do need antibacterials. The practitioner may choose to stress the effect on normal flora in terms of thrush (candidiasis), diarrhoea and selection of a resistant strain or creating a vacuum for a resistant strain to be picked up from someone else.
Of course, the practitioner must tailor the information to the education and skill level of the individual patient. Some patients respond also to the ‘green’ message: that unnecessary antibacterials breed resistant bacteria (which are genetically modified organisms!) which can harm them or which they can spread to others, i.e. they are bad for public health and the planet.
Provide written information: A number of brochures are available which provide information about the usefulness of antibacterials or on the management of specific conditions. Fact sheets on common infections can be found on the US Centers for Disease Control and Prevention website (http://www.cdc.gov). A number of useful information sheets directed at certain URTIs are available on the worldwide web. These are listed in table I. You may choose to develop your own handouts.
Empower patients: There is considerable scope for empowering patients in the decision-making and therapeutic process. The current popularity of alternative medicines attests to the fact that patients are seeking more control over their illnesses. Emphasising the positive effects of symptomatic treatments and providing more detailed prescriptions of how these could be used, as well as the value of antibacterials only when they are really necessary, can give the patient some sense of control. One method of achieving this is to write a ‘symptomatic prescription’ that contains instructions and useful information about the various symptom remedies; this offers the benefits of ‘value for money’ and ‘written information’ in the guise of a true script. An example can be found on the Australian National Prescribing Service website (http://www.nps.org.au).
Consider conditional or deferred prescribing: A useful technique for patients who have a sustained belief in the need for antibacterials when they are not needed is conditional prescribing. This means writing a prescription and suggesting to the patient that they have it filled only if certain conditions develop, the most common being ‘worse the next day’ or ‘no better after 2 days’ (these are fairly lenient conditions). One sore throat study in the UK used this technique as 1 of 3 arms of a prospective study and showed that more that two-thirds of patients did not have their script filled.[12] Another study, in patients with otitis media, combined this strategy with a patient/parent handout and showed a significant reduction in prescribing compared with a control general practice.[13]
Directed campaign: Simple but deliberate education campaigns can be effective.[14] One general practice study was able to show that simultaneous education of the prescribers in their practice, and their patients, led to a significant drop in the number of prescriptions (table II). Patient information was provided through a poster in the waiting rooms, at the time of consultation and by a generic brochure handed to patients who did not require antibacterials for their respiratory tract infection.
Reduction in prescriptions after educational intervention (adapted from Rogers & Light[14])
Alternative medicines: Herbal and other over-the-counter remedies have become popular in recent years and many are advocated by the manufacturers for the treatment of infections. In particular, echinacea, in various forms, has received some scientific scrutiny and has been the subject of systematic review in URTIs.[15,16] There is some evidence to suggest that echinacea reduces the duration of symptoms in URTIs, but insufficient to recommend which product or preparation may be best, as several studies have used multiple actives (i.e. that include echinacea along with other ‘active’ agents). There is evidence that echinacea is ineffective as prophylaxis for rhinovirus infections.[17] Sharing this information with patients who are interested in alternative medicines may assist the patient with positive alternatives to antibacterial therapy.
3. URTI Syndromes
3.1 Undifferentiated URTI
Undifferentiated URTI is the most common category of URTI presenting to general practitioners. This diagnosis is often made when symptoms suggest one or more of the URTI-specific syndromes, but are sufficiently indistinct on history and examination to make a diagnosis. It is clear that this condition is viral and there is no indication for either microbiological investigations or antimicrobial treatment. The prescription for this condition is obviously symptomatic relief: whatever you think will most appeal to the patient. More importantly, follow-up of worsening symptoms will usually lead to a syndromic diagnosis.
3.2 Acute Rhinitis (Common Cold)
3.2.1 Clinical Points
Acute rhinitis, ‘head cold’ or the common cold, although more common in winter, is prevalent all year round and only a small proportion of patients seek medical help. They often do so as parents of children with purulent rhinitis, a very common problem in the young child.[18] It is usually in the context of clear nasal discharge becoming purulent that medical help is sought, either with children, or with adults who assume that purulent discharge is a sign of sinusitis and that sinusitis must be treated with antibacterials. Antibacterial prescribing is common for this condition[1,18] but is almost never required.
3.2.2 Pathogens
All acute rhinitis is viral, even with purulent discharge. Rhinoviruses are the most frequent, followed by coronaviruses and influenza viruses.
3.2.3 Investigations
Culture of purulent nasal discharges often reveals what seem to be significant pathogens such as S. pneumoniae, Haemophilus influenzae or Staphylococcus aureus. However, these are opportunistic colonisers and should be ignored. There are no useful routine microbiological investigations for acute rhinitis.
3.2.4 Issues
Because purulent rhinitis suggests a component of bacterial overgrowth contributing to the illness, there have been 9 placebo-controlled trials of antibacterials, conducted in URTI, to both treat and prevent purulent rhinitis.[19] None of these studies has demonstrated a benefit for antibacterials either as treatment or to prevent rhinitis becoming purulent.
3.2.5 Treatment
Medications to control secretions are all that is required. Antibacterials should never be prescribed unless the diagnosis is considered to be acute sinusitis, and then only when certain conditions are fulfilled (see section 3.6).
Topical or oral decongestants are the most widely used, and many topical agents are available over the counter. Single doses have been shown to be quite effective in short term relief of symptoms but repeated use over days shows little extra benefit.[20] Nasal decongestants are not without their problems, and alternatives such as saline nasal sprays are recommended by some to prevent the rebound congestion associated with decongestant medications. Steam inhalations, although still widely used, are probably of no greater benefit than saline nasal spray, both achieving the same aim of thinning secretions to facilitate their clearance. If decongestants are prescribed or recommended, their use should be restricted to 5 days or less to reduce the risk of rebound congestion.
Zinc and high dose ascorbic acid (vitamin C) have also been examined critically in systematic reviews. Whereas zinc shows no benefit and runs the risk of producing adverse effects,[21] trials have shown that high dose ascorbic acid can reduce the duration of symptom days by 8 to 9%.[22]
3.3 Sore Throat (Acute Pharyngitis)
3.3.1 Clinical Points
The second most common general practice presentation after undifferentiated URTI is sore throat. Usually the patient presents because symptoms are sufficiently severe to affect eating and swallowing. If the sore throat is accompanied by rhinitis or cough, it is highly likely that the infection is viral. It is important to exclude Epstein-Barr virus infection in the appropriate age group. This virus tends to cause the most severe sore throats. It can be suspected when patients have lymphadenopathy apart from in the anterior cervical area, namely posterior cervical, axillary and inguinal, plus splenomegaly.
3.3.2 Pathogens
Viruses are the most common cause of sore throat. Streptococcus pyogenes is the only important bacterial cause and is more common between the ages of 5 and 15 years. Corynebacterium diphtheriae is very rare now. Another bacterium that causes sore throat, Arcanobacterium haemolyticum, is considered an uncommon cause of pharyngitis.
3.3.3 Issues
There is a strong belief in the role of antibacterials for sore throat in both prescribers and the public. The former are keen on antibacterials because of the well documented difficulty in distinguishing streptococcal infection from viral infections. Consequently, the medical profession often prescribes antibacterials and the public come to assume that antibacterials are necessary for sore throat.
Although is it possible to shorten symptom duration by antibacterial treatment of streptococcal pharyngitis, it is only by a matter of hours. The principal reason for treating streptococcal pharyngitis is to prevent the complications of rheumatic fever and acute glomerulonephritis. There is no doubt that antibacterials can prevent a significant proportion of rheumatic fever. However, rheumatogenic strains of S. pyogenes are now very rare in many populations in developed countries. A meta-analysis has shown no measurable effect on reducing rates of acute glomerulonephritis.[19] The value of antibacterials in preventing suppurative complications such as quinsy, otitis media and sinusitis has also been examined. One systematic review concluded that antibacterials did reduce the rates of these complications but that, because the complications themselves are infrequent, a very large number of patients need to be treated to prevent suppurative complications in a few.[23] Thus, the need for antibacterials at all has been questioned, even in patients with proven streptococcal disease.[23]
A group from Canada has recently developed a scoring method to improve the likelihood of distinguishing viral from streptococcal infection[24] (fig. 1). This simple method, which can be performed within a minute, is based on history and throat examination, and it offers the potential for the patient to participate, giving them some power to understand the decision-making process. This group has been able to show that antibacterial use can be reduced overall in sore throat prescribing, without prejudicing outcomes.
Scoring method to improve the likelihood of distinguishing viral from streptococcal infection. From McIsaac et al.[24] by permission of the publisher. ©1998 Canadian Medical Association (http://www.cma.ca).
3.3.4 Investigations
Culture of throat swabs is the gold standard for the diagnosis of S. pyogenes infection. In general, if antibacterials are going to be prescribed, it is under the assumption that there is streptococcal infection. In US office practice it is common to test throat swabs with point-of-care antigen tests and manage the patient on the basis of the results. Negative antigen tests are sent for culture because generally the specificity of these tests is high but the sensitivity is lower (≈70%).[25]
In other countries, antigen tests are not relied upon and culture is recommended. If the scoring method is used, the likelihood of streptococcal infection is not high, and thus a throat swab is still useful. If the results of throat swab culture are negative, the correct approach is to notify the patient to cease the antibacterial. Alternatively, the conditional prescribing strategy could be used − a script written but filled only if the culture is positive.[12] Throat swab results are often available the next day (identification only). There is no evidence that this puts the patient at increased risk of suppurative or nonsuppurative complications. Except possibly for Group C streptococci, the findings of other types of β-haemolytic streptococci have no clinical significance, even if the laboratory elects to report it.
3.3.5 Treatment
Symptomatic relief should be the primary concern. There are many over-the-counter anti-inflammatory, antiseptic and anaesthetic remedies for sore throat (lozenges and gargles are the most popular). Unfortunately, there is no useful scientific evidence for or against any of these. Preparations that use topical antiseptics should probably be avoided, as they can sometimes co-select for antibacterial resistance. Excellent self help and information can be found at the following website: http://www.ghc.org/web/health_info/disease/flu_cold.jhtml.
The current US recommendations are to diagnose an infection and treat those confirmed as positive on antigen testing or culture. In contrast, the current Australian recommendations (table III) suggest treatment for only a proportion of patients with presumptive or proven streptococcal infection. This is based on the rationale that in communities where rheumatic fever is rare, the benefit of antibacterial treatment for streptococcal sore throat is marginal.
When antibacterials are needed, the drug of choice is phenoxymethylpenicillin (penicillin V). There is still a tendency to prescribe the broader spectrum amoxicillin for this condition,[26] on the mistaken belief that because it is better absorbed it must be a better choice. However, S. pyogenes remains highly susceptible to penicillin, and phenoxymethylpenicillin is more than adequate to cover it. Amoxicillin has a higher rate of adverse effects than phenoxymethylpenicillin and is, therefore, an inferior choice. For patients with penicillin allergy, roxithromycin or erythromycin should be used. Cefalexin or cefaclor could be used but are broader spectrum and unnecessary unless the patient is also intolerant of macrolides.
3.4 Acute Otitis Media
3.4.1 Clinical Points
Acute otitis media is an acute infection in the middle ear secondary to obstruction of the Eustachian tube and trapping of potential pathogens resident in the nasopharynx. It is a difficult condition to diagnose clinically, yet clinical findings are the way to make a diagnosis. The condition is most common in young children, and the important symptoms, such as middle ear pain/ache and hearing impairment due to the accompanying effusion, cannot be articulated at this age. Furthermore, visualising the tympanic membrane can be a challenge in this age group, but unless the tympanic membrane can be seen, the diagnosis is only presumptive. A useful additional feature is ear tugging in the younger age group. Most importantly, reddening and/or dullness (loss of light reflex) of the tympanic membrane is common in URTI and does not constitute acute otitis media, which can be diagnosed only when there is obvious middle ear effusion characterised by bulging and/or failure of movement on insufflation.
3.4.2 Pathogens
Tympanocentesis studies show that S. pneumoniae is responsible for 40 to 50% of infections, H. influenzae 20 to 30%, Moraxella catarrhalis 10 to 15%, other bacteria approximately 5% and viruses alone around 10%.[27] There is a difference between the bacteriology of previously untreated acute otitis media and that of patients with persistent infection,[28] resistant bacteria being more common in the latter.
3.4.3 Issues
Pain is the principal clinical problem in otitis media, and the main reason that medical help is sought. Thus, pain relief is the main target of therapy. However, more than half of patients will be pain free within 24 hours of presentation whether antibacterial therapy is used or not.[29]
Meta-analyses have quantified the benefit of antibacterials.[29,30] The most widely cited meta-analysis concluded that the spontaneous cure rate without antibacterials or tympanocentesis was 81%, and that antibacterial therapy increased the cure rate by 14%, or 1 patient in 7.[30] There was no clear benefit of one antibacterial over another. Other large studies have shown that without any antibacterial therapy the rates of complications such as meningitis and mastoiditis are less than 0.025 and 0.05%, respectively.[31] Therefore, antibacterial therapy is aimed at earlier symptom relief for the 14% of patients known to benefit. Unfortunately, there are no known features at the time of presentation that distinguish those who will benefit from the majority who will not benefit. Were these able to be defined, the prescriber would be in a better position to prescribe only for those who needed antibacterials.
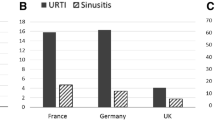
In 1990, there was considerable international variation in prescription rates of antibacterials for otitis media, ranging from 31% in The Netherlands to 98% in Australia.[32] Most countries examined in this study had prescribing rates above 90%. Rates are likely to be lower now that the message about the marginal benefits of antibacterials has become disseminated.
3.4.4 Investigations
The ideal microbiological investigation for acute otitis media is tympanocentesis. It both relieves pressure, and therefore pain, and permits culture for bacterial pathogens (and viruses if so desired). Understandably, this difficult procedure is not recommended routinely. Instead, otoscopy findings are the key to the diagnosis, and recommendations about which antibacterials are best refer to the results of cultures from studies where tympanocentesis has been performed in all patients. If the tympanic membrane is already perforated, it is possible to culture any pus that may be present. However, the value of antibacterials after the infection has progressed to perforation is unclear, as the condition has already undergone self-drainage and pain has been relieved.
3.4.5 Treatment
Pain relief should be the main concern of therapy and patience an integral part of the management. Authorities differ in their recommendations for the use of antibacterials. In the US, routine use of antibacterials is recommended for otoscopy-proven acute otitis media (but not otitis media with effusion).[33] The US rationale is that there is proven benefit in some patients and that at the time of presentation these cannot be distinguished from others who will not benefit. The Dutch approach is quite different, with antibacterials being withheld for 24 to 72 hours, after which time patient contact is made to determine whether there are persistent symptoms[34] (table IV). Australia has elected to follow the Dutch guidelines in large part.[6]
It is widely agreed that amoxicillin is the drug of choice, even though resistance in the 3 important bacteria is common. The rationale is that only a small proportion of patients benefit, that resistance in the main bacterial pathogen, S. pneumoniae, is mostly low level and the pathogen will respond to amoxicillin, and that coverage is superior to that of cefaclor, roxithromycin and cotrimoxazole. In the patients who is allergic to penicillin, choices are more restricted. Second and third generation oral cephalosporins, such as cefaclor, cefuroxime axetil, cefixime, cefpodoxime proxetil, ceftibuten, cefdinir, cefprozil and loracarbef can be used, although all have less activity against strains of S. pneumoniae with reduced penicillin susceptibility than amoxicillin when pharmacodynamic factors are taken into account.[35] Intramuscular ceftriaxone can also be used. Cephalosporins should be avoided if there is a history of anaphylaxis to penicillins. The rates of resistance to cotrimoxazole (>30%) are now too high in most countries for this agent to be recommended. Newer macrolides such as roxithromycin, clarithromycin or azithromycin can be used, but their activity against H. influenzae is limited, and rates of resistance in S. pneumoniae range from 5 to 20% or more.
The duration of therapy in the first instance should be 5 days at most, as longer courses have been shown in meta-analyses not to be of additional value.[36,37] Longer courses are recommended in children aged less than 2 years[33] or in patients with a history of recurrence, where there are data to support the use of longer courses of 10 days.[37]
In patients who fail to respond to first-line treatment, the drug of choice is amoxicillin/clavulanic acid, as it is assumed that bacteria resistant to amoxicillin are still present. If the patient is penicillin allergic or reacted to amoxicillin in the previous course, all the currently available alternatives are suboptimal. The cephalosporins or macrolides noted in the previous paragraph or cotrimoxazole may be tried, but if failure is a result of penicillin-resistant S. pneumoniae, there is a high likelihood of resistance to these agents as well. The new fluoroquinolones such as moxifloxacin or gatifloxacin may be used in adults, but their use in children is restricted by the current nonavailability of paediatric formulations and there is considerable controversy about whether these agents should be used at all in children because of resistance selection in pneumococci.[38]
3.5 Otitis Media with Effusion
3.5.1 Clinical points
Otitis media with effusion (OME) should not be confused clinically with acute otitis media. It is a subacute process manifest by persistent middle ear effusion following acute otitis media. Therefore, it presents primarily as impaired hearing on the affected side, and examination shows dullness with or without some bulging of the tympanic membrane. There are no signs or symptoms of acute inflammation, i.e. no pain, fever or redness of the tympanic membrane.
3.5.2 Issues
OME can either follow a documented occurrence of acute otitis media or present de novo. In either case it follows an episode of otitis media that has not drained either through the Eustachian tube or the tympanic membrane. The role of bacteria in this condition is unclear. Tympanocentesis cultures demonstrate bacteria in fewer than 30% of patients.[39]
The natural history of effusion is well documented. After acute otitis media, 50% still have an effusion after 1 month, 20% after 2 months and 10% after 3 months.[40] In other words, effusion is mostly asymptomatic and a common finding after acute otitis media, and it is likely resolve with the passage of time without intervention.
Two meta-analyses of antibacterial use have demonstrated a significant but small benefit for antibacterial use over placebo in the range of 16 to 25% better outcomes.[41,42] Patients without a preceding history of acute otitis media appear to experience greater benefit.
3.5.3 Investigations
There are no useful simple investigations for OME. The diagnosis is made on history and otoscopic examination.
3.5.4 Treatment
The benefits of antibacterial treatment in OME are small. As a result, all authorities agree that routine antibacterial treatment is not recommended. Reassurance of the parents is the most useful first approach, provided that there is not a history of frequently recurrent acute otitis media. Decongestants do not help and systemic corticosteroids, although they may provide some benefit, are not recommended because the risks are thought to outweigh the benefits.[43] Antibacterials should be considered as the first intervention when the effusion persists for longer than 3 months. Choices should be similar to those of failure of first-line treatment of acute otitis media. The duration is contentious but courses of as long as 1 month would not be unreasonable. Failure of antibacterial treatment or the presence of significant complications of OME warrant surgical intervention (tympanostomy tube).[43]
3.6 Acute Sinusitis
3.6.1 Clinical Points
Acute sinusitis is characterised by fever, headache and facial pain and/or tenderness over the maxillary or frontal sinus(es). It is principally an adult disease. These features are often present early in the course of acute rhinitis in the absence of bacterial infection. It is also tempting to diagnose sinusitis if nasal secretions become purulent. Acute sinusitis, like acute otitis media, is usually a disease of obstruction and bacterial trapping. Therefore, the presence of nasal pus suggests either inflammation in the nasal cavity itself or that sinuses are draining.
3.6.2 Issues
Meta-analyses have not shown a major benefit from the use of antibacterials in patients with acute sinusitis.[44,45] The natural resolution rate without antibacterials within 1 week of presentation is about 70%.[45] If antibacterials are prescribed for sinusitis-like symptoms without further investigation, at least 1 study has confirmed that antibacterials are not superior to placebo.[46] It is likely that the poor efficacy of antibacterials in this setting is because of the fact that sinusitis-like symptoms are common in viral rhinitis, and thus early in the course of illness most patients with such symptoms have a purely viral and self-resolving infection. For this reason, most authorities now do not recommend administering antibacterials to all patients with sinusitis-like symptoms.
3.6.3 Pathogens
The bacteriology of acute sinusitis is similar to that of acute otitis media, being dominated by S. pneumoniae, H. influenzae and M. catarrhalis.[47]
3.6.4 Investigations
As for acute otitis media, the ideal investigations, sinus tapping or washout for culture, are not general practice procedures. Cultures of nasal secretions are not useful and can be quite misleading. Plain radiography has moderate sensitivity and specificity, and is most beneficial in excluding the diagnosis (high negative predictive value). Be wary, as minor degrees of sinus mucosal thickening are also common in viral URTIs. More sensitive tests such as CT scan should be reserved for patients with a complicated disease course.
3.6.5 Treatment
Authorities currently recommend withholding antimicrobials unless specific conditions have been met. US recommendations are to administer narrow spectrum antibacterials in the first instance if the clinical criteria for the diagnosis are met: prolonged rhinosinusitis signs and symptoms without improvement for >10 to 14 days, or more severe rhinosinusitis symptoms such as fever ≥39°C, facial swelling and facial pain.[47] The current Australian guidelines are shown in table V. Early in the course of illness the infection should be managed symptomatically with agents such as topical or systemic decongestants.
Because the bacteriology of acute sinusitis is similar to that of acute otitis media, the choices of antibacterial, when they are indicated, are similar, with the added benefit that doxycycline can be used as this is mainly an adult disease. The rationale of choices is explained in section 3.5.4, with amoxicillin as the drug of choice. In patients who are penicillin-allergic, oral second or third generation cephalosporins or doxycycline are the best alternatives, and failure to respond or relapses should be treated with amoxicillin/clavulanic acid.
3.7 Acute Laryngitis and Tracheitis
3.7.1 Clinical Points
Although they might be regarded as lower respiratory tract infections, acute laryngitis and tracheitis are often part of upper respiratory syndromes, especially the common cold. Hoarseness or loss of voice is the hallmark of laryngitis, whereas the features of tracheitis are cough and retrosternal chest pain exacerbated by coughing. The presence of productive sputum implies bronchitis in addition, and the condition should be managed as such.
One condition that can mimic laryngitis is acute epiglottitis, most often caused by the invasive H. influenzae type b. It is now a rare disease in children because of vaccination, but it must be emphasised that this condition can still occur in inadequately vaccinated children and also rarely in adults. Acute epiglottitis is life-threatening as a result of sudden airway obstruction. In children, acute viral laryngitis and tracheitis can occasionally cause severe subglottic oedema, resulting in partial airway obstruction with a characteristic cough and inspiratory stridor, that is, croup. Both acute epiglottitis and croup require urgent hospitalisation to manage the patient’s airway.
3.7.2 Pathogens
Acute laryngitis and tracheitis are almost always viral in origin, with parainfluenza virus, rhinovirus, adenovirus and influenza viruses being the most common agents.
3.7.3 Issues
Two controlled trials with antibacterials have shown no useful symptomatic benefit from their use.[48,49] This is indirect evidence that bacterial superinfection does not play a role.
3.7.4 Investigations
No investigations are required for these conditions.
3.7.5 Treatment
Symptomatic management is all that is required: voice rest and humidification are used most commonly. Cough suppression may be tried if retrosternal pain on coughing is a problem but is not recommended as a routine. Antibacterial therapy is never required.
4. Conclusion
We have entered a new era in the management of upper respiratory tract infections: it is the era of minimal antibacterial prescribing. The general practitioner must take a leading role in winding back the high community expectation of a ‘pill for every ill’ when that pill is an antibacterial. Even though we do not yet have the bedside tests to distinguish with certainty that patients might benefit from antibacterials at the time of consultation, there are now simple algorithms and lists for providing confidence. There is also a good deal of educational material to assist patients and parents in understanding that URTIs are largely self-resolving and in recognising the downsides of inappropriate antibacterial use. Every opportunity should be taken to re-educate the public about the minor role of antibacterials in URTI.
References
Nyquist A-C, Gonzales R, Steiner JF, et al. Antibiotic prescribing for children with colds, upper respiratory tract infections, and bronchitis. JAMA 1998; 279: 875–7
Schwartz RH, Freij BJ, Ziai M, et al. Antimicrobial prescribing for acute purulent rhinitis in children: a survey of pediatricians and family practitioners. Pediatr Infect Dis J 1997; 16: 185–90
McCaig LF, Hughes JM. Trends in antimicrobial drug prescribing among office-based physicians in the United States. JAMA 1995; 273: 214–9
World Health Organization. Global strategy for containment of antimicrobial resistance —draft [online]. Available from URL: http://www.who.int/emc/globalstrategy/strategy.html [Accessed 2000 Sep]
Collignon PJ, Turnidge JD. Antibiotic resistance in Streptococcus pneumoniae. Med J Aust 2000; 173: S58–64
Therapeutic guidelines —antibiotic. 11th ed. Melbourne: Therapeutic Guidelines Inc., 2000
Turnidge J. Quantifying the impact of resistance for prescribers and drug developers —a function of natural resolution rates. J Antimicrob Chemother 2000; 45: 925–6
Del Mar C, Glasziou P, Hayem M. Are antibiotics indicated as initial treatment for children with acute otitis media? A meta-analysis. BMJ 1997; 314: 1526–9
Del Mar CB, Glasziou PP, Spinks AB. Antibiotics for sore throat (Cochrane review). In: The Cochrane Library 1999; 4. Oxford: Update Software
de Ferranti SD, Ioannidis JP, Lau J, et al. Are amoxycillin and folate antagonists as effective as other antibiotics for acute sinusitis? A meta-analysis. BMJ 1998; 317: 632–7
Butler CC, Rollnick S, Pill R, et al. Understanding the culture of prescribing: qualitative study of general practitioners’ and patients’ perceptions of antibiotics for sore throats. BMJ 1998; 317: 637–42
Little PP, Williamson I, Warner G, et al. Open randomised trial of prescribing strategies in managing sore throat. BMJ 1997; 314: 722–7
Cates C. An evidence based approach to reducing antibiotic use in children with acute otitis media: controlled before and after study. BMJ 1999; 318: 715–6
Rogers S, Light I. A role for GPs in diminishing antibiotic resistance. Newsletters of the Commonwealth Department of Health and Aged Care —Be Wise with Medicines campaign. MediScene 1998 May
Barrett B, Vohlman M, Calabrese C. Echinacea for upper respiratory infections. J Fam Pract 1999; 48: 628–35
Melchart D, Linde K, Fischer P, et al. Echinacea for preventing and treating the common cold. Cochrane Database Syst Rev 2000; CD000530
Turner RB, Riker DK, Gangemi JD. Ineffectiveness of echinacea for prevention of experimental rhinovirus colds. Antimicrob Agents Chemother 2000; 44: 1708–9
Schwartz RH, Freij BJ, Ziai M, et al. Antimicrobial prescribing for acute purulent rhinitis in children: a survey of paediatricians and family practitioners. Pediatr Infect Dis J 1997; 16: 185–90
Rosenstein N, Phillips WR, Gerber MA, et al. The common cold —principles of judicious use of antimicrobial agents. Pediatrics 1998; 101: 181–4
Taverner D, Bickford L, Draper M. Nasal decongestants for the common cold (Cochrane review). In: The Cochrane Library 2000; 4. Oxford: Update Software, 2000
Marshall I. Zinc for the common cold (Cochrane review). In: The Cochrane Library 2000; 4. Oxford: Update Software, 2000
Douglas RM, Chalker EB, Treacy B. Vitamin C for preventing and treating the common cold (Cochrane review). In: The Cochrane Library 2001; 3. Oxford: Update Software, 2001
Del Mar C. Managing sore throat: a literature review. II. Do antibiotics confer benefit? Med J Aust 1992; 156: 644–9
McIsaac WJ, White D, Tanneribaurn D, et al. A clinical scoring method to reduce unnecessary antibiotic use in patients with sore throat. Can Med Assoc J 1998; 158: 75–83
Schwarz B, Marcy SM, Phillips WR, et al. Pharyngitis —principles of judicious use of antimicrobial agents. Pediatrics 1998; 101: 171–4
National Prescribing Service. Prescribing practice review no. 9, August 2000. (http://www.nps.org.au)
Dowell SF, Butler JC, Gicbink GS, et al. Acute otitis media: management and surveillance in an era of pneumococcal resistance —a report from the Drug-resistant Streptococcus ptneumoniae Therapeutic Working Group. Pediatr Infect Dis J 1999; 18: 1–9
Pichichero ME. Recurrent and persistent otitis media. Pediatr Infect Dis J 2000; 19: 911–6
Glasziou PP, Del Mar CB, Hayern M, et al. Antibiotic for acute otitis media in children (Cochrane review). In: The Cochrane Library. Cochrane Library 2000; 4. Oxford: Update Software
Rosenfeld RM, Vertrees JE, Carr J, et al. Clinical efficacy of antimicrobial drugs for acute otitis media: metaanalysis of 5400 children from thirty three randomised trials. J Pediatr 1994; 124: 355–67
Van Buchem FL, Peeters NF, van’t Hof MA. Acute otitis media: a new treatment strategy. BMJ 1985; 290: 1033–7
Froom J, Culpepper L, Grob P, et al. Diagnosis and antibiotic treatment of acute otitis media: report from International Primary Care Network. BMJ 1990; 300: 582–6
Dowell SF, Marcy SM, Phillips WR, et al. Otitis media —principles of judicious use of antimicrobial agents. Pediatrics 1998; 101: 165–71
Froom J, Culpepper L, Jacobs M, et al. Antimicrobials for acute otitis media? A review from the International Primary Care Network. BMJ 1997; 315: 98–102
Craig WA, Andes D. Pharmacokinetics and pharmacodynamics of antibiotics in otitis media. Pediatr Infect Dis J 1996; 15: 944–8
Kozyrskyj AL, Hildes-Ripstein E, Longstaffe SEA, et al. Treatment of acute otitis media with shortened courses of antibiotics. JAMA 1998; 279: 1736–42
Pichichero ME. Short course antibiotic therapy for respiratory infections: a review of the evidence. Pediatr Infect Dis J 2000; 19: 929–37
Heffelfinger JD, Dowell SF, Jorgensen JH, et al. Management of community-acquired pneumonia in the era of pneumococcal resistance: a report from the Drug-resistant Streptococcus pneumoniae Therapeutic Working Group. Arch Intern Med 2000; 160: 1399–408
Sutton DV, Derkay CS, Darrow DH, et al. Resistant bacteria in middle ear fluid at the time of tympanotomy tube surgery. Ann Otol Rhinol Laryngol 2000; 109: 24–9
Teele DW, Klein JO, Rosner BA. Epidemiology of otitis media in children. Ann Otol Rhinol Laryngol 1980; 89 Suppl.: 5–6
Rosenfeld RM, Post JC. Meta-analysis of antibiotics for the treatment of otitis media with effusion. Otolaryngol Head Neck Surg 1992; 106: 378–86
Williams RL, Chalmers TC, Stange KC, et al. Use of antibiotics in preventing recurrent otitis media and in treating otitis media with effusion. A meta-analytic attempt to resolve the brouhaha. JAMA 1993; 270: 1344–51
Bluestone CD. Role of surgery for otitis media in the era of resistant bacteria. Pediatr Infect Dis J 1998; 17: 1090–8
de Bock GH, Dekker FW, Stolk J, et al. Antimicrobial treatment in acute maxillary sinusitis: a meta-analysis. J Clin Epidemiol 1997; 50: 881–90
de Ferranti SD, Ioannidis JPA, Lau J, et al. Are amoxycillin and folate inhibitors as effective as other antibiotics for acute sinusitis? A meta-analysis. BMJ 1998; 317: 632
Stalman W, van Essen GA, van der Graaf Y, et al. The end of antibiotic treatment in adults with sinusitis-like complaints in general practice? A placebo-controlled double-blind randomised doxycycline trial. Br J Gen Pract 1997; 47: 794–9
O’Brien KL, Dowell SF, Schwartz B, et al. Acute sinusitis —principles of judicious use of antimicrobial agents. Pediatrics 1998; 101: 174–7
Schalen L, Christensen P, Eliasson I, et al. Inefficacy of penicillin V in acute laryngitis in adults. Evaluation from results of double-blind study. Ann Otol Rhinol Laryngol 1985; 94: 14–7
Schalen L, Eliasson I, Kamme C, et al. Erythromycin in acute laryngitis in adults. Ann Otol Rhinol Laryngol 1993; 102: 209–14
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Turnidge, J. Responsible Prescribing for Upper Respiratory Tract Infections. Drugs 61, 2065–2077 (2001). https://doi.org/10.2165/00003495-200161140-00004
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-200161140-00004