Abstract
Background
Excessive opioid prescribing is common after curative-intent surgery, but little is known about what factors influence prescribing behaviors among surgeons. To identify targets for intervention, we performed a qualitative study of opioid prescribing after curative-intent surgery using the Theoretical Domains Framework, a well-established implementation science method for identifying factors influencing healthcare provider behavior.
Methods
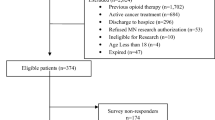
Prior to data collection, we constructed a semi-structured interview guide to explore decision making for opioid prescribing. We then conducted interviews with surgical oncology providers at a single comprehensive cancer center. Interviews were recorded, transcribed verbatim, then independently coded by two investigators using the Theoretical Domains Framework to identify theoretical domains relevant to opioid prescribing. Relevant domains were then linked to behavior models to select targeted interventions likely to improve opioid prescribing.
Results
Twenty-one subjects were interviewed from November 2016 to May 2017, including attending surgeons, resident surgeons, physician assistants, and nurses. Five theoretical domains emerged as relevant to opioid prescribing: environmental context and resources; social influences; beliefs about consequences; social/professional role and identity; and goals. Using these domains, three interventions were identified as likely to change opioid prescribing behavior: (1) enablement (deploy nurses during preoperative visits to counsel patients on opioid use); (2) environmental restructuring (provide on-screen prompts with normative data on the quantity of opioid prescribed); and (3) education (provide prescribing guidelines).
Conclusions
Key determinants of opioid prescribing behavior after curative-intent surgery include environmental and social factors. Interventions targeting these factors are likely to improve opioid prescribing in surgical oncology.


Similar content being viewed by others
References
Rudd RA, Seth P, David F, Scholl L. Increases in drug and opioid-involved overdose deaths—United States, 2010–2015. MMWR. 2016;65(5051):1445–52.
Levy B, Paulozzi L, Mack KA, Jones CM. Trends in opioid analgesic-prescribing rates by specialty, U.S., 2007–2012. Am J Prev Med. 2015;49(3):409–13.
Brummett CM, Waljee JF, Goesling J, et al. New persistent opioid use after minor and major surgical procedures in US adults. JAMA Surg. 2017;152(6):e170504.
Lee JS, Hu HM, Edelman AL, et al. New persistent opioid use among patients with cancer after curative-intent surgery. J Clin Oncol. 2017;35(36):4042–9.
Jung BF, Herrmann D, Griggs J, Oaklander AL, Dworkin RH. Neuropathic pain associated with non-surgical treatment of breast cancer. Pain. 2005;118(1–2):10–4.
Land SR, Kopec JA, Cecchini RS, et al. Neurotoxicity from oxaliplatin combined with weekly bolus fluorouracil and leucovorin as surgical adjuvant chemotherapy for stage II and III colon cancer: NSABP C-07. J Clin Oncol. 2007;25(16):2205–11.
Mols F, Beijers T, Lemmens V, van den Hurk CJ, Vreugdenhil G, van de Poll-Franse LV. Chemotherapy-induced neuropathy and its association with quality of life among 2–11 year colorectal cancer survivors: results from the population-based PROFILES registry. J Clin Oncol. 2013;31(21):2699–707.
Portenoy RK. Treatment of cancer pain. Lancet. 2011;377(9784):2236–47.
Swarm RA, Abernethy AP, Anghelescu DL, et al. Adult cancer pain. J Natl Compr Cancer Netw. 2013;11(8):992–1022.
Fann JR, Ell K, Sharpe M. Integrating psychosocial care into cancer services. J Clin Oncol. 2012;30(11):1178–86.
Zabora J, BrintzenhofeSzoc K, Curbow B, Hooker C, Piantadosi S. The prevalence of psychological distress by cancer site. Psychooncology. 2001;10(1):19–28.
Brummett CM, Janda AM, Schueller CM, et al. Survey criteria for fibromyalgia independently predict increased postoperative opioid consumption after lower-extremity joint arthroplasty: a prospective, observational cohort study. Anesthesiology. 2013;119(6):1434–43.
Janda AM, As-Sanie S, Rajala B, et al. Fibromyalgia survey criteria are associated with increased postoperative opioid consumption in women undergoing hysterectomy. Anesthesiology. 2015;122(5):1103–11.
Dreyer T, Rontal R, Gabriel K, Udow-Phillips M. Uncoordinated Prescription Opioid Use in Michigan. Ann Arbor, MI: Center for Healthcare Research and Transformation; Dec 2015. http://www.chrt.org/publication/uncoordinated-prescription-opioid-use-in-michigan/. Accessed 20 Feb 2017.
Hill MV, McMahon ML, Stucke RS, Barth RJ Jr. Wide variation and excessive dosage of opioid prescriptions for common general surgical procedures. Ann Surg. 2017;265(4):709–14.
Atkins L, Francis J, Islam R, et al. A guide to using the Theoretical Domains Framework of behaviour change to investigate implementation problems. Implement Sci. 2017;12(1):77.
Cane J, O’Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci. 2012;7:37.
Michie S, Johnston M, Abraham C, Lawton R, Parker D, Walker A. Making psychological theory useful for implementing evidence based practice: a consensus approach. Qual Saf Health Care. 2005;14(1):26.
Islam R, Tinmouth AT, Francis JJ, et al. A cross-country comparison of intensive care physicians’ beliefs about their transfusion behaviour: a qualitative study using the Theoretical Domains Framework. Implement Sci. 2012;7:93.
Duncan EM, Francis JJ, Johnston M, et al. Learning curves, taking instructions, and patient safety: using a theoretical domains framework in an interview study to investigate prescribing errors among trainee doctors. Implement Sci. 2012;7(1):86.
McSherry LA, Dombrowski SU, Francis JJ, et al. ‘It’s a can of worms’: understanding primary care practitioners’ behaviours in relation to HPV using the theoretical domains framework. Implement Sci. 2012;7(1):73.
Michie S, Pilling S, Garety P, et al. Difficulties implementing a mental health guideline: an exploratory investigation using psychological theory. Implement Sci. 2007;2:8.
Patey AM, Islam R, Francis JJ, Bryson GL, Grimshaw JM. Anesthesiologists’ and surgeons’ perceptions about routine pre-operative testing in low-risk patients: application of the Theoretical Domains Framework (TDF) to identify factors that influence physicians’ decisions to order pre-operative tests. Implement Sci. 2012;7(1):52.
Biezen R, Brijnath B, Grando D, Mazza D. Management of respiratory tract infections in young children: a qualitative study of primary care providers’ perspectives. NPJ Prim Care Respir Med. 2017;27:15.
Walker AE, Grimshaw J, Johnston M, Pitts N, Steen N, Eccles M. PRIME—PRocess modelling in ImpleMEntation research: selecting a theoretical basis for interventions to change clinical practice. BMC Health Serv. Res. 2003;3(1):22.
Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42.
Soneji N, Clarke HA, Ko DT, Wijeysundera DN. Risks of developing persistent opioid use after major surgery. JAMA Surg. 2016;151(11):1083–4.
Clarke H, Soneji N, Ko DT, Yun L, Wijeysundera DN. Rates and risk factors for prolonged opioid use after major surgery: population based cohort study. BMJ. 2014;348:g1251.
Alam A, Gomes T, Zheng H, Mamdani MM, Juurlink DN, Bell CM. Long-term analgesic use after low-risk surgery: a retrospective cohort study. Arch Intern Med. 2012;172(5):425–30.
Lee JS, Hu HM, Brummett CM, et al. Postoperative opioid prescribing and the pain scores on hospital consumer assessment of healthcare providers and systems survey. JAMA. 2017;317(19):2013–5.
Bartels K, Mayes LM, Dingmann C, Bullard KJ, Hopfer CJ, Binswanger IA. Opioid use and storage patterns by patients after hospital discharge following surgery. PLoS ONE. 2016;11(1):e0147972.
Bates C, Laciak R, Southwick A, Bishoff J. Overprescription of postoperative narcotics: a look at postoperative pain medication delivery, consumption and disposal in urological practice. J Urol. 2011;185(2):551–5.
Bicket MC, Long JJ, Pronovost PJ, Alexander GC, Wu CL. Prescription opioid analgesics commonly unused after surgery: a systematic review. JAMA Surg. 2017;152(11):1066–71.
Harris K, Curtis J, Larsen B, et al. Opioid pain medication use after dermatologic surgery a prospective observational study of 212 dermatologic surgery patients. JAMA Dermatol. 2013;149(3):317–21.
Maughan BC, Hersh EV, Shofer FS, et al. Unused opioid analgesics and drug disposal following outpatient dental surgery: a randomized controlled trial. Drug Alcohol Depend. 2016;168(1879-0046):328–34.
Rodgers J, Cunningham K, Fitzgerald K, Finnerty E. Opioid consumption following outpatient upper extremity surgery. J Hand Surg Am. 2012;37(4):645–50.
Steinmo SH, Michie S, Fuller C, Stanley S, Stapleton C, Stone SP. Bridging the gap between pragmatic intervention design and theory: using behavioural science tools to modify an existing quality improvement programme to implement “Sepsis Six”. Implement Sci. 2016;11(1):14.
Hill MV, Stucke RS, McMahon ML, Beeman JL, Barth RJ Jr. An Educational Intervention Decreases Opioid Prescribing After General Surgical Operations. Ann Surg. 2017; 267(3):468.
Howard RA, Waljee JF, Brummett CM, Englesbe MJ, Lee JS. Reduction in opioid prescribing through implementation of evidence-based prescribing guidelines. JAMA Surg. 2017.
Arabi YM, Al-Dorzi HM, Alamry A, et al. The impact of a multifaceted intervention including sepsis electronic alert system and sepsis response team on the outcomes of patients with sepsis and septic shock. Ann Intensiv Care. 2017;7(1):57.
Steinmo S, Fuller C, Stone SP, Michie S. Characterising an implementation intervention in terms of behaviour change techniques and theory: the ‘Sepsis Six’ clinical care bundle. Implement Sci. 2015;10(1):111.
Chiu AS, Healy JM, DeWane MP, Longo WE, Yoo PS. Trainees as agents of change in the opioid epidemic: optimizing the opioid prescription practices of surgical residents. J Surg Educ. 2018;75(1):65–71.
Funding
Dr. Lee is a National Research Service Award postdoctoral fellow supported by the National Cancer Institute (5T32 CA009672-23), and Dr. Waljee receives funding from the Michigan Department of Health and Human Services, the National Institute on Drug Abuse (RO1 DA042859), and the Agency for Healthcare Research and Quality (1K08 HS023313-01). The contents of this study are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health or the Michigan Department of Health and Human Services.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix 1
Semi-structured Interview Guide
Decision Making for the Initial Postoperative Opioid Prescription
-
1.
We are going to discuss your practice for prescribing opioids to cancer patients. How do you decide what pain medication to use and how much to prescribe (dose, quantity of pills, refills)?
-
2.
How did you come up with the above strategy?
-
3.
How much do you prescribe relative to how much you think the patient will actually consume?
-
If applicable, why do you prescribe more than they need? What are the possible risks of this unused medication?
-
-
4.
What do you think other surgeons do with regard to prescribing opioids?
-
5.
What would consider ideal practice for prescribing opioids?
-
6.
What are the barriers to prescribing less opioid medication?
Counseling Patients on Safe Opioid Use:
-
7.
Now we are going to discuss counseling patients on opioid use. What key factors do you address when counseling patients on opioid use?
-
If applicable, why do you not discuss the following factors: risk of abuse, risk of diversion, safe disposal of medication.
-
-
8.
Describe how counseling on opioid use is typically delivered to your patients (who provides it, who receives it, when is it given, written vs. oral)?
-
9.
What do you think other physicians do for counseling patients?
-
10.
What would you consider ideal practice?
-
11.
What are the barriers to achieving this?
Management of Opioid Misuse:
-
12.
After discharge, who most commonly answers questions from patients regarding opioid use and pain management?
-
13.
How do you determine if a patient is inappropriately using opioids?
-
14.
What do you do for these patients?
-
15.
How do you think other physicians identify and manage inappropriate opioid use?
-
16.
What would you consider to be ideal practice for identifying and managing inappropriate opioid use?
-
17.
What are the barriers to achieving this?
How a Cancer Diagnosis Affects Opioid Prescribing:
-
18.
How does a patient’s diagnosis of cancer affect your practice for prescribing opioids, counseling, and managing postoperative opioid use?
-
19.
Anything else you would like to add?
Appendix 2
See Table 2.
Rights and permissions
About this article
Cite this article
Lee, J.S., Parashar, V., Miller, J.B. et al. Opioid Prescribing After Curative-Intent Surgery: A Qualitative Study Using the Theoretical Domains Framework. Ann Surg Oncol 25, 1843–1851 (2018). https://doi.org/10.1245/s10434-018-6466-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-018-6466-x