Abstract
Objective
The aim of this study was to summarize the current literature comparing the surgical outcomes of invasive intraductal papillary mucinous neoplasms (IPMNINV) and conventional pancreatic ductal adenocarcinomas (PDAC) in order to determine the differences in disease characteristics and prognosis.
Methods
Systematic review of the literature yielded 12 comparative studies reporting the clinicopathological characteristics and overall survival (OS) of 1,450 patients with IPMNINV with 19,304 patients with conventional PDAC.
Results
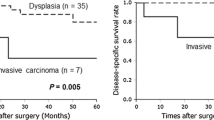
IPMNINV had a significantly lower likelihood of tumors extending beyond the pancreas [27.6 vs. 94.3 %; T4 vs. T1: odds ratio (OR) 0.111, 95 % confidence intervals (CI) 0.057–0.214], nodal metastasis (45.4 vs. 62.9 %: OR 0.507, 95 % CI 0.347–0.741), positive margin (14.2 vs. 28.3 %; OR 0.438, 95 % CI 0.322–0.596), perineural invasion (49.2 vs. 76.5 %; OR 0.304, 95 % CI 0.106–0.877) and vascular invasion (25.2 vs. 45.7 % OR 0.417, 95 % CI 0.177–0.980) when compared with PDAC. The 5-year OS of IPMNINV was significantly better than PDAC [31.4 vs. 12.4 %: hazard ratio (HR) 0.659, 95 % CI 0.574–0.756]. The tubular subtype had a poorer 5-year OS and demonstrated significantly more aggressive features such as nodal metastases, vascular invasion, and perineural invasion compared with the colloid subtype.
Conclusion
IPMNINV were significantly more likely to present at an earlier stage and were less likely to demonstrate nodal involvement, perineural invasion and vascular invasion. When controlled for stage, IPMNINV had an improved OS when compared with PDAC in the early stages.


Similar content being viewed by others
References
Kloppel G, Solcia E, Longnecker DS, Capella C, Sobin LH. Histological typing of exocrine pancreas. Berlin. Springer; 1996.
Goh BK, Tan YM, Cheow PC, et al. Cystic neoplasms of the pancreas with mucin-production. Eur J Surg Oncol. 2005;31:282–287.
Goh BK, Tan YM, Chung YF, et al. A review of mucinous cystic neoplasms of the pancreas defined by ovarian-type stroma: clinicopathologic features of 344 patients. World J Surg. 2006;30(12):2236–45.
Longnecker DS, Adler G, Hruban RH, Kloppel G. Intraductal papillary-mucinous neoplasms of the pancreas. In: Hamilton SR, Bltonen LA, editors. Pathology and genetics of tumours of the digestive system. Lyon: IARC Press; 2000:237e40.
Sohn TA, Yeo CJ, Cameron JL, et al. Intraductal papillary mucinous neoplasms of the pancreas: anupdated experience. Ann Surg. 2004;239(6):788–97.
Wada K, Kozarek RA, Traverso LW. Outcomes following resection of invasive and noninvasiveintraductal papillary mucinous neoplasms of the pancreas. Am J Surg. 2005;189(5):632–6.
Sohn TA, Yeo CJ, Cameron JL, Iacobuzio-Donahue CA, Hruban RH, Lillemoe KD. Intraductal papillary mucinous neoplasms of the pancreas: an increasingly recognized clinicopathologic entity. Ann Surg. 2001;234(3):313–21.
Schnelldorfer T, Sarr MG, Nagorney DM, et al. Experience with 208 resections for intraductal papillary mucinous neoplasm of the pancreas. Arch Surg. 2008;143(7):639–46.
Nara S, Shimada K, Sakamoto Y, Esaki M, Kosuge T, Hiraoka N. Clinical significance of frozen section analysis during resection of intraductal papillary mucinous neoplasm: should a positive pancreatic margin for adenoma or borderline lesion be resected additionally? J Am Coll Surg. 2009;209:614–621.
Crippa S, Fernández-del Castillo C, Salvia R, et al. Mucin-producing neoplasms of the pancreas: an analysis of distinguishing clinical and epidemiologic characteristics. Clin Gastroenterol Hepatol. 2010;8:213–219.
Salvia R, Fernandez-del Castillo C, Bassi C, et al. Main-duct intraductal papillary mucinous neoplasms of the pancreas: clinical predictors of malignancy and long-term survival following resection. Ann Surg. 2004;239(5):678–85.
Maire F, Hammel P, Terris B, et al. Prognosis of malignant intraductal papillary mucinous tumours of the pancreas after surgical resection. Comparison with pancreatic ductal adenocarcinoma. Gut. 2002;51(5):717–22.
Wasif N, Bentrem DJ, Farrell JJ, Ko CY, Hines OJ, Reber HA, et al. Invasive intraductal papillary mucinous neoplasm versus sporadic pancreatic adenocarcinoma: a stage-matched comparison of outcomes. Cancer. 2010;116(14):3369–77.
Yamaguchi K, Kanemitsu S, Hatori T, et al. Pancreatic ductal adenocarcinoma derived from IPMN and pancreatic ductal adenocarcinoma concomitant with IPMN. Pancreas. 2011;40(4):571–80.
Waters JA, Schnelldorfer T, Aguilar-Saavedra JR, et al. Survival after resection for invasive intraductal papillary mucinous neoplasm and for pancreatic adenocarcinoma: a multi-institutional comparison according to American Joint Committee on Cancer Stage. J Am Coll Surg. 2011;213(2):275–83.
Yopp AC, Katabi N, Janakos M, et al. Invasive carcinoma arising in intraductal papillary mucinous neoplasms of the pancreas: a matched control study with conventional pancreatic ductal adenocarcinoma. Ann Surg. 2011;253(5):968–74.
Poultsides GA, Reddy S, Cameron JL, et al. Histopathologic basis for the favorable survival after resection of intraductal papillary mucinous neoplasm-associated invasive adenocarcinoma of the pancreas. Ann Surg. 2010;251(3):470–6.
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700.
Japan Pancreas Society. Classification of pancreatic carcinoma. 2nd English ed. Tokyo: Kanehara & Co, Ltd; 2003.
Sobin LH, Wittekind C; International Union Against Cancer. TNM classification of malignant tumours. 6th ed. New York: Wiley-Liss; 2002.
Fleming ID, Cooper JS, Henson D, et al. AJCC cancer staging manual. 5th ed. New York: Lippincott-Raven; 1997.
Schlesselman J, Stolley P. Case-control studies, design, conduct, analysis. New York: Oxford University Press; 1982.
Shimada K, Sakamoto Y, Sano T, Kosuge T, Hiraoka N. Invasive carcinoma originating in an intraductal papillary mucinous neoplasm of the pancreas: a clinicopathologic comparison with a common type of invasive ductal carcinoma. Pancreas. 2006;32(3):281–7.
Woo SM, Ryu JK, Lee SH, Yoo JW, Park JK, Kim YT, et al. Survival and prognosis of invasive intraductal papillary mucinous neoplasms of the pancreas: comparison with pancreatic ductal adenocarcinoma. Pancreas. 2008;36(1):50–5.
Murakami Y, Uemura K, Sudo T, Hayashidani Y, Hashimoto Y, Nakashima A, et al. Invasive intraductal papillary-mucinous neoplasm of the pancreas: comparison with pancreatic ductal adenocarcinoma. J Surg Oncol. 2009;100(1):13–8.
Mino-Kenudson M, Fernández-del Castillo C, Baba Y, et al. Prognosis of invasive intraductal papillary mucinous neoplasm depends on histological and precursor epithelial subtypes. Gut 2011;60(12):1712–20.
Chinn S. A simple method for converting an odds ratio to effect size for use in meta-analysis. Stat Med 2000;19:3127–3131.
Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials. 2007;8:16.
Dickersin K, Berlin JA. Meta-analysis: state-of-the-science. Epidermiol Rev. 1992;14:154–176.
Kang MJ, Lee KB, Jang JY, Kwon W, Park JW, Chang YR, et al. Disease spectrum of intraductal papillary mucinous neoplasm with an associated invasive carcinoma invasive IPMN versus pancreatic ductal adenocarcinoma-associated IPMN. Pancreas. 2013;42(8):1267–74.
Sadakari Y, Ohuchida K, Nakata K, et al. Invasive carcinoma derived from the nonintestinal type intraductal papillary mucinous neoplasm of the pancreas has a poorer prognosis than that derived from the intestinal type. Surgery. 2010;147(6):812–7.
Goh BK, Tan YM, Cheow PC, Chung YF, Chow PK, Wong WK, et al. Outcome of distal pancreatectomy for pancreatic adenocarcinoma. Dig Surg. 2008;25(1):32–8.
Le H, Ziogas A, Rhee JM, Lee JG, Lipkin SM, Zell JA. A population-based, descriptive analysis of malignant intraductal papillary mucinous neoplasms of the pancreas. Cancer Epidemiol Biomarkers Prev. 2008;17(10):2737–41.
Goh BK, Thng CH, Tan DM, et al. Evaluation of the Sendai and 2012 International Consensus Guidelines based on initial cross-sectional imaging findings for the management of mucinous cystic lesions of the pancreas: a single institution experience with 114 surgically-treated patients. Am J Surg. Epub 17 Jan 2014.
Winter JM, Cameron JL, Campbell KA, et al. 1423 pancreaticoduodenectomies for pancreatic cancer: a single-institution experience. J Gastrointest Surg. 2006;10(9):1199–210.
Conlon KC, Klimstra DS, Brennan MF. Long-term survival after curative resection for pancreatic ductal adenocarcinoma. Clinicopathologic analysis of 5-year survivors. Ann Surg. 1996;223(3):273–279.
Konstantinidis IT, Vinuela EF, Tang LH, et al. Incidentally discovered pancreatic intraepithelial neoplasia: what is its clinical significance? Ann Surg Oncol. 2013;20:3643–7.
Goh BK, Tan DM, Thng CH, et al. Are the Sendai and Fukuoka consensus guidelines for mucinous neoplasms of the pancreas useful in the initial triage of all suspected pancreatic cystic neoplasms? A single institution experience with 317 surgically-treated patients. Ann Surg Oncol. Epub 7 Feb 2014.
Goh BK, Tan DM, Ho MF, Lim KH, Chung AY, Ooi LL. Utility of the Sendai consensus guidelines for branch-duct intraductal papillary mucinous neoplasms: a systematic review. J Gastrointestin Surg. In press.
Fritz S, Fernandez-del Castillo C, Mino-Kenudson M, et al. Global genomic analysis of intraductal papillary mucinous neoplasms of the pancreas reveals significant molecular differences compared to ductal adenocarcinoma. Ann Surg. 2009;249(3):440–7.
Tanaka M, Chari S, Adsay V, et al. International consensus guidelines for management of intraductal papillary mucinous neoplasms and mucinous cystic neoplasms of the pancreas. Pancreatology. 2006;6:17–32.
Salvia R, Partelli S, Crippa S, et al. Intraductal papillary mucinous neoplasms of the pancreas with multifocal involvement of branch ducts. Am J Surg. 2009;198(5):709–14.
Oettle H, Post S, Neuhaus P, et al. Adjuvant chemotherapy with gemcitabine vs observation in patients undergoing curative-intent resection of pancreatic cancer: a randomized controlled trial. JAMA 2007;297(3):267–77.
Oettle H, Neuhaus P, Hochhaus A, et al. Adjuvant chemotherapy with gemcitabine and long-term outcomes among patients with resected pancreatic cancer: the CONKO-001 randomized trial. JAMA. 2013;310(14):1473–1481.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix 1. Statistical Analyses
To facilitate the pooling of results across studies in the meta-analysis, the number of individuals with or without the event of interest in the IPMN and PDAC groups was used for dichotomous outcomes. The Mantel–Haenszel (MH) method was used to pool the OR across studies. A Woolf–Haldane continuity correction of 0.5 was used when the number of events for one of the groups was zero.22 Studies in which there was no event in an outcome of interest for both groups were excluded.
Four studies reported tumor size as a continuous outcome,13,15,23,24 while four others reported it as a dichotomized outcome.14,16,25,26 ORs were transformed into effect sizes allowing the pooling of results as effect measures for continuous outcomes by using the inverse-variance (IV) approach.27
Analysis of the 5-year OS was performed by computing the p value for the test of survival difference between the two groups, the number of events in each group, and the number of patients in each group. These statistics were used to compute the HR and its corresponding variance for each study. The HRs and variances from the 11 studies were, in turn, pooled together via the IV approach.28
Heterogeneity between the studies was evaluated using the Chi squared test of heterogeneity. If there was limited evidence supporting the assumption of homogeneity of studies for an outcome (i.e. the p value of the heterogeneity Chi squared test was <0.1), a random effects model was used;29 otherwise, a fixed effects model was used. Two separate sets of sensitivity analyses were performed: (1) excluding each study individually; and (2) excluding studies with a sample size fewer than 20 patients in each group, from the analysis of each outcome. Pooled results from these subgroups were computed and compared with the pooled results from the set of studies without these exclusion criteria. The meta-analysis was conducted using STATA SE 10 (StataCorp. LP, College Station, TX, USA).
Appendix 2
See Fig. 3.
Appendix 3
See Fig. 4.
Forest plots illustrating the results of a meta-analysis comparing pathological characteristics in invasive IPMN and conventional PDAC. Pooled ORs or weighted mean differences (WMDs) with 95 % CIs were calculated using the fixed effects or random effects* model where appropriate. a Tumor size; b margin status; c lymphatic invasion; d tumor grade
Appendix 4
See Fig. 5.
Forest plots illustrating the results of a meta-analysis comparing clinical characteristics in invasive IPMN and conventional PDAC. Pooled ORs with 95 % CIs are calculated using the fixed effects or random effects* model where appropriate. a Location; b surgical type: distal vs. Whipple, and c total vs. Whipple; d local spread: T2 vs. T1, e T3 vs. T1, and f T4 vs. T1; g tumor stage: TNM2 vs. TNM1, hTNM3 vs. TNM1, and iTNM4 vs. TNM1
Appendix 5
Sensitivity analyses were carried out by excluding each study individually from the analysis of each outcome (Appendix 6). Among outcomes with a p value less than 0.05 in Table 3, location, surgical type, local spread, tumor stage, nodal metastasis, and margin status had consistent findings in the sensitivity analyses. Although surgical type, perineural invasion, and vascular invasion had p-values exceeding 0.05 in the sensitivity analyses, the ORs were in the same consistent direction as those in Table 3. Among outcomes with a p value more than 0.05 in Table 3, local spread (T2 vs. T1), tumor stage (TNM stage 4 vs. TNM stage 1), lymphatic invasion, and tumor size had p-values lower than 0.05 in the sensitivity analyses. The ORs and effect sizes were consistent with those in Table 3.
Additional sensitivity analyses were performed by including those studies with more than 20 patients in each group (Appendix 7). The exclusion of studies with small sample sizes reduces heterogeneity across the studies and did not change the conclusion for all outcomes. This suggests that the findings based on all available studies shown were robust.
Appendix 6
See Table 6.
Appendix 7
See Table 7.
Rights and permissions
About this article
Cite this article
Koh, YX., Chok, AY., Zheng, HL. et al. Systematic Review and Meta-Analysis Comparing the Surgical Outcomes of Invasive Intraductal Papillary Mucinous Neoplasms and Conventional Pancreatic Ductal Adenocarcinoma. Ann Surg Oncol 21, 2782–2800 (2014). https://doi.org/10.1245/s10434-014-3639-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-014-3639-0