Abstract
Background
Although recommendations for breast cancer follow-up frequency exist, current follow-up guidelines are standardized, without consideration of individual patient characteristics. Some studies suggest oncologists are using these characteristics to tailor follow-up recommendations, but it is unclear how this is translating into practice. The objective of this study was to examine current patterns of oncologist breast cancer follow-up and determine the association between patient and tumor characteristics and follow-up frequency.
Methods
The Surveillance, Epidemiology, and End Results (SEER)-Medicare database was used to identify stage I–III breast cancer patients diagnosed 2000–2007 (n = 39,241). Oncologist follow-up visits were defined using Medicare specialty provider codes and the linked AMA Masterfile. Multinomial logistic regression determined the association between patient and tumor characteristics and oncologist follow-up visit frequency.
Results
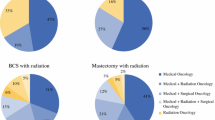
Younger age (p < 0.001), positive nodes (p < 0.001), estrogen receptor/progesterone receptor positivity (p < 0.001), and increasing treatment intensity (p < 0.001) were most strongly associated with more frequent follow-up. However, after accounting for these characteristics, significant variation in follow-up frequency was observed. In addition to patient factors, the number and types of oncologists involved in follow-up were associated with follow-up frequency (p < 0.001). Types of oncologists providing follow-up varied, with medical oncologists the sole providers of follow-up for 19–51 % of breast cancer survivors. Overall, 58 % of patients received surgical oncology, and 51 % undergoing radiation received radiation oncology follow-up, usually in combination with medical oncology.
Conclusions
Significant variation in breast cancer follow-up frequency exists. Developing follow-up guidelines tailored for patient, tumor, and treatment characteristics while also providing guidance on who should provide follow-up has the potential to increase clinical efficiency.



Similar content being viewed by others
References
Siegel R, Desantis C, Virgo K, et al. Cancer treatment and survivorship statistics, 2012. CA Cancer J Clin. 2012;62:220–41.
Khatcheressian JL, Wolff AC, Smith TJ, et al. American Society of Clinical Oncology 2006 update of the breast cancer follow-up and management guidelines in the adjuvant setting. J Clin Oncol. 2006;24:5091–7.
National Comprehensive Cancer Network. National Comprehensive Cancer Network clinical practice guidelines in oncology: breast cancer. v.2. 2010. http://www.nccn.org/professionals/physician_gls/f_guidelines.asp#site. Accessed 28 July 2010.
Haffty BG, Yang Q, Reiss M, et al. Locoregional relapse and distant metastasis in conservatively managed triple negative early-stage breast cancer. J Clin Oncol. 2006;24:5652–7.
Kyndi M, Sorensen FB, Knudsen H, Overgaard M, Nielsen HM, Overgaard J. Estrogen receptor, progesterone receptor, HER-2, and response to postmastectomy radiotherapy in high-risk breast cancer: the Danish Breast Cancer Cooperative Group. J Clin Oncol. 2008;26:1419–26.
Lowery AJ, Kell MR, Glynn RW, Kerin MJ, Sweeney KJ. Locoregional recurrence after breast cancer surgery: a systematic review by receptor phenotype. Breast Cancer Res Treat. 2012;133:831–41.
Millar EK, Graham PH, O’Toole SA, et al. Prediction of local recurrence, distant metastases, and death after breast-conserving therapy in early-stage invasive breast cancer using a five-biomarker panel. J Clin Oncol. 2009;27:4701–8.
Nguyen PL, Taghian AG, Katz MS, et al. Breast cancer subtype approximated by estrogen receptor, progesterone receptor, and HER-2 is associated with local and distant recurrence after breast-conserving therapy. J Clin Oncol. 2008;26:2373–8.
Donnelly P, Hiller L, Bathers S, Bowden S, Coleman R. Questioning specialists’ attitudes to breast cancer follow-up in primary care. Ann Oncol. 2007;18:1467–76.
van Hezewijk M, Hille ET, Scholten AN, Marijnen CA, Stiggelbout AM, van de Velde CJ. Professionals’ opinion on follow-up in breast cancer patients; perceived purpose and influence of patients’ risk factors. Eur J Surg Oncol. 2011;37:217–24.
Watson EK, Sugden EM, Rose PW. Views of primary care physicians and oncologists on cancer follow-up initiatives in primary care: an online survey. J Cancer Surviv. 2010;4:159–66.
Greenblatt DY, Weber SM, O’Connor ES, LoConte NK, Liou JI, Smith MA. Readmission after colectomy for cancer predicts one-year mortality. Ann Surg. 2010;251:659–69.
O’Connor ES, Greenblatt DY, LoConte NK, et al. Adjuvant chemotherapy for stage II colon cancer with poor prognostic features. J Clin Oncol. 2011;29:3381–8.
Weiss JM, Pfau PR, O’Connor ES, et al. Mortality by stage for right- versus left-sided colon cancer: analysis of surveillance, epidemiology, and end results—Medicare data. J Clin Oncol. 2011;29:4401–9.
Potosky AL, Riley GF, Lubitz JD, Mentnech RM, Kessler LG. Potential for cancer related health services research using a linked Medicare-tumor registry database. Med Care. 1993;31:732–48.
Warren JL, Klabunde CN, Schrag D, Bach PB, Riley GF. Overview of the SEER-Medicare data: content, research applications, and generalizability to the United States elderly population. Med Care. 2002;40(8 Suppl):IV-3–18.
Keating NL, Landrum MB, Guadagnoli E, Winer EP, Ayanian JZ. Factors related to underuse of surveillance mammography among breast cancer survivors. J Clin Oncol. 2006;24:85–94.
Lamont EB, Herndon JE 2nd, Weeks JC, et al. Measuring disease-free survival and cancer relapse using Medicare claims from CALGB breast cancer trial participants (companion to 9344). J Natl Cancer Inst. 2006;98:1335–8.
Smith BD, Gross CP, Smith GL, Galusha DH, Bekelman JE, Haffty BG. Effectiveness of radiation therapy for older women with early breast cancer. J Natl Cancer Inst. 2006;98:681–90.
Stokes ME, Thompson D, Montoya EL, Weinstein MC, Winer EP, Earle CC. Ten-year survival and cost following breast cancer recurrence: estimates from SEER–Medicare data. Value Health. 2008;11:213–20.
Pollack LA, Adamache W, Eheman CR, Ryerson AB, Richardson LC. Enhancement of identifying cancer specialists through the linkage of Medicare claims to additional sources of physician specialty. Health Serv Res. 2009;44(2 Pt 1):562–76.
Baldwin LM, Adamache W, Klabunde CN, Kenward K, Dahlman C, L Warren J. Linking physician characteristics and Medicare claims data: issues in data availability, quality, and measurement. Med Care. 2002;40(8 Suppl):IV-82–95.
Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–9.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Greene FL, Page DL, Balch CM, Fleming ID, Fritz AG. AJCC cancer staging manual. 6th ed. New York: Springer, 2002.
Murphy CC, Bartholomew LK, Carpentier MY, Bluethmann SM, Vernon SW. Adherence to adjuvant hormonal therapy among breast cancer survivors in clinical practice: a systematic review. Breast Cancer Res Treat. 2012;134:459–78.
Howlader N, Noone AM, Krapcho M, et al. SEER cancer statistics review, 1975–2008. Bethesda, MD: National Cancer Institute.
Acknowledgment
This project was funded under Contract No. HHSA290201000006I from the Agency for Healthcare Research and Quality (AHRQ) as part of the Developing Evidence to Inform Decisions about Effectiveness (DEcIDE) program. Further funding came from a Clinical Scholar Award from the Society of University Surgeons; an investigator-initiated pilot grant from the University of Wisconsin Carbone Cancer Center; Grant number P30 CA014520 from the National Cancer Institute with support to the University of Wisconsin Carbone Comprehensive Cancer Center (UWCCC); as well as the Health Innovation Program, the Community-Academic Partnerships core of the University of Wisconsin Institute for Clinical and Translational Research [Grant number UL1TR0000427 from the Clinical and Translational Science Award program of the National Center for Research Resources, NIH National Center for Advancing Translational Sciences (NCATS)] and the UW School of Medicine and Public Health from The Wisconsin Partnership Program. This study used the linked SEER-Medicare database. The interpretation and reporting of these data are the sole responsibility of the authors. The authors acknowledge the efforts of the Applied Research Program, NCI; the Office of Research, Development and Information, CMS; Information Management Services (IMS), Inc.; and the Surveillance, Epidemiology, and End Results (SEER) Program tumor registries in the creation of the SEER-Medicare database. The collection of the California cancer incidence data used in this study was supported by the California Department of Public Health as part of the statewide cancer reporting program mandated by California Health and Safety Code Section 103885; the National Cancer Institute's Surveillance, Epidemiology and End Results Program under contract N01-PC-35136 awarded to the Northern California Cancer Center, contract N01-PC-35139 awarded to the University of Southern California, and contract N02-PC-15105 awarded to the Public Health Institute; and the Centers for Disease Control and Prevention's National Program of Cancer Registries, under agreement #U55/CCR921930-02 awarded to the Public Health Institute. The ideas and opinions expressed herein are those of the author(s) and endorsement by the State of California, Department of Public Health the National Cancer Institute, and the Centers for Disease Control and Prevention or their Contractors and Subcontractors is not intended nor should be inferred.
Disclosure
The authors declare no conflict of interest. The authors of this report are responsible for its content. Statements in the report should not be construed as endorsement by the Agency for Healthcare Research and Quality, the U.S. Department of Health and Human Services, or the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Appendix
Rights and permissions
About this article
Cite this article
Neuman, H.B., Weiss, J.M., Schrag, D. et al. Patient Demographic and Tumor Characteristics Influencing Oncologist Follow-Up Frequency in Older Breast Cancer Survivors. Ann Surg Oncol 20, 4128–4136 (2013). https://doi.org/10.1245/s10434-013-3170-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-013-3170-8