Abstract
Background
A herbal medicinal product (HMP) with centaury, lovage, and rosemary as active ingredients (brand name: Canephron® N) has been widely used for treatment and prevention of urinary tract infections (UTIs) and other urinary system disorders. Non-clinical in vitro and in vivo data indicate its diuretic, spasmolytic, anti-inflammatory, antioxidative and analgesic effects. The purpose of this non-interventional, prospective, multicenter study was to collect data on the use of the HMP in the Russian pediatric outpatient population.
Results
In total, 636 outpatients aged 1–17 years were enrolled. Of these, 634 received at least one dose of the HMP and were included in the safety set, which was used for analysis. 61 patients were 12–23 months, 227 were 2–5 years, 234 were 6–11 years and 112 were 12–17 years of age. The oral solution of the HMP was prescribed in 66.4%, and tablets (dragées) in 33.6% of the patients. For 48% of the patients the HMP was prescribed to treat an acute or chronic disease, 25% of the patients received it for prophylaxis, and 27% for both. More than half of the patients (53%) received the HMP as monotherapy.
Main treatment indications were UTIs (34.1%) and pyelonephritis (30.0%). The proportion of UTIs was the highest within the youngest age group (51%), while the proportion of different cystitis forms increased in patients older than 2 years. Relevant proportions of different nephritis forms and urolithiasis were only observed in patients aged 12–17 years. Forms of cystitis were more frequent in female than in male patients (15% vs. 1%), while forms of nephritis, urolithiasis, and dysmetabolic nephropathy / crystalluria were more frequent in male patients.
At the end of the observational period, 20% of the patients were reported as recovered from their disease, and 65% were reported to show improvements. For 91% of all patients with HMP monotherapy the investigators evaluated the effectiveness of the HMP as ‘good’ or ‘very good’. Nearly all patients (99%) evaluated the tolerability as ‘good‘or ‘very good‘. Five adverse drug reactions were observed.
Conclusions
The treatment of children aged 1–17 years with the HMP is safe and well tolerated. The study results support the use of the HMP for treatment and prophylaxis of urinary system diseases.
Similar content being viewed by others
Background
Urinary system diseases in pediatric practice comprise a broad spectrum of various pathological disorders. The most common urinary system disease in children and adolescents is a urinary tract infection (UTI), which is also one of the most frequent pediatric infections in general. The clinical manifestations of UTIs vary from general signs (e.g. fever, vomiting, refusing food, irritability) to specific urinary manifestations (e.g. frequent urination, pain and burning during urination, urinary incontinence) [1, 2]. UTIs, primarily pyelonephritis, may result in kidney damage with long-term complications such as hypertension, impaired renal function, and end-stage chronic kidney diseases. Timely diagnosis and effective treatment of UTIs may prevent severe disorders and long-term complications in patients with recurrent infections [1, 2].
In Russian pediatric practice, routine treatment of UTIs involves administration of antimicrobial agents and different herbal products, one of them is a herbal medicinal product (HMP) with centaury herb, lovage root, and rosemary leaves as active ingredients (brand name: Canephron® N, manufacturer: Bionorica SE, Germany). During many years, this HMP has been widely used for treatment and prevention of UTIs as well as other urinary system disorders. The HMP was shown to be effective in the treatment and prophylaxis of UTIs both in adults and children [3].
Centaury herb contains xanthones with antibacterial and anticholinergic effects [4, 5]. It is traditionally used to support expulsion of kidney stones and for diuresis [6,7,8,9]. Lovage root with its furanocoumarines is proven to have spasmolytic and diuretic effects [10, 11] and is used for irrigation therapy of lower urinary tract inflammation [10, 12]. Diterpenes, polyphenols and phenols from rosemary leaves have antioxidative, antibacterial, antiviral, anti-inflammatory, spasmolytic and anticonvulsant effects [13, 14]. Rosemary leaves are supportive for renal excretion and diuresis [8, 15,16,17,18]. Diuretic activity was shown to be increased by all components of the HMP [19, 20]. Anti-inflammatory, analgesic and antioxidative mechanisms of the active pharmaceutical ingredients (APIs) of the HMP, i.e. the mixture of pulverized centaury herb, rosemary leaves and lovage root, involve reduction of prostaglandin E2 release and inhibition of PGE2-producing enzymes [21,22,23]. It reduces the physiologically relevant reactive oxygen and nitrogen species, hydroxyl radicals, peroxyl radicals and peroxynitrite [22]. Spasmolytic and antinociceptive properties have been investigated in an animal model of cyclophosphamide-induced cystitis. Here the API of the HMP was shown to reduce the contraction frequency and to normalize bladder capacity [24] and to normalize cyclophosphamide-induced hyperalgesia [22]. The API of the HMP concentration-dependently inhibited the adhesion of E. coli to bladder cells [24], supporting its beneficial effects in bacterial urinary tract infections.
Consequently, the primary pharmacodynamic properties of the HMP related to the indication comprise anti-inflammatory / anti-oxidative activity, spasmolytic activity, antinociceptive activity, anti-adhesive activity, and diuretic activity [3, 21, 23]. Placebo-controlled studies on the clinical efficacy of the HMP have not been carried out yet.
Intestinal dysbiosis has been shown to be a risk factor for pyelonephritis recurrence. Normalization of the microbial environment by means of pre- and probiotic preparations together with the HMP is a promising approach for pyelonephritis recurrence prevention [25]. Also with respect to uncomplicated UTIs, the preservation of the beneficial microbial flora has been focused recently, and use of anti-inflammatory instead of antibacterial approaches has been discussed [26]. In an open-label, non-randomized clinical trial with 125 female patients with uncomplicated UTI, the HMP demonstrated significant improvement of all symptoms and antibiotics were only required in 2% of the patients [27]. Prophylactic administration of the HMP in children undergoing surgical correction of vesicoureteral reflux improved clinical outcomes [28]. Study results support its use as add-on in therapy after urinary stone lithotripsy and it may also have had a positive effect on prevention of urolithiasis [29, 30]. Pregnant women showed earlier relief of symptoms and normalization of pyuria on additional treatment with the herbal combination [3].
The HMP has a favorable safety profile and good tolerability as compared with other medications for urinary disease treatment, e.g. antibiotics, nitrofurans [3]. It is available as coated tabletsFootnote 1 (dragées) and oral solution allowing its safe and adequate dosing even in very small children. However, large-scale data on prescription profile, effectiveness and safety of the HMP in the Russian pediatric population with various urinary system diseases in a real-life setting were missing.
The current non-interventional study (NIS) was planned to provide unique data on the clinical use, the effectiveness and safety of the HMP in Russian pediatric outpatients with urinary system diseases in routine practice. The study results could contribute to the optimization of management of urinary system diseases in children.
Methods
Study design and procedures
The purpose of this non-interventional, prospective, multicenter study was to collect data on the use of the HMP in the Russian pediatric outpatient population. The NIS was conducted in compliance with the Declaration of Helsinki, the Guidelines for Good Pharmacoepidemiology Practice [31], all applicable norms of Good Clinical Practice (ICH-GCP) and the Russian national GCP standard. The NIS was approved by the local ethics committees and conducted with site monitoring by a contract research organization (CRO) authorized by the study sponsor. The monitoring plan included 100% source data verification for Informed Consent Forms, adverse events (AE) and serious adverse events (SAE). Further, 100% data verification was planned for the first two patients per site to identify documentation issues and train the study site, if necessary, to receive accurate and robust data. To ensure patient safety as well as correct patient selection, in- and exclusion criteria were verified for the first five patients per site.
The NIS was carried out at 26 polyclinics and outpatient departments in different regions of Russia. All physicians were specialists, e.g. pediatricians, pediatric nephrologists and pediatric urologists. Participants were pediatric outpatients from 1 to 17 years of age with a verified diagnosis of urinary system disease who were prescribed treatment with the HMP. Exclusion criteria comprised contraindications from the product information (hypersensitivity to any components of the HMP, gastric ulcer and duodenal ulcer in the acute phase) and participation in a clinical trial simultaneously or during three months before enrolment. Only patients, whose parents and/or legally acceptable representatives provided written informed consent to the participation in the study were enrolled. Patients at the age of 14 to 17 years were required to sign a written assent form in addition.
The treating physician had to prescribe the HMP in accordance with the Russian product information on the HMP (Instruction for the use of the product for the medicinal use; oral solution or tablets) to eligible patients. Correspondingly, the HMP is used for “complex therapy in the treatment of chronic infections of the bladder (cystitis) and the kidneys (pyelonephritis), non-infectious chronic inflammation of the kidneys (glomerulonephritis, interstitial nephritis), and for prevention of urinary stone formation (also after urinary stone removal)”. The dosing recommendations for school age children are 25 drops or 1 tablet 3 times a day, and 15 drops 3 times a day for preschool age children. After decreasing of acuity of disease it is recommended to continue the treatment with preparation for 2–4 weeks. All information on special warnings, contraindications, etc. could be taken from the product information and was presented in the study observational plan. In line with the product information, there were no restrictions for concomitant therapies.
Treatment duration was at the discretion of the treating physician according to the individual patient’s clinical picture of the disease. The duration could vary from a few days to several weeks or months. Patients could have been treated with the HMP before enrolment into the NIS. In this case, they were included into the safety set used for analysis only if they had taken at least one dose of the HMP during the NIS.
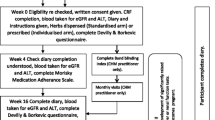
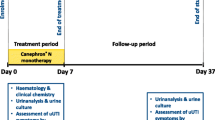
The observational period included the study treatment phase and a follow-up period and was limited to a maximum of six weeks. Data were collected at baseline, after two weeks, and after six weeks of treatment during routine patient visits to physicians or during phone calls (Fig. 1). Any special data collection procedures were not stipulated within the framework of this NIS.
The following key parameters were assessed: indications the HMP was prescribed for, the prescribed product forms, the prescribed treatment regimen, the prescribed and the actual treatment durations, the type of prescribed use (prophylactic, treatment or both), and concomitant medications including non-drug therapy. Treatment regimen was defined as the number and percentage of patients who received different daily doses and frequency of administration. The reported indications were coded by a CRO data manager using MedDRA dictionary version 19.0 [32]. Concomitant medications were medications, which had not been stopped before study start, and were coded using WHO DDE dictionary version dated as of 1 June 2016. Based on the actual and prescribed treatment duration, patient compliance was calculated (Compliance (%) = actual duration (days) / prescribed duration (days)*100%).
The HMP’s overall effectiveness and tolerability were assessed by physicians and by patients/parents using a 5-point verbal rating scale. Urinary symptoms and urinary disease outcomes (complete recovery, improvement, without changes, deterioration, and relapse) were also documented. Study variables which are not reported here were treatment for urinary disease within two weeks prior to study entry, non-drug therapy, and vital signs.
Assessment of safety comprised the documentation of all AEs, treatment-emergent AEs, adverse drug reactions (ADRs), treatment-emergent ADRs, SAEs, and serious ADRs. AEs and ADRs were coded according to MedDRA dictionary version 19.0. An ADR was an AE reported to be related to the HMP, as assessed by the physicians. Treatment-emergent AEs and ADRs are presented. Treatment-emergent means that those events were not present before the start of treatment or worsened in severity following the start of treatment.
Subgroups
Subgroup analyses were performed by age category, by use of concomitant medication (monotherapy vs. combination therapy), and by indication. Age categories were defined as follows: small children (12–23 months), pre-school age (2–5 years), early school age (6–11 years), teens (12–17 years). HMP monotherapy included all patients who had taken the HMP without any additional concomitant medication during the NIS. If a patient received any medication together with the HMP for urinary system disease treatment, he or she was included in the combination subgroup. For analysis by indication, it was planned to group the reported indications. The indication groups were defined upon the list of the most frequent indications as documented in the case report form (CRF). The final number of indication groups was limited to six.
Statistical analysis
Study data were analyzed descriptively. Statistics included summary tables (continuous variables: n, mean, median, standard deviation, minimum and maximum; categorical values: n, frequency and percentage). Proportion was assessed together with 95% confidence interval, if applicable. All analyses were performed with SAS® version 9.3.
Results
From September 2015 to June 2016, 636 children were enrolled at 26 sites. Of these, 620 patients completed the study per protocol (Table 1), 16 patients prematurely discontinued due to AEs (n = 8), loss to follow-up (n = 5), and other reasons (n = 3). In total, 634 patients (99.7% of all enrolled patients) received at least one dose of the HMP and were included in the safety set, which was used for analysis (percentages refer to the safety set unless otherwise noted). A subset of 37 patients had already started treatment with the HMP before enrolment in the NIS. Patient characteristics are summarized in Table 2.
The oral solution of the HMP was prescribed in 66.4% of the enrolled patients, and tablets were prescribed in 33.6% of the enrolled patients. For most of the children less than six years of age the solution was prescribed (Table 2). No difference in gender distribution between solution and tablets was observed.
The majority of the patients (98.3%) took the HMP three times per day. In 48% of the patients the HMP was prescribed for treatment of an acute or chronic disease, 25% of the patients received the HMP for prophylaxis, and for 27% of the patients the HMP was prescribed for both prophylaxis and treatment. Distribution of patients who took solution or tablets was similar.
In 75.2% of all patients the HMP was prescribed for indications coded in the System Organ Class (SOC) ‘Infections and infestations’. Within this SOC, UTIs (34.1%) and pyelonephritis (30.0%) were the most frequent indications. For 36% of the patients, indications from the SOC ‘Renal and urinary disorders’ were documented as reason for treatment with the HMP (Table 3). In some cases the HMP was used in unlabeled indications like neurogenic bladder, hydronephrosis, and hypotonic urinary bladder. In rare cases (1.6%) the HMP was prescribed for indications within the SOC ‘Congenital, familial and genetic disorders’.
Patients were distributed as follows into six indication groups for further analysis (Table 4): group of unspecified UTIs (216 patients), group ‘pyelonephritis’ (190 patients), dysmetabolic nephropathy / crystalluria (120 patients), group ‘cystitis’ (73 patients), urolithiasis (26 patients), and group ‘nephritis’ (23 patients). Of the 120 patients with dysmetabolic nephropathy / crystalluria, 106 patients (88%) had hyperoxaluria, and 31 patients (26%) had hypercalciuria (a patient could have more than one diagnosis – 120 patients had 150 diagnoses).
The proportion of UTIs was the highest within the youngest age group (51%) and decreased in the older patients while the proportion of indications of the group ‘cystitis’ increased in patients older than 2 years. Relevant proportions of urolithiasis and indications of the group ‘nephritis’ were only observed in patients aged 12 to 17 years (Fig. 2). Indications of the group ‘cystitis’ were more frequent in female than in male patients (15% vs. 1%), while indications of the group ‘nephritis’, urolithiasis, and dysmetabolic nephropathy / crystalluria were more frequent in male patients (Fig. 3).
392 patients (61.8%) have received concomitant medication at any time point of the observation, i.e. not necessarily at the same time as the HMP treatment. 377 of these patients have received the concomitant medication together with HMP and were thus classified as patients with combination therapy, and 257 were monotherapy patients. Monotherapy patients are patients who may have received concomitant medication but not at the same time as the HMP treatment or who had no concomitant medication at all. 22% of the patients received one combination medication, 16% received two combination medications, and 9% received three or more combination medications. The indication group with the highest proportion of patients receiving combination therapy was ‘nephritis’ (65%, Fig. 4). The highest proportions of the monotherapy use were observed for dysmetabolic nephropathy / crystalluria (61%), urolithiasis (58%) and urinary tract infections as well as ‘cystitis’ (51% each) (Fig. 4).
The prescribed duration of HMP intake varied from 7 to 84 days. On average, the HMP was taken approximately two days longer than prescribed by the investigators, resulting in a compliance rate of 106.3 ± 23.6%, without notable differences between dosage forms and indication groups. Mean treatment duration was the shortest for UTIs and the longest for indications of the group ‘nephritis’ (Fig. 5). The actual treatment duration of HMP intake was 30.6 days in patients with monotherapy, and with 32.5 days slightly longer if the HMP was taken in combination with other treatment. Treatment duration did not differ between patients who received for prophylaxis, treatment or both. After six weeks of treatment, reduction of urinary symptoms (e.g. skin pallor, frequency and portion changes of urination, urine macroscopic changes) was reported in the majority of study patients. Analysis of urinary disease outcomes at the end of the observational period, revealed that the disease was unresolved in less than 4% of all enrolled patients. 20% of the patients were reported as recovered from their disease by the end of the study and 65% were reported to show improvements. 13% reported no changes, while 1% reported a deterioration or relapse (each). The highest recovery rate was shown for UTIs (37.4%). In total, there were 10% more patients who rated ‘recovered’ at the end of study than at Visit 2 and 5% less ‘without changes’ assessments at the end of study than at Visit 2, while the rate of subjects with deterioration and relapse did not change (Fig. 6).
For 88% and 91% of all patients with HMP monotherapy the investigators evaluated the effectiveness of the HMP as ‘good’ or ‘very good’ at visit 2 (week 2) and at the end of the study, respectively. The proportion of an evaluation of the effectiveness as ‘very good’ increased during the observational period (Figs. 7 and 8). No differences were observed between monotherapy and combination therapy. Patients rated the effectiveness similarly to the investigators.
99% of patients evaluated the tolerability as ‚good‘ or ‘very good‘ at the end of the study. In all age groups, the proportions of the ratings ‘good’ and ‘very good’ were similarly high (Fig. 9). 96 adverse events (AE) were reported in 82 (12.9%) patients during the observational period, whereby ‘infections and infestations’ (55 patients) and ‘renal and urinary disorders’ (11) were most frequently documented. The most frequent AEs by preferred term were ‘respiratory tract infection viral’ (15 patients), ‘nasopharyngitis’ (7), ‘cystitis’ (5), and ‘respiratory tract infection’ (5). All other AEs were reported in ≤4 patients. Most AEs were of mild intensity (67 patients). Severe AEs did not occur.
Adverse drug reactions (ADRs) were only reported in 5 patients: 3 patients had ‘dermatitis allergic’, 1 ‘patient dyspepsia’, and 1 ‘renal colic’. 4 of these patients belonged to the combination therapy group and only 1 patient (‘dermatitis allergic’) to the monotherapy group. One ADR (‘renal colic’) in the combination therapy group was assessed as serious. The renal colic resulted in the departure of the renal calculus.
Only 8 (1.3%) patients prematurely withdrew the NIS because of AEs/ADRs (monotherapy: 3, combination therapy: 5), including 3 patients with dermatitis and 1 patient each with functional GI-disorders, vomiting, pyelonephritis, UTI, and renal colic (Table 5).
Discussion
Phytotherapeutics, including the HMP investigated in the present study, are widely used in routine practice for the treatment and prophylaxis of different urinary system diseases in the pediatric population in Russia [33]. However, placebo-controlled studies on the efficacy of the HMP have not been performed yet. Since the present study was non-interventional, the treating physicians had to prescribe the HMP in accordance with the product information approved in the Russian Federation. However, the use of the HMP was not limited to any indications. The present results therefore reflect real-life practice in pediatric patients. They can contribute to the optimization of disease management in children with urinary system diseases and to the improvement of outcomes of these frequent disorders.
Smaller children of less than six years of age mostly were prescribed the solution, which corresponds to the approved product information, where tablets (dragées) are only indicated for children aged six years or older. The predominance of female patients in the observed population reflects the known gender differences in UTIs. Reported incidence rates in girls are two to four-fold higher than in boys [34]. In most patients, the HMP was administered for treatment or prophylaxis of UTIs, pyelonephritis and cystitis. Of note, clinical diagnosis terms (terms used by investigators in source documentation) are not identical to MedDRA preferred terms. For instance, the term ‘urinary tract infection’ according to MedDRA coding does not include cystitis and pyelonephritis forms, which are coded separately. The HMP was used in routine pediatric practice for a broad spectrum of indications including off-label use. Untypical indications like neurogenic bladder, hydronephrosis, or hypotonic urinary bladder demonstrate the variety of use of the HMP. Dysmetabolic nephropathy or crystalluria was reported as indication for treatment with the HMP in 120 cases. In fact, “dysmetabolic nephropathy” is a specific term used by Russian pediatricians. Dysmetabolic nephropathies are comprehended as a large group of nephropathies with different etiology which are associated to metabolic disorders and prominent crystalluria [35]. Since dysmetabolic nephropathy is missing in the ICD and MedDRA coding systems, for the purpose of coding, a special study specific approach was taken at the data management phase of the study and all physicians were queried about the type of crystalluria they met in each concerned patient with dysmetabolic nephropathy.
The benefits and the good tolerability of the HMP in the treatment and prophylaxis of urinary diseases were demonstrated in children of 1 to 17 years of age. Urinary symptoms were reduced and the majority of patients had recovered from their disease or showed improvements. For some chronic diseases like urolithiasis or chronic pyelonephritis, recovery is a hardly expected outcome during relatively short time treatment and this was a reason for a portion of patients with poor outcomes (‘without changes’, ‘deterioration’, ‘relapse’) at the end of the observation. For almost all patients, the effectiveness was rated to be good or very good at the end of the study. These results are in line with previous studies in adult and children previously reviewed by Naber et al., who evaluated 17 studies. Naber et al. concluded that the HMP positively affects infections and inflammation in the urinary tract, supports elimination of small calcium oxalate stones, and might prevent lithogenesis [3]. In a further comparative study in 86 children with recurrent pyelonephritis, the HMP in combination with standard antimicrobial therapy resulted in complete remission in 61% of the patients. The study showed that the antimicrobial course for the anti-relapse treatment of pyelonephritis may be shortened and thus, the side effects of antibacterial drugs could be reduced [36]. The results were in line with another study with 26 preschool age children with pyelonephritis. There, in comparison with historical controls of pediatric patients without HMP treatment, HMP use improved therapeutic results with respect to general condition, pain, dysuric symptoms and body temperature [37]. A combination therapy with the HMP in pediatric pyelonephritis is capable of improving microalbuminuria, which is an early sign of renal parenchyma damage [38].
The HMP was used as monotherapy in about half of the patients with cystitis. According to a previous clinical study in adult patients with uncomplicated lower UTIs (cystitis), it could be shown in both studies that the HMP monotherapy is sufficient for the treatment of uncomplicated UTIs and additional use of antibiotics is not necessary in most of the cases [27].
The use of the HMP is very flexible and duration can be adapted at the discretion of the physician. In the present study, treatment durations varied from a few days to several weeks, depending on the patient’s individual requirements. A 100% compliance rate towards the prescribed treatment duration was reached for both dosage forms and all indication groups, which might be a result of the good tolerability of the HMP; 99% of the patients rated the tolerability to be good or very good; only eight patients discontinued from the study due to adverse events. The good safety profile has been consistently reported from previous studies [3]. The most common adverse drug reactions as summarized by the product information comprise disorders of the gastrointestinal tract, e.g. nausea, vomiting or diarrhea, and allergic reactions.
Conclusions
Based on the present data, it can be concluded that treatment of children aged 1 to 17 years with the HMP is safe and well tolerated. The medication can be effectively used for the treatment of urinary system diseases. Clinical trials would help to better understand the benefit of the HMP in selected populations with respect to clinical outcomes in relevant indications.
Notes
Registration of Canephron® N differs between countries with respect to indications and naming of the dosage forms.
Abbreviations
- ADR:
-
Adverse drug reaction
- AE:
-
Adverse event
- API:
-
Active pharmaceutical ingredient
- CRF:
-
Case report form
- CRO:
-
Contract research organization
- GCP:
-
Good clinical practice
- HMP:
-
Herbal medicinal product
- ICH:
-
International conference on harmonization
- LLT:
-
Lowest Level Term
- MedDRA:
-
Medical Dictionary for Regulatory Activities
- N:
-
Number of patients in the population or subset or with available data
- n:
-
Number of patients with event
- NIS:
-
Non-interventional study
- PGE2 :
-
Prostaglandin E2
- SAE:
-
Serious adverse event
- SD:
-
Standard deviation
- SOC:
-
System organ class
- UTI:
-
Urinary tract infection
- WHO DDE:
-
World Health Organization Drug Dictionary Enhanced
References
Zelikovic I, Adelman RD, Nancarrow PA. Urinary tract infections in children. An update. West J Med. 1992;157:554–61.
Stein R, Dogan HS, Hoebeke P, Kocvara R, Nijman RJ, Radmayr C, et al. Urinary tract infections in children: EAU/ESPU guidelines. Eur Urol. 2015;67:546–58.
Naber KG. Efficacy and safety of the phytotherapeutic drug Canephron(R) N in prevention and treatment of urogenital and gestational disease: review of clinical experience in Eastern Europe and Central Asia. Res Rep Urol. 2013;5:39–46.
EMA, HMPC. European herbal monograph on Centaurium erythraea rafn, herba. EMA/HMPC/277493/2015. 2015. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/Herbal_-_Herbal_monograph/2016/01/WC500200308.pdf. Accessed 27 Feb 2018.
European Scientific Cooperative on Phytotherapy (ESCOP). Centaurii herba (Centaury herb). In: ESCOP Monographs. 2nd ed. Stuttgart-New York: Thieme Verlag; 2003. p. 70–3.
Blaschek W, Ebel S, Hackenthal E, Holzgrabe U, Keller K, Reichling J, Schulz V. Centaurium. In: Hager Handbook. 6th ed. Stuttgart: Wissenschaftliche Verlagsgesellschaft mbH; 2007. p. 159–68.
Claisse R. Drogues de la Pharmacopée traditionelle de la ragion de Rabat-Salé. In: Plantes médicinales et phytothérapie, vol. XXIII; 1989. p. 315–31.
Fournier. Centaurée Jaune. In: Le livre des Plantés Medicinales et Vénéneuses de France; 1947. p. 324–7.
EMA. Assessment report on Centaurium erythraea Rafn. s.l., herba, EMA/HMPC/277491/2015. 2016. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/Herbal_-_HMPC_assessment_report/2016/01/WC500200306.pdf. Accessed 27 Feb 2018.
German Commission E monograph for Levistici radix. Bundesanzeiger No.101; 1990.
Willuhn G. Levistici radix, Liebstöckelwurzel. In: Teedrogen. 4th ed. Stuttgart: Wiss. Verlagsgesellschaft; 2002. p. 335–7.
EMA. Assessment report on Levisticum officinale Koch, radix, EMA/HMPC/524623/2011. 2011. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/Herbal_-_HMPC_assessment_report/2013/02/WC500139223.pdf. Accessed 27 Feb 2018.
EMA, HMPC. Community herbal monograph on Rosmarinus officinalis L., folium. EMA/HMPC/13633/2009. 2009. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/Herbal_-_Community_herbal_monograph/2009/12/WC500018299.pdf. Accessed 27 Feb 2018.
European Scientific Cooperative on Phytotherapy (ESCOP). Rosmarini folium (Rosemary leaf). In: ESCOP Monographs. 2nd ed. Stuttgart-New York: Thieme Verlag; 2003. p. 429–36.
AWMF. S3 Guideline (S3-Leitlinie), AWMF-Register-Nr. 043/044: Epidemiologie, Diagnostik, Therapie und Management unkomplizierter bakterieller ambulant erworbener Harnwegsinfektionen bei erwachsenen Patienten. 2017. Available from: https://www.awmf.org/uploads/tx_szleitlinien/043-044l_S3_Harnwegsinfektionen_2017-05.pdf. Accessed 27 Feb 2018.
British Herbal Medicines Association. Rosmarinus. In: British Pharmacopoeia; 1983. p. 180–1.
Fluck. Romarin. In: Petit Guide panoramique des Herbes Médicinales. p. 1973–124.
EMA. Assessment report on Rosmarinus officinalis L., aetheroleum and Rosmarinus officinalis L., folium, EMA/HMPC/13631/2009. 2011. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/Herbal_-_HMPC_assessment_report/2011/02/WC500101693.pdf. Accessed 27 Feb 2018.
Yarnell E. Botanical medicines for the urinary tract. World J Urol. 2002;20:285–93.
Haloui M, Louedec L, Michel JB, Lyoussi B. Experimental diuretic effects of Rosmarinus officinalis and Centaurium erythraea. J Ethnopharmacol. 2000;71:465–72.
Nausch B, Koeberle A, Werz O, Ammendola A, Künstle G. Canephron® N reduces pain in experimental cystitis and prostatitis putatively by inhibition of PGE2 production. Eur Urol Suppl. 2016;15:e262.
Nausch B, Künstle G, Mönch B, Koeberle A, Werz O, Haunschild J. Canephron® N alleviates pain in experimental cystitis and inhibits reactive oxygen/nitrogen species as well as microsomal prostaglandin E2 synthase-1. Der Urologe. 2015;54:28.
Nausch B, Röhrl J, Koeberle A, Harler U, Joannidis M, Werz O, et al. Canephron N reduced immune cell recruitment in experimental cystitis. Eur Urol Suppl. 2017;16:e230–1.
Künstle G, Brenneis C, Haunschild J. Efficacy of Canephron® N against bacterial adhesion, inflammation and bladder hyperactivity. In: 28th European Association of Urology Congress; 2013.
Vialkova AA, Gritsenko VA, Zorin IV, Gordienko LM. On the treatment and prevention of recurrent urinary tract infection in children. Rossiyskiy Vestnik Perinatologii i Pediatrii (Russian Bulletin of Perinatology and Pediatrics). 2010;55(6):77-80.
Naber KG, Kogan M, Wagenlehner FME, Siener R, Gessner A. How the microbiome is influenced by the therapy of urological diseases: standard versus alternative approaches. Clin Phytoscience. 2017;3:8.
Ivanov D, Abramov-Sommariva D, Moritz K, Eskötter H, Kostinenko T, Martynyuk L, et al. An open label, non-controlled, multicentre, interventional trial to investigate the safety and efficacy of Canephron® N in the management of uncomplicated urinary tract infections (uUTIs). Clin Phytoscience. 2015;1:7.
Kirillov VI, Runenko VI, Bogdanova NA, Mstislavskaya SA. Effect of complex therapy on the kidneys of children with vesicoureteral reflux in the postoperative period. Questions Modern Pediatrics. 2007;6:36–42.
Alyaev UG, Amosov AV, Grigoryan VA, Sultanova EA, Krupinov GE, Akopyan GN. The possibilities of using Canephron® N for the treatment and prevention of urolithiasis. Russian Med J. 2007;12:1023-8.
Ceban A. Efficacy of a fixed combination of Centaurii herba, Levistici radix and Rosmarini folium in urinary lithiasis. Results of an open randomised cohort study. Z Phytotherapy. 2012;33:19–23.
Guidelines for Good Pharmacoepidemiology Practices (GPP). 2007. Available from: www.pharmacoepi.org/resources/guidelines_08027.cfm. Accessed 29 Dec 2017.
MedDRA. Introductory Guide MedDRA Version 19.0. 2016. Available from: https://www.meddra.org/sites/default/files/guidance/file/intguide_19_0_english.pdf. Accessed 29 Dec 2017.
Mamaeva MA. The Role of Phytomedications in Complex Therapy of Urinal Infections in Children. Issues of modern pediatrics: Scientific and Practical Journal of the Union of Pediatricians of Russia. 2008;7:101–4.
Kwok WY, de Kwaadsteniet MC, Harmsen M, van Suijlekom-Smit LW, Schellevis FG, van der Wouden JC. Incidence rates and management of urinary tract infections among children in Dutch general practice: results from a nation-wide registration study. BMC Pediatr. 2006;6:10.
Dlin VV, Shatokhina OV, Osmanov IM, Yurieva EA. Canephron N Effectiveness in Children with Dysmetabolic Nephropathy with Oxalate-Calcium Crystalluria. Bull Pediatric Pharmacol Nutriciol. 2008;5:66–9.
Kiselnikova OV, Puhova TG. Influence of present-day Phytotherapy on recurrent pyelonephritis in children. Bull Pediatric Pharmacol Nutriciol. 2007;4:64-7.
Kljuchnikov SO, Gadzhialieva MM. Use of herbal drug Canephron in complex therapy of pyelonephritis in children of preschool age. Bull Pediatric Pharmacol Nutriciol. 2007;4:51-4.
Nezhdanova MV, Volgayeva YV, Galchina OV. Results of original herbal medicinal product use in combination therapy of pyelonephritis in children. Issues of modern pediatrics: Scientific and Practical Journal of the Union of Pediatricians of Russia. 2010;9:113–6.
Acknowledgements
We gratefully thank all participating clinical sites for their commitment and successful conduct of this study:
Prof. Igor B. Osipov; State budget educational institution of Higher professional education “St. Petersburg State Pediatric Medical University”, Ministry of Health of the Russian Federation.
Dr. Olga V. Kiselnikova; State budget educational institution of Higher professional education “Yaroslavl State Medical University”, Ministry of Health of the Russian Federation.
Prof. Maria K. Soboleva; Medical Center “AVICENNA” CJSC.
Prof. Nataliya N. Martynovich; “Clinic of the Center for molecular diagnostics” LLC.
Dr. Irina F. Vladimirtseva; State Budgetary Healthcare Institution of Samara region “Samara city hospital №6”.
Linar N. Sayapov; State Budgetary Healthcare Institution of Republic of Bashkiria “Children’s polyclinic №3 in Ufa”.
Prof. Lyudmila A. Deryugina; Clinic of Pediatrics of Doctor Trukhmanov «ENT-PLUS» LLC.
Dr. Elena V. Tush; State Budgetary Healthcare Institution of Nizhny Novgorod region “Children’s City Clinical Hospital No. 1 of the Prioksky District of Nizhny Novgorod”.
Marina V. Scherbakova; State Budgetary Healthcare Institution of Ryazan region “Children’s polyclinic №2”.
Elena K. Kushner; Regional State Budgetary Healthcare Institution “Children’s regional clinical hospital”.
Prof. Gulnara R. Sagitova; State Budgetary Healthcare Institution of Astrakhan region “Children’s city polyclinic №3”.
Dr. Ilya M. Kagantsov; State Institution “Republican Children’s Hospital”.
Natalya V. Ushakova; State Budgetary Healthcare Institution“Nizhny Novgorod regional children’s clinical hospital”.
Dr. Natalia F. Shaposhnikova; State budget educational institution of Higher professional education “Volgograd State Medical University”, Ministry of Health of the Russian Federation.
Dr. Anton A. Solovyev; State budget educational institution of Higher professional education “St. Petersburg State Pediatric Medical University”, Ministry of Health of the Russian Federation.
Dr. Elena I. Slobodyan; State Budgetary Healthcare Institution of the Republic of Crimea “Evpatoria City Children’s Clinical Hospital”.
Medical writing support was provided by Karin Eichele (mediwiz).
Funding
This work was supported by a research grant from Bionorica LLC, Moscow, Russia. Medical writing assistance was funded by Bionorica SE, Germany.
Availability of data and materials
Original data will not be shared due to confidentiality reasons.
Author information
Authors and Affiliations
Contributions
VVD has made substantial contributions to the conduct of the presented study as the coordinating investigator, acquisition and interpretation of data. DAS has made substantial contributions to conception and design of the study, has been substantially involved in the interpretation of data and has given final approval of the version to be published. NIA, TLN, SLM, INZ, MVE, GML, TVM have made substantial contributions to the conduct of the presented study and acquisition of data. IIK has made substantial contributions to conception, design, and to the management of the study, and has been involved in drafting the manuscript, revising it critically for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This non-interventional study was conducted in compliance with the Declaration of Helsinki, the Guidelines for Good Pharmacoepidemiology Practices, all applicable norms of Good Clinical Practice (ICH-GCP) and the Russian national GCP standard. The study was approved by the Independent Interdisciplinary Ethics Committee on Ethical Review for Clinical Studies (Moscow) and local ethics committees.
Informed consent process in this study was carried out according to applicable pediatric studies regulations. Only patients, whose parent(s) and legally acceptable representative(s) provided written informed consent, and who provided a written assent form themselves (if aged 14 to 17 years) to participate in the study, were to be enrolled into this study.
Consent for publication
Not applicable.
Competing interests
Dimitri Abramov-Sommariva is an employee of Bionorica SE, Germany. Dr. Ivan Kolchenko is an employee of Bionorica LLC, Russia. Dr. Tea Margieva was a lecturer for Bionorica. Other authors didn’t have any conflict of interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Dlin, V.V., Abramov-Sommariva, D., Zakharova, I.N. et al. A non-interventional, prospective, multicenter study for evaluation of the use of the herbal medicinal product Canephron® N in the pediatric outpatient population in Russia. Clin Phytosci 4, 31 (2018). https://doi.org/10.1186/s40816-018-0092-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40816-018-0092-9