Abstract
Background
Prior reports indicate that intentional coverage of the accessory renal arteries (ARAs) with a diameter larger than 3 mm during endovascular aneurysm repair (EVAR) increases risk of additional treatment for type II endoleak. Here, we report a case of prophylactic coil embolization for a 4 mm ARA originating from an abdominal aortic aneurysm.
Case presentation
A 76-year-old woman was admitted to our hospital after noticing an abdominal pulsatile mass. Computed tomography (CT) imaging revealed an abdominal aortic aneurysm (AAA) with a maximum diameter of 53 mm. Preoperative CT scan showed a right ARA, 4 mm in diameter, which was considered likely to lead to type II endoleak following EVAR. ARA coil embolization was performed at the time of EVAR. We observed no endoleaks and no infarct of the inferior pole of the right kidney on completion angiography. The postoperative course was uneventful, and the patient was discharged 7 days later. Postoperative eGFR (58.4 ml/min) was not significantly different from preoperative level (56.7 ml/min). After EVAR, blood pressure was under control, and no additional anti-hypertensive medicines were required. Postoperative enhanced CT image showed that the distal portion of the ARA was well perfused without type II endoleak from ARA.
Conclusions
Prophylactic coil embolization for a large ARA originating from an abdominal aortic aneurysm appears to be safe and effective in preventing type II endoleak following EVAR.
Similar content being viewed by others
Background
The reported prevalence of accessory renal artery (ARA) is 12 to 49% [1, 2]. Prior reports indicate that kidney function is not affected by ARA coverage during endovascular aneurysm repair (EVAR), though if ARA diameter is larger than 3 mm, additional treatments for type II endoleak are needed [3,4,5,6]. Here, we report a case of prophylactic coil embolization for a 4 mm ARA originating from an abdominal aortic aneurysm.
Case presentation
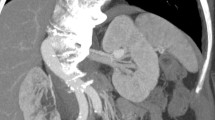
A 76-year-old woman presented at our department with an abdominal pulsatile mass. She had hypertension (nifedipine 20 mg, candesartan 4 mg, indapamide 0.5 mg), dyslipidemia, congestive heart failure, and complete atrioventricular block. She had previously undergone an operation that included endovascular aneurysm repair and prophylactic accessory renal artery coil embolization for advanced uterine cancer. Enhanced computed tomography (CT) imaging revealed an abdominal aortic aneurysm (AAA) with a maximum diameter of 53 × 57 mm and a right ARA (4 mm in diameter) (Fig. 1). Since open repair was considered risky due to her coexisting diseases, we decided to perform EVAR despite the presence of ARA.
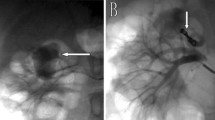
Under general anesthesia, bilateral transfemoral access was obtained via surgical cutdown, and 7Fr short sheaths were placed in both common femoral arteries. Prior to EVAR, the ARA was selectively catheterized with a 6Fr RDC guiding catheter and a 5Fr RDC catheter, and embolization was performed with two 0.018-in coils (Interlock, Boston Scientific, Marlborough, MA, USA). After coiling, the main body of the stentgraft (Aorfix™, Lombard Medical, Oxfordshire, UK) was deployed with its proximal end just below the renal arteries, and bilateral common iliac arteries were used as distal landing zones. We completed the procedures having seen no perfusion defect of the inferior pole of the right kidney from the right renal artery on completion angiography (Fig. 2).
The postoperative course was uneventful, and the patient was discharged 7 days later. Postoperative eGFR (58.4 ml/min) was not significantly different from preoperative (56.7 ml/min). After surgery, blood pressure was under control, and no additional blood pressure medicines were required. Postoperative enhanced CT showed that there was no endoleak. The distal portion of her right ARA from coils including the right kidney was well perfused (Fig. 3).
Discussion
The reported prevalence of ARA ranges from 12 to 49% [1, 2]. The problems most likely to occur during EVAR for AAA with ARA are renal infarction caused by ARA obstruction and type II endoleaks from ARA blood flow. As ARA coverage has been reported to increase risk of renal infarction, with reported rates ranging from 0 to 84%, ARA reconstruction procedures have been devised using fenestrated stentgrafts, branched stentgrafts, or debranching [7,8,9]. Yet some believe that the reconstruction of ARA is unnecessary since it offers no significant benefit in terms of eGFR or blood pressure control [3,4,5,6]. Type II endoleak occurs from the lumbar artery, inferior mesenteric artery (IMA), median sacral artery, and accessory renal artery (ARA). These branches act as inflow or outflow depending on the pressure gradient between the aorta and each branch. When a renal artery is covered with a stentgraft, the pressure on the kidney parenchyma is decreased. Yet covering the ARA while leaving the renal artery uncovered would result in high pressure, and the ARA would act as inflow. Therefore, ARA larger than 3 mm has been reported as a potential cause of type II endoleak [5]. Because of this, prophylactic ARA coil embolization for ARAs larger than 3 mm is effective for reduction of type II endoleak. In general, routine embolization for lumbar artery, IMA, and median sacral artery is not recommended. In our case, we did not embolize any of these branches.
No previous report has discussed the differences between ARA arising from the aortic neck and that arising from the aneurysm wall. In our case, because the ARA arose from the aneurysm wall and was over 4 mm in diameter, the patient was considered at high risk for type II endoleak from ARA; accordingly, we decided to perform the ARA coil embolization. After coiling, contrary to our concerns, eGFR and blood pressure were well under control, and no type II endoleak from ARA was seen. Additional studies are required to further decrease the incidence of type II endoleaks.
Conclusions
Prophylactic coil embolization for a large ARA originating from an abdominal aortic aneurysm appears to be safe and effective in preventing type II endoleak following EVAR.
Abbreviations
- AAA:
-
Abdominal aortic aneurysm
- ARA:
-
Accessory renal artery
- EVAR:
-
Endovascular aneurysm repair
References
Urban BA, Ratner LE, Fishman EK. Three-dimensional volume-rendered CT angiography of the renal arteries and veins: normal anatomy, variants, and clinical applications. Radiographics. 2001;21:373–86.
Ozkan U, Oguzkurt L, Tercan F, Kizilkilic O, Koc Z, Koca N. Renal artery origins and variations: angiographic evaluation of 855 consecutive patients. Diagn Interv Radiol. 2006;12:183–6.
Antoniou GA, Karkos CD, Antoniou SA, Georgiadis GS. Can an accessory renal artery be safely covered during endovascular aortic aneurysm repair? Interact Cardiovasc Thorac Surg. 2013;17:1025–7.
Greenberg JI, Dorsey C, Dalman RL, Lee JT, Harris EJ, Hernandez-Boussard T, Mell MW. Long-term results after accessory renal artery coverage during endovascular aortic aneurysm repair. J Vasc Surg. 2012;56:291–6.
Karmacharya J, Parmer SS, Antezana JN, Fairman RM, Woo EY, Velazquez OC, Golden MA, Carpenter JP. Outcomes of accessory renal artery occlusion during endovascular aneurysm repair. J Vasc Surg. 2006;43:8–13.
Malgor RD, Oderich GS, Vrtiska TJ, Kalra M, Duncan AA, Gloviczki P, Cha S, Bower TC. A case-control study of intentional occlusion of accessory renal arteries during endovascular aortic aneurysm repair. J Vasc Surg. 2013;58:1467–75.
Bakoyiannis C, Cagiannos C, Wasilljew S, Puerschel A, Pinter L, Kolvenbach R. Laparoscopic hybrid techniques for ectopic or accessory renal arteries debranching in complex endovascular aneurysm repair. J Cardiovasc Surg. 2008;49:67–71.
Canyigit M, Hidiroglu M, Uguz E, Cetin H. Iliorenal periscope graft to maintain blood flow to accessory renal artery. Diagn Interv Radiol. 2015;21:334–7.
Mendes BC, Oderich GS, Reis de Souza L, Banga P, Macedo TA, de Martino RR, Misra S, Gloviczki P. Implications of renal artery anatomy for endovascular repair using fenestrated, branched, or parallel stent graft techniques. J Vasc Surg. 2016;63:1163–9.
Authors’ contributions
RY described and designed the article. SF, EI, and YM edited the article. NT, TA, and TO supervised the editing of the manuscript. The remaining co-authors collected the data and discussed the content of the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
This patient was properly informed and gave consent for her clinical information to be included in an Elsevier publication.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Nishie, R., Toya, N., Fukushima, S. et al. Prophylactic accessory renal artery coil embolization for prevention of type II endoleak following endovascular aneurysm repair: a case report. surg case rep 3, 58 (2017). https://doi.org/10.1186/s40792-017-0334-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40792-017-0334-y