Abstract
Introduction
Duplication of the vertebral artery (VA) is a rare vascular variant. To the best our knowledge, only fourteen cases have been reported with angiographic findings that they have dual origin of the VA from ipsilateral subclavian artery. Herein, we present a case of duplication of right VA which was incidentally detected by magnetic resonance (MR) angiography.
Case description
A 69-year-old female patient presented with headache for 30 days. She underwent brain MR imaging with MR angiography for evaluating possible intracranial cause. There was a dual origin of the right vertebral artery (VA) as an incidental finding without other significant abnormalities.
Discussion and Evaluation
Diagnosis of duplicated VA can be difficult due to its rarity and misinterpreted as the vascular dissection. In addition, a detailed knowledge of this variation is potentially important to prevent inadvertent challenges during endovascular procedure. Because duplicated VA has smaller lumen and usually enters the higher transverse foramen than those of normal side, it can be influence the choice or route of endovascular treatment.
Conclusions
We suggested that the understanding of embryologic background about VA can be helpful to identify unexpected vascular findings on imaging studies in clinical practice.
Similar content being viewed by others
Background
Duplication of vertebral artery (VA) is rare and represents 0.72 % in autopsy studies (Bergman et al. 1988). This vascular variant is considered a developmental anomaly that shows a dual origin with a variable level of fusion in the neck (Goddard et al. 2001). According to previous articles, there are 36 reported cases about this vascular variant (Komiyama et al. 1999; Watanabe et al. 2015). However, a total of 14 cases have been reported with angiographic findings in literature that they have dual origin of the VA from ipsilateral subclavian artery (SCA), including a case of bilateral VA duplications. It is clinically significant because it can be mistaken for a dissection of VA (Thomas et al. 2008). Herein, we present a case of duplication of VA as an incidental finding during magnetic resonance angiography (MRA) examination of a patient with headache. Further, we also reviewed its embryological mechanism and clinical significance of this variation.
Case description
A 69-year-old female patient presented with headache for 30 days. She had no other clinical manifestation or significant past medical history. There was no abnormal finding at the initial neurological examination.
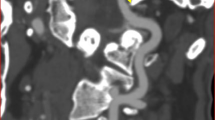
She underwent cranial magnetic resonance image (MRI) with 3D time-of-flight (TOF) intracranial MRA and gadolinium-enhanced neck MRA, using 1.5T system (Signa Excite, GE Medical Systems, Milwaukee, WI, USA). Routine cranial MR images revealed no significant focal lesion in the brain parenchyma. 3D TOF intracranial MRA was also normal. Contrast-enhanced neck MRA demonstrated a duplication of the right VA with two origins from ipsilateral SCA before the origin of right internal thoracic artery (Fig. 1). The two limbs of duplicated VA confined to proximal V1 segment, and converged to form one main trunk at the 3.6 cm distal from each orifice. The first and second limbs of duplicated V1 segment measured 2.8 and 2.6 mm in diameter at the points of origin, respectively. The distance between two limbs calculated 8.0 mm. The diameter of the common trunk of right VA was 3.8 mm at the point of reconstitution. On the left side, the VA arose from the left SCA and measured 4.1 mm in diameter. There was no other vascular abnormality in the major cervical arteries. The patient was managed conservatively and the patient’s clinical symptoms were relieved after 7 days.
Discussion
Duplicated VA is a rare vascular variant (Bergman et al. 1988). It is defined that VA has two origins with fusion at a variable level of the neck. Duplication of the VA has been confused with fenestration of VA, which is a different condition showing a single origin with a short segment of two limbs of VA and one connection with each other along its course (Goddard et al. 2001; Thomas et al. 2008).
Embryologically, the VA is formed by the development of postcostal longitudinal anastomosis which links the intersegmental arteries. The intersegmental arteries eventually obliterated with an exception of the seventh, which becomes the proximal SCA and includes the VA point of origin in adults (Newton and Mani 1974). Duplication of VA is a result from abnormality of embryologic development of aortic arch and persistence of the intersegmental artery (Polguj et al. 2013a). Whereas dual origin of VA originating from the right SCA or brachiocephalic artery occurs due to persistence of the right fourth or fifth (or less frequently third) intersegmental arteries, persistence of the left fourth or fifth (or less frequently third) intersegmental arteries can result in aortic origin or dual origin of the left VA (Komiyama et al. 1999). In addition, the level of entrance into the transverse foramen indicates which intersegmental artery or arteries persist (Meila et al. 2012).
To our best knowledge, only fourteen cases have been reported the duplicated VA with dual origin from SCA among total 36 reported cases of duplicated VA (Table 1) (Babin and Haller 1974; Harada et al. 1987; Hashimoto et al. 1987; Mahmutyazicioğlu et al. 1998; Goddard et al. 2001; Ionete and Omojola 2006; Harnier et al. 2008; Mordasisni et al. 2008; Thomas et al. 2008; Meila et al. 2012; Melki et al. 2012; Polguj et al. 2013b; Rameshbabu et al. 2014). Unilateral duplication of VA was more commonly observed in left side (Goddard et al. 2001). In most cases, the two limbs of the duplicated VA arise from the aorta and the SCA. The limb of duplicated artery also can be originated from common carotid artery, brachiocephalic trunk, or thyrocervical trunk (Bergman et al. 1988; Rameshbabu et al. 2014). Generally, the normal VA is the 1st vessel branching of the SCA and it contributes to the posterior circulation of the head and neck. Whereas normal VA almost always enters the C6 transverse foramen, duplication of VA usually enters the higher transverse foramen (Thomas et al. 2008).
The clinical feature of the duplication of the VA is nonspecific and usually asymptomatic. And it is still controversy whether duplication of the VA is associated with other pathologic conditions. Ionete and Omojola (2006) demonstrated that duplicated VA was normal variation as incidental finding with no significant clinical or pathologic consequences. Conversely, anecdotal reports stated this vascular variant may predispose the patient to VA dissection, intracranial aneurysm, kinking, and arteriovenous malformation (Rameshbabu et al. 2014).
Dual origin of the VA is usually diagnosed as an incidental finding that occurs during imaging workups for other clinical situations. However, a detailed knowledge of this variation is potentially important to prevent inadvertent diagnostic or therapeutic challenges during endovascular procedure. Because duplicated VA has smaller lumen of its proximal V1 than that of normal side, it can be influence the choice or route of endovascular treatment (Thomas et al. 2008; Ionete and Omojola 2006).
Conclusion
In conclusion, we provide a rare case of the right VA with dual origin as an incidental finding on MRA. This report suggested that the awareness of embryologic background about VA can be helpful to identify unexpected vascular findings on computed tomographic angiography (CTA) or MRA, and differentiate this variation from other pathologic conditions such arterial dissection in clinical practice.
Abbreviations
- VA:
-
vertebral artery
- SCA:
-
subclavian artery
- MRA:
-
magnetic resonance angiography
- MRI:
-
magnetic resonance image
- TOF:
-
time-of-flight
- CTA:
-
computed tomographic angiography
References
Babin E, Haller M (1974) Correlation between bony radiological signs and dolichoarterial loops of the cervical vertebral artery. Neuroradiology 7(1):15–17
Bergman RA, Thompson SA, Afifi AK, Saadeh FA (1988) Compendium of human anatomic variation: text, atlas and world literature. Urban and Schwarzenberg, Baltimore, pp 71–72, 358–359
Goddard AJ, Annesley-Wiliams D, Guthrie JA, Weston M (2001) Duplication of the vertebral artery: report of two cases and review of the literature. Neuroradiology 43(6):477–480
Harada J, Nishijima M, Yamatani K, Endo S, Takaku A (1987) A case of the duplicate origin of right vertebral artery. No Shinkei Geka 15(3):321–325
Harnier S, Harzheim A, Limmroth V, Horz R, Kuhn J (2008) Duplication of the common carotid artery and the ipsilateral vertebral artery with a fenestration of the contralateral common carotid artery. Neurol India 56(4):491–493
Hashimoto H, Ohnishi H, Yuasa T, Kawaguchi S (1987) Duplicate origin of the vertebral artery: report of two cases. Neuroradiology 29(3):301–303
Ionete C, Omojola MF (2006) MR angiographic demonstration of bilateral duplication of the extracranial vertebral artery: unusual course and review of the literature. AJNR Am J Neuroradiol 27(6):1304–1306
Komiyama M, Nakajima H, Yamanaka K, Iwai Y (1999) Dual origin of the vertebral artery—case report. Neurol Med Chir (Tokyo) 39(13):932–937
Mahmutyazicioğlu K, Saraç K, Bölük A, Kutlu R (1998) Duplicate origin of left vertebral artery with thrombosis at the origin: color doppler sonography and CT angiography findings. J Clin Ultrasound 26(6):323–325
Meila D, Tysiac M, Petersen M et al (2012) Origin and course of the extracranial vertebral artery: CTA findings and embryologic considerations. Clin Neuroradiol 22(4):327–333
Melki E, Nasser G, Vandendries C, Adams D, Ducreux D, Denier C (2012) Congenital vertebral duplication: a predisposing risk factor for dissection. J Neurol Sci 314(1–2):161–162
Mordasisni P, Schmidt F, Schroth G, Remonda L (2008) Asymmetrical bilateral duplication of the extracranial vertebral arteries: report of a unique case. Eur J Radiol Extra 67:e91–e94
Newton TH, Mani RL (1974) The vertebral artery. In: Newton TH, Potts DG (eds) Radiology of skull and brain. Mosby, St. Louis, pp 1659–1672
Polguj M, Podgórski M, Jędrzejewski K, Topol M, Majos A (2013a) Fenestration and duplication of the vertebral artery: the anatomical and clinical points of view. Clin Anat 26(8):933–943
Polguj M, Jędrzejewski K, Topol M, Wieczorek-Pastusiak J, Majos A (2013b) Duplication of the left vertebral artery in a patient with dissection of the right internal carotid artery and Ehlers–Danlos syndrome: case report and review of the literature. Anat Sci Int 88(2):109–114
Rameshbabu C, Gupta OP, Gupta KK, Qasim M (2014) Bilateral asymmetrical duplicated origin of vertebral arteries: multidetector row CT angiographic study. Indian J Radiol Imaging 24(1):61–65
Thomas AJ, Germanwala AV, Vora N et al (2008) Dual origin extracranial vertebral artery: case report and embryology. J Neuroimaging 18(2):173–176
Watanabe K, Saga T, Iwanaga J, Tabira Y, Yamaki KI (2015) A rare case of dual origin of the left vertebral artery without convergence. Folia Morphol (Warsz) 75(1):136–142
Authors’ contributions
Concept and design: HJB, KHC. Acquisition of data: JB. Analysis and interpretation of data: HJB, JB, HSS. Drafting the manuscript: HJB, JB. Final approval: JB, HJB, HSS, KHC. All authors read and approved the final manuscript.
Acknowledgements
None.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Informed consent for publication of this report and any accompanying images was obtained from the patient.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Baik, J., Baek, H.J., Shin, H.S. et al. Duplication of the right vertebral artery: MRA findings and review of the literature. SpringerPlus 5, 1123 (2016). https://doi.org/10.1186/s40064-016-2807-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40064-016-2807-z