Abstract
Background
Papua New Guinea (PNG) is one of the 14 countries categorised as having a triple burden of tuberculosis (TB), multidrug-resistant TB (MDR TB), and TB-human immunodeficiency virus (HIV) co-infections. TB infection prevention and control (TB-IPC) guidelines were introduced in 2011 by the National Health Department of PNG. This study assesses the implementation of this policy in a sample of district hospitals in two regions of PNG.
Methods
The implementation of TB-IPC policy was assessed using a survey method based on the World Health Organization (WHO) IPC assessment framework (IPCAF) to implement the WHO’s IPC core components. The study included facility assessment at ten district hospitals and validation observations of TB-IPC practices.
Results
Overall, implementation of IPC and TB-IPC guidelines was inadequate in participating facilities. Though 80% of facilities had an IPC program, many needed more clearly defined IPC objectives, budget allocation, and yearly work plans. In addition, they did not include senior facility managers in the IPC committee. 80% (n = 8 of 10) of hospitals had no IPC training and education; 90% had no IPC committee to support the IPC team; 70% had no surveillance protocols to monitor infections, and only 20% used multimodal strategies for IPC activities. Similarly, 70% of facilities had a TB-IPC program without a proper budget and did not include facility managers in the TB-IPC team; 80% indicated that patient flow poses a risk of TB transmission; 70% had poor ventilation systems; 90% had inadequate isolation rooms; and though 80% have personal protective equipment available, frequent shortages were reported.
Conclusions
The WHO-recommended TB-IPC policy is not effectively implemented in most of the participating district hospitals. Improvements in implementing and disseminating TB-IPC guidelines, monitoring TB-IPC practices, and systematic healthcare worker training are essential to improve TB-IPC guidelines’ operationalisation in health settings to reduce TB prevalence in PNG.
Similar content being viewed by others
Background
Suboptimal infection prevention and control (IPC) practices in health settings are a major driver of growing antimicrobial resistance and healthcare-associated infections (HAIs). This presents a critical concern for healthcare workers (HCWs) and governments globally [1, 2]. In Europe, one in 18 patients admitted to hospitals and one in 25 in the United States develop HAIs during hospitalisation [3]. In recent decades, the importance of IPC has been overlooked in many health settings worldwide. However, the coronavirus disease (COVID-19) pandemic has highlighted the significance of IPC practices in ensuring the safety of HCWs and patients and reducing the spread into the community [4, 5]. The pandemic has demonstrated that even sophisticated healthcare systems have gaps in implementing IPC measures [6]. Effective IPC strategies such as proper hand hygiene, isolation of patients suspected or confirmed with infectious pathogens, and personal protective equipment (PPE) are essential to minimise HAIs and transmission of infectious disease, thereby underpinning healthcare quality and safety [7].
Effective IPC practices recommended by the World Health Organization (WHO) provide an important framework for IPC programs. These IPC practices are the cornerstones in improving patients’ and HCW’s safety, preventing disease outbreaks, and quality of healthcare in clinical settings worldwide [8]. However, comprehensive information on the assessment of IPC implementation in healthcare settings has been largely limited to high-income settings. In 2018, the WHO developed the IPC Assessment Framework (IPCAF) to strengthen the implementation of their IPC core components in healthcare settings [9]. The IPCAF is a structured closed-formatted survey with an associated scoring system primarily aimed at being self-administered by facility staff. The framework is intended for acute healthcare institutions but can be used in other clinical settings [10].
Recently, the WHO has assessed the implementation of the IPC core components in 81 countries using the IPCAF tool [11]. The WHO assessment found an overall median score of 605 out of 800, demonstrating an advanced level of IPC implementation in many healthcare institutions [11]. However, despite the high IPCAF scores globally, significant variations in the IPC core components remain across different countries [1]. For instance, among the low-income countries studied, only nine (45%) indicated having a national IPC program, four (20%) guidelines on implementation methods, and one (5%) monitored compliance with IPC practice [5]. The global assessment showed that more efforts are needed to strengthen IPC strategies in low-income countries susceptible to disease outbreaks such as COVID-19 and tuberculosis [12].
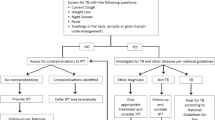
Tuberculosis infection prevention and control (TB-IPC) is part of the broad IPC strategy. IPC and TB-IPC strategies have overlapping activities such as infrastructure, space, management, and organisation of care. Therefore, establishing an IPC program can influence TB infection control practices and in turn, contribute to the quality of TB care in primary healthcare settings (Fig. 1). The WHO recommends IPC as one of the three measures for reducing the high burden of TB in TB/HIV-prevalent countries [13]. These measures include isoniazid preventive treatment, intensified case finding, and IPC. TB-IPC, such as the administrative, environmental, and respiratory control measures implemented in health settings, can effectively prevent the incidence and prevalence of Mycobacterium TB transmission [14,15,16,17,18]. For example, introducing a cough officer screening (COS) system in a hospital in Taiwan has improved TB detection and prevents TB transmission among healthcare staff, patients and guardians and eventually spread into the community [19].
PNG is among the 14 countries in the world with a triple burden of TB, multidrug-resistant TB (MDR TB), and TB-HIV dual infections [20]. In 2011, TB-IPC was incorporated into the PNG National TB Management plan as policy [21]. Healthcare settings were instructed to implement TB-IPC measures as one of the main strategies to address the TB burden in PNG. However, available data shows that there has been no reduction in TB prevalence despite the requirement to implement this policy in PNG [22, 23]. The number of case notifications of all forms of TB increased between 2008 and 2014 but stabilised during 2015–2016 [22]. In 2019, PNG had an estimated TB incidence of 432 new cases per 100 000 population compared to 333 per 100 000 in 2016 [22, 24]. Since the release of the TB-IPC policy, there has been a limited review of implementation in the PNG health sector. This review is critical to better understand where implementation gaps are to prioritise investment and human resources.
Methods
Study design
This survey research was based on a self-administered structured questionnaire adapted from the WHO IPCAF, TB-IPC, and site observations [25]. This design was selected because of its simplicity, affordability, and ease of implementation [26]. This study was approved by the Griffith University Human Research Ethics Committee, Australia, GU Ref No: 2021/921, and PNG Medical Research Advisory Committee (MRAC), MRAC # 22.01. Informed written and verbal consent was obtained from participants during data collection. Approval was also sought from gatekeepers to access health facilities staff and documents.
Setting and study population
This study was conducted in district hospitals in the PNG Highlands and Momase regions. The district hospitals were targeted because they provide specialised TB services, including sputum examination, radiography, registration of diagnosed cases, and treatment [27, 28]. Of the 23 district hospitals that provide TB services within the two regions, 13 facilities were randomly selected using a random number algorithm available through Excel [29]. The first 13 facilities were included in the study. Out of 13 district hospitals, seven were chosen from the Highlands region and six from the Momase region. However, it was impossible to visit three health facilities for security reasons resulting in a final number of ten facilities, with five from the Highlands and five from the Momase region. The participating health facilities consist of six non-government and four government facilities (Table 1).
Data collection
IPCAF survey instrument
Data collection was conducted from March to June 2022. The implementation of IPC guidelines was evaluated at the health facilities using the structured IPCAF tool [9]. The IPCAF is a validated health facility evaluation tool used globally to assess a facility’s IPC program [11]. The IPCAF evaluates the core components of IPC measured out of 100 points: [1] IPC programs, [2] IPC guidelines, [3] IPC education and training, [4] healthcare-associated infections (HAI) surveillance, [5] multimodal strategies for implementation of IPC interventions, [6] monitoring/audits of IPC practices and feedback, [7] workload, staffing, and bed occupancy and [8] built environment, materials, and equipment for IPC at the facility level, which is inclusive of TB-IPC. This tool uses a four-tier system. Depending on the final score (ranging from 0 to 800), the facility IPC program implementation is grouped into four different IPC categories: inadequate (0-200), basic (201–400), intermediate (401–600), or advanced (601–800).
The IPCAF was also used to assess the implementation of TB-IPC measures including (i) administrative, (ii) environmental, and (iii) personal respiratory measures [9]. This assessment was done through a self-reported survey by facility managers, nursing directors, TB program managers, laboratory workers, and outpatient staff and by observations by the lead researcher of TB-IPC practices in selected locations, including outpatient, laboratory, and TB wards. Based on the overall score achieved in the three TB-IPC measures, the facility was assigned to one of the four TB-IPC levels: inadequate (0–80), basic (80–160), intermediate (160–240), or advanced (240–320).
Site observations of TB-IPC practices
An unannounced direct observation of control measures was performed using the WHO TB-IPC health facility assessment checklist to gain an objective assessment of implementation [30]. Observation is considered as an important aspect of data collection to observe the physical and social environment of the research settings including TB ward, isolation room, and laboratory setting. It allows researchers to gain a better knowledge of how activity or program operates as it permits the researcher to witness areas that program employees and participants may omit in an interview [31]. Questions were related to the three TB-IPC measures including administrative, environmental, and personal protective control measures. These observations were conducted between two shifts (morning and evening) [9]. For quality control, the questionnaires and checklists were pilot tested in a non-participating facility and revised accordingly [32].
Data analysis
Statistical analyses were performed using Statistical Package for the Social Sciences (SPSS) Version 26.0 [33]. Descriptive statistics were conducted for categorical data using univariate frequency analysis and percentages. We summarised the scores by frequency, percentage, and median with the interquartile range [33, 34]. Data from the IPCAF survey were linked with data from facility observations to allow for multidimensional descriptions of TB-IPC components at the facility level. The non-parametric Mann-Whitney U Test was used to compare whether there is a statistical difference or similarity in the median IPC scores between the non-government and government health facilities, which are two independent groups that have implemented TBIPC guidelines [25]. Statistical significance was assessed at p < = 0.05.
Results
Health setting information
The assessment included 10 district hospitals covering over 40% (10 of 23) of the Highlands and Momase region facilities. The findings provide a good coverage of non-government and government district hospitals and bed capacity, and the surveyed health facilities are representative of the total sampled district hospitals within the two regions. Among these facilities, the average bed capacity was 60 beds per facility (range of 20 to 120 beds). Six were non-government facilities, and four were government hospitals (Table 1). The profile of the participating health facilities is derived from the Provincial Health Authority (PHA) annual performance reports and health facility websites. A summary of the findings has been provided to the participating district hospitals for quality improvement. The key assessment findings related to health facility-level TB-IPC programs proposed by WHO and the National Department of Health in PNG are discussed in the following sections.
Distribution of IPCAF score
The overall median score from the surveyed facilities was 315 out of 800, with an interquartile range of 164.5 to 403.5. The two district hospitals with the highest IPCAF scores (574 and 474) obtained ‘intermediate’ IPC levels according to the WHO IPCAF category. When categorised into IPC level by the score, three (30%) facilities fall into the inadequate (0-200 points) category, five (50%) fall into the basic (201–400) category, and two (20%) facilities fall into the intermediate (401–600) category, with no facilities in the advanced (601–800) category. Overall, the median score for each of the 8 core components varied across each health facility (Fig. 2). The non-parametric Mann-Whitney U Test identified there was no statistically significant difference in the median IPC score between the non-government and government district hospitals (p = 1.00) The data shows that 80% of the health facilities have either inadequate or basic IPC levels. Figure 2 summarises the implementation of IPC core components in the participating health facilities in the Highlands and Momase region, PNG.
Analysis of infection prevention and control (IPC) implementation in district hospitals
The core components (CC) with the lowest scores and critical areas for attention were: (i) multimodal strategies for implementation of IPC interventions (CC5), (ii) healthcare-associated infections (HAIs) surveillance (CC4), (iii) IPC education and training (CC3), and (vi) IPC program (CC1). Table 2 summarises the distribution of the core components of the surveyed facilities.
IPC program (CC1)
The median score for the IPC program was 32.0 (IQR:12.0–55.25). Eight (80%) of the ten district hospitals had an IPC program. However, many IPC programs did not include all the WHO-recommended guidelines, including funding for IPC activities, annual activity plans, staff training, IPC committee, and clearly defined objectives related to local epidemiology. There was also an inadequate representation of senior facility managers in the IPC team and no demonstrable support for IPC objectives and indicators within the facility.
Of the district hospitals included in the survey, 9 (90%) facilities reported no IPC committee comprising a multidisciplinary team actively supporting the IPC team. Further, there were no full-time IPC nurses and inadequate professional development opportunities for IPC practitioners. Only one facility (10%) had access to an adequate microbiology laboratory and provided sufficient quality results on time.
IPC education and training (CC3)
CC3 had a median score of 25.0 (IQR: 19.75–39.25). Seven (70%) of the ten facilities do not have expertise in IPC or infectious diseases to lead IPC training. As a result, there is no IPC training for clinical and non-clinical HCWs, including nurses, doctors, administrative and managerial staff, and janitors directly involved with patient care in the facility. Additionally, eight (80%) facilities do not provide ongoing education for IPC staff, including regularly attending conferences and other IPC-related courses. Only two (20%) facilities conducted IPC training for all clinical staff as part of new employee induction and mandatory training.
Healthcare-associated infections (HAIs) surveillance (CC4)
CC4 had a median value of 24.50 (IQR: 12.75–42.50). None of the facilities have a person responsible for HAI surveillance activities. Subsequently, HAI surveillance was not conducted in the facilities. Eight (80%) facilities have no established systems for device-associated infections, colonization, or diseases caused by antimicrobial-resistant pathogens. It was also noted that only two (20%) facilities have surveillance protocols, including device-associated infections, local priority epidemic-prone infections (TB and typhoid), and conditions in vulnerable populations. Seven (70%) facilities indicated having no protocol to perform surveillance on HAI and evaluate if the surveillance is in line with the current needs and priorities of the facility.
Multimodal strategies for implementation of IPC interventions (CC5)
CC5 received the lowest score in the facility assessment, with a median of 22.0 (IQR: 8.25–52.75). Overall, two (20%) facilities used multimodal strategies such as system change, education and training, monitoring and feedback, communications and reminders, and safety climate and culture change. These two facilities reported ensuring the necessary infrastructure and continuous availability of supplies and addressing ergonomics, and accessibility, such as the best placement of central venous catheter set and tray. Nine (90%) facilities do not have a multidisciplinary team to implement IPC multimodal strategies. They do not regularly link to colleagues from quality improvement and patient safety to promote IPC multimodal strategies.
Analysis of tuberculosis infection prevention and control (TB-IPC) measures in the facilities
The control measures with the lowest scores and critical areas for attention were environmental and personal respiratory control measures. Table 3 summarises the distribution of the TB-IPC measures in the participating health facilities in the Highlands and Momase region, PNG.
Distribution of TB-IPC scores
The overall median score of the TB-IPC was 45.50 out of 320, with an interquartile range between 34 and 53. When categorised by the score into the four TB-IPC implementation levels, one (10%) facility falls into the inadequate (0–80 points) category, seven (70%) fall into the basic ( 80–160) category, one (10%) fall into the intermediate (160–240) category, with one (10%) facility fall in the advanced (240–320) category. Overall, the median score for each of the three core components varied across each health facility. The non-parametric Mann-Whitney U Test identified there was no statistically significant difference in the median TB-IPC score between the non-government and government district hospitals (p = 1.00). The data shows that 80% of the health facilities have either inadequate or basic TBIPC practices. Figure 3 summarises the TB-IPC practices in the participating health facilities in the Highlands and Momase region, PNG.
Administrative control measures
The highest median score of 235.0 (IQR: 197.50–327.50) was for the administrative control measures. Of the ten rural hospitals participating in this survey, seven (70%) facilities had a facility TB-IPC plan. However, none of the TB-IPC plans had all the WHO-recommended guidelines, such as a proper budget for TB-IPC activities, TB-IPC committee, staff training on TB-IPC, clearly defined objectives, and work plans based on local epidemiology. Nine (90%) facilities indicated conducting triaging, systematic screening for coughing patients, and regular health education for health workers, patients, and visitors. However, from the site observations, 7 (70%) facilities have not separated coughing patients from other patients. Subsequently, coughing patients congregated with others in the outpatient area, posing a risk of TB transmission to other patients. Additionally, in 8 (80%) facilities, the flow of suspected TB cases through the facility poses a risk for TB transmission. The increasing risk for TB transmission among patients is consistent with the findings from direct observation, where poor physical distancing resulted in overcrowding in the emergency waiting area.
Environmental control measures
Environmental control measures had the lowest median score at 60.0 (IQR: 37.27–85.75). None of the facilities surveyed indicated having designated waiting areas for TB patients. Therefore, the available waiting space is for all patients, not TB patients. The inadequate waiting space was consistent with the findings from direct observations where all patients waited in the outpatient waiting areas for medical consultations. However, patients with positive TB who were discharged and returned for review report directly to the TB clinic. The site observations are consistent with this practice in all health facilities.
Eight (80%) facilities indicated using natural ventilation such as opening doors and windows, especially in waiting areas, sputum collection rooms, and patient wards. However, 7 (70%) facilities had poor ventilation systems. The low level of ventilation system in the wards was consistent with the findings from direct observation, where TB ward doors and windows were opened occasionally or not at all. Nine (90%) facilities do not have an isolation room, while five (50%) facilities reported that they do not have a TB ward. Upon site observation in all ten facilities, patients diagnosed with TB are admitted for two months before being discharged with other patients in the medical ward, increasing TB transmission to other potentially immunosuppressed patients.
Personal respiratory control measures
Personal respiratory control has the second-highest median score at 65.0 (IQR: 42.25–85.0). Eight (80%) facilities reported having personal protective equipment (PPE) for staff at the health center. However, essential PPE, including N95 respirators and medical face masks, are not continuously available in sufficient quantities for HCWs. The low availability of PPE in health facilities was consistent with the findings from direct observation, where most staff did not use N95 respirators during their consultations with patients. The inadequate PPE has influenced HCWs and patients’ compliance with recommended standards in 7 (70%) facilities. This practice was consistent with the findings from direct observation, where 9 (90%) facilities have inconsistent practices in which HCWs, and patients do not use the recommended PPE during HCW-patient consultations.
Discussion
This is the first known regional health facility survey using the WHO IPCAF to assess the implementation of IPC and TB-IPC guidelines in PNG district hospitals. The key finding is that most district hospitals had either inadequate or basic IPC and TB-IPC levels. Overall, this study showed that the availability of IPC and TB-IPC programs in the regions does not directly correspond to a well-functioning facility-level TB-IPC practice where main TB-IPC components are implemented.
Specifically, we found challenges related to setting clear objectives and funding for IPC programs. Although many (80%) facilities in the Highlands and Momase region had an IPC program, there was no funding or clear objectives for IPC activities based on the local epidemiology, as the WHO recommends. This result is consistent with the WHO global survey on IPC in healthcare facilities [11] showing that despite the advanced IPC program, overall, only 15.2% of facilities met all indicators considered as minimum criteria for an IPC program [11]. These findings corroborate with other literature evaluating core components of IPC programs. For example, 38 of the 41 (83%) hospitals in Georgia that had an IPC program lacked funding and had unclear objectives [3]. Objectives help define goals, prioritise conflicting activities, guide decision-making, and ensure accountability of resources within the health institution, such as funding. This lack of clear objectives and strategies has led to the neglect of achieving the IPC goals of reducing healthcare-associated infections such as tuberculosis.
Our findings show that specialised IPC and TB-IPC training and education were not offered for HCWs in eight facilities resulting in limited opportunities for ongoing staff development and capacity building. The inadequate capacity building for HCWs in PNG is consistent with a study in Pakistan and Bangladesh that found that limited IPC training among HCWs affected TB-IPC practice. Additionally, TB-IPC training was available for facility managers and senior HCWs but not all staff [13]. Similarly, a study in seven high TB-burden countries found that over half of the HCWs receiving training on TB-IPC guidelines did not understand the content and were unaware of many IPC interventions [36].This point suggests that the quality of training is important. Therefore, standardising training on IPC can achieve more consistent practice nationally supported by adequate educational materials. Mandatory training and resourcing IPC guidelines would strengthen the practice and improve the standard of IPC in the facility. The suboptimal results regarding IPC expertise and inadequate training for HCWs highlight an essential gap and a critical priority area for improvement.
This study shows that few of the Highlands and Momase regions facilities have TB wards, ventilation facilities, and isolation rooms. Limited infrastructure is not unique to PNG; other studies in South Africa, Pakistan, China, and Bangladesh found that inadequate isolation and ventilation systems in healthcare facilities have limited the operationalisation of recommended TB-IPC measures [35, 36]. A similar situation was observed in Ghana, where comparable shortcomings increased TB transmission [37]. A continuing lack of essential health infrastructure, such as a TB ward in district hospitals, will significantly impact TB-IPC strategies and, in turn, the development and transmission of TB among patients, HCWs, and communities. Improving healthcare infrastructure, combined with other methods such as consistent availability of medical equipment and HCWs training, will enhance healthcare quality and prevent TB transmission in healthcare facilities.
Many facilities in this survey reported that PPE was insufficient to adequately protect frontline HCWs. A similar situation was observed in South Africa, where a shortage of PPE in healthcare facilities has seriously affected infection control plans. Additionally, the South African facilities did not provide PPE regularly, and it was supplied to specific departments such as the multi-drug resistant TB (MDR TB) unit [38, 39]. The COVID-19 pandemic has highlighted the significance of IPC in health settings [5]. One important consideration was an investment in PPE to prevent the transmission of COVID-19 among HCWs, patients, and the public. This increased visibility and recognition of PPE should serve to promote the use of such resources and reinforce TB-IPC measures in health settings. This requires regular financial and human investments, including specialised expertise, and highlights the importance of sufficient funding dedicated to IPC.
Strengths and Limitations
The survey used the WHO IPCAF and allowed for direct comparison with the global study of IPC in healthcare settings. Almost half of the district hospitals in the two regions participated and were randomly selected, allowing careful extrapolations to the regional level. Besides these strengths, the study has several limitations. The IPCAF requires a sound knowledge of the WHO terminology. Participants who self-administered the survey needed to understand unfamiliar terms, including multimodal strategies, creating the potential for misinterpretation and false reporting. This study is limited to the Highlands and Momase regions in PNG. A national survey is therefore recommended to determine the extent of the implementation of TB-IPC across PNG.
Conclusion
This study assessed the implementation of TB-IPC practice in district hospitals in the Highlands and Momase region, PNG. The study included site assessment followed by validation of practices using the WHO IPCAF survey tool. Our survey findings show a lack of IPC programs, insufficient IPC training and education for HCWs to implement programs, and a lack of IPC infrastructure and personal protective equipment in health facilities. Implementing TB-IPC policy at the provincial level via committees, plans, personnel appointments, improved IPC facilities, and ongoing staff training are effective strategies for improving TB-IPC policy implementation in healthcare institutions.
Data availability
The data (health facility assessment survey) are available from the corresponding author upon request.
Abbreviations
- CC:
-
Core component
- COVID:
-
Coronavirus disease
- GU:
-
Griffith University
- HAI:
-
Healthcare associated infections
- HCW:
-
Healthcare workers’
- IPCAF:
-
Infection Prevention and Control Assessment Framework
- MDR TB:
-
Multidrug resistant tuberculosis
- PNG MRAC:
-
Papua New Guinea Medical Advisory Research Committee
- PNG:
-
Papua New Guinea
- TB:
-
Tuberculosis
- TB-HIV:
-
Tuberculosis-human immunodeficiency virus
- TBIPC:
-
Tuberculosis Infection Prevention and Control
- WHO:
-
World Health Organization
References
Aghdassi SJS, Hansen S, Bischoff P, Behnke M, Gastmeier P. A national survey on the implementation of key infection prevention and control structures in german hospitals: results from 736 hospitals conducting the WHO infection Prevention and Control Assessment Framework (IPCAF). Antimicrob Resist Infect Control. 2019;8(1):1–9.
Ogunsola FT, Mehtar S. Challenges regarding the control of environmental sources of contamination in healthcare settings in low-and middle-income countries: a narrative review. Antimicrob Resist Infect Control. 2020;9(1):1–9.
Deryabina A, Lyman M, Yee D, Gelieshvilli M, Sanodze L, Madzgarashvili L et al. Core components of infection prevention and control programs at the facility level in Georgia: key challenges and opportunities. Antimicrobial Resistance and Infection Control [Internet]. 2021;10(1):1–20. Available from: https://doi.org/10.1186/s13756-020-00879-3
World Health Organization. Infection prevention and control during healthcare when Coronavirus Disease (COVID-19) is suspected or confirmed. World Health Organization Interim Guidance [Internet]. 2021;(July 2021):1–5. Available from: https://apps.who.int/iris/rest/bitstreams/1272420/retrieve
Tomczyk S, Storr J, Kilpatrick C, Allegranzi B. Infection prevention and control (IPC) implementation in low-resource settings: a qualitative analysis. Antimicrobial Resistance and Infection Control [Internet]. 2021;10(1):1–11. Available from: https://doi.org/10.1186/s13756-021-00962-3
Zhou Z. COVID-19 Worldwide: strategies to reduce risk for frontline healthcare workers. Sci Eng Technol. 2022;8(January 2020):412–9.
Hopman J, Allegranzi B, Mehtar S. Managing COVID-19 in low- and middle-income countries. N Engl J Med. 2020;382(18):1677–9.
Houghton C, Meskell P, Delaney H, Smalle M, Glenton C, Booth A et al. Barriers and facilitators to healthcare workers’ adherence with infection prevention and control (IPC) guidelines for respiratory infectious diseases: a rapid qualitative evidence synthesis (Review).Cochrane Database of Systematic Reviews. 2020;(4):CD013582.
World Health Organization (WHO). WHO guidelines on tuberculosis infection prevention and control, 2019 update [Internet]. World Health Organization. 2019. 1–72 p. Available from: WHO guidelines on tuberculosis infection prevention and control: 2019 update https://www.ncbi.nlm.nih.gov/books/NBK539301/
World Health Organization. Infection prevention and control assessment framework at the facility level [Internet]. Vol. 2016, World Health Organization. Geneva: World Health Organization; 2018. 1–16 p. Available from: https://www.who.int/infection-prevention/tools/core-components/IPCAF-facility.PDF Infection prevention and control assessment framework at the facility level (who.int)
Tomczyk S, Twyman A, de Kraker MEA, Coutinho Rehse AP, Tartari E, Toledo JP, et al. The first WHO global survey on infection prevention and control in health-care facilities. Lancet Infect Dis. 2022;22(6):845–56.
Cohen R, Gesser-Edelsburg A, Singhal A, Benenson S, Moses AE. Translating a theory-based positive deviance approach into an applied tool: mitigating barriers among health professionals (HPs) regarding infection prevention and control (IPC) guidelines. PLoS ONE [Internet]. 2022;17(6 June):1–18. Available from: https://doi.org/10.1371/journal.pone.0269124
Islam S, Tarannum S, Banu S, Chowdhury KIA, Nazneen A, Chughtai AA et al. Preparedness of tertiary care hospitals to implement the national TB infection prevention and control guidelines in Bangladesh: a qualitative exploration. PLoS ONE [Internet]. 2022;17(2 February):1–15. Available from: https://doi.org/10.1371/journal.pone.0263115
Escombe AR, Ticona E, Chávez-Pérez V, Espinoza M, Moore DAJ. Improving natural ventilation in hospital waiting and consulting rooms to reduce nosocomial tuberculosis transmission risk in a low resource setting. BMC Infectious Diseases [Internet]. 2019;19(88):2–7. Available from: https://www.scopus.com/inward
Maclntyre C, Zhang Y, Chughtai AA, Seale H, Zhang D, Chu Y et al. Cluster randomised controlled trial to examine medical mask use as source control for people with respiratory illness. BMJ Open [Internet]. 2016;6(12):1–9. Available from: https://doi.org/10.1136/bmjopen-2016-012330
Tiemersma EW, Huong NT, Yen PH, Tinh BT, Thuy TTB, Hung N et al. Infection control and tuberculosis among health care workers in Viet Nam, 2009–2013: a cross-sectional survey. BMC Infectious Diseases [Internet]. 2016;16(1):7–9. Available from: https://doi.org/10.1186/s12879-016-1993-1
Dharmadhikari AS, Mphahlele M, Stoltz A, Venter K, Mathebula R, Masotla T et al. Surgical face masks worn by patients with multidrug-resistant tuberculosis: impact on infectivity of air on a hospital ward. American Journal of Respiratory and Critical Care Medicine [Internet]. 2012;185(10):1104–9. Available from: https://www.scopus.com/inward
Marme G, Rutherford S, Harris N. What tuberculosis infection control measures are effective in resource-constrained primary healthcare facilities? A systematic review of the literature. Rural and remote health [Internet]. 2022; Available from: https://www.rrh.org.au/journal/article/7175
Lin C-H, Tsai C-H, Liu C-E, Huang M-L, Chang S-C, Wen J-H et al. Cough officer screening improves detection of pulmonary tuberculosis in hospital in-patients. BMC Public Health [Internet]. 2010;10(238):2–7. Available from: https://www.scopus.com/inward
World Health Organization. WHO global lists of high burden countries for tuberculosis (TB), TB / HIV and TB (MDR / RR-TB) [Internet]. Geneva. ; 2021. Available from: https://apps.who.int/iris/handle/10665/341980
Department of Foreign Affairs & Trade (DFAT). TB prevention and control in Papua New Guinea: report of the review of contribution of DFAT investments 2011–2018 [Internet]. Port Moresby. ; 2019. Available from: https://www.dfat.gov.au
Aia P, Wangchuk L, Morishita F, Kisomb J, Yasi R, Kal M, et al. Epidemiology of tuberculosis in Papua New Guinea: analysis of case notification and treatment-outcome data, 2008–2016. Western Pac Surveillance Response J. 2018;9(2):9–19.
Diefenbach-Elstob T. The epidemiology of tuberculosis in the Balimo region of Western Province, Papua New Guinea [Internet]. James Cook University; 2018. Available from: https://researchonline.jcu.edu.au/56210/1/JCU_56210-diefenbach-elstob-2018-thesis.pdf
Diefenbach-Elstob T, Guernier V, Burgess G, Pelowa D, Dowi R, Gula B et al. Molecular evidence of drug-resistant tuberculosis in the Balimo region of Papua New Guinea. Tropical Medicine and Infectious Disease Article [Internet]. 2019;4(33):1–10. Available from: www.mdpi.com/journal/tropicalmed
Godfrey C, Tauscher G, Hunsberger S, Austin M, Scott L, Schouten JT et al. A survey of tuberculosis infection control practices at the NIH / NIAID / DAIDS- supported clinical trial sites in low and middle income countries. BMC Infectious Diseases [Internet]. 2016;16(269):1–7. Available from: https://doi.org/10.1186/s12879-016-1579-y
Odoh M, Chinedum I. Research designs, survey and case study. IOSR J VLSI Signal Process. 2014;4(6):16–22.
John G, Paison D, Ken W, Anna M, Maxine W. Independent state of Papua New Guinea health system review. Volume 9. Port Moresby: PNG Government Press; 2019.
Field E, Usurup J, Nathan S, Rosewell A. Contextual factors and health service performance from the perspective of the provincial health administrators in Papua New Guinea.Rural and Remote Health. 2018;18(4).
Bhardwaj P. Types of sampling in research. J Pract Cardiovasc Sci. 2019;5(3):157.
Buregyeya E, Nuwaha F, Verver S, Criel B, Colebunders R, Wanyenze R et al. Implementation of tuberculosis infection control in health facilities in Mukono and Wakiso districts, Uganda.BMC Infectious Diseases. 2013;13(1).
Espedal G, Lovaas BJ, Sirris S, Waeraas A. Researching values: methodological approaches for understanding Values work in organisations and leadership [Internet]. Switzerland: Palgrave Macmillan; 2022. XIX, 309. Available from: https://doi.org/10.1007/978-3-030-90769-3
Sorra J, Zebrak K, Yount N, Famolaro T, Gray L, Franklin M, et al. Development and pilot testing of survey items to assess the culture of value and efficiency in hospitals and medical offices. BMJ Qual Saf. 2022;31(7):493–502.
Yockey R. SPSS demystified: a step-by-step guide to successful data analysis. Second edi. New York: Routledge;: Routledge Taylor & Francis Group; 2016.
Kuyinu YA, Mohammed AS, Adeyeye OO, Odugbemi BA, Goodman OO, Odusanya OO. Tuberculosis infection control measures in health care facilities offering tb services in Ikeja local government area, Lagos, South West, Nigeria. BMC Infectious Diseases [Internet]. 2016;16(1). Available from: https://doi.org/10.1186/s12879-016-1453-y
Chen B, Liu M, Gu H, Wang X, Qiu W, Shen J, et al. Implementation of tuberculosis infection control measures in designated hospitals in Zhejiang Province, China: are we doing enough to prevent nosocomial tuberculosis infections? BMJ Open. 2016;6(3):1–8.
Islam MS, Chughtai AA, Banu S, Seale H. Context matters: examining the factors impacting the implementation of tuberculosis infection prevention and control guidelines in health settings in seven high tuberculosis burden countries. Journal of Infection and Public Health [Internet]. 2021;14(5):588–97. Available from: https://doi.org/10.1016/j.jiph.2021.01.014
Der JB, Grant AD, Grint D, Narh CT, Bonsu F, Bond V. Barriers to tuberculosis case finding in primary and secondary health facilities in Ghana: perceptions, experiences and practices of healthcare workers. BMC Health Services Research [Internet]. 2022;22(1):1–14. Available from: https://doi.org/10.1186/s12913-022-07711-1
Vigenschow A, Edoa JR, Adegbite BR, Agbo PA, Adegnika AA, Alabi A, et al. Knowledge, attitudes and practices regarding tuberculosis amongst healthcare workers in Moyen-Ogooué Province, Gabon. BMC Infect Dis. 2021;21(1):1–7.
Vigenschow A, Adegbite BR, Edoa J, Alabi A, Adegnika AA, Grobusch MP, et al. Tuberculosis infection control measures in healthcare facilities in Moyen-Ogooué Province, Gabon. BMC Health Serv Res. 2021;21(1200):1–11.
Acknowledgements
We acknowledge the Provincial Health Authorities in the two regions of Papua New Guinea for their approval to access the health facilities and the participants. We also recognise the Chief Executive Officers (CEO), hospital administrators, and director of nursing of the surveyed facilities to allow access to facility documents and staff.
Funding
Griffith University supported this work as part of the first author’s PhD program. The authors are responsible for the views expressed in this article and do not necessarily represent the views, decisions, or policies of the institutions with which the authors are affiliated.
Author information
Authors and Affiliations
Contributions
GM, JK, P-AZ, NH, and SR reviewed and validated the data collection tools. GM conducted the survey and site observations. GM, JK, P-AZ, NH, and SR analysed the data, and all authors validated the initial analysis results. All authors contributed to writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The health facility survey and analysis were conducted as part of Gigil Marme’s PhD study at Griffith University, Australia. All surveyed facilities and participants consented to participate, and ethics approvals were provided by Griffith University and Medical Advisory Research Committee.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Marme, G., Kuzma, J., Zimmerman, PA. et al. Tuberculosis infection prevention and control in rural Papua New Guinea: an evaluation using the infection prevention and control assessment framework. Antimicrob Resist Infect Control 12, 31 (2023). https://doi.org/10.1186/s13756-023-01237-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13756-023-01237-9