Abstract
Background
Hemophagocytic lymphohistiocytosis (HLH) is a rapid-onset, potentially fatal hyperinflammatory syndrome. A prompt molecular diagnosis is crucial for appropriate clinical management. Here, we validated and prospectively evaluated a targeted high-throughput sequencing approach for HLH diagnostics.
Methods
A high-throughput sequencing strategy of 12 genes linked to HLH was validated in 13 patients with previously identified HLH-associated mutations and prospectively evaluated in 58 HLH patients. Moreover, 2504 healthy individuals from the 1000 Genomes project were analyzed in silico for variants in the same genes.
Results
Analyses revealed a mutation detection sensitivity of 97.3 %, an average coverage per gene of 98.0 %, and adequate coverage over 98.6 % of sites previously reported as mutated in these genes. In the prospective cohort, we achieved a diagnosis in 22 out of 58 patients (38 %). Genetically undiagnosed HLH patients had a later age at onset and manifested higher frequencies of known secondary HLH triggers. Rare, putatively pathogenic monoallelic variants were identified in nine patients. However, such monoallelic variants were not enriched compared with healthy individuals.
Conclusions
We have established a comprehensive high-throughput platform for genetic screening of patients with HLH. Almost all cases with reduced natural killer cell function received a diagnosis, but the majority of the prospective cases remain genetically unexplained, highlighting genetic heterogeneity and environmental impact within HLH. Moreover, in silico analyses of the genetic variation affecting HLH-related genes in the general population suggest caution with respect to interpreting causality between monoallelic mutations and HLH. A complete understanding of the genetic susceptibility to HLH thus requires further in-depth investigations, including genome sequencing and detailed immunological characterization.
Similar content being viewed by others
Background
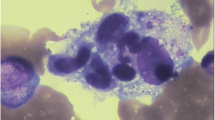
Hemophagocytic lymphohistiocytosis (HLH) is a severe hyperinflammatory syndrome that presents with unremitting fever, splenomegaly and cytopenia [1]. According to the HLH-2004 protocol, HLH can be defined as fulfillment of at least five of eight clinical and laboratory criteria [2]. Primary, genetic, as well as secondary forms of HLH have been described. HLH is typically treated by immunosuppression, followed by hematopoietic stem cell transplantation in familial cases [1]. Current HLH criteria poorly discriminate underlying causes of disease. Importantly, therapies tailored to different etiologies of HLH may improve treatment outcome [3].
Several genetic disorders predispose to HLH, but vary in their risk of developing disease. Congenital defects affecting the perforin-mediated lymphocyte cytotoxicity, such as autosomal recessive mutations in PRF1, UNC13D, STX11, and STXBP2, represent the most common causes of primary HLH, termed familial HLH (FHL) type 2, 3, 4 and 5, respectively [1, 4]. The impaired killing of infected as well as activated immune cells results in the sustained hyperinflammatory state characteristic of HLH, where animal models have postulated a critical role for CD8+ T cells and interferon (IFN)-γ [5]. Patients with autosomal recessive mutations in RAB27A and LYST, causative of Griscelli syndrome type 2 (GS2) and Chediak-Higashi syndrome (CHS), respectively, also frequently develop HLH. Besides defective lymphocyte cytotoxicity, these syndromes are associated with hypopigmentation [6, 7]. Only one case of HLH has been reported in Hermansky-Pudlak syndrome type 2, another hypopigmentation syndrome specifically caused by mutations in AP3B1 and associated with impaired lymphocyte cytotoxicity [8]. Moreover, HLH has so far not been reported in Hermansky-Pudlak syndrome type 9 patients, caused by mutations in BLOC1S6 and also reported to display impaired lymphocyte cytotoxicity [9]. Genetic disorders displaying a more limited impairment of lymphocyte cytotoxicity may also present with HLH or related lymphoproliferative diseases. Patients with hemizygous mutations in SH2D1A or XIAP, associated with X-linked lymphoproliferative disease, typically present with HLH or lymphoproliferative diseases, often triggered by Epstein-Barr virus (EBV) infection [10]. Lymphoproliferation and severe EBV infections are also features of autosomal recessive mutations in ITK [11] and hemizygous mutations in MAGT1 [12], with sporadic cases of HLH [13, 14]. Episodes of HLH have also been reported in patients harboring other primary immunodeficiencies [3, 15–17], providing evidence for hyperinflammatory syndromes fulfilling current HLH criteria in an immunological context of T-cell deficiency or absent IFN-γ signaling. HLH may also arise in the context of inborn errors of metabolism and lysosomal storage disorders, or secondary to infections, malignancies or autoimmune disorders in individuals without any established genetic disease susceptibility [1].
Patients with defective lymphocyte cytotoxicity usually develop early-onset HLH with high penetrance and require the most radical immunosuppressive therapy. Defective natural killer (NK) cell cytotoxic activity, as measured by the 51Cr-release assay, is included among the HLH-2004 diagnostic criteria [2]. However, pathological results with this assay do not necessarily reflect functional defects in lymphocyte cytotoxicity, but can also be caused by low NK cell numbers. Refined assays have been developed for the identification of patients with defects in lymphocyte cytotoxicity as well as XIAP signaling [18–20]. These assays require considerable technical expertise and rely on fresh blood samples. Therefore, improved diagnostic procedures are required for guidance of treatment decisions.
With current insights, patients with defective lymphocyte cytotoxicity can also be diagnosed by DNA sequencing. To influence the clinical management of HLH patients, genetic diagnostics must be rapid and accurate. Due to genetic heterogeneity, achieving a molecular diagnosis by conventional Sanger sequencing is labor-intensive and time-consuming. Technological advances have increased sequencing throughput, with decreased sequencing times and costs [21]. As more bench-top sized machines have been pushed to the market, appealing solutions for diagnostic laboratory settings have become available [22]. Aimed at diagnosing a broad range of immune defects, high-throughput assays have recently been reported for the simultaneous study of a number of primary immunodeficiency syndromes [23–25].
Here, we report our experience in implementing a targeted resequencing approach for identification of HLH patients with defective lymphocyte cytotoxicity. Moreover, we characterize the genetic variants in HLH-related genes in the general population and discuss the implications to interpretation of association of rare, potentially damaging monoallelic variants with disease.
Methods
Patients
The study was performed using genomic DNA (gDNA) samples from (1) 13 patients with a confirmed molecular diagnosis in an HLH-related gene, (2) 58 patients, prospectively recruited over a 12 months period, fulfilling five or more HLH diagnostic criteria (n = 56) or with a cytotoxicity defect suggestive of primary HLH (n = 2). Informed consent was obtained from all study participants in accordance with the Declaration of Helsinki. The study was approved by the Regional Ethics Review Board in Stockholm, Sweden.
AmpliSeq custom panel design
A targeted resequencing panel covering 12 HLH-associated genes was designed according to Ion AmpliSeq technology (Ion Torrent, Thermo Fisher Scientific, MA, USA; Table 1). Using genome build hg19 as reference, the coding regions, with 25 intronic base pairs around exons, were targeted. For PRF1, UNC13D, STX11, and STXBP2, the evolutionarily conserved non-coding regions, identified using the software Alamut (Interactive Bio-software, Rouen, France), were also included. Sequencing data generated by this study has been submitted to the European Genome-phenome Archive and is available from the authors on request.
Library preparation and sequencing
Library preparation was performed with 10 ng gDNA using Ion AmpliSeq Library Kit 2.0 for each multiplex PCR reaction (Ion Torrent, Thermo Fisher Scientific). The library was thereafter ligated with sequencing adaptors containing barcodes (Ion Xpress Barcode Adapters 1–16 Kit, Ion Torrent, Thermo Fisher Scientific). After purification (Agencourt AMPure XP reagent, Beckman Coulter, Brea, CA, USA), libraries were quantified on an Agilent 2100 Bioanalyzer (Agilent Technologies, CA, USA) and diluted to a concentration of 100 pM. Diluted libraries were pooled and further amplified with an emulsion PCR. Enriched templates were loaded onto an Ion 314 or Ion 316 Chip (Ion Torrent, Thermo Fisher Scientific).
Bioinformatics analyses
Assessment of sequencing quality control, mapping, coverage analysis and variant calling were performed using the Ion Torrent Suite Software (versions 4.0.2 and 4.0.3, Thermo Fisher Scientific). Mapping of sequencing reads to the genome build hg19 was performed using TMAP software. The Ion Torrent Variant caller (version 4.2.0) was used in “Germline - low stringency” mode with default settings. Integrative Genomics Viewer (IGV) version 2.3.32 [26] was used for the inspection of sequencing reads and visual assessment of detected variants. Called variants were first annotated with Variant Effector Predictor [27] followed by GEMINI (version 0.11.0) [28]. Further analyses were performed with R (version 3.1.2) [29]. In silico evaluation of candidate variants was performed by reviewing CADD [30], PolyPhen-2 [31] and SIFT scores [32]. NNSPLICE 0.9 was used for predicting the effect of splice-site variants [33].
Sanger validation and sequencing of poorly covered amplicons
All variants considered pathogenic were validated by Sanger sequencing. Moreover, non-covered or poorly amplified exonic regions were Sanger sequenced in unexplained patients. Primers and PCR conditions are available upon request. The PCR products were purified and sequenced on an ABI 3730 Genetic Analyzer (Applied Biosystems, Thermo Fisher Scientific) and analyzed with SeqScape (version 2.5; Applied Biosystem, Thermo Fisher Scientific). Variant segregation in the family was evaluated depending on availability of parental DNA.
Analysis of mutational load in FHL genes in the 1000 Genomes dataset
Variant call format (vcf) files including sequencing data from 2504 individuals from the 1000 Genomes project were analyzed with respect to genes included in the panel (ftp://ftp-trace.ncbi.nih.gov/1000genomes/ftp/release/20130502/, accessed January 2015). Variants were annotated using Variant Effector Predictor [27] and GEMINI [28]. All variants deviating from Hardy-Weinberg equilibrium (p value < 0.05) were removed. Further analyses were performed with R (version 3.1.2).
Immunological analyses
Intracellular expression of perforin, granzymes, CD107a, and SAP as well as cytotoxic lymphocyte exocytosis was evaluated by flow cytometry [20]. NK cell cytotoxicity against K562 target cells was evaluated with a standard 4-hour 51Cr-release assay using peripheral blood mononuclear cells (PBMCs) [34] and the data are shown as lytic units at 25 % specific lysis. All flow cytometry data were acquired on a LSR Fortessa instrument (BD Biosciences, CA, USA). Analyses were performed in Flow Jo v9.7 and R (version 3.1.2).
Results
Coverage analysis
A custom targeted resequencing panel was designed to cover 12 genes in which mutations have been associated with HLH or lymphoproliferative disorders (Table 1). The panel consisted of 355 primer pairs, with an amplicon size range of 125–175 bp, covering up to 97.3 % of the desired target. Specific primers could not be designed for 1125 bp, due to repetitive regions. Following sequencing, analyses revealed that some amplicons repeatedly failed to generate adequate coverage, as determined by a ≤10× cut-off of mean coverage across samples (Fig. 1a; Additional file 1). Excluding two amplicons that failed in nearly all samples (mean coverage ≤10×), the effective coverage of our initial target sequences was estimated to be 96.6 % of the initial regions of interest, with an average coverage per gene over exonic and splice-site regions of 98 % (Table 1). To ensure clinical efficacy, we calculated the proportion of previously reported mutations (based on the Human Gene Mutation database (HGMD), accessed June 2015) with adequate coverage. Overall, 98.6 % of the mutations listed in HGMD were covered by our design (Table 1).
Analysis of coverage efficiency and variant filtering strategy. a Heatmap indicating coverage for each individual amplicon (355 amplicons) in each patient sample. The coverage is categorized in <10×, 10–50× or >50× coverage. Patient samples and amplicon are shown in columns and rows, respectively. Patient samples from both the validation and the prospective cohorts are included. Rows are sorted by position. Columns are sorted by average coverage for each patient. On the right side the bar plot is shown the number of samples with lower coverage (<10× and 10–50×). The detailed coverage information of all amplicons is reported in Additional file 1. b Flowchart of filtering strategy in the prospective HLH cohort. For each step the bar chart on the right shows the proportions of different types of variants. MAF minor allele frequency, UTR untranslated region
Assay validation
To validate our gene panel, we sequenced gDNA from 13 patients with previously identified genetic defects (Table 2). The patients carried a wide spectrum of mutations located in different genes (Table 2). In order to assess the reliability of the method for detection of homozygous exonic deletions, we also included a patient with a 298-bp homozygous exonic deletion of STXBP2. We could identify all 18 small genetic aberrations upon read inspection in IGV. Nonetheless, the variant calling software detected only 17 out of 18 small genetic aberrations (Table 2). The RAB27A c.148_149delinsC InDel, located in a homopolymer nucleotide stretch, was instead erroneously called as a synonymous variant (c.148A>C; Fig. S1a in Additional file 2). The exonic deletion was easily detected by visual assessment of the coverage over the amplicons (Fig. S1b in Additional file 2).
We next sought to estimate the overall sensitivity of the variant calling strategy by assessing all exonic polymorphisms (n = 56) previously identified in the 13 control samples (Additional file 3). In total, 74 variants (n = 18 mutations and n = 56 polymorphisms) were used for the sensitivity analysis. Out of these, 72 variants were properly called. The overall sensitivity was 97.3 % (95 % confidence interval 90.7–99.2, Wilson score method).
Prospective cohort of HLH patients
Following validation, we sequenced a cohort of 58 prospectively recruited HLH patients (Fig. 2a). The median age at diagnosis of HLH was 3 years, ranging from a few days to 70 years (interquartile range = 0.4–13.2 years; Table 3). Eight patients were above 18 years of age at diagnosis of HLH. The included patients were of different ethnic origin, including 43 % from Turkey. Parental consanguinity was reported in 24 cases. Interestingly, six patients also suffered from albinism and eight patients had a familial history of HLH or unexplained siblings’ death in childhood (Table 3). Hyperferritinemia, splenomegaly and hypertriglyceridemia and/or hypofibrinogenemia were the most common findings in our cohort. Soluble interleukin-2 receptor (sCD25) was elevated in all seven patients tested (Table 3).
Clinical, genetic and functional characteristics of the patients included in the prospective cohort. a Heatmap of clinical and functional features of the implementation cohort in relation to HLH-2004 diagnostic criteria [2]. The patients are ordered based on age at diagnosis of HLH. A family history refers to a positive family history for HLH or unexplained siblings’ death in childhood. b The different molecular diagnoses achieved in the prospective cohort according to age group at diagnosis of HLH. c NK cell cytotoxic activity, displayed as lytic units at 25 % specific lysis, in healthy controls and patients from the implementation cohort grouped in diagnosed (n = 10) and undiagnosed (n = 13) (significance level *p < 0.05, ****p < 0.0001). d Intracellular expression of perforin, CD107a, granzyme A and B, and SAP in PBMCs of HLH patients from the implementation cohort. Patients are grouped by their molecular diagnosis (FHL2, n = 4; FHL3-4,GS2,CHS, n = 9; No diagnosis, n = 19). The data are expressed as percentage of normalized median fluorescence intensity (MFI) in comparison with healthy controls. Exocytic activity of CD3−CD56+ NK cells (e) and CD8+CD57+ T cells (f) was measured as percentage of CD107a+ cells in healthy controls and HLH patients from the implementation cohort. P815 target cells were used alone and in combination with anti-CD16 antibody for NK cells and anti-CD3 antibody for CD8 T cells. Exocytic activity of NK cells was also measured using K562 target cells. Patients are grouped by their molecular diagnosis (FHL2, n = 4; FHL3-4,GS2,CHS, n = 9; No diagnosis, n = 20). The controls used were both local and transport controls
Overall, 246 genetic variants were identified in the prospective cohort. Filtering for variants with a possible impact at the protein level, and with a minor allele frequency <0.05 in the Exome Aggregation Consortium dataset [35], 71 potentially pathogenic variants were selected for further analysis (Fig. 1b). After manual curation, 19 variants (single-nucleotide variants or small indels), either in homozygous or compound heterozygous state, were classified as disease-causing (Table 4; Additional file 4). One additional disease-causing mutation was found upon read inspection in IGV, namely c.148_149delinsC in RAB27A (P53). The same disease-causing mutation was also missed by the variant calling program in our validation study (Table 2; Fig. S1a in Additional file 2).
In addition to analysis of single nucleotide variants and small indels, we performed coverage analysis to identify larger homozygous deletions (Fig. 1a). We identified a hemizygous deletion of XIAP in P26 and a large homozygous deletion of STX11 in P56 (Fig. S1c, d in Additional file 2).
Molecular diagnoses
In total, we identified and validated 22 unique disease-causing mutations located in six different genes (Table 4), achieving a molecular diagnosis in 22 patients (overall diagnostic rate 38 %, 22 of 58). The diagnostic yield was higher, 65 % (13 of 20), in the group of patients with HLH presentation before one year of age compared with 24 % (9 of 37) among the older patients (Fig. 2b). Excluding adult cases of HLH (n = 8), the diagnostic rate was 44 % (22 of 50) among the pediatric cases. Interestingly, the oldest patient with primary HLH in this cohort, aged 16 years (P48), had compound heterozygous variants in PRF1, c.272C>T (p.Ala91Val) and c.1288G>T (p.Asp430Tyr). The variant p.Ala91Val has been associated with later onset of disease when in trans to other PRF1 mutations [36].
We identified patients with biallelic mutations in PRF1 (n = 7), UNC13D (n = 6), STX11 (n = 4), RAB27A (n = 2) and LYST (n = 2) as well as a patient with a hemizygous mutation in XIAP (Fig. 2b, Table 4). The mutational spectrum was broad, including missense, nonsense, and splicing mutations, indels, small and large deletions. Eight of the 22 identified mutations are novel (Table 4). Mutations were identified in five out of six patients presenting with albinism and HLH. Interestingly, one such patient with albinism (P1) was diagnosed with a homozygous UNC13D splice-site mutation (c.570-1G>A). No patients were found to have mutations in STXBP2, SH2D1A, ITK, MAGT1, AP3B1, and BLOC1S6.
Finally, in 36 out of 58 patients, biallelic variants that could explain the disease phenotype were not detected. The age at diagnosis of HLH was significantly higher compared with genetically diagnosed patients (Wilcoxon rank sum test, p = 0.06). Moreover, 61 % (22 of 36) were diagnosed with a concomitant disease known to predispose to secondary HLH. The most commonly associated diseases were EBV infection (n = 10), other infections (n = 4), and hematological cancer (n = 3). In contrast, an infectious trigger was reported in only 4 of 22 (18 %) of the genetically diagnosed patients. Thus, the group of undiagnosed patients had a higher frequency of known triggers of HLH (Fisher’s exact test, p = 0.002). Of note, seven out of the eight adult HLH cases (88 %) were associated with a known trigger of HLH, suggesting that these may truly represent secondary HLH cases.
Correlation between genetic and functional findings
Results from at least one NK cell or CD8+ T cell functional assay were available from 33 patients, including 13 patients with a molecular diagnosis and 20 patients without a definitive diagnosis. Substantiating the genetic findings, immunological analyses revealed defective NK cell cytotoxicity and virtually absent perforin expression in the four patients with biallelic PRF1 mutations studied (Fig. 2a, c, d). Moreover, CD8+ T-cell and NK cell exocytosis was defective in patients with mutations in UNC13D, STX11, RAB27A, and LYST (Fig. 2a, e, f). Interestingly, a patient with RAB27A mutations presented with defective NK and CD8+ T cell exocytosis, but normal NK cell cytotoxicity, while a patient with LYST mutations displayed defective NK cell cytotoxicity but only abnormal NK and CD8+ T-cell exocytosis (Fig. 2a, d, e). Overall, all patients with a genetic diagnosis for which functional data were available displayed a functional defect by at least one diagnostic assay.
Among the undiagnosed patients, seven patients displayed defective NK cell cytotoxicity (<10 LU; n = 6) and/or exocytosis (<5 % CD107a+ NK cells following K562 target cell incubation; n = 4). Three such cases belonged to the adult HLH cohort (Fig. 2a). Therefore, 4 out of 15 pediatric HLH cases (26 %) for which functional data were available displayed a defective NK cell function. In a few cases, the low NK cell cytotoxicity could reflect the low percentage of NK cells in PBMCs (Additional file 5). Notably, none of the undiagnosed patients with defective exocytosis against K562 target cells displayed concomitant defective NK cell exocytosis following anti-CD16 stimulation or defective CD8+CD57+ T-cell exocytosis following anti-CD3 stimulation (Fig. 2e). This result contrasted patients with biallelic UNC13D, STX11, STXBP2, RAB27A, or LYST mutations, which all displayed defective exocytosis in response to all stimuli. A greater variability has been noted in assays quantifying NK cell exocytosis in response to Fc receptor engagement or CD8+CD57+ T-cell exocytosis in response to T-cell receptor engagement [20]. Taken together, it is possible that impaired K562 target cell-induced exocytosis in these patients does not reflect mutations in proteins generally required for cytotoxic lymphocyte exocytosis.
Contribution of monoallelic mutations as cause of HLH
In patients without an established molecular diagnosis based on biallelic or hemizygous mutations, we identified seven different monoallelic variants in nine patients with damaging predictions by either SIFT or PolyPhen-2 (Additional file 6). These were regarded as monoallelic variants of unknown significance. Three patients carried the variant PRF1 c.272C>T p.Ala91Val in a heterozygous state. One of these patients also carried an additional rare variant with pathogenic prediction in STXBP2 (c.1034C>T, p.Thr345Met), a combination previously reported in two patients with HLH [37]. The monoallelic variants were identified among both pediatric (n = 7) and adult (n = 2) patients. Four out of the nine patients with monoallelic variants were reported to have a known trigger of HLH and only one had a positive family history of unexplained siblings’ death in childhood. Overall, 25 % of HLH patients without an established molecular diagnosis carried at least one variant with an in silico damaging prediction.
To interpret findings in patients without an established molecular diagnosis and provide an overview of genetic variations in genes linked to HLH, we examined the frequency of variants in genes included in our panel among 2504 unrelated individuals from the 1000 Genomes project. Discarding intronic variants outside splice-site regions and synonymous variants, 1956 individuals carried at least one variant with a minor allele frequency lower than 0.05. Applying more strict filters (i.e., at least one damaging prediction by either SIFT or PolyPhen-2), 636 individuals (25.4 %) were identified as carrying at least one possibly damaging variant (Additional file 7). The majority of variants were found in LYST and UNC13D, likely reflecting gene size (Fig. S3a, b in Additional file 8). Limiting the analysis to FHL genes, 413 individuals carried at least one possibly damaging variant. Surprisingly, monoallelic variants in genes linked to HLH were thus not enriched in patients with HLH lacking a molecular diagnosis (Fig. S3c, d in Additional file 8). Nonetheless, the PRF1 c.272C>T (p.Ala91Val) variant, in a heterozygous state, showed a weak enrichment (Fisher’s exact test, p value = 0.07) in patients with HLH but no biallelic mutations. However, a larger cohort of HLH patients lacking biallelic mutations is required to study this association further. Of note, two individuals out of 2504 were homozygous for possibly damaging variants in HLH-related genes, namely PRF1 c.272C>T (p.Ala91Val) and UNC13D c.1579C>T (p.Arg527Trp).
Discussion
Current HLH diagnostic criteria are not specific in discriminating patients with a strong genetic predisposition, typically involving defects in lymphocyte cytotoxicity, from those with a number of other etiologies also associated with HLH [1, 3]. As treatment recommendations may differ between the groups, molecular studies can have a direct impact on clinical management. Recent technological advances in DNA sequencing have enabled more comprehensive approaches for genetic screening [38–40]. In this study, we developed and validated a targeted high-throughput sequencing approach in order to rapidly identify patients with mutations in genes required for lymphocyte cytotoxicity. Furthermore, we tested the efficacy of our approach on a prospective cohort of 58 patients fulfilling clinical HLH criteria.
Twelve genes, previously linked to HLH, albinism with HLH, or susceptibility to severe EBV infections, were included in our panel. Overall, we achieved 96.6 % coverage of the genes of interest, with an average coverage per gene of 98 %. Moreover, our design covered almost all sites previously reported as mutated. Lack of coverage was mainly due to difficulty of primer design in repetitive regions. Of the designed primer pairs, only a few amplicons failed sequencing. While panels for the simultaneous analysis of several primary immunodeficiency genes have recently been described [23–25], this is the first report of an HLH gene-specific panel implemented on a substantial number of HLH patients. To our knowledge, this also represents the first resequencing panel that targets evolutionarily conserved intronic regions, which is of importance because such regions harbor disease-causing mutations in HLH patients [34, 41]. The combination of exonic and intronic targets and the spectrum of genes targeted make our panel a comprehensive solution for the molecular diagnostics of HLH patients.
For validation of our variant calling strategy we analyzed 13 patients with a known molecular diagnosis that harbored 18 different mutations and 56 additional variants. The patients were selected in order to cover different kinds of mutations distributed over multiple genes. Our analysis revealed a sensitivity of 97.3 %, comparable to other panels based on Ion Torrent technology [24]. The only missed disease-causing mutation was located in a homopolymer stretch, regions that are challenging to sequence with Ion Torrent technology [42–44]. All variants were correctly visualized in IGV, suggesting that sensitivity potentially can approximate 100 % through further optimization of variant calling software.
When applied to a heterogeneous cohort of 58 patients, with a clinical diagnosis of HLH (n = 56) or with a functional defect suggestive of primary HLH (n = 2; defective NK cell activity combined with defective exocytosis or decreased perforin expression), we identified 22 disease-causing mutations, of which eight were novel, in six of the twelve genes included in the panel. In agreement with the results from the validation cohort, the spectrum of mutations identified in the prospective cohort clearly demonstrated that our method identified different kinds of mutations, including a 22-bp homozygous deletion in LYST. Notably, three patients were found to carry a homozygous indel (STX11 c.369_376delinsTGG), which was not detected in another resequencing study [23]. Moreover, large homozygous deletions were readily identified by coverage analysis and inspection of sequencing reads in both the validation and implementation cohorts. Overall, we achieved a definitive molecular diagnosis in 22 patients (38 %). Biallelic mutations in PRF1 (n = 7) and UNC13D (n = 6) represented the most common finding.
The diagnostic yield was high in the group of patients diagnosed with HLH before one year of age (65 %). In the largest collection of patients with a suspected diagnosis of HLH studied for mutations in PRF1, UNC13D and STXBP2, biallelic mutations were found in 11 % of all cases, and 24 % of cases with onset of disease before 1 year of age [45]. The larger proportion of patients with a genetic diagnosis in our cohort may reflect the larger number of genes studied, more specific inclusion criteria, and a high frequency of consanguinity. Rather, our results compare well with data from the Italian HLH registry, where 40 % of HLH patients overall received a definitive molecular diagnosis [46]. In this cohort, 64 % of HLH patients with an age at onset below 1 year received a molecular diagnosis. Of note, one patient with albinism and HLH was reclassified post-sequencing as FHL3, illustrating a case where phenotypic characteristics potentially could misguide targeted genetic investigations. Conversely, genetic analyses can correct for overlooked phenotypic manifestations [47]. Moreover, RAB27A mutations have recently also been reported in patients without albinism, necessitating RAB27A sequencing in all HLH patients with defective exocytosis [48].
Despite our efforts, 36 patients remained without a definitive molecular diagnosis. Bioinformatics analyses were complemented by visual inspection of sequencing reads and Sanger sequencing of poorly covered amplicons, reducing the likelihood of overlooking mutations. Regulatory mutations or mutations in genes not included in this panel, as well as secondary forms of HLH, are plausible explanations for the lack of genetic findings in these patients. For instance, our small cohort of adult HLH cases may represent secondary HLH. Nonetheless, adult HLH cases should still be studied for primary HLH, as a relatively small proportion of them do harbor biallelic mutations in HLH-related genes [45, 46, 49]. For three undiagnosed patients with a family history of unexplained siblings’ death in childhood, the medical records of the siblings’ disease were scarce. Thus, we could not be sure that these represented familial HLH. Conversely, the sister of an additional undiagnosed patient with EBV-driven HLH (P7) also suffered from a prolonged EBV infection with hepatitis, leukopenia, anemia, and prolonged fever at the age of 7 years, suggesting a familial susceptibility to severe EBV infections in this family. Generally, undiagnosed patients had a higher median age at diagnosis and frequency of known triggers for secondary HLH, with the most common trigger being EBV infection. Four undiagnosed pediatric HLH patients displayed defective NK cell cytotoxicity and/or a selective defect in NK cell exocytosis against K562 target cells, possibly suggesting an immune defect more restricted to NK cell function in these patients.
Interestingly, rare monoallelic variants in genes required for lymphocyte cytotoxicity have previously been reported in HLH patients [37, 45]. However, their contribution to disease development is unclear. We identified nine patients with seven distinct rare monoallelic variants with in silico pathogenic predictions, without any obvious enrichment by age at onset or HLH trigger. Three patients carried the variant PRF1 p.Ala91Val. To gain understanding of the role of monoallelic variants in HLH, we determined the mutational load of the genes included in our panel among 2504 adults from the 1000 Genomes project [50]. Remarkably, in comparison to our cohort of undiagnosed patients and even to a larger cohort from the Italian registry with 18 % of monoallelic variants in sporadic HLH [46], a similar frequency of rare possibly pathogenic variants was found in the 1000 Genomes cohort. Of the 25 rare, possibly pathogenic heterozygous PRF1 variants identified in the 1000 Genomes project cohort, 11 (36 %) have previously been reported as homozygous or compound heterozygous mutations in patients diagnosed with FHL2. Although rare genetic variants may contribute to disease susceptibility, such conclusions require more rigorous experimental validations as recently exemplified for a dominant-negative STXBP2 variant [51]. Although limited in scale and demography, our results suggest a similar burden of heterozygous variants with pathogenic prediction in HLH-associated genes between HLH patients without a known genetic defect and healthy individuals. Thus, prudence is warranted with respect to interpreting causality between rare monoallelic variants and HLH.
Conclusions
We have demonstrated the efficacy of a high-throughput sequencing approach for the molecular diagnosis of patients with suspected HLH. With more than half of the patients lacking an identified genetic aberration, the genetic susceptibility to HLH remains to be discovered with further genome sequencing and immunological characterization. Moreover, we determined the burden of heterozygous variants with pathogenic prediction of HLH-related genes in the general population and unexpectedly found it similar to that observed in HLH patients without a clear genetic diagnosis. Albeit based on a small cohort, our results imply prudence in ascertaining any causality between monoallelic mutations and HLH. Despite the good accuracy in high-throughput sequencing, such diagnostic approaches are best combined with sensitive functional assays for reliable molecular diagnoses of patients with HLH.
Abbreviations
- CHS:
-
Chediak-Higashi syndrome
- EBV:
-
Epstein-Barr virus
- FHL:
-
familial hemophagocytic lymphohistiocytosis
- gDNA:
-
genomic DNA
- GS2:
-
Griscelli syndrome type 2
- HGMD:
-
Human Gene Mutation Database
- HLH:
-
hemophagocytic lymphohistiocytosis
- IFN:
-
interferon
- IGV:
-
Integrative Genomics Viewer
- NK:
-
natural killer
- PBMC:
-
peripheral blood mononuclear cells
References
Janka GE, Lehmberg K. Hemophagocytic syndromes — An update. Blood Rev. 2014;28:135–42.
Henter J-I, Horne A, Aricó M, Egeler RM, Filipovich AH, Imashuku S, et al. HLH-2004: Diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2007;48:124–31.
Bode SF, Ammann S, Al-Herz W, Bataneant M, Dvorak CC, Gehring S, et al. The syndrome of hemophagocytic lymphohistiocytosis in primary immunodeficiencies: implications for differential diagnosis and pathogenesis. Haematologica. 2015;100:978–88.
de Saint BG, Ménasché G, Fischer A. Molecular mechanisms of biogenesis and exocytosis of cytotoxic granules. Nat Rev Immunol. 2010;10:568–79.
Jordan MB. An animal model of hemophagocytic lymphohistiocytosis (HLH): CD8+ T cells and interferon gamma are essential for the disorder. Blood. 2004;104:735–43.
Ménasché G, Pastural E, Feldmann J, Certain S, Ersoy F, Dupuis S, et al. Mutations in RAB27A cause Griscelli syndrome associated with haemophagocytic syndrome. Nat Genet. 2000;25:173–6.
Nagle DL, Karim MA, Woolf EA, Holmgren L, Bork P, Misumi DJ, et al. Identification and mutation analysis of the complete gene for Chediak–Higashi syndrome. Nat Genet. 1996;14:307–11.
Enders A. Lethal hemophagocytic lymphohistiocytosis in Hermansky-Pudlak syndrome type II. Blood. 2006;108:81–7.
Badolato R, Prandini A, Caracciolo S, Colombo F, Tabellini G, Giacomelli M, et al. Exome sequencing reveals a pallidin mutation in a Hermansky-Pudlak–like primary immunodeficiency syndrome. Blood. 2012;119:3185–7.
Schmid JP, Canioni D, Moshous D, Touzot F, Mahlaoui N, Hauck F, et al. Clinical similarities and differences of patients with X-linked lymphoproliferative syndrome type 1 (XLP-1/SAP deficiency) versus type 2 (XLP-2/XIAP deficiency). Blood. 2010;117:1522–9.
Huck K, Feyen O, Niehues T, Ruschendorf F, Hubner N, Laws H-J, et al. Girls homozygous for an IL-2-inducible T cell kinase mutation that leads to protein deficiency develop fatal EBV-associated lymphoproliferation. J Clin Invest. 2009;119:1350–8.
Li F-Y, Chaigne-Delalande B, Kanellopoulou C, Davis JC, Matthews HF, Douek DC, et al. Second messenger role for Mg2+ revealed by human T-cell immunodeficiency. Nature. 2011;475:471–6.
Ghosh S, Bienemann K, Boztug K, Borkhardt A. Interleukin-2-inducible T-cell kinase (ITK) deficiency--clinical and molecular aspects. J Clin Immunol. 2014;34:892–9.
Li F-Y, Chaigne-Delalande B, Su H, Uzel G, Matthews H, Lenardo MJ. XMEN disease: a new primary immunodeficiency affecting Mg2+ regulation of immunity against Epstein-Barr virus. Blood. 2014;123:2148–52.
Alkhairy OK, Perez-Becker R, Driessen GJ, Abolhassani H, van Montfrans J, Borte S, et al. Novel mutations in TNFRSF7/CD27: Clinical, immunologic, and genetic characterization of human CD27 deficiency. J Allergy Clin Immunol. 2015;136:703–12. e10.
Faitelson Y, Grunebaum E. Hemophagocytic lymphohistiocytosis and primary immune deficiency disorders. Clin Immunol. 2014;155:118–25.
Tesi B, Sieni E, Neves C, Romano F, Cetica V, Cordeiro AI, et al. Hemophagocytic lymphohistiocytosis in 2 patients with underlying IFN-γ receptor deficiency. J Allergy Clin Immunol. 2015;135:1638–41. e5.
Ammann S, Elling R, Gyrd-Hansen M, Dückers G, Bredius R, Burns SO, et al. A new functional assay for the diagnosis of X-linked inhibitor of apoptosis (XIAP) deficiency. Clin Exp Immunol. 2014;176:394–400.
Bryceson YT, Pende D, Maul-Pavicic A, Gilmour KC, Ufheil H, Vraetz T, et al. A prospective evaluation of degranulation assays in the rapid diagnosis of familial hemophagocytic syndromes. Blood. 2012;119:2754–63.
Chiang SCC, Theorell J, Entesarian M, Meeths M, Mastafa M, Al-Herz W, et al. Comparison of primary human cytotoxic T-cell and natural killer cell responses reveal similar molecular requirements for lytic granule exocytosis but differences in cytokine production. Blood. 2013;121:1345–56.
Metzker ML. Sequencing technologies — the next generation. Nat Rev Genet. 2010;11:31–46.
Sikkema-Raddatz B, Johansson LF, de Boer EN, Almomani R, Boven LG, van den Berg MP, et al. Targeted next-generation sequencing can replace Sanger sequencing in clinical diagnostics. Hum Mutat. 2013;34:1035–42.
Nijman IJ, van Montfrans JM, Hoogstraat M, Boes ML, van de Corput L, Renner ED, et al. Targeted next-generation sequencing: A novel diagnostic tool for primary immunodeficiencies. J Allergy Clin Immunol. 2014;133:529–34. e1.
Stoddard JL, Niemela JE, Fleisher TA, Rosenzweig SD. Targeted NGS: a cost-effective approach to molecular diagnosis of PIDs. Front Immunol. 2014;5:531.
Moens LN, Falk-Sörqvist E, Asplund AC, Bernatowska E, Smith CIE, Nilsson M. Diagnostics of primary immunodeficiency diseases: a sequencing capture approach. PLoS One. 2014;9, e114901.
Thorvaldsdóttir H, Robinson JT, Mesirov JP. Integrative Genomics Viewer (IGV): high-performance genomics data visualization and exploration. Brief Bioinform. 2013;14:178–92.
McLaren W, Pritchard B, Rios D, Chen Y, Flicek P, Cunningham F. Deriving the consequences of genomic variants with the Ensembl API and SNP Effect Predictor. Bioinformatics. 2010;26:2069–70.
Paila U, Chapman BA, Kirchner R, Quinlan AR. GEMINI: integrative exploration of genetic variation and genome annotations. PLoS Comput Biol. 2013;9, e1003153.
TEAM RdC, others. R: A language and environment for statistical computing. R Foundation for Statistical Computing: Vienna, Austria; 2010. http://www.R-project.org.
Kircher M, Witten DM, Jain P, O’Roak BJ, Cooper GM, Shendure J. A general framework for estimating the relative pathogenicity of human genetic variants. Nat Genet. 2014;46:310–5.
Adzhubei IA, Schmidt S, Peshkin L, Ramensky VE, Gerasimova A, Bork P, et al. A method and server for predicting damaging missense mutations. Nat Methods. 2010;7:248–9.
Ng PC, Henikoff S. SIFT: predicting amino acid changes that affect protein function. Nucleic Acids Res. 2003;31:3812–4.
Reese MG, Eeckman FH, Kulp D, Haussler D. Improved splice site detection in Genie. J Comput Biol. 1997;4:311–23.
Meeths M, Chiang SCC, Wood SM, Entesarian M, Schlums H, Bang B, et al. Familial hemophagocytic lymphohistiocytosis type 3 (FHL3) caused by deep intronic mutation and inversion in UNC13D. Blood. 2011;118:5783–93.
Exome Aggregation Consortium (ExAC). http://exac.broadinstitute.org.
Clementi R, Emmi L, Maccario R, Liotta F, Moretta L, Danesino C, et al. Adult onset and atypical presentation of hemophagocytic lymphohistiocytosis in siblings carrying PRF1 mutations. Blood. 2002;100:2266–7.
Zhang K, Chandrakasan S, Chapman H, Valencia CA, Husami A, Kissell D, et al. Synergistic defects of different molecules in the cytotoxic pathway lead to clinical familial hemophagocytic lymphohistiocytosis. Blood. 2014;124:1331–4.
Chae JH, Vasta V, Cho A, Lim BC, Zhang Q, Eun SH, et al. Utility of next generation sequencing in genetic diagnosis of early onset neuromuscular disorders. J Med Genet. 2015;52:208–16.
Costa JL, Sousa S, Justino A, Kay T, Fernandes S, Cirnes L, et al. Nonoptical massive parallel DNA sequencing of BRCA1 and BRCA2 genes in a diagnostic setting. Hum Mutat. 2013;34:629–35.
Justino A, Dias P, João Pina M, Sousa S, Cirnes L, Berta Sousa A, et al. Comprehensive massive parallel DNA sequencing strategy for the genetic diagnosis of the neuro-cardio-facio-cutaneous syndromes. Eur J Hum Genet. 2015;23:347–53.
Entesarian M, Chiang SCC, Schlums H, Meeths M, Chan M-Y, Mya S-N, et al. Novel deep intronic and missense UNC13D mutations in familial haemophagocytic lymphohistiocytosis type 3. Br J Haematol. 2013;162:415–8.
Loman NJ, Misra RV, Dallman TJ, Constantinidou C, Gharbia SE, Wain J, et al. Performance comparison of benchtop high-throughput sequencing platforms. Nat Biotechnol. 2012;30:434–9.
Singh RR, Patel KP, Routbort MJ, Reddy NG, Barkoh BA, Handal B, et al. Clinical validation of a next-generation sequencing screen for mutational hotspots in 46 cancer-related genes. J Mol Diagn. 2013;15:607–22.
Millat G, Chanavat V, Rousson R. Evaluation of a new high-throughput next-generation sequencing method based on a custom AmpliSeq™ library and ion torrent PGMTM sequencing for the rapid detection of genetic variations in long QT syndrome. Mol Diagn Ther. 2014;18:533–9.
Zhang K, Jordan MB, Marsh RA, Johnson JA, Kissell D, Meller J, et al. Hypomorphic mutations in PRF1, MUNC13-4, and STXBP2 are associated with adult-onset familial HLH. Blood. 2011;118:5794–8.
Cetica V, Sieni E, Pende D, Danesino C, De Fusco C, Locatelli F, et al. Genetic predisposition to hemophagocytic lymphohistiocytosis: Report on 500 patients from the Italian registry. J Allergy Clin Immunol. 2015. doi:10.1016/j.jaci.2015.06.048.
Meeths M, Bryceson YT, Rudd E, Zheng C, Wood SM, Ramme K, et al. Clinical presentation of Griscelli syndrome type 2 and spectrum of RAB27A mutations. Pediatr Blood Cancer. 2010;54:563–72.
Cetica V, Hackmann Y, Grieve S, Sieni E, Ciambotti B, Coniglio ML, et al. Patients with Griscelli syndrome and normal pigmentation identify RAB27A mutations that selectively disrupt MUNC13-4 binding. J Allergy Clin Immunol. 2015;135:1310–8. e1.
Wang Y, Wang Z, Zhang J, Wei Q, Tang R, Qi J, et al. Genetic features of late onset primary hemophagocytic lymphohistiocytosis in adolescence or adulthood. PLoS One. 2014;9, e107386.
McVean GA, Altshuler DM, Durbin RM, Abecasis GR, Bentley DR, Chakravarti A, et al. An integrated map of genetic variation from 1,092 human genomes. Nature. 2012;491:56–65.
Spessott WA, Sanmillan ML, McCormick ME, Patel N, Villanueva J, Zhang K, et al. Hemophagocytic lymphohistiocytosis caused by dominant-negative mutations in STXBP2 that inhibit SNARE-mediated membrane fusion. Blood. 2015;125:1566–77.
Santoro A, Cannella S, Trizzino A, Nigro LL, Corsello G, Arico M. A single amino acid change A91V in perforin: a novel, frequent predisposing factor to childhood acute lymphoblastic leukemia? Haematologica. 2005;90:697–8.
Stadt UZ, Beutel K, Kolberg S, Schneppenheim R, Kabisch H, Janka G, et al. Mutation spectrum in children with primary hemophagocytic lymphohistiocytosis: molecular and functional analyses of PRF1, UNC13D, STX11, and RAB27A. Hum Mutat. 2006;27:62–8.
Mamishi S, Modarressi MH, Pourakbari B, Tamizifar B, Mahjoub F, Fahimzad A, et al. Analysis of RAB27A gene in Griscelli syndrome type 2: novel mutations including a deletion hotspot. J Clin Immunol. 2008;28:384–9.
Karim MA, Nagle DL, Kandil HH, Burger J, Moore KJ, Spritz RA. Mutations in the Chediak-Higashi syndrome gene (CHS1) indicate requirement for the complete 3801 amino acid CHS protein. Hum Mol Genet. 1997;6:1087–9.
Bryceson YT, Rudd E, Zheng C, Edner J, Ma D, Wood SM, et al. Defective cytotoxic lymphocyte degranulation in syntaxin-11-deficient familial hemophagocytic lymphohistiocytosis 4 (FHL4) patients. Blood. 2007;110:1906–15.
Stepp SE, Dufourcq-Lagelouse R, Deist FL, Bhawan S, Certain S, Mathew PA, et al. Perforin gene defects in familial hemophagocytic lymphohistiocytosis. Science. 1999;286:1957–9.
Ueda I, Kurokawa Y, Koike K, Ito S, Sakata A, Matsumora T, et al. Late-onset cases of familial hemophagocytic lymphohistiocytosis with missenseperforin gene mutations. Am J Hematol. 2007;82:427–32.
Feldmann J, Callebaut I, Raposo G, Certain S, Bacq D, Dumont C, et al. Munc13-4 is essential for cytolytic granules fusion and is mutated in a form of familial hemophagocytic lymphohistiocytosis (FHL3). Cell. 2003;115:461–73.
zur Stadt U, Schmidt S, Kasper B, Beutel K, Diler AS, Henter J-I, et al. Linkage of familial hemophagocytic lymphohistiocytosis (FHL) type-4 to chromosome 6q24 and identification of mutations in syntaxin 11. Hum Mol Genet. 2005;14:827–34.
Certain S, Barrat F, Pastural E, Deist FL, Goyo-Rivas J, Jabado N, et al. Protein truncation test of LYST reveals heterogenous mutations in patients with Chediak-Higashi syndrome. Blood. 2000;95:979–83.
Acknowledgements
The authors thank the physicians that referred the patients for genetic and immunological evaluations and Nina Jäntti and Anh Nhi Tran for technical assistance. This study was supported by the European Research Council under the European Union’s Seventh Framework Programme (FP/2007-2013)/ERC Grant Agreement no. 311335, Swedish Research Council, Swedish Children’s Cancer Foundation, Swedish Cancer Foundation, Swedish Foundation for Strategic Research, Wallenberg Foundation and the Stockholm County Council (ALF project). B.T. was supported by a PhD student scholarship awarded by the Board of Postgraduate Studies at Karolinska Institutet.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
BT designed research, performed genetic analyses, interpreted results, and wrote the manuscript; K.L. designed and performed genetic analyses; SC designed and performed immunological analyses and analyzed data; EBB performed genetic analyses; MA, BB, OD, ZF, AYEJ, HCE, MM, HHH, JH, ZK, SN, TP, MS, ETS, THT, EU, SU, AU provided samples and clinical information; MM and JIH analyzed data and interpreted results; M.N. designed research and interpreted results; YTB conceived the study, designed research, interpreted results, and wrote the manuscript. All the authors reviewed and approved the final manuscript.
Additional files
Additional file 1: Table S1.
Coverage information for each amplicon. (XLSX 73 kb)
Additional file 2: Figure S1.
(a) IGV screenshot over the RAB27A c.148_149delinsC indel missed by the variant calling. (b) Coverage distribution over the STXBP2 gene in a control patient and a patient with a deletion of exon 2. (c) Coverage distribution over the STX11 gene in a control patient and in P56, a patient with a STX11 deletion. (d) Coverage distribution over the XIAP gene in a control patient and in P26, a patient with a XIAP deletion. (EPS 3130 kb)
Additional file 3: Table S2.
Polymorphisms and rare variants used in the validation analysis. (DOCX 19 kb)
Additional file 4: Table S3.
Classification of rare variants identified in the prospective cohort. (DOCX 56 kb)
Additional file 5: Figure S2.
Scatterplot of NK cell cytotoxic activity, displayed as lytic units at 25 % specific lysis, and frequency of NK cells in PBMCs. The patients are grouped by their molecular diagnosis. The individuals with very low NK cytotoxicity are also displayed in the zoomed plot for better resolution. Transport controls are included (triangles). (EPS 1171 kb)
Additional file 6: Table S4.
Monoallelic rare variants with in silico pathogenic predictions identified in the patients without a definitive diagnosis. (XLSX 38 kb)
Additional file 7: Table S5.
Monoallelic rare variants with in silico pathogenic predictions identified in the 1000 Genomes cohort. (XLSX 100 kb)
Additional file 8: Figure S3.
Distribution of all variants (a) and variants with likely pathogenic effect (b) by gene. Frequency of at least one rare variant with pathogenic in silico prediction in the 1000 Genomes cohort versus the undiagnosed patients in all 12 genes analyzed (c) or in the FHL genes only (d). (EPS 1784 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Tesi, B., Lagerstedt-Robinson, K., Chiang, S.C.C. et al. Targeted high-throughput sequencing for genetic diagnostics of hemophagocytic lymphohistiocytosis. Genome Med 7, 130 (2015). https://doi.org/10.1186/s13073-015-0244-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13073-015-0244-1