Abstract
Background
The recurrence rate in lumbar disc herniations (LDH) has been reported between 5 and 25%. There are only few data about this phenomenon that occurs within days of the initial operation. We analyse early recurrent LDH by analysis of data from the German Spine register.
Methods
Data from patients undergoing disc herniation surgery in the lumbar region were extracted from the German Spine Registry between 1st January 2012 and 31st December 2016. Patients with early recurrent LDH within days of initial surgery were separately analysed.
Results
A total of 9310 surgeries for LDH were documented in the German Spine Register. From these patients 115 (1.2%) presented an early recurrent disc surgeries within days of the initial surgery. The mean age was 70 ± 2.50 years. Most affected segment was L4/5 (47 cases, 41%), followed by L3/4 (45 cases, 39%). The most of our patients showed a normal or overweight Body Mass Index. Surgery for early recurrent LDH was associated with a high rate of incidental durotomies (20 cases, 17.6%). In 3 cases (2.6%) therapy with a lumbar drain was necessary.
Conclusions
The rate of early recurrent LDH within days of surgery is 1.2%. Age seems to be an important factor in early recurrent LDH while obesity does not. The data of the German Spine Register seems to have a reliable data collection system that can perform multicentre data analysis. The databases from this Register could be used in the future for various purposes, such as the evaluation of multicentre surgical techniques, results in patients with various surgical procedures and basic research in spine surgery.
Similar content being viewed by others
Background
The recurrence rate in lumbar disc herniations (LDH) has been reported to be 5 to 25%. Nowadays there are only few data about this phenomenon that occur within days of the initial operation. The most affected segment is L4/5 [1,2,3]. On the other hand, there are few data available on the incidence of recurrence while the patient is still in hospital [4, 5].
Currently it is not clear which factors exert an influence on the genesis of this recurrency. Due to the biomechanics of the pathology, advanced age and pre-existing conditions such as overweight and obesity, as well as the localisation of the affected segment could play a role in the pathology [2, 6,7,8].
Methods
The aim of this study is that with the help of the available data of the German Spine Register (DWG register), the question should be answered, how often an early recurrence can be expected during the inpatient stay after microsurgical Lumbar nucleotomy.
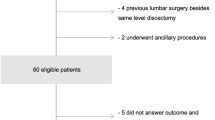
From 1st January 2012 to 31st December 2016, 9310 intervertebral disc operations were recorded using the DWG Register. These data were analysed for the occurrence of early recurrence and for any risk factors for this. With regard to all patients with lumbar disc herniation (n = 9310), 115 early recurrences were detected (1.2%).
Results
We found 115 early recurrences (1.2%) in 9310 surgical procedures due to a lumbar disc herniation.
The mean age of patients with an early recurrence was 70 ± 2.50 years with 75 women and 50 men.
The segment L4 / 5 (n = 47, 41%) was most frequently affected, followed by the segment L3 / 4 (n = 45, 39%) and the segment L5 / S1 (n = 23, 20%).
Regarding Body Mass Index (BMI): 4 patients (3.5%) were underweight (< 20 BMI), 45 (39%) were of normal weight (20–25 BMI), 45 (39%) patients were overweight (26–30 BMI), 19 (16.8%) had Grade 1 obesity (31–35 BMI) and 2 (1.7%) had Grade 2 obesity (> 35 BMI).
A dura-injury occurred in n = 20 (17.6%), while n = 3 (2.6%) had to be treated with a lumbar drainage system.
Of the patients treated for a herniated disc (n = 84, 82%), 18 (17%) experienced an improvement in their symptoms, while none (0.9%) experienced no relief.
For a detailed view of the overall results, see Table 1.
Discussion
This analysis of data from the DWG Register from 9310 patients shows an early recurrence rate of 1.2%. The L4 / 5 segment is most frequently affected. Misleadingly, one might come to the premature conclusion that the most frequently affected segment would be L5 / S1 [2], as it represents biomechanically represents the location of maximum lumbar region mobility. Considering our results and the data presented in the literature, it would be useful if spinal biomechanics were more closely examined in terms of the pathogenesis of recurrences in future studies [2].
Due to the loss of elasticity of the tissue, which can create conditions for a primary prolapse, age is a very important factor in the pathogenesis of this pathology [6, 8]. This is also confirmed by the data we obtained in our study. However, obesity may not be a factor in the development of early relapse, as this pathology may not be due to the biomechanics of the L4 / L5 segment, since axial load over the intervertebral space may be of little concern for recurrence [2, 7].
Occasionally, as a result of the enormous compression of the epidural veins in to the spinal canal through the Lumbar Disc Herniation, significant postoperative bleeding with considerable compression of the neural structures as well as an early Lumbar Disc Herniation recurrence may occur after decompression (Fig. 1).
MRI T2 weight from the Lumbar spine. a and b show a massive Lumbar Disc Herniation in the Segment L4/L5 in sagital and axial views. c and d show after 36 h an early recurrent disc herniation with postoperative Bleeding (↑) and compression of the Cauda Equina causing bowel and bladder retention in sagital and axial views
Most of our patients experience an improvement of their symptoms in the following days. This could be explained by the preservation of the nerve structures without Wallerian-degeneration and per se lack of pain or neurological deficits with an improvement in symptoms during the days following surgery by this early recurrent Lumbar Disc Herniation [9,10,11,12,13,14].
The main limitation in our study is the retrospective data collection with its inherent bias, typical from this study design, with possible inconsistences in documentation. Furthermore it is not possible to differentiate with the data in the register, whether the cause for this early recurrent Lumbar Disc Herniation is remaining intervertebral disc tissue or a true recurrence.
Conclusion
With help from the The German Spine Society Register we found a frequence of 1.2% in early recurrent LDH. Hence the German Spine Society Register seems to have a reliable data collection system that can perform multicentre data analysis. This data supports similar epidemiological studies to come to consistent values. The databases from this Register could be used in the future for various purposes, such as the evaluation of multicentre surgical techniques, results from patients with various surgical procedures and basic research in spinal surgery.
References
Yaman ME, Kazancı A, Yaman ND, Baş F, Ayberk G. Factors that influence recurrent lumbar disc herniation. Hong Kong Med J. 2017;23:258–63.
Berjano P, Pejrona M, Damilano M. Microdiscectomy for recurrent L5-S1 disc herniation. Eur Spine J. 2013;22:2915–7.
Penning L, Wilmink JT, van Woerden HH. Inability to prove instability. A critical appraisal of clinical-radiological flexion-extension studies in lumbar disc degeneration. Diagn Imaging Clin Med. 1984;53:186–92.
Herron L. Recurrent lumbar disc herniation: results of repeat laminectomy and discectomy. J Spinal Disord. 1994;7:161–6.
Guzmán J, Esmail R, Karjalainen K, Malmivaara A, Irvin E, Bombardier C. Multidisciplinary bio-psycho-social rehabilitation for chronic low back pain. Cochrane Database Syst Rev. 2002;1:CD000963. Comment in: Evid Based Nurs, 2002; 5: 116
Fehlings MG, Tetreault L, Nater A, Choma T, Harrop J, Mroz T, et al. The aging of the global population: the changing epidemiology of disease and spinal disorders. Neurosurgery. 2015;4:S1–5.
Singh DC, Yue JK, Metz LN, Winkler EA, Zhang WR, Burch S, et al. Obesity is an independent risk factor of early complications after revision spine surgery. Spine. 2016;41:E632–403.
Yao Y, Liu H, Zhang H, Wang H, Zhang C, Zhang Z, et al. Risk factors for the recurrent herniation after microendoscopic discectomy. World Neurosurg. 2016;95:451–5.
Baker GA, Cizik AM, Bransford RJ, Bellabarba C, Konodi MA, Chapman JR, et al. Risk factors for unintended durotomy during spine surgery: a multivariate analysis. Spine J. 2012;12:121–6.
Yoshihara H, Chatterjee D, Paulino CB, Errico TJ. Revision surgery for “real” recurrent lumbar disk herniation: a systematic review. Clin Spine Surg. 2016;29:111–8.
Buchmann N, Preuß A, Gempt J, Ryang YM, Vazan M, Stoffel M, et al. Outcome after surgical treatment for late recurrent lumbar disc herniations in standard open microsurgery. World Neurosurg. 2016;89:382–6.
Albayrak S, Ozturk S, Durdag E, Ayden Ö. Surgical management of recurrent disc herniations with microdiscectomy and long-term results on life quality: detailed analysis of 70 cases. J Neurosci Rural Pract. 2016;7:87–90.
Le H, Sandhu FA, Fessler RG. Clinical outcomes after minimal-access surgery for recurrent lumbar disc herniation. Clinical outcomes after minimal-access surgery for recurrent lumbar disc herniation. Neurosurg Focus. 2003;15:E12.
Laus M, Bertoni F, Bacchini P, Alfonso C, Giunti A. Recurrent lumbar disc herniation: what recurs? (A morphological study of recurrent disc herniation). Chir Organi Mov. 1993;78:147–54.
Acknowledgments
The publication costs for this article were covered in full by a grant from the Colorado Physician Insurance Company (http://www.copic.com) to Philip F. Stahel, MD.
COPIC had no influence on authorship or scientific content of this article.
Funding
No funding was received for this research.
Availability of data and materials
The datasets generated and/or analysed during the current study are available in the [DWG-register home page] repository, [https://dwg.memdoc.org/].
Author information
Authors and Affiliations
Consortia
Contributions
VRJ: carried out main manuscript writing and also literature research. SAM: carried out the statistical analysis. VBM: contributed with ideas and literature searching. MGF: contributed with Figures and tables and also manuscript writing. MF: Senior reviewer and owner of the idea in this research. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable
Competing interests
All authors certify that they have no affiliations with or involvement in any organisation or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Vinas-Rios, J.M., Sanchez-Aguilar, M., Medina Govea, F.A. et al. Incidence of early postoperative complications requiring surgical revision for recurrent lumbar disc herniation after spinal surgery: a retrospective observational study of 9,310 patients from the German Spine Register. Patient Saf Surg 12, 9 (2018). https://doi.org/10.1186/s13037-018-0157-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13037-018-0157-1