Abstract
Background
Evidence on the effectiveness of printed educational messages in contributing to increasing evidence-based clinical practice is contradictory. Nonetheless, these messages flood physician offices, in an attempt to promote treatments that can reduce costs while improving patient outcomes.
This study evaluated the ability of printed educational messages to promote the choice of thiazides as the first-line treatment for individuals newly diagnosed with hypertension, a practice supported by good evidence and included in guidelines, and one which could reduce costs to the health care system.
Methods
The study uses a pragmatic, cluster randomized controlled trial (randomized by physician practice group).
Setting
The setting involves all Ontario general/family practice physicians.
Messages advising the use of thiazides as the first-line treatment of hypertension were mailed to each physician in conjunction with a widely read professional newsletter. Physicians were randomized to receive differing versions of printed educational messages: an “insert” (two-page evidence-based article) and/or one of two different versions of an “outsert” (short, directive message stapled to the outside of the newsletter). One outsert was developed without an explicit theory and one with messages developed targeting factors from the theory of planned behaviour or neither (newsletter only, with no mention of thiazides).
The percentage of patients aged over 65 and newly diagnosed with hypertension who were prescribed a thiazide as the sole initial prescription medication. The effect of the intervention was estimated using a logistic regression model estimated using generalized estimating equation methods to account for the clustering of patients within physician practices.
Results
Four thousand five hundred four physicians (with 23,508 patients) were randomized, providing 97 % power to detect a 5 % absolute increase in prescription of thiazides. No intervention effect was detected. Thiazides were prescribed to 27.6 % of the patients who saw control physicians, 27.4 % for the insert, 26.8 % for the outsert and 28.3 % of the patients who saw insert + outsert physicians, p = 0.54.
Conclusions
The study conclusively failed to demonstrate any impact of the printed educational messages on increasing prescribing of thiazide diuretics for first-line management of hypertension.
Trial registration
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
The cost-effectiveness of treatment options, particularly for the treatment of common health conditions, can have a large impact on the cost of health care. At the time of the conduct of the present trial, over a third of Canadians between the ages of 18 and 74 years had hypertension [1]; and despite the fact that only a fraction of these individuals were being treated [2], prescription drugs used in the treatment of hypertension are the leading therapeutic category of prescription drugs in Canada, accounting for 20 % of total prescription drug sales [3]. Decisions concerning the medical management of hypertension therefore have the potential to have a significant impact on health care costs.
Initial treatment of hypertension with thiazide diuretics has been shown to significantly reduce morbidity and mortality, with benefits at least as great as with other classes of antihypertensive drugs, at less cost [4]. Yet in Canada and elsewhere, there is evidence of low adherence to published recommendations that thiazides be used as the first-line treatment for patients with uncomplicated hypertension [2]. The cost to patients and insurers may be high: one study estimated savings of $13.8 million (in US dollars in the year 2000) for Canada (year 2000 population 31,281,100) by using thiazides as the first-line antihypertensive drug [2]. Since most individuals with hypertension were not being treated [2, 5], more aggressive screening and treatment of hypertension would markedly increase the number of prescriptions and thus the beneficial economic impact of choosing thiazides over other antihypertensive treatment.
Printed educational messages (PEMs) directed to physicians are one way to address health care gaps that are under physician influence. While PEMs have the advantages of low cost and easy dissemination, there is great uncertainty about their effects. Several early systematic reviews concluded that printed materials, on their own, do not lead to change in physician practices [6, 7]. However, Grimshaw observed that the median effect in the RCTs where guidelines were disseminated as PEMs was 8.1 % absolute risk reduction (range +3.6 to +17.0 %) [8], on par with other much more expensive interventions like audit and feedback or academic outreach, and this result was the main stimulus for the current trial. A subsequent larger review of PEMs observed a smaller effect size, showing a median absolute risk difference of 0.02 (range 0 to 0.11) in seven RCTs reporting categorical outcomes and a standardized mean difference of 0.13 (range −0.16 to 0.36) in three RCTs reporting continuous outcomes [9]. A recent review of trials of PEMs for improving physician behaviour specifically in primary care settings did not show significant improvement in physician behaviour across included trials [10].
The uncertainty in the evidence leaves policy makers uncertain about the role of PEMs, at a time when closing evidence-to-practice gaps has become a more cost-effective investment of health system resources than developing new interventions [11].
Reviews cannot overcome limitations of the primary evidence: the small number of trials (of varying size) and methodological weaknesses (insufficient power to detect modest effects, unit of analysis errors). Thus, there is a need for a pragmatic [12], randomized controlled trial on the effect of PEMs on guideline adherence, conducted in real-world settings, on typical practitioners, taking into account group practices. Given the simplicity and low cost of PEM-based practice change programs, and the large population impact that even modest improvements may achieve when applied to all potential beneficiaries, a large trial is needed.
We developed and used four criteria to identify important evidence/practice gaps in Ontario primary care on which to test the impact of PEMs in a pragmatic trial: the gap is large and important to patients; it involves a common disorder; evidence-based practice is not constrained by structural or financial barriers; and process indicators exist that are measurable using the administrative datasets available to us.
The present study addresses these criteria by targeting first-line treatment of uncomplicated hypertension using a thiazide diuretic. This clearly qualifies as an important primary care gap involving a common disorder not constrained by structural or financial barriers and for which routinely collected administrative data could be used to evaluate an intervention. If the above-mentioned modest impact on clinical practice of PEMs is applied, then at the trivial cost of a letter to each physician, Ontario’s health care system stands to save over $1 million, at current levels of treatment of hypertension [2, 5], with correspondingly greater savings if identification and treatment of hypertension is improved. The Ontario Printed Educational Materials (OPEM) trial aimed to evaluate different forms of PEMs: long inserts compared to shorter bullet-pointed outserts and different forms of outserts. We hypothesized that active arms would be superior to control, that individually, different forms of PEMs would be similarly effective on prescribing thiazides, and would be more effective when combined and when developed using a theory of behaviour.
Methods
The interventions
informed was a free, peer-reviewed, evidence-based practice synopsis, mailed to nearly 15,000 primary care providers in Ontario from 1994 to January 2007 (when publication ceased). Articles were developed by clinical and research staff from the Institute for Clinical Evaluative Sciences (ICES).
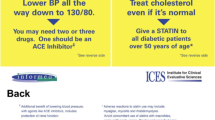
Two types of PEMs addressed the identified evidence-practice gap: a two-page article, indistinguishable from the rest of the newsletter in size and style (the “insert”) and two versions of a short, directive, evidence-based PEM on a postcard-sized card stapled to the front page of informed (the “outsert”). The insert and one of the versions of the outsert (the atheoretical outsert) were developed without any explicit theory of action using input from a diverse group of physicians who identified barriers to evidence-based practice and from a communications expert. The second outsert (the theory of planned behaviour-based outsert) was developed by a group consisting of three health psychologists and two implementation researchers with experience using theories of behaviour. Full details about the development process for this outsert are described in the study protocol [13]. The addition of the “theory of planned behaviour-based” outsert allowed us to test the hypothesis that a message inspired by a psychological theory, specifically the theory of planned behaviour [14] (TPB), would be more effective in changing clinical behaviour toward more evidence-based practice than a message designed without an explicit theoretical basis. The study design is shown in Table 1. Table 2 shows the two versions of the outserts, and the insert is included in Additional file 1. The interventions were included with the July 2005 edition of informed.
Data sources
Ontario has a single-payer public health insurance system, in which necessary medical and hospital care and prescription drugs are covered for all Ontario residents aged 65 years and older. The following administrative data sources from this insurance plan were used [15, 16]:
-
The OHIP Claim History Database details payments to health care professionals, including an encoded provider number unique to each health care professional, an anonymous, encoded patient identifier unique to each patient, the service provided and the service date.
-
The Canadian Institute for Health Information (CIHI) Discharge Abstract Database (DAD) contains the primary and up to 24 secondary diagnoses for all discharges from acute care hospitals.
-
The OHIP Registered Persons Database (RPDB) contains basic demographic, place of residence and vital status information for each insured person.
-
The OHIP Corporate Provider Database contains demographic and practice information for each physician.
-
The Ontario Drug Benefit (ODB) Program database contains prescription drug claims data for eligible beneficiaries (age over 65, patients on social assistance and qualifying for Trillium [low income] drug program) of the program, including an encoded prescriber identifier.
Records from these datasets were linked, using unique, encoded patient and physician identifiers and analysed at the Institute for Clinical Evaluative Sciences (ICES; www.ices.on.ca), to determine which individuals were newly treated for hypertension during the study period, and which of the target physicians prescribed their antihypertensive medication.
Study practices
All Ontario physicians with an active general/family practice in Ontario in 2003/2004 were eligible for inclusion. “Active” practice was defined as having a total billing volume for the year of at least $50,000 and writing prescriptions for at least 100 different patients (aged 65 years and older), with at least one prescription in at least 10 of the 12 months.
Physician identifiers were linked to the College of Physicians and Surgeons of Ontario (CPSO) number at ICES. CPSO numbers were then hand-linked to the publicly available CPSO database (www.cpso.on.ca) to obtain practice addresses.
Trials of interventions aimed at changing clinical practice must be randomized at the level at which they are directed—in this case, the family physician. In a group practice, doctors may share information. To prevent contamination, we randomized at the level of the practice. Physicians were placed into practices on the basis of a shared address.
Study patients
The Ontario Drug Benefit database was used to identify Ontario residents who filled one or more prescriptions for an antihypertensive medication between July 11, 2005, and July 24, 2006. To ensure that these individuals were started on an antihypertensive agent for treatment of hypertension and not another indication, the cohort was linked with the CIHI DAD, the RPDB and the ODB Database. We excluded those patients with OHIP claims within 3 years or CIHI claims within 4 years (or any antihypertensive medications prescribed within 1 year) for any of the following conditions: myocardial infarction or angina, heart failure, arrhythmias, renal disease (including nephropathy), liver disease (including oesophageal varices), stroke or transient ischemic attack, hyperthyroidism or migraines [17]. Consistent with guideline recommendations for treatment of hypertension [18], we focused on thiazide prescribing as the first-line treatment in individuals with uncomplicated hypertension. In order to ensure that the cohort included only individuals newly treated for hypertension, individuals who had filled a prescription for any antihypertensive medication in the year prior to the intervention were also excluded [17]. Only the first prescription for an antihypertensive filled during the observation year was included; all prescriptions filled on the same day were taken into consideration when determining the outcome. While data were available for individuals 65 years and over, all individuals included in the study were at least 66 years old at the time they filled their first prescription for an antihypertensive medication in order to ensure that information covering a 1-year look back period for prior prescriptions was available.
Using the OHIP physician claims database, we identified the physician seen during the 14 days prior to and including the date the antihypertensive prescription was filled. In some cases, more than one study physician was selected. (Patients who had not visited any of the study physicians during the 14-day period were not included in the analysis.) We included patient visits to the physician’s office, physician visits to the patient’s home or to a patient in a long-term care facility and physician phone calls to the patient.
Study design
The study was a pragmatic, factorial, cluster-randomized controlled trial with the physician practice as the unit of randomization. Practices were randomly assigned to one of six intervention groups by the study statistician (see Table 1), using computer-generated random numbers. Patient and physician participants were unaware of allocation and administrative data were collected without knowledge of the research under way. Full details of the study design can be seen in the published protocols [13, 19, 20].
Outcomes
The objectives of the study were to determine whether the format of the PEM affected the likelihood that the only medication initially prescribed for hypertension was a thiazide and whether a theory of planned behaviour-based approach to developing the message was any more effective than a PEM developed without use of explicit theory. A “successful” outcome was a first-line prescription for a thiazide and no other antihypertensive medication. Combinations of a thiazide plus potassium or a potassium-sparing medication were counted as a “success”; combinations of a thiazide plus another diuretic were counted as a “failure”. A prescription for any non-thiazide antihypertensive medication was also counted as a “failure”.
Power
Even a 5 % improvement in the prevalence of care for common conditions represents a meaningful health benefit. Based on pilot data, Monte Carlo simulations, assuming an intracluster correlation coefficient of 0.092, three patients per physician, a baseline success rate of 0.36 and absolute intervention effects of 0.05, 0.075 and 0.10, demonstrated that a trial with 1250 practices per arm would provide over 97 % power to detect a 5 % increase, and over 98 % power to distinguish between the effects of the combined intervention and either alone, assuming the combined effect to be additive. This original power calculation was based on testing the effectiveness of the insert and one version of the outsert. We conducted a follow-up simulation to assess whether we could test a second version of the outsert (theory of planned behaviour-based), which suggested that the power would be greater than 80 %. The research opportunity that this modification presented was judged to outweigh the loss of power. These decisions were made during the design phase and prior to randomization, as detailed in our published protocols [13, 19, 20].
Statistical analysis
Logistic regression was used to test the hypothesis that the intervention affected the choice of first-line medication for hypertension. While the unit of randomization was the physician practice, outcomes were measured at the individual patient level. The logistic regression model was estimated using generalized estimating equations (GEE) to account for the clustering of patients within physician practices [21]. This method of analysis allows for the inclusion of patient-level and physician-level covariates (e.g. patient age, physician age), while at the same time accounting for possible correlations amongst patient outcomes within a practice.
Analysis was on an intention-to-treat basis. As shown in Table 3, models were fit to test: insert and both outserts combined, and insert and two outserts split (theory of planned behaviour-based vs. atheoretical). These were fit using unadjusted (regressions 1a and 2a) models and models adjusting for patient- and physician-level covariates (regressions 1b and 2b). The full model in 1b included interaction terms between the intervention and each covariate, to determine whether the impact of the intervention depended on patient and/or physician characteristics.
Patient and physician characteristics were compared between randomization arms using chi-square tests for categorical variables and Kruskal-Wallis tests for continuous variables.
All analyses were performed at ICES using SAS version 9 (SAS Institute, Cary, North Carolina). Two-tailed p values less than or equal to 0.05 were considered to be significant.
Results
Physician and patient selection
Figure 1 shows the number of physicians and patients included in the study. Three quarters of Ontarians aged 66 years and older filled a prescription for an antihypertensive medication in the year following the mail-out, but almost all (92 %) had already filled a prescription for an antihypertensive medication during the preceding year. A further 38 % of those who filled a prescription for the first time were excluded because there was evidence that the antihypertensive might have been prescribed for a reason other than hypertension. We identified 38,102 individuals who were taking medication for hypertension for the first time and were able to link the prescriptions of 23,508 of these individuals to one of the physicians targeted by the intervention (Fig. 1). Thirteen percent of family physicians randomized to receive one of the interventions were excluded from the analysis because they were not linked to at least one patient newly treated for hypertension.
Physician and patient characteristics
There were small, statistically significant but clinically unimportant, differences between the characteristics of the physicians in the six intervention groups (Table 4).
Analysis of intervention effects
The intracluster correlation coefficient was 0.18 (95 % confidence interval 0.16 to 0.19). Intervention effects are shown in Table 3. Neither the unadjusted nor the adjusted results show evidence that any of the interventions, alone or in combination, were effective. The widest confidence interval reported in the table, an odds ratio between 0.91 and 1.21 for the insert + TPB-based outsert corresponds to a true absolute effect of the intervention lying between a decrease of 1.5 % and an increase of 3.5 %. Thus, not only did the intervention fail to achieve statistical significance but as well the confidence interval does not contain values of much practical importance.
While the probability of being prescribed a thiazide as the first-line drug depended on both physician and patient characteristics, there was no indication that the interventions themselves were any more or less effective in any physician or patient sub-group. The p values for the interactions between the intervention and the physician/patient variables were all non-significant, ranging from 0.15 to 0.97.
Discussion
This printed information intervention was designed to increase physician prescribing of thiazides as the first-line pharmaceutical treatment for hypertension. The interventions, evaluated in a very large trial, with sufficient power to detect a small change in physician behaviour, failed to change prescribing practice. This confirms the results of studies [22] that found no impact of mailing the Ontario hypertension guidelines to all physicians in Ontario.
Given the pragmatic and representative nature of our study, we propose that these results may apply also to primary care practitioners in other health care settings with universal health insurance and no cost to patient for drugs.
This is the first published trial reporting a head-to-head comparison of TPB-based vs. atheoretical implementation interventions. Although this trial did not detect any difference in effectiveness between these two approaches to intervention, this question needs further research.
We found that only 27.5 % of the individuals newly started on antihypertension medication were started on only a thiazide. This is similar to the rate of 29 % reported by Morgan et al. [3] for another Canadian jurisdiction (although Morgan et al. included patients whose first hypertension treatment was a thiazide diuretic along with another antihypertensive drug, in addition to those who received only a thiazide diuretic) but lower than the 35 % rate reported for Ontario between 1994 and 2002 [17].
Female patients and older patients were more likely to be prescribed thiazides as first-line treatment, corresponding to patterns observed elsewhere [3, 17, 23]. Female physicians, physicians who had been in practice longer, physicians in group practices and physicians practicing in rural locations were more likely to prescribe thiazides as first-line treatment (Table 3).
Depending on the condition being treated, improvements in prescribing patterns have the potential to save patients/insurers money as well as improving patient outcomes. It is therefore important to pursue other ways of changing prescribing practices. Several studies report that a combination of prescribing feedback plus educational intervention is effective in increasing the rate of thiazide prescribing [24–26]. The Canadian Hypertension Education Program (CHEP) has been able to produce sustained improvements in the clinical management of hypertension by combining annual updates of its recommendations with an extensive implementation program that includes both passive and active dissemination, including workshops and academic detailing [27].
An economic analysis found that if the initial improvements in practice can be sustained, they may be cost-effective [2, 28]. Furthermore, cost-effectiveness of these interventions should improve as changes in patient demographics mean that physicians are likely to see increasing numbers of patients with hypertension in their practices.
A strength of our study was the use of informed as the vehicle carrying the PEMs into physician offices. The effectiveness of printed educational materials depends, firstly, on whether they are read. In 1997, The Strategic Council Inc. contacted 500 Ontario physicians by phone to determine readership and recall of informed. They found that 71 % of the respondents recalled receiving informed and that of these, 89 % found it useful or very useful and 53 % read most or every issue [29]. Two surveys of informed subscribers, conducted in 1995 and 1999, found that the newsletter was a respected and valued source of information [29]. It is unlikely, then, that the failure of this study to change outcomes was related to the perceived trustworthiness of the source or the failure of the physicians to notice the messages.
Another strength of the study was the use of administrative data, which allowed us to examine the impact of our interventions across the full spectrum of physicians and patients in Ontario. This strength also imposes some limitations, one of which is the inability to study non-fee-for-service physicians. However, it is estimated that only 2 % of Ontario primary care physicians were on alternative payment plans whose billings did not appear in OHIP claims at the time of the study [30].
A second limitation imposed by reliance on administrative data is that we cannot differentiate between failure of the PEM to be delivered, read or remembered, failure of the physician to advise the patient and failure of the patient to act on that advice. While the Canadian postal service is highly reliable, and the addresses used are equally so, it is possible that, despite the widely recognized brand of informed as an evidence-based newsletter from a respected research institute (rather than a product marketing leaflet), it may not have been received by study physicians. This is a possible fate for all PEMs and so does not detract from our main conclusion that PEMs do not change practice.
From the perspective of patient health, interventions are useful only if they affect the treatment the patient receives. This was a pragmatic trial, designed to give a definitive answer about the value of a particular mode of information transmission for the purpose of improving health care. The trial was not designed to explain the barriers that remained. We did however investigate the reasons that may explain the lack of observed effect in a theory-based process evaluation conducted alongside the trial [31].
Conclusions
Consistent with systematic review findings [9], this study supports the conclusion that PEMs, whether long and discursive, or short and directive, and whether based on a theory of behaviour or no theory at all, did not, on their own, bring about an effective change in physician prescribing, even in the absence of financial and structural barriers to change.
References
Joffres MR, Hamet P, MacLean DF, L’italien GJ, Fodor G. Distribution of blood pressure and hypertension in Canada and the United States. Am J Hypertens. 2001;14:1099–105.
Fretheim A, Aaserud M, Oxman A. The potential savings of using thiazides as the first choice antihypertensive drug; cost-minimisation analysis. BMC Health Serv Res. 2003;3:18.
Morgan S, Bassett KL, Wright JM, Yan L. First-line first? Trends in thiazide prescribing for hypertensive seniors. PLoS Med. 2005;2, e80.
ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA. 2002;288(23):2981–97.
Wolf-Maier K, Cooper RS, Banegas JR, Giampaoli S, Hense H-W, Joffrew M, et al. Hypertension prevalence and blood pressure levels in 6 European countries, Canada, and the United Stats. JAMA. 2003;289:2363–9.
Lomas J. Words without action? The production, dissemination and impact of consensus recommendations. Ann Rev Pub Health. 1991;12:41–65.
Implementing clinical practice guidelines: can guidelines be used to improve clinical practice? Effective Health Care. Dec 1994, Vol 8. Nuffield Institute for Health, University of Leeds. Centre for Health Economics and the NHS Centre for Review and Dissemination, University of York.
Grimshaw JM, Thomas RE, Maclennan G, Fraser C, Ramsay CR, Vale L, et al. Effectiveness and efficiency of guideline dissemination and implementation strategies. Health Technol Assess. 2004;8:iii–iv. 1-72.
Giguère A, Légaré F, Grimshaw J, Turcotte S, Fiander M, Grudniewicz A, Makosso-Kallyth S, Wolf FM, Farmer AP, Gagnon MP. Printed educational materials: effects on professional practice and healthcare outcomes. Cochrane Database of Syst Rev. 2012; (10):Art. No.: CD004398. doi:10.1002/14651858.CD004398.pub3.
Grudniewicz A, Kealy R, Rodseth RN, Hamid J, Rudoler D, Straus SE. What is the effectiveness of printed educational materials on primary care physician knowledge, behaviour, and patient outcomes: a systematic review and meta-analyses. Implement Sci. 2015;10(1):164.
Woolf SH, Johnson RE. The break-even point: when medical advances are less important than improving the fidelity with which they are delivered. Ann Fam Med. 2005;3:545–52.
Schwartz D, Lellouch J. Explanatory and pragmatic attitudes in therapeutic trials. J Chron Dis. 1967;20:637–48.
Francis JJ, Grimshaw JM, Zwarenstein M, Eccles MP, Shiller S, Godin G, Johnston M, O’Rourke K, Presseau J, Tetroe J. Testing a TheoRY-inspired MEssage (‘TRY-ME’): a sub-trial within the Ontario Printed Educational Message (OPEM) trial. Implement Sci. 2007;2:39.
Ajzen I. The theory of planned behaviour. Organ Behav Hum Decis Process. 1991;50:179–211.
Ontario Ministry of Health and Long-Term Care. Ontario health planning data guide, Release 3.0. February 28, 2006. Accessed 15 August 2016 at http://www.ontla.on.ca/library/repository/mon/13000/260075.pdf
Hux JE, Ivis F, Flintoft V, Bica A. Diabetes in Ontario: determination of prevalence and incidence using a validated administrative data algorithm. Diabetes Care. 2002;25:512–6.
Tu K, Campbell NR, Chen Z, McAlister FA. Thiazide diuretics for hypertension: prescribing practices and predictors of use in 194,761 elderly patients with hypertension. Am J Geriatr Pharmacother. 2006;4:161–7.
Campbell N. 2004 CHEP hypertension recommendations. Perspectives in Cardiology. 2004;20:26–33.
Zwarenstein M, Hux JE, Kelsall D, Paterson M, Grimshaw J, Davis D, Laupacis A, Evans M, Austin PC, Slaughter PM, Shiller SK, Croxford R, Tu K. The Ontario printed educational message (OPEM) trial to narrow the evidence-practice gap with respect to prescribing practices of general and family physicians: a cluster randomized controlled trial, targeting the care of individuals with diabetes and hypertension in Ontario, Canada. Implement Sci. 2007;2:37.
Grimshaw JM, Zwarenstein M, Tetroe JM, Godin G, Graham ID, Lemyre L, Eccles MP, Johnston M, Francis JJ, Hux J, O’Rourke K, Légaré F, Presseau J. Looking inside the black box: a theory-based process evaluation alongside a randomised controlled trial of printed educational materials (the Ontario printed educational message, OPEM) to improve referral and prescribing practices in primary care in Ontario, Canada. Implement Sci. 2007;2(1):38.
Austin PC. A comparison of the statistical power of different methods for the analysis of cluster randomization trials with binary outcomes. Stat Med. 2007;26:3550–65.
Tu K, Mamdani MM, Tu JV. Hypertension guidelines in elderly patients: is anybody listening? Am J Med. 2002;113:52–8.
Walley T, Duggan AK, Haycox AR, Nizio CH. Treatment for newly diagnosed hypertension: patterns of prescribing and antihypertensive effectiveness in the UK. J R Soc Med. 2003;96:525–31.
Herbert CP, Wright JM, Maclure M, Wakefield J, Dormuth C, Brett-MacLean P, et al. Better prescribing project: a randomized controlled trial of the impact of case-based educational modules and personal prescribing feedback on prescribing for hypertension in primary care. Fam Pract. 2004;21:575–82.
Fretheim A, Aaserud M, Oxman AD. Rational prescribing in primary care (RaPP): economic evaluation of an intervention to improve professional practice. PLoS Med. 2006;3, e216.
Simon SR, Majumdar SR, Prosser LA, Salem-Schatz S, Warner C, Kleinman K, et al. Group versus individual academic detailing to improve the use of antihypertensive medications in primary care: a cluster-randomized controlled trial. Am J Med. 2005;118:521–8.
Hemmelgarn BR, Chen G, Walker R, McAlister FA, Quan H, Tu K, et al. Trends in antihypertensive drug prescriptions and physician visits in Canada between 1996 and 2006. Can J Cardiol. 2008;24:507–12.
Simon SR, Rodrigues HP, Majumdar SR, Kleinman K, Warner C, Salem-Schatz S, Miroshnik I, Soumerai SB, Prosser LA. Economic analysis in a randomized trial of academic detailing interventions to improve use of antihypertensive medications. J Clin Hypertens. 2007;9:15–20.
Diane Kelsall, former editor of informed, personal communication.
Chan BTB, Schultz SE. Supply and utilization of general practitioner and family physician services in Ontario. ICES Investigative Report. Toronto: Institute for Clinical Evaluative Sciences; 2005.
Presseau J, Grimshaw JM, Tetroe JM, Eccles MP, Francis JJ, Godin G, Graham ID, Hux JE, Johnston M, Légaré F, Lemyre L, Robinson N, Zwarenstein M. (under review). A theory-based process evaluation alongside a randomized controlled trial of printed educational messages to increase primary care physicians’ prescription of thiazide diuretics for hypertension [ISRCTN72772651]. Implement Sci.
Acknowledgements
This study was also supported by the Institute for Clinical Evaluative Sciences (ICES), which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). The opinions, results and conclusions reported in this paper are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred. Parts of this material are based on data and information compiled and provided by the Canadian Institute for Health Information (CIHI). However, the analyses, conclusions, opinions and statements expressed herein are those of the author and not necessarily those of CIHI. We thank the IMS Brogan Inc. for the use of their Drug Information Database. Dr. Austin is supported in part by a Career Investigator Award from the Heart and Stroke Foundation of Canada (Ontario office). Dr. Tu receives a Research Scholar Award from the Department of Family and Community Medicine at the University of Toronto.
Funding
(Canadian Institutes of Health Research, award number 724180703) The Canadian Institutes of Health Research had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; or in the preparation, review or approval of the manuscript.
Availability of data and materials
The raw data cannot be shared as it is held within ICES for use under government and research ethics board mandated conditions and may not be released. Materials used are available in Table 2 and Additional file 1.
Authors’ contributions
MZ conceived the study, wrote the protocol and led the analysis and write-up of results. He takes responsibility for the integrity of the data and the accuracy of the data analysis. JH, JG, PA, SS and AL contributed to protocol development and design. SS, PS, KT, JH, DK and MZ contributed to the design of the insert, outsert and patient reminders. JF, JG, ME, GG and MJ contributed to the development of the theory-based message. RC, JG, JP, GG, JT, JF, MJ and LY contributed to the analysis and write-up. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The research protocol was approved by the Research Ethics Board at the Sunnybrook Health Sciences Centre.
Author information
Authors and Affiliations
Corresponding author
Additional file
Additional file 1:
Under pressure: the latest on managing hypertension. (PDF 291 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Zwarenstein, M., Grimshaw, J.M., Presseau, J. et al. Printed educational messages fail to increase use of thiazides as first-line medication for hypertension in primary care: a cluster randomized controlled trial [ISRCTN72772651]. Implementation Sci 11, 124 (2015). https://doi.org/10.1186/s13012-016-0486-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13012-016-0486-3