Abstract
Objective
To study the role of recombinant human LH supplementation in women with hypo-response to ovarian stimulation.
Methods
We performed a systematic review and meta-analysis of prospective clinical trials in which recombinant FSH monotherapy protocols were compared with LH-supplemented protocols in hypo-responders. A search was conducted of the Scopus, MEDLINE databases without time or language restrictions. Primary outcome was clinical pregnancy rate.
Results
Significantly higher clinical pregnancy rates (odds ratio: 2.03, P = 0.003), implantation rates (odds ratio: 2.62, P = 0.004) and number of oocytes retrieved (weight mean differences: 1.98, P = 0.03) were observed in hypo-responders supplemented with recombinant LH versus hypo-responders who underwent FSH monotherapy. No differences in terms of mature oocytes or miscarriage rates were found between the two groups.
Conclusion
In conclusion, our analysis confirms that women with a hypo-response to exogenous gonadotropins might benefit from LH supplementation. However, more trials are required before a definitive conclusion can be drawn.
Similar content being viewed by others
Introduction
An appropriate ovarian response to controlled ovarian stimulation (COS) is crucial for the success of assisted reproductive technologies (ART) [1]. The number of oocytes retrieved at the end of stimulation is the parameter most often used to assess ovarian response to exogenous gonadotropin and is strictly related to live birth rate [2]. Based on ovarian biomarkers and oocyte number, women are classically defined as poor, normal or hyper-responders [1, 3]. However, there is a specific subgroup of women termed “hypo-responders” who have an unexpectedly poor or suboptimal response to gonadotropin therapy despite adequate ovarian pre-stimulation parameters [4, 5].
Hypo-responders are hyposensitive to standard age, ovarian biomarkers, and BMI-matched doses of exogenous FSH [4,5,6]. This ovarian resistance to gonadotropin stimulation might clinically manifest as an “initial slow response” [7, 8] or be retrospectively diagnosed in women who require higher-than-expected doses of gonadotropins on the basis of age, BMI, and ovarian reserve [9]. The hypo-responder patient differs from the classic poor responder patient in at least two aspects. First, in hypo-responders, the number of oocytes is retrieved is higher than three, albeit at the expense of elevated gonadotropin consumption, whereas in classic poor responders, the number of oocytes retrieved is usually lower irrespective of the amount of gonadotropin administered. Second, hypo-responders have normal ovarian reserve tests (i.e., anti-Müllerian hormone and antral follicle count), which are usually deranged in women with the classic poor ovarian response.
The reasons for the hypo-responsiveness to gonadotropin stimulation are not entirely understood, but it has been suggested that genetic mutations or single nucleotide polymorphisms (SNPs) of gonadotropins and their receptors might influence ovarian sensitivity to exogenous gonadotropins [6, 10,11,12]. Hypo-responders undergoing ART treatments might face increased treatment costs, decreased cumulative live birth rates, and increased time to live birth, suggesting a negative impact on fertility. Yet, is still unclear how to most optimally manage this group of patients, although recent evidence suggests that hypo-responders might benefit from recombinant LH (rLH) supplementation during ovarian stimulation [13,14,15]. Physiologically, LH activity is crucial for proper folliculogenesis. Indeed, in the late follicular phase, granulosa cells are receptive to LH which can sustain follicular growth even when exogenous FSH administration is discontinued [16]. While the indiscriminate use of LH supplementation remains equivocal in normal responders, who are characterized by a normal function of the gonadal axis, the addition of LH supplementation in hypo-responders may be clinically beneficial as these patients can harbor polygenic traits affecting the functional properties of endogenous gonadotropins and/or their receptors [11]. To verify these preliminary observations, we aggregated the available published data of prospective clinical trials on the effect of rLH supplementation in hypo-responders using meta-analysis. Our aim was to summarize the evidence on the clinical utility of adding rLH to COS in hypo-responders undergoing ART.
Methods
Search strategy
We conducted a systematic search using Medline/PubMed and Scopus databases to identify all relevant studies. The search terms used, alone or combined, were “luteinizing hormone”, “recombinant LH”, “rLH”, “rhLH”, “ovulation induction”, “assisted reproductive technology”, “ART”, “in vitro fertilization”, “IVF”, “steady response”, “hyporesponse” (Additional file 1: Table S1). Hand searches of relevant review articles and reference lists were carried out. No time restriction and language restriction were applied and the end date for all searches was March 2018.
Eligibility and data extraction
We included only prospective clinical trials in which recombinant human FSH (rFSH) alone protocols were compared with rFSH + rLH supplementation in women undergoing IVF/ICSI with a hypo-response to exogenous rFSH monotherapy. Hypo-response was defined according to authors’ criteria of included studies provided they met with our inclusion criteria. Specifically, hypo-responders were normogonadotropic women who required an elevated total dose of rFSH (> 2500 IU) to obtain an adequate number of oocytes retrieved or who had a plateau on follicular growth with no or only marginal increase in the estradiol level and in the follicular size during stimulation. Data extraction was performed independently by three authors (IS, PD and AF) using predefined data fields.
Outcome measures
The primary outcome was clinical pregnancy rate (defined as the number of clinical pregnancies, i.e., presence of one or more gestational sacs with foetal heart beat seen at ultrasound examination at 6–8 weeks, expressed per started cycle. Secondary outcomes were the number of oocytes retrieved and number of metaphase II (MII) oocytes, implantation rate (defined as the number of gestational sacs observed divided by the number of embryos transferred), and live birth rate (defined as the number of deliveries per started cycles).
Protocol
This study was exempt from institutional review board approval because it did not involve any human intervention. We adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [17].
Study selection
First, the titles and abstracts of all articles were screened. Duplications were removed using both Endnote online software and manually. Disagreements were resolved by discussion among authors. The full texts of eligible articles published were subsequently obtained. The grey literature, namely, unpublished studies and those published outside widely available journals, case reports, conference proceedings, doctoral theses, dissertations, etc., was not considered [18] (Additional file 1: Table S1).
Bias assessment
Three authors (IS, PD and AF) independently assessed the risk of bias of the studies eligible for the review using the checklist created by the Cochrane Menstrual Disorders and Subfertility Group [19]. The quality of allocation concealment was graded as adequate (A), unclear (B) or inadequate (C). Non-randomized trials were assessed using the Newcastle–Ottawa Scale (NOS) and each study was judged on three issues: selection of the study group, comparability between groups, and ascertainment of exposed and non-exposed cohorts [20].
Risk of bias across the studies was assessed by multiple analyses (Additional file 2: Table S2). Funnel plots of the primary outcome were evaluated both visually and formally with the ‘trim and fill’ method and the Egger test [21, 22].
Quantitative analysis
Statistical analysis was carried out using Review Manager 5.3 (The Nordic Cochrane Centre, The Cochrane Collaboration). Categorical data were combined with a pooled odds ratio (OR) using the Mantel-Haenszel method. Continuous data were combined with weight mean differences (WMD) using the inverse variance method. The meta-analysis was conducted using the fixed-effect-model (FEM) or the random effect model (REM). REM was used in case of significant heterogeneity among studies. Heterogeneity was assessed using the percentage of total variation in the estimated effect across studies (I2). An I2 value > 50% indicates substantial heterogeneity. P values < 0.05 were considered statistically significant.
Subgroup and sensitivity analysis
Subgroup analyses were carried out by study type, namely, randomized controlled trials and non-randomized controlled trials to identify potential sources of heterogeneity. Sensitivity analysis was carried out to assess the leverage of studies judged to be at high risk of bias (Additional file 3: Table S3). In detail, the risk of bias was evaluated considering the following issues: study design; imprecision (effect size with wide confidence interval), concerns regarding random sequence generation and allocation concealment.
Results
Study selection and characteristics
A total of 5906 items were identified in the Medline/PubMed (N = 3670) and Scopus databases (n = 2236) (Fig. 1). Duplications were removed by Endnote Online (N = 368). Abstracts and titles (N = 5538) were reviewed by two authors (AC, FC). Disagreements were resolved by discussion with senior authors (CA, SE, GD). Twenty-five full-text papers were assessed for eligibility. Twenty studies were excluded because they did not fulfill the inclusion criteria [23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42] (Additional file 4: Table S4). Five studies met the inclusion criteria and were included in our review. The characteristics of the studies and the risk of bias are reported in Table 1 and Additional file 2: Table S2.
Summary of results
Clinical pregnancy rate
Clinical pregnancy rates were investigated in three RCTs [7,8,9] and in one cohort study [43] for a total of 361 participants (Fig. 2). The clinical pregnancy rate was significantly higher in the rFSH plus rLH group than in the rFSH alone group (OR 2.03, 95% CI 1.27–3.25, P = 0.003). The consistency in the direction of the effect, and the overlap in confidence intervals across studies increases confidence in the results. Sensitivity analysis indicated that removing the papers that were considered to have a high risk of bias [9, 43] did not affect the pooled effect size.
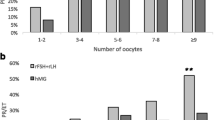
Number of oocytes retrieved
Two RCTs [7, 8] and one cohort study [43], for a total of 319 participants, were analyzed (Fig. 3). The estimated pooled increase in the number of oocytes retrieved was 1.98 (WMD 1.98, 95% CI 0.17 to 3.80, I2 = 78%; P = 0.03), thus indicating a positive association between the use of rLH supplementation and number of oocyte retrieved in hypo-responders. To assess the cause of the heterogeneity, subgroup analysis was performed according to by study type. Heterogeneity was reduced to 0% in the RCT studies, suggesting that the difference between studies is explained by study type. The observed pooled effect size was larger for RCTs, with a higher number of oocytes retrieved compared to non-RCT (P = 003; Fig. 3). Sensitivity analysis indicated that removal of the study that had a high risk of bias [43] had no material effect on the results.
Number of metaphase II oocytes
Two RCTs [7, 9] and one cohort study [43], for a total of 257 subjects, were pooled. Additional file 5: Figure S1). Overall, no significant difference was observed between patients stimulated with rFSH + rLH and those with rFSH monotherapy in terms of number of MII oocytes retrieved (WMD 0.61, 95% CI -2.08 to 3.31; I2 = 90%). In subgroup analysis, the study type did not explain the heterogeneity between studies. Sensitivity analysis indicated that removal of the study with a high risk of bias [43] did not affect the pooled effect estimates.
Implantation rates
Four RCTs [7,8,9, 44] and one cohort study [43] for a total of 766 subjects, were analyzed (Fig. 4). The estimated pooled increase in implantation rates was 2.62 (95% CI OR 1.37–4.99, I2 = 52%, P = 0.004) favoring the rFSH + rLH group versus the rFSH alone group. The heterogeneity estimates were not materially affected by performing analyses separately by study type. However, heterogeneity in low risk of bias studies was reduced to 40% compared to 52% in the overall analysis (Additional file 3: Table S3), which suggests that some of the differences between studies are explained by study quality. These results are therefore consistent in suggesting a positive association between rLH supplementation and implantation rates, but they also indicate the need for additional studies to confirm the size of this association. Sensitivity analysis indicated that removal of studies with a high risk of bias [43, 44] did not affect the pooled effect estimates.
Live birth rates
Live birth rates were investigated in only one RCT [8]. As shown in Additional file 6: Figure S2, live birth rates were significantly higher in the rFSH + rLH group than in the rFSH alone group (OR 2.44, 95% CI 1.03–2.77, P = 0.04).
Miscarriage rate
Two RCTs [7, 8] and one cohort study [43] for a total of 319 participants, were pooled in this meta-analysis (Additional file 7: Figure S3). Overall, there was no significant difference in the estimated pooled miscarriage rate between patients stimulated with rFSH + rLH and patients on rFSH monotherapy (OR 1.01, 95% CI 0.52–1.99; I2 = 0%). Subgroup analysis demonstrated that study type had no material effect on the results. Similarly, sensitivity analyses showed that the removal of the study with a high risk of bias [43] did not affect the pooled effect size.
Risk of bias across studies
The risk of a significant bias across studies regarding the primary outcome (clinical pregnancy rate) was excluded by Egger’s test (P = 0.642), which is confirmed by visual inspection of the funnel plots and the trim and fill method (Additional file 8: Figure S4).
Discussion
Summary of evidence
This meta-analysis indicates that women with ovarian resistance to exogenous gonadotropin who undergo COS for ART, the so-called “hypo-responders”, might benefit from rLH supplementation. The use of rLH supplementation was associated with increased clinical pregnancy, number of oocytes retrieved, and implantation rates, whereas no effect was noted concerning the number of MII oocytes and risk of miscarriage. The effect on live birth was less clear as to date, only one trial has reported LBRs in hypo-responders co-treated with rLH versus rFSH monotherapy during COS [8].
Interpretation of results and clinical considerations
The concept of hypo-response to exogenous gonadotropin was introduced over a decade ago to describe women who have an impaired response to ovarian stimulation [5, 45, 46]. These normo-ovulatory and normo-gonadotropic women differ from classical poor responders in the sense that they are usually younger and have a normal age-matched ovarian reserve [13]. This ovarian resistance can clinically manifest as an “initial slow response” or “stagnation” in follicle growth during ovarian stimulation with FSH monotherapy [7, 8]. In particular, stagnation was defined by an absence or only marginal growth of both follicles and estradiol levels during OS. In other cases, a hypo-response can be retrospectively diagnosed in women who require higher-than-expected doses of gonadotropins on the basis of age, BMI and ovarian reserve [9, 47]. The trends seen in this meta-analysis are consistent with a beneficial effect of rLH supplementation during ovarian stimulation.
The mechanism by which rLH exerts its beneficial effect in hypo-responders is not fully understood. However, the fact that these patients and normal responders to gonadotropin stimulation share similar phenotypic characteristics suggests a genotype-based mechanism [10, 12, 48,49,50]. In other words, these women might have a peculiar genotype profile that could influence their response to ovarian stimulation. Since hypo-responders exhibit serum LH levels comparable to those of normal responders, it has been hypothesized that either the endogenous LH molecule or the LH receptor, or both, are functionally deficient and, therefore, implicated in the pathogenesis of hypo-response. Indeed, it has been reported that patients with a less functional common LH β chain variant have an increased resistance to gonadotropin stimulation [11, 51]. Furthermore, preliminary data show that even specific LH receptor polymorphisms could influence ovarian response during COS [52, 53]. In a previous study, we found that the prevalence of hypo-response was higher in carriers of the Serine variant of a common FSH-R polymorphism than in wild-type haplotypes [54]. Polymorphism of the FSH-R promoter was also associated with an impaired response to ovarian stimulation, i.e., higher consumption of exogenous gonadotropin in A allele carriers than in G allele carriers [55, 56].
It is, therefore, biologically plausible that LH supplementation in women with genetic polymorphisms involving gonadotropins and their receptors might overcome the genetically determined ovarian resistance to gonadotropin stimulation. In line with this hypothesis, Ramaraju et al. observed that both women heterozygous or homozygous for the G allele required higher doses of rLH supplementation during OS than those without these genetic traits; in their study, the use of rLH supplementation resulted in increased clinical pregnancy rates [57]. The added LH during stimulation acts on theca cells and increases androgen synthesis, which in turn improve FSH receptor sensitivity during COS [58,59,60]. This hypothesis should be verified in specific trials and could be a fruitful research topic.
As for the type of LH activity, rLH seems to be associated with better outcomes in hypo-responders than hMG. Indeed, a significantly lower implantation rate was observed in hypo-responders treated with hMG than with rLH [8]. This observation might be explained by the differential effect of LH activity provided by LH and hCG-containing drugs on the endometrium. Current evidence suggests that hCG (versus rLH) might adversely affect the endometrial function [61, 62]. Indeed, this phenomenon might explain why ongoing pregnancy rates are higher in frozen embryo transfer (FET) using natural cycles with spontaneous LH surge compared to natural cycles with exogenous hCG [63].
Additionally, there are differential biological activity of these two molecules on granulosa cells. Recombinant LH exerts both proliferative and antiapoptotic actions through phosphorylated extracellular-regulated kinase 1/2 (pERK1/2) and phosphorylated AKT signals [64]. By contrast, LH activity provided by hCG, contained in hMG formulations, displays a steroidogenic and proapoptotic effect mediated by cAMP and protein kinase A (PKA) [64]. These molecular differences might translate in improved pregnancy success among IVF patients treated with rLH rather than hMG, as shown in a 2017 large meta-analysis [14].
Limitations and strengths
The main limitation of this study is the low number of trials conducted thus far. Ovarian resistance to gonadotropin stimulation remains a largely undervalued issue in the reproductive field. This may be because until recently, most clinicians did not consider the issue of hypo-responsiveness if the number of oocytes retrieved after stimulation was consistent with women’s reproduction potential and the antral follicle count at the beginning of stimulation. Indeed, previous systematic reviews investigated the role of rLH supplementation without distinguishing hypo-response from other conditions such a poor or normal response [19, 65]. In a 2014 meta-analysis for a total of 1129 ART cycles in POR patients supplemented or not with rLH illustrates this phenomenon [66]. In fact, it was noted that more oocytes were retrieved in rLH-supplemented cycles than with rFSH monotherapy (12 studies, n = 1077; weighted mean difference + 0.75 oocytes; 95% CI 0.14–1.36). In that study, the use of rLH supplementation also improved clinical pregnancy rates (14 studies, n = 1179; relative risk [RR] 1.30; 95% confidence interval [CI] 1.01–1.67; intention-to-treat population [ITT] population). Nevertheless, a careful examination of the included studies reveals that the beneficial effect of rLH was more pronounced in studies involving hypo-responders than in those with classic POR. The inclusion of studies involving hypo-responders in the Lehert et al. (2014) review thus explains the overall favorable results observed with rLH supplementation in the POR patient.
The merit of our review is that, albeit at the cost of a low number of observations, it focused on prospective clinical trials involving the specific subgroup of hypo-responders. Moreover, the low heterogeneity among trials utilized in our meta-analyzes concerning the primary outcome provides evidence that the observed effect was causal. Nevertheless, heterogeneity was high among most secondary outcomes, which might be partially explained by study type and quality, as the subgroup and sensitivity analyses demonstrated. Furthermore, different protocols and rLH dosages were used in the studies examined. It was not possible to evaluate outcomes according to the dosage and time of LH administration due to the low number of studies. Only one trial demonstrated that 150 IU of rLH result in more oocytes retrieved and a higher percentage of mature oocytes than do 75 IU in a long GnRH agonist protocol [23]. Along the same lines, the effect of rLH supplementation in hypo-responders undergoing OS with GnRH antagonists remains to be established, as the trials included in this meta-analysis utilized pituitary suppression with GnRH agonist. Despite the low number of studies and high heterogeneity in some of the outcome measures, there was no evidence of publication bias. Furthermore, sensitivity analyses demonstrated minimal differences when studies with high risk of bias were excluded, thus indicating our results are conservative.
Future research
Ovarian resistance to exogenous gonadotropin still represents an undervalued topic in the reproductive field. There is a lack of a standardized definition and limited knowledge about its pathophysiology mechanisms. Two years ago, hypo-responsiveness to gonadotropin stimulation was included in a novel stratification system, designated the POSEIDON criteria, for infertility patients undergoing ART [4, 67, 68]. Novel markers that accurately reflect the “dynamic” nature of follicular growth in response to exogenous gonadotropin are under investigation, an example being the follicle-to-oocytes index (FOI), which is the ratio between the number of oocytes retrieved and AFC at the beginning of stimulation [69]. A better understanding of the effect exerted by genetic polymorphisms of gonadotropins and their receptors, and subsequently COS outcomes, will help to improve treatment and counseling for patients seeking ART.
Additional studies, in particular those that assess various LH supplementation doses and regimes, including GnRH antagonists and cumulative LBR as the main outcome measure, are required. Such studies might increase the precision of the estimated effect sizes, thus allowing better appraisal of the clinical importance of our findings.
Conclusion
In conclusion, our analyses indicate that women with a previous hypo-response to exogenous FSH stimulation benefit from LH supplementation as a means of increasing clinical pregnancy, implantation, and number of oocytes retrieved. LH supplementation might be added during COS on the same cycle to rescue an ongoing hypo-response or in a subsequent cycle. Further research is required to quantify the effect of LH supplementation more precisely and to evaluate the clinical utility of LH supplementation in hypo-responders using the GnRH antagonist protocol.
Change history
14 March 2019
.
References
La Marca A, Sunkara SK. Individualization of controlled ovarian stimulation in IVF using ovarian reserve markers: from theory to practice. Hum Reprod Update. 2014;20:124–40.
Sunkara SK, Rittenberg V, Raine-Fenning N, Bhattacharya S, Zamora J, Coomarasamy A. Association between the number of eggs and live birth in IVF treatment: an analysis of 400 135 treatment cycles. Human Reprod. 2011;26:1768–74.
Conforti A, Cariati F, Vallone R, Alviggi C, de Placido G. Individualization of treatment in controlled ovarian stimulation: myth or reality? Biochimica Clinica. 2017;41:294–305.
Alviggi C, Andersen CY, Buehler K, Conforti A, De Placido G, Esteves SC, et al. A new more detailed stratification of low responders to ovarian stimulation: from a poor ovarian response to a low prognosis concept. Fertil Steril. 2016;105:1452–3.
Devroey P, Fauser BC, Diedrich K. Approaches to improve the diagnosis and management of infertility. Hum Reprod Update. 2009;15:391–408.
Esteves SC, Humaidan P, Alviggi C, Fischer R. The novel POSEIDON stratification of 'Low prognosis patients in Assisted Reproductive Technology' and its proposed marker of successful outcome. F1000Research. 2016;23;5:2911.
De Placido G, Alviggi C, Perino A, Strina I, Lisi F, Fasolino A, et al. Recombinant human LH supplementation versus recombinant human FSH (rFSH) step-up protocol during controlled ovarian stimulation in normogonadotrophic women with initial inadequate ovarian response to rFSH. A multicentre, prospective, randomized controlled trial. Human Reprod. 2005;20:390–6.
Ferraretti AP, Gianaroli L, Magli MC, D'Angelo A, Farfalli V, Montanaro N. Exogenous luteinizing hormone in controlled ovarian hyperstimulation for assisted reproduction techniques. Fertil Steril. 2004;82:1521–6.
Ruvolo G, Bosco L, Pane A, Morici G, Cittadini E, Roccheri MC. Lower apoptosis rate in human cumulus cells after administration of recombinant luteinizing hormone to women undergoing ovarian stimulation for in vitro fertilization procedures. Fertil Steril. 2007;87:542–6.
Alviggi C, Conforti A, Esteves SC. Impact of mutations and polymorphisms of gonadotrophins and their receptors on the outcome of controlled ovarian stimulation. Principles and Practice of Controlled Ovarian Stimulation in ART. 2015147–56.
Alviggi C, Pettersson K, Longobardi S, Andersen CY, Conforti A, De Rosa P, et al. A common polymorphic allele of the LH beta-subunit gene is associated with higher exogenous FSH consumption during controlled ovarian stimulation for assisted reproductive technology. Reprod Biol Endocrinol. 2013;11:51.
Conforti A, Alfano S, De Rosa P, Alviggi C, De Placido G. The role of gonadotropin polymorphisms and their receptors in assisted reproductive technologies and controlled ovarian stimulation: a prospective observational study. Italian J Gynaecol Obstet. 2017;29:15–21.
Alviggi C, Conforti A, Esteves SC, Andersen CY, Bosch E, Bühler K, et al. Recombinant luteinizing hormone supplementation in assisted reproductive technology: a systematic review. Fertil Steril. 2018;109:644–64.
Santi D, Casarini L, Alviggi C, Simoni M. Efficacy of follicle-stimulating hormone (FSH) alone, FSH + luteinizing hormone, human menopausal gonadotropin or FSH + human chorionic gonadotropin on assisted reproductive technology outcomes in the "personalized" medicine era: a meta-analysis. Front Endocrinol. 2017;8:114.
Alviggi C, Clarizia R, Mollo A, Ranieri A, De Placido G. Who needs LH in ovarian stimulation? Reprod BioMed Online. 2011;22(Suppl 1):S33–41.
Filicori M. Use of luteinizing hormone in the treatment of infertility: time for reassessment? Fertil Steril. 2003;79:253–5.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ (Clinical research ed). 2009;339:b2700.
Conn VS, Valentine JC, Cooper HM, Rantz MJ. Grey literature in meta-analyses. Nurs Res. 2003;52:256–61.
Mochtar MH, Van der V, Ziech M, van Wely M. Recombinant Luteinizing Hormone (rLH) for controlled ovarian hyperstimulation in assisted reproductive cycles. The Cochrane database of systematic reviews. 2007Cd005070.
Wells G, Shea B, O’connell D, Peterson J, Welch V, Losos M, et al. Quality Assessment Scales for Observational Studies. Ottawa Health Research Institute 2004.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ (Clinical research ed). 1997;315:629–34.
Sutton AJ, Duval SJ, Tweedie RL, Abrams KR, Jones DR. Empirical assessment of effect of publication bias on meta-analyses. BMJ (Clinical research ed). 2000;320:1574–7.
De Placido G, Alviggi C, Mollo A, Strina I, Ranieri A, Alviggi E, et al. Effects of recombinant LH (rLH) supplementation during controlled ovarian hyperstimulation (COH) in normogonadotrophic women with an initial inadequate response to recombinant FSH (rFSH) after pituitary downregulation. Clin Endocrinol. 2004;60:637–43.
Bosch E, Labarta E, Crespo J, Simon C, Remohi J, Pellicer A. Impact of luteinizing hormone administration on gonadotropin-releasing hormone antagonist cycles: an age-adjusted analysis. Fertil Steril. 2011;95:1031–6.
Marrs R, Meldrum D, Muasher S, Schoolcraft W, Werlin L, Kelly E. Randomized trial to compare the effect of recombinant human FSH (follitropin alfa) with or without recombinant human LH in women undergoing assisted reproduction treatment. Reprod BioMed Online. 2004;8:175–82.
De Placido G, Mollo A, Alviggi C, Strina I, Varricchio MT, Ranieri A, et al. Rescue of IVF cycles by HMG in pituitary down-regulated normogonadotrophic young women characterized by a poor initial response to recombinant FSH. Human Reprod. 2001;16:1875–9.
Balasch J, Creus M, Fabregues F, Civico S, Carmona F, Puerto B, et al. The effect of exogenous luteinizing hormone (LH) on oocyte viability: evidence from a comparative study using recombinant human follicle-stimulating hormone (FSH) alone or in combination with recombinant LH for ovarian stimulation in pituitary-suppressed women undergoing assisted reproduction. J Assist Reprod Genet. 2001;18:250–6.
Cedrin-Durnerin I, Grange-Dujardin D, Laffy A, Parneix I, Massin N, Galey J, et al. Recombinant human LH supplementation during GnRH antagonist administration in IVF/ICSI cycles: a prospective randomized study. Human Reprod. 2004;19:1979–84.
Garcia-Velasco JA, Coelingh Bennink HJ, Epifanio R, Escudero E, Pellicer A, Simon C. High-dose recombinant LH add-back strategy using high-dose GnRH antagonist is an innovative protocol compared with standard GnRH antagonist. Reprod BioMed Online. 2007;15:280–7.
Griesinger G, Schultze-Mosgau A, Dafopoulos K, Schroeder A, Schroer A, von Otte S, et al. Recombinant luteinizing hormone supplementation to recombinant follicle-stimulating hormone induced ovarian hyperstimulation in the GnRH-antagonist multiple-dose protocol. Human Reprod. 2005;20:1200–6.
Humaidan P, Bungum M, Bungum L, Yding AC. Effects of recombinant LH supplementation in women undergoing assisted reproduction with GnRH agonist down-regulation and stimulation with recombinant FSH: an opening study. Reprod BioMed Online. 2004;8:635–43.
Lahoud R, Ryan J, Illingworth P, Quinn F, Costello M. Recombinant LH supplementation in patients with a relative reduction in LH levels during IVF/ICSI cycles: a prospective randomized controlled trial. Eur J Obstet Gynecol Reprod Biol. 2017;210:300–5.
Levi-Setti PE, Cavagna M, Bulletti C. Recombinant gonadotrophins associated with GnRH antagonist (cetrorelix) in ovarian stimulation for ICSI: comparison of r-FSH alone and in combination with r-LH. Eur J Obstet Gynecol Reprod Biol. 2006;126:212–6.
Musters AM, van Wely M, Mastenbroek S, Kaaijk EM, Repping S, van der Veen F, et al. The effect of recombinant LH on embryo quality: a randomized controlled trial in women with poor ovarian reserve. Human Reprod. 2012;27:244–50.
NyboeAndersen A, Humaidan P, Fried G, Hausken J, Antila L, Bangsboll S, et al. Recombinant LH supplementation to recombinant FSH during the final days of controlled ovarian stimulation for in vitro fertilization. A multicentre, prospective, randomized, controlled trial. Human Reprod. 2008;23:427–34.
Pezzuto A, Ferrari B, Coppola F, Nardelli GB. LH supplementation in down-regulated women undergoing assisted reproduction with baseline low serum LH levels. Gynecol Endocrinol. 2010;26:118–24.
Sauer MV, Thornton MH 2nd, Schoolcraft W, Frishman GN. Comparative efficacy and safety of cetrorelix with or without mid-cycle recombinant LH and leuprolide acetate for inhibition of premature LH surges in assisted reproduction. Reprod BioMed Online. 2004;9:487–93.
Sills ES, Levy DP, Moomjy M, McGee M, Rosenwaks Z. A prospective, randomized comparison of ovulation induction using highly purified follicle-stimulating hormone alone and with recombinant human luteinizing hormone in in-vitro fertilization. Human Reprod. 1999;14:2230–5.
Tarlatzis B, Tavmergen E, Szamatowicz M, Barash A, Amit A, Levitas E, et al. The use of recombinant human LH (lutropin alfa) in the late stimulation phase of assisted reproduction cycles: a double-blind, randomized, prospective study. Human Reprod. 2006;21:90–4.
Humaidan P, Chin W, Rogoff D, D'Hooghe T, Longobardi S, Hubbard J, et al. Efficacy and safety of follitropin alfa/lutropin alfa in ART: a randomized controlled trial in poor ovarian responders. Human Reprod. 2017;32:544–55.
Lisi F, Rinaldi L, Fishel S, Caserta D, Lisi R, Campbell A. Evaluation of two doses of recombinant luteinizing hormone supplementation in an unselected group of women undergoing follicular stimulation for in vitro fertilization. Fertil Steril. 2005;83:309–15.
Westergaard LG, Laursen SB, Andersen CY. Increased risk of early pregnancy loss by profound suppression of luteinizing hormone during ovarian stimulation in normogonadotrophic women undergoing assisted reproduction. Human Reprod. 2000;15:1003–8.
Yazici Yilmaz F, Gorkemli H, Colakoglu MC, Aktan M, Gezginc K. The evaluation of recombinant LH supplementation in patients with suboptimal response to recombinant FSH undergoing IVF treatment with GnRH agonist down-regulation. Gynecol Endocrinol. 2015;31:141–4.
Lisi F, Rinaldi L, Fishel S, Lisi R, Pepe GP, Picconeri MG, et al. Use of recombinant LH in a group of unselected IVF patients. Reprod BioMed Online. 2002;5:104–8.
Alviggi C, Clarizia R, Mollo A, Ranieri A, De Placido G. Outlook: who needs LH in ovarian stimulation? Reprod BioMed Online. 2006;12:599–607.
Alviggi C, Mollo A, Clarizia R, De Placido G. Exploiting LH in ovarian stimulation. Reprod BioMed Online. 2006;12:221–33.
Lisi F, Rinaldi L, Fishel S, Lisi R, Pepe G, Picconeri MG, et al. Use of recombinant FSH and recombinant LH in multiple follicular stimulation for IVF: a preliminary study. Reprod BioMed Online. 2001;3:190–4.
La Marca A, Papaleo E, Alviggi C, Ruvolo G, De Placido G, Candiani M, et al. The combination of genetic variants of the FSHB and FSHR genes affects serum FSH in women of reproductive age. Hum Reprod. 2013;28:1369–74.
Alviggi C, Conforti A, Fabozzi F, De Placido G. Ovarian stimulation for IVF/ICSI cycles: a pharmacogenomic approach. Medecine Therapeutique Medecine de la Reproduction, Gynecologie et Endocrinologie. 2009;11:271–7.
Alviggi C, Conforti A, Santi D, Esteves SC, Andersen CY, Humaidan P, et al. Clinical relevance of genetic variants of gonadotrophins and their receptors in controlled ovarian stimulation: a systematic review and meta-analysis. Hum Reprod Update. 2018;24:599–614.
Alviggi C, Clarizia R, Pettersson K, Mollo A, Humaidan P, Strina I, et al. Suboptimal response to GnRHa long protocol is associated with a common LH polymorphism. Reprod BioMed Online. 2011;22(Suppl 1):S67–72.
Lindgren I, Baath M, Uvebrant K, Dejmek A, Kjaer L, Henic E, et al. Combined assessment of polymorphisms in the LHCGR and FSHR genes predict chance of pregnancy after in vitro fertilization. Human Reprod. 2016;31:672–83.
Alviggi C, Conforti A, Cariati F, Alfano S, Strina I, Huhtaniemi I, et al. Abstracts of the 32nd annual meeting of the European Society of Human Reproduction and Embryology. Hum Reprod. 2016;31:i1–i513.
Alviggi C, Conforti A, Caprio F, Gizzo S, Noventa M, Strina I, et al. In Estimated Good Prognosis Patients Could Unexpected "Hyporesponse" to Controlled Ovarian Stimulation be Related to Genetic Polymorphisms of FSH Receptor? Reprod Sci. 2016;23:1103–8.
Achrekar SK, Modi DN, Desai SK, Mangoli VS, Mangoli RV, Mahale SD. Poor ovarian response to gonadotrophin stimulation is associated with FSH receptor polymorphism. Reprod BioMed Online. 2009;18:509–15.
Desai SS, Achrekar SK, Pathak BR, Desai SK, Mangoli VS, Mangoli RV, et al. Follicle-stimulating hormone receptor polymorphism (G-29A) is associated with altered level of receptor expression in granulosa cells. J Clin Endocrinol Metab. 2011;96:2805–12.
Ramaraju GA, Cheemakurthi R, Prathigudupu K, Balabomma KL, Kalagara M, Thota S, et al. Role of Lh polymorphisms and r-hLh supplementation in GnRh agonist treated ART cycles: a cross sectional study. Eur J Obstet Gynecol Reprod Biol. 2018;222:119–25.
Bosdou JK, Venetis CA, Dafopoulos K, Zepiridis L, Chatzimeletiou K, Anifandis G, et al. Transdermal testosterone pretreatment in poor responders undergoing ICSI: a randomized clinical trial. Human Reprod. 2016;31:977–85.
Vendola KA, Zhou J, Adesanya OO, Weil SJ, Bondy CA. Androgens stimulate early stages of follicular growth in the primate ovary. J Clin Invest. 1998;101:2622–9.
Weil S, Vendola K, Zhou J, Bondy CA. Androgen and follicle-stimulating hormone interactions in primate ovarian follicle development. J Clin Endocrinol Metab. 1999;84:2951–6.
Evans J, Salamonsen LA. Too much of a good thing? Experimental evidence suggests prolonged exposure to hCG is detrimental to endometrial receptivity. Human Reprod (Oxford, England). 2013;28:1610–9.
Kyrou D, Kolibianakis EM, Fatemi HM, Grimbizis GF, Theodoridis TD, Camus M, et al. Spontaneous triggering of ovulation versus HCG administration in patients undergoing IUI: a prospective randomized study. Reprod BioMed Online. 2012;25:278–83.
Fatemi HM, Kyrou D, Bourgain C, Van den Abbeel E, Griesinger G, Devroey P. Cryopreserved-thawed human embryo transfer: spontaneous natural cycle is superior to human chorionic gonadotropin-induced natural cycle. Fertil Steril. 2010;94:2054–8.
Casarini L, Santi D, Brigante G, Simoni M. Two hormones for one receptor: evolution, biochemistry, actions, and pathophysiology of LH and hCG. Endocr Rev. 2018;39:549–92.
Mochtar MH, Danhof NA, Ayeleke RO, Van der Veen F, van Wely M. Recombinant luteinizing hormone (rLH) and recombinant follicle stimulating hormone (rFSH) for ovarian stimulation in IVF/ICSI cycles. Cochrane Database Syst Rev. 2017;5:Cd005070.
Lehert P, Kolibianakis EM, Venetis CA, Schertz J, Saunders H, Arriagada P, et al. Recombinant human follicle-stimulating hormone (r-hFSH) plus recombinant luteinizing hormone versus r-hFSH alone for ovarian stimulation during assisted reproductive technology: systematic review and meta-analysis. Reprod Biol Endocrinol. 2014;12:17.
Humaidan P, Alviggi C, Fischer R, Esteves SC. The novel POSEIDON stratification of 'Low prognosis patients in Assisted Reproductive Technology' and its proposed marker of successful outcome. F1000Research. 2016;5:2911.
Esteves SC, Roque M, Bedoschi GM, Conforti A, Humaidan P, Alviggi C. Defining low prognosis patients undergoing assisted reproductive technology: POSEIDON criteria-the why. Front Endocrinol. 2018;9:461.
Alviggi C, Conforti A, Esteves SC, Vallone R, Venturella R, Staiano S, et al. Understanding ovarian hypo-response to exogenous gonadotropin in ovarian stimulation and its new proposed marker-the follicle-to-oocyte (FOI) index. Front Endocrinol. 2018;9:589.
Acknowledgments
The authors thank Jean Gilder (Scientific Communication srl., Naples, Italy) for revising and editing the manuscript.
Funding
None.
Availability of data and materials
Not applicable.
Author information
Authors and Affiliations
Contributions
CA, AC, SE, FZ, GD participated in study design. CA, AC and SE wrote the first draft of the manuscript; AC performed the statistical analysis. FD contributed in the re-appraisal and revision of the manuscript. IS, PD and AF extracted data and assessed bias risk. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
Prof Alviggi reports personal fees and honoraria from Merck outside the submitted work. Prof. Esteves declares receipt of speaker’s fees from Merck, Lilly, and Besins outside the present study. Dr. Conforti, Dr. Di Rella Dr. Strina, Dr. De Rosa, Dr. Fiorenza, Prof Zullo and Prof. De Placido have nothing to disclose.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:
Table S1. Search and selection strategy. (DOCX 11 kb)
Additional file 2:
Table S2. Quality of study included. (DOCX 12 kb)
Additional file 3:
Table S3. Sensitivity analysis. (DOCX 13 kb)
Additional file 4:
TableS4. Excluded studies with reasons. (DOCX 12 kb)
Additional file 5:
Figure S1. Forest plot of weight mean difference for the number of metaphase II oocytes in rFSH + rLH versus rFSH alone treatment. (TIF 243 kb)
Additional file 6:
Figure S2. Forest plot of odds ratio for live birth rate in rFSH + rLH versus rFSH alone treatment. (TIF 107 kb)
Additional file 7:
Figure S3. Forest plot of odds ratio for miscarriage in rFSH + rLH versus rFSH alone treatment. (TIF 263 kb)
Additional file 8:
Figure S4. Funnel-plots and “trim and firm” analysis of primary outcome. (TIF 948 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Conforti, A., Esteves, S.C., Di Rella, F. et al. The role of recombinant LH in women with hypo-response to controlled ovarian stimulation: a systematic review and meta-analysis. Reprod Biol Endocrinol 17, 18 (2019). https://doi.org/10.1186/s12958-019-0460-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12958-019-0460-4