Abstract
Background
Visfatin has been reported to be associated with breast cancer progression, but the interaction between the visfatin and clinicopathologic factors in breast cancer progression status requires further investigation. To address this problem, it is better to simultaneously consider multiple factors in sensitivity and specificity assays.
Methods
In this study, a dataset for 105 breast cancer patients (84 disease-free and 21 progressing) were chosen. Individual and cumulative receiver operating characteristics (ROC) were used to analyze the impact of each factor along with interaction effects.
Results
In individual ROC analysis, only 3 of 13 factors showed better performance for area under curve (AUC), i.e., AUC > 7 for hormone therapy (HT), tissue visfatin, and lymph node (LN) metastasis. Under our proposed scoring system, the cumulative ROC analysis provides higher AUC performance (0.746–0.886) than individual ROC analysis in predicting breast cancer progression. Considering the interaction between these factors, a minimum of six factors, including HT, tissue visfatin, LN metastasis, tumor stage, age, and tumor size, were identified as being highly interactive and associated with breast cancer progression, providing potential and optimal discriminators for predicting breast cancer progression.
Conclusion
Taken together, the cumulative ROC analysis provides better prediction for breast cancer progression than individual ROC analysis.
Similar content being viewed by others
Background
A high occurrence of ongoing breast cancer progression and metastasis events influences quality of life and survival in breast cancer patients, providing a rationale for an in-depth analysis of the interaction among clinicopathologic factors [1], such as age, family history, genetic specificity, hormonal status and lifestyle [2,3,4,5,6,7]. Early diagnosis of breast cancer followed by local and/or systematic treatments produces high survival rates [8]. However, recurrence or metastasis of breast cancer is sometimes unavoidable and reduces survival rate [6].
Clinicopathologic factors such as age, tumor size, stage, nodal status, hormone receptor (HR) status (estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER2)) are widely considered in risk-adapted therapy decisions and as prognostic indicators for breast cancer progression [6, 7]. However, these factors are generally taken individually without considering possible mutual interactions.
Visfatin (nicotinamide phosphoribosyltransferase or NAMPT) [9] plays an important role in regulating metabolism, inflammation, and carcinogenesis [10, 11]. Visfatin was also reported to overexpress in many types of cancer, such as colorectal [12], prostatic [13], gastric [14], esophageal [15], and breast cancer [16,17,18,19,20]. Therefore, visfatin is considered to be an oncoprotein. Our previous study [21] reported that visfatin was highly expressed in breast cancer tissues and is associated with tumor size, ER negativity (−), PR (−), and poor disease-free/overall survival as well as low recurrence rates for hormone therapy. The correlation between visfatin and several clinicopathologic factors were analyzed individually [21], but possible interaction between visfatin and breast cancer progression-associated clinicopathologic factors has not been investigated. Moreover, the specificity and sensitivity of visfatin as an independent prognosis predictor for breast cancer has not been addressed.
Receiver operating characteristic (ROC) analysis is widely used to evaluate diagnostic test performance for predicting dichotomous results by comparing sensitivity versus specificity [22, 23]. ROC analysis is also used to evaluate the accuracy of various biomarkers for diagnosis, prognosis and survival predictions for cancer patients [24,25,26,27,28,29,30,31]. Recently, ROC analysis has been improved by simultaneously considering multiple factors in terms of cumulative ROC analysis [32,33,34].
Previously statistical analysis approaches for breast cancer prognosis typically depend on regression models, including logistic regression and the Cox proportional regression method. ROC analysis could provide another strategy for breast cancer prognosis based on sensitivity and specificity. In addition, possible interaction between visfatin and clinicopathologic factors in breast cancer progression has not been investigated. Thus, this study aims to evaluate the interaction effects of clinicopathologic factors in breast cancer progression and identifies high risk factors through cumulative ROC analysis.
Methods
Dataset information
The dataset was derived from our previous work [21] with Institutional Review Board (IRB) approval (KMUH-IRB-980567) and informed consent. A total of 105 female breast cancer patients treated with surgery but without radiotherapy or chemotherapy were enrolled at the Department of Surgery, Kaohsiung Medical University Hospital during 2003–2008. Data including visfatin levels and clinicopathological factors is downloadable at https://wp.kmu.edu.tw/changhw/files/2017/05/ROC_tissue-visfatin_dataset.xlsx.
Grouping for breast cancer progression
Breast cancer patients were classified into progressing and disease-free groups. The progressing group included patients with local/regional recurrence or distant metastasis of breast cancer along with those did not survive the follow-up period. The disease-free group included patients who remained disease-free for 60 months following initial diagnosis and who survived the follow-up period.
Clinicopathologic factors
As standard prognostic indicators for breast cancer progression [6, 7], we included 13 clinicopathologic factors: Visfatin positive cells (%), tumor stage, grade and size, age, body mass index (BMI), lymph node (LN) metastasis, radiotherapy (RT), chemotherapy (CT), hormone therapy (HT), and breast cancer molecular makers (ER, PR, and HER2).
Individual ROC analysis
Clinicopathologic factors were dichotomized by ROC curve analysis. The area under the ROC curve (AUC) is used to calculate the accuracy of dichotomous results for predicting the risk of breast cancer progression. A higher AUC value represents a better prognosis prediction for breast cancer progression.
Cumulative ROC analysis
To score cumulative ROC analysis, the top-ranked factors are ranked according to the AUC of individual ROC analysis. This system transforms individual ROC analysis data into dichotomous data for cumulative ROC analysis. In brief, the cutoff point for each clinicopathologic factor was determined from its individual ROC curve. Values of each factor either above or below its the cutoff point were respectively assigned scores of 1 and 0. All data were transformed into this scoring system for further cumulative ROC analysis.
Different factors were chosen to calculate their cumulative AUC values. This cumulative analysis began with selecting the first two factors with the top AUC values for an individual ROC. Other factors were then tested as the third one and the cumulative AUC value was calculated. Only the factor that provided the highest cumulative AUC value was kept. This process was repeated for other factor combinations. Accordingly, different numbers of clinicopathologic factors that generated the largest cumulative AUC value were selected to investigate the joint effects of clinicopathologic factors associated with breast cancer progression.
Statistical analyses
Table 1 summarizes the distribution of clinicopathologic factors between the disease-free and the progressing groups. The difference between both groups was estimated using the Fisher’s exact test or χ2 test. The dichotomous analysis for single and combinational clinicopathologic factors were determined by individual and cumulative ROC as mentioned above (2.3 and 2.4). Combining different factors, the likelihood ratio (LR) [23] was chosen to evaluate disease-free status in patients. LR+, i.e., sensitivity/(1 − specificity) [23], is the ratio of the probability of a positive test in the progressing patients to that of disease-free patients. In contrast, LR−, i.e., 1 − sensitivity)/specificity [23], is the ratio of the probability of a negative test in the progressing patients to that of disease-free patients. All statistical calculations were analyzed by STATA version 11.0.
Results
Clinicopathologic characteristics and progression of breast cancer
Disease progression developed in 21 (20.0%) of the 105 breast cancer patients tracked within 5-year follow-up. Table 1 summarizes the clinicopathologic characteristics of breast cancer patients in disease-free and progressing statuses. Compared to the disease-free patients, the progressing patients had a significantly higher proportion of tissue visfatin > 50% (81.0%), stage III/IV (52.4%), grade 3 (33.3%), age ≥ 52 years (76.2%), tumor size ≥ 2 cm (81.0%), LN metastasis (71.4%), triple negative subtype (38.1%), and hormone therapy (71.4%).
AUC for individual clinicopathologic factors for breast cancer progression
Table 2 presents the dichotomous results for the various single clinicopathologic factors listed in Table 1. Hormone therapy (AUC = 0.7143), tissue visfatin (AUC = 0.7083), and LN metastasis (AUC = 0.7083) show acceptable performance in the AUC results (≥ 0.7) under single factor analysis, indicating these clinicopathologic factors are acceptable prognosis factors for breast cancer progression. The AUC values for other factors were less than 0.7.
Cumulative ROC analysis of breast cancer progression
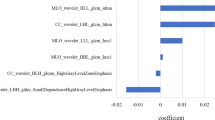
Our proposed cumulative ROC analysis scoring system was used to determine the combined effects of tissue visfatin and these clinicopathologic factors. As shown in Table 3, the cumulative AUC value for the combinations of cumulative top-ranked clinicopathologic factors was calculated using the AUC value for different factor combinations, where the factors were added individually in descending order of individual AUC value (Table 2). The scoring system obtained the highest AUC value (0.886) for the 6 cumulative top-ranked factors combination, including HT, tissue visfatin, LN metastasis, stage, age, and tumor size. AUC values increased from 0.764 to 0.886 for the cumulative top-ranked clinicopathologic factors, but decreased slightly after combining 7 or more cumulative top-ranked factors. Therefore, 6 dichotomized clinicopathologic factors yielded the best prognosis prediction for breast cancer progression.
Cumulative ROC analysis performance for predicting breast cancer progression
According to the cumulative top-ranked clinicopathologic factors scoring results, 6 selected dichotomized clinicopathologic factors provided scores ranging from 0 to 6 (Table 4). Both scores 1 and 2 have 100% sensitivity (i.e., all progressing patients are correctly classified). However, score 2 has a higher specificity compared to score 1 (45.24% vs 14.29%), indicating that score 2 can predict disease-free patients more precisely. Score 4 has the best result, with a correctly classification of 83.81% for disease progression with the best combination of sensitivity (76.19%) and specificity (85.71%) as well as good LR performance (LR+ 5.33 and LR− 0.28).
Distribution of scores and selected factors associated with breast cancer progression
Because score 1 has low sensitivity (Table 4) and may provide little contribution to predicting breast cancer progression, we started the distribution analysis from score 2 (Table 5). Scores 5 and 6 have similar specificity levels (94.05 and 97.26%) but score 6 has relatively poor sensitivity (19.05%). Thus, score 6 provides little contribution to predicting breast cancer progression and we combined score 6 with score 5 for distribution analysis. Accordingly, the final prognosis scores ranged from ≤ 2 to ≥ 5.
As shown in Table 5, 56 (53.3%) of the 105 patients scored ≤ 2, but only 2 (3.6%) were progressing patients with LN metastasis, 1 (1.8%) had tissue visfatin > 50%, and 1 (1.8%) was age > 50 years. A total of 21 (20.0%) patients scored 3, 2 (9.5%) of which were progressing patients with non-HT (no receiving HT), tissue visfatin > 50%, LN metastasis, age > 50 years, and tumor size ≥ 2 cm. In patients who scored 4, about half were progressing patients with tumor size ≥ 2 cm (42.9%; 6/14), followed by non-HT, tissue visfatin > 50%, and age > 50 years (35.7%; 5/14). A total of 9 (64.3%) of 14 progressing patients with a score of ≥ 5 had tissue visfatin > 50% and tumor size ≥ 2 cm, followed by non-HT, LN metastasis and age > 50 years (57.1%; 8/14).
Discussion
We previously reported that the correlation between tissue visfatin and several individual clinicopathologic factors [21], but the specificity and sensitivity, along with mutual interactions, were not investigated for breast cancer progression. In the current study, individual ROC analysis was used to evaluate the specificity and sensitivity performance of these clinicopathologic factors associated with breast cancer progression. However, as shown in Table 2, aside from HT, tissue visfatin and LN metastasis, the other clinicopathologic factors displayed weak ROC performance (individual AUC < 0.7), and contributed less impact to breast cancer progression. These results suggest that many single factors may have a differential impact on breast cancer progression. Moreover, the possible interactions between tissue visfatin and clinicopathologic factors were not examined by individual ROC analysis.
A similar effect (Additional file 1) was found in univariate logistic regression results, but multivariate analysis produced inconsistent results, except for LN metastasis. According to the individual ROC results (Table 2), the individual AUC of LN metastasis is 0.7083, with a cumulative AUC combining HT, tissue visfatin, LN metastasis, stage, and age, and the tumor size is 0.886. Although multivariate logistic regression analysis presents a novel approach to breast cancer diagnosis, the ROC analysis approach based on sensitivity and specificity also provides acceptable results.
Cumulative ROC analysis has recently been applied in many research fields [32,33,34,35,36,37]. Six of 25 cephalometric measurements were selected by cumulative ROC analysis to optimize the determination of surgical or nonsurgical treatment for skeletal Class III malocclusions [32]. Cumulative ROC analysis has also been applied in cancer association studies, identifying cumulative risks for five SNPs for association with papillary thyroid carcinoma [33]. Thus, cumulative ROC can effectively identify joint effects of multiple disease- or gene-associated factors.
Similarly, our study developed a scoring system for multiple factors-based cumulative ROC analysis and identified a minimum of 6 clinicopathologic factors for predicting breast cancer progression: HT, tissue visfatin, LN metastasis, tumor stage, age, and tumor size (Table 3). Only 4 of these 6 factors provided acceptable sensitivity, specificity, and classification accuracy for predicting breast cancer progression through cumulative ROC analysis with a high AUC score of 0.886 (Table 4). These results suggest that the cumulative ROC analysis strategy can be effectively used to identify the joint effect of multiple factors for breast cancer progression.
Recently, interactions between genes and physical activities has been emphasized [38,39,40], with a particular focus on genetic polymorphisms. In the current study, we focus on the genetic expression of tissue visfatin in terms of protein level in tissue histochemistry. Cumulative ROC analysis shows tissue visfatin levels can combine with common clinicopathologic factors to provide an analysis of the interaction between breast tumor biomarkers and clinicopathologic factors.
Among these interactions, HT is the best single predictor for breast cancer progression (Table 2). Clinical studies have suggested that breast cancer patients may benefit from adjuvant HT [41,42,43]. Tissue visfatin has also been reported to be an important biomarker for breast cancer progression [21]. In the current study, HT and tissue visfatin were shown to have a strong joint association with breast cancer progression. In addition, tumor size and lymph node metastasis are common prognosis factors for both breast cancer progression [44, 45] and Nottingham prognostic index [45]. Advanced stage (III/IV) breast cancer is typically characterized by greater tumor size, lymph node invasion, pathological change in the surrounding tissue, or metastases in distant organs. Advanced stage tumor burden is usually associated with a poor disease prognosis in breast cancer [46,47,48]. Furthermore, age has been suggested to be an important risk factor for breast cancer, as inferred from the association with age-related tissue microenvironment alteration [49]. Moreover, therapeutic impact differs with age [50, 51]. Hence, breast cancer progression is significantly associated with tumor characteristics and aging [48], but how this age-dependency increases in disease progression remains unclear. Moreover, the proportion of progressing patients with 6 selected high-risk clinicopathologic factors (No-HT, tissue visfatin > 50%, LN metastasis, tumor stage III/IV, age > 50 years, and tumor size ≥ 2 cm) increased with cumulative score, indicating that these selected high-risk clinicopathologic factors were highly associated with breast cancer progression. Accordingly, these factors exhibit a high degree of mutual interactivity in cumulative ROC analysis.
Although our study did not consider the follow-up interval for breast cancer progression, our proposed strategy for cumulative ROC analysis shows the joint effect of clinicopathologic factors for predicting breast cancer progression in terms of sensitivity and specificity for disease prediction. Furthermore, the proposed scoring system was based on the highest AUC performance from cumulative ROC analysis and did not account for the association of low AUC clinicopathologic factors effects on breast cancer progression.
The present study is subject to several limitations. No follow-up intervals are included and the cumulated ROC approach is mainly affected by the AUC ranking results, which might restrict exhaustive search for all possible combinations of complex interactions. For example, although ER, PR and Her2 status were reported to be highly associated with breast cancer progression, the cumulated AUC ranking results for the combined interactions still excluded these 3 factors. In addition, we did not include molecular subtype (TNBC, luminal A, luminal B and Her 2 enriched). Moreover, the visfatin level was examined from the tumor specimens of breast cancer patients, indicating the visfatin level required invasive procedures. Further examination of visfatin level through the secretary samples such as blood should be considered.
Conclusions
The current study examined the impact of 13 clinicopathologic factors for predicting breast cancer progression. Under our proposed scoring system, the cumulative ROC analysis provides better AUC performance than individual ROC analysis in predicting breast cancer progression. Analysis of factor interaction identified a minimum of 6 factors which display a high degree of mutual interaction and association with breast cancer progression: HT, tissue visfatin, LN metastasis, tumor stage, age, and tumor size.
Abbreviations
- ROC:
-
cumulative receiver operating characteristic
- AUC:
-
area under curve
- HT:
-
hormone therapy
- LN:
-
lymph node
- ER:
-
estrogen receptor
- PR:
-
progesterone receptor
- HER2:
-
human epidermal growth factor receptor 2
- NAMPT:
-
nicotinamide phosphoribosyltransferase
- BMI:
-
body mass index
- CT:
-
chemotherapy
- LR:
-
likelihood ratio
References
Karam AK. Breast cancer posttreatment surveillance: diagnosis and management of recurrent disease. Clin Obstet Gynecol. 2016;59(4):772–8.
Ibrahim EM, Al-Foheidi ME, Al-Mansour MM, Kazkaz GA. The prognostic value of tumor-infiltrating lymphocytes in triple-negative breast cancer: a meta-analysis. Breast Cancer Res Treat. 2014;148(3):467–76.
Yang ZY, Di MY, Yuan JQ, Shen WX, Zheng DY, Chen JZ, Mao C, Tang JL. The prognostic value of phosphorylated Akt in breast cancer: a systematic review. Sci Rep. 2015;5:7758.
Stevens KN, Vachon CM, Couch FJ. Genetic susceptibility to triple-negative breast cancer. Cancer Res. 2013;73(7):2025–30.
Chang WP, Liu ME, Chang WC, Yang AC, Ku YC, Pai JT, Lin YW, Tsai SJ. Sleep apnea and the subsequent risk of breast cancer in women: a nationwide population-based cohort study. Sleep Med. 2014;15(9):1016–20.
Bundred NJ. Prognostic and predictive factors in breast cancer. Cancer Treat Rev. 2001;27(3):137–42.
Fung F, Cornacchi SD, Vanniyasingam T, Dao D, Thabane L, Simunovic M, Hodgson N, O’Brien MA, Reid S, Heller B, et al. Predictors of 5-year local, regional, and distant recurrent events in a population-based cohort of breast cancer patients. Am J Surg. 2017;213(2):418–25.
Goldhirsch A, Wood WC, Gelber RD, Coates AS, Thurlimann B, Senn HJ. Progress and promise: highlights of the international expert consensus on the primary therapy of early breast cancer 2007. Ann Oncol. 2007;18(7):1133–44.
Romacho T, Sanchez-Ferrer CF, Peiro C. Visfatin/Nampt: an adipokine with cardiovascular impact. Mediators Inflamm. 2013;2013:946427.
Galli M, Van Gool F, Rongvaux A, Andris F, Leo O. The nicotinamide phosphoribosyltransferase: a molecular link between metabolism, inflammation, and cancer. Cancer Res. 2010;70(1):8–11.
Bi TQ, Che XM. Nampt/PBEF/visfatin and cancer. Cancer Biol Ther. 2010;10(2):119–25.
Nakajima TE, Yamada Y, Hamano T, Furuta K, Matsuda T, Fujita S, Kato K, Hamaguchi T, Shimada Y. Adipocytokines as new promising markers of colorectal tumors: adiponectin for colorectal adenoma, and resistin and visfatin for colorectal cancer. Cancer Sci. 2010;101(5):1286–91.
Patel ST, Mistry T, Brown JE, Digby JE, Adya R, Desai KM, Randeva HS. A novel role for the adipokine visfatin/pre-B cell colony-enhancing factor 1 in prostate carcinogenesis. Peptides. 2010;31(1):51–7.
Nakajima TE, Yamada Y, Hamano T, Furuta K, Gotoda T, Katai H, Kato K, Hamaguchi T, Shimada Y. Adipocytokine levels in gastric cancer patients: resistin and visfatin as biomarkers of gastric cancer. J Gastroenterol. 2009;44(7):685–90.
Nakajima TE, Yamada Y, Hamano T, Furuta K, Oda I, Kato H, Kato K, Hamaguchi T, Shimada Y. Adipocytokines and squamous cell carcinoma of the esophagus. J Cancer Res Clin Oncol. 2010;136(2):261–6.
Folgueira MA, Carraro DM, Brentani H, Patrao DF, Barbosa EM, Netto MM, Caldeira JR, Katayama ML, Soares FA, Oliveira CT, et al. Gene expression profile associated with response to doxorubicin-based therapy in breast cancer. Clin Cancer Res. 2005;11(20):7434–43.
Bae SK, Kim SR, Kim JG, Kim JY, Koo TH, Jang HO, Yun I, Yoo MA, Bae MK. Hypoxic induction of human visfatin gene is directly mediated by hypoxia-inducible factor-1. FEBS Lett. 2006;580(17):4105–13.
Yonezawa T, Haga S, Kobayashi Y, Takahashi T, Obara Y. Visfatin is present in bovine mammary epithelial cells, lactating mammary gland and milk, and its expression is regulated by cAMP pathway. FEBS Lett. 2006;580(28–29):6635–43.
Gholinejad Z, Kheiripour N, Nourbakhsh M, Ilbeigi D, Behroozfar K, Hesari Z, Golestani A, Shabani M, Einollahi N. Extracellular NAMPT/Visfatin induces proliferation through ERK1/2 and AKT and inhibits apoptosis in breast cancer cells. Peptides. 2017;92:9–15.
Behrouzfar K, Alaee M, Nourbakhsh M, Gholinejad Z, Golestani A. Extracellular NAMPT/visfatin causes p53 deacetylation via NAD production and SIRT1 activation in breast cancer cells. Cell Biochem Funct. 2017;35(6):327–33.
Lee YC, Yang YH, Su JH, Chang HL, Hou MF, Yuan SS. High visfatin expression in breast cancer tissue is associated with poor survival. Cancer Epidemiol Biomark Prev. 2011;20(9):1892–901.
Hajian-Tilaki K. Receiver operating characteristic (ROC) curve analysis for medical diagnostic test evaluation. Caspian J Intern Med. 2013;4(2):627–35.
Florkowski CM. Sensitivity, specificity, receiver-operating characteristic (ROC) curves and likelihood ratios: communicating the performance of diagnostic tests. Clin Biochem Rev. 2008;29(Suppl 1):S83–7.
Yen CY, Chen CH, Chang CH, Tseng HF, Liu SY, Chuang LY, Wen CH, Chang HW. Matrix metalloproteinases (MMP) 1 and MMP10 but not MMP12 are potential oral cancer markers. Biomarkers. 2009;14(4):244–9.
Yen CY, Huang CY, Hou MF, Yang YH, Chang CH, Huang HW, Chen CH, Chang HW. Evaluating the performance of fibronectin 1 (FN1), integrin alpha4beta1 (ITGA4), syndecan-2 (SDC2), and glycoprotein CD44 as the potential biomarkers of oral squamous cell carcinoma (OSCC). Biomarkers. 2013;18(1):63–72.
Shih Ie M. Application of human leukocyte antigen-G expression in the diagnosis of human cancer. Hum Immunol. 2007;68(4):272–6.
Jin H, Daly DS, Marks JR, Zangar RC. Oxidatively modified proteins as plasma biomarkers in breast cancer. Cancer Biomark. 2013;13(3):193–200.
Baskic D, Popovic S, Bankovic D, Arsovic A, Vukovic V, Zelen I, Djurdjevic P. Evaluation of inflammatory biomarkers as helping diagnostic tool in patients with breast cancer. Cancer Biomark. 2014;14(6):401–8.
Zhao Y, Wang M, Cui C, Zhang L, Liao F, Li H, Wu X. Significance of combined tests of serum golgi glycoprotein 73 and other biomarkers in diagnosis of small primary hepatocellular carcinoma. Cancer Biomark. 2015;15(5):677–83.
Hamashima C, Sasazuki S, Inoue M, Tsugane S, Group JS. Receiver operating characteristic analysis of prediction for gastric cancer development using serum pepsinogen and Helicobacter pylori antibody tests. BMC Cancer. 2017;17(1):183.
Wong HS, Chang WC. Correlation of clinical features and genetic profiles of stromal interaction molecule 1 (STIM1) in colorectal cancers. Oncotarget. 2015;6(39):42169–82.
Tseng YC, Pan CY, Chou ST, Liao CY, Lai ST, Chen CM, Chang HP, Yang YH. Treatment of adult Class III malocclusions with orthodontic therapy or orthognathic surgery: receiver operating characteristic analysis. Am J Orthod Dentofacial Orthop. 2011;139(5):e485–93.
Liyanarachchi S, Wojcicka A, Li W, Czetwertynska M, Stachlewska E, Nagy R, Hoag K, Wen B, Ploski R, Ringel MD, et al. Cumulative risk impact of five genetic variants associated with papillary thyroid carcinoma. Thyroid. 2013;23(12):1532–40.
Yang CH, Moi SH, Chuang LY, Yuan SF, Hou MF, Lee YC, Chang HW. Interaction of MRE11 and clinicopathologic characteristics in recurrence of breast cancer: individual and cumulated receiver operating characteristic analyses. Biomed Res Int. 2017;2017:2563910.
El-mezayen HA, Metwally FM, Darwish H. A novel discriminant score based on tumor-associated trypsin inhibitor for accurate diagnosis of metastasis in patients with breast cancer. Tumour Biol. 2014;35(3):2759–67.
Rozalski R, Gackowski D, Siomek-Gorecka A, Starczak M, Modrzejewska M, Banaszkiewicz Z, Olinski R. Urinary 5-hydroxymethyluracil and 8-oxo-7,8-dihydroguanine as potential biomarkers in patients with colorectal cancer. Biomarkers. 2015;20(5):287–91.
De Paoli M, Perco P, Muhlberger I, Lukas A, Pandha H, Morgan R, Feng GJ, Marquette C. Disease map-based biomarker selection and pre-validation for bladder cancer diagnostic. Biomarkers. 2015;20(5):328–37.
Li CI, Li TC, Liao LN, Liu CS, Yang CW, Lin CH, Hsiao JH, Meng NH, Lin WY, Wu FY, et al. Joint effect of gene-physical activity and the interactions among CRP, TNF-alpha, and LTA polymorphisms on serum CRP, TNF-alpha levels, and handgrip strength in community-dwelling elders in Taiwan—TCHS-E. Age (Dordr). 2016;38(2):46.
Ahmad S, Rukh G, Varga TV, Ali A, Kurbasic A, Shungin D, Ericson U, Koivula RW, Chu AY, Rose LM, et al. Gene x physical activity interactions in obesity: combined analysis of 111,421 individuals of European ancestry. PLoS Genet. 2013;9(7):e1003607.
Montasser ME, Gu D, Chen J, Shimmin LC, Gu C, Kelly TN, Jaquish CE, Rice T, Rao DC, Cao J, et al. Interactions of genetic variants with physical activity are associated with blood pressure in Chinese: the GenSalt study. Am J Hypertens. 2011;24(9):1035–40.
Early Breast Cancer Trialists’ Collaborative G, Davies C, Godwin J, Gray R, Clarke M, Cutter D, Darby S, McGale P, Pan HC, Taylor C, et al. Relevance of breast cancer hormone receptors and other factors to the efficacy of adjuvant tamoxifen: patient-level meta-analysis of randomised trials. Lancet. 2011;378(9793):771–84.
Blok EJ, Derks MG, van der Hoeven JJ, van de Velde CJ, Kroep JR. Extended adjuvant endocrine therapy in hormone-receptor positive early breast cancer: current and future evidence. Cancer Treat Rev. 2015;41(3):271–6.
Siyam T, Ross S, Campbell S, Eurich DT, Yuksel N. The effect of hormone therapy on quality of life and breast cancer risk after risk-reducing salpingo-oophorectomy: a systematic review. BMC Womens Health. 2017;17(1):22.
D’Eredita G, Giardina C, Martellotta M, Natale T, Ferrarese F. Prognostic factors in breast cancer: the predictive value of the Nottingham Prognostic Index in patients with a long-term follow-up that were treated in a single institution. Eur J Cancer. 2001;37(5):591–6.
Rampaul RS, Pinder SE, Elston CW, Ellis IO, Nottingham Breast T. Prognostic and predictive factors in primary breast cancer and their role in patient management: the Nottingham Breast Team. Eur J Surg Oncol. 2001;27(3):229–38.
Mu Z, Wang C, Ye Z, Austin L, Civan J, Hyslop T, Palazzo JP, Jaslow R, Li B, Myers RE, et al. Prospective assessment of the prognostic value of circulating tumor cells and their clusters in patients with advanced-stage breast cancer. Breast Cancer Res Treat. 2015;154(3):563–71.
Witherby S, Rizack T, Sakr BJ, Legare RD, Sikov WM. Advances in medical management of early stage and advanced breast cancer: 2015. Semin Radiat Oncol. 2016;26(1):59–70.
Yasmeen S, Hubbard RA, Romano PS, Zhu W, Geller BM, Onega T, Yankaskas BC, Miglioretti DL, Kerlikowske K. Risk of advanced-stage breast cancer among older women with comorbidities. Cancer Epidemiol Biomark Prev. 2012;21(9):1510–9.
LaBarge MA, Mora-Blanco EL, Samson S, Miyano M. Breast cancer beyond the age of mutation. Gerontology. 2016;62(4):434–42.
Liu J, Chen K, Mao K, Su F, Liu Q, Jacobs LK. The prognostic value of age for invasive lobular breast cancer depending on estrogen receptor and progesterone receptor-defined subtypes: a NCDB analysis. Oncotarget. 2016;7(5):6063–73.
Meresse M, Bouhnik AD, Bendiane MK, Retornaz F, Rousseau F, Rey D, Giorgi R. Chemotherapy in old women with breast cancer: is age still a predictor for under treatment? Breast J. 2017;23(3):256–66.
Authors’ contributions
S-HM and Y-CL drafted the manuscript. Y-CL and S-SFY were responsible for the data processing and interpretation. S-HM and L-YC performed statistics analyses. FO-Y, M-FH, C-HY, and H-WC were involved in discussion. C-HY and H-WC conceived and designed the study and fully revised the final manuscript. All authors read and approved the final manuscript.
Acknowledgements
This work was supported by several funds listed in funding section.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
https://wp.kmu.edu.tw/changhw/files/2017/05/ROC_tissue-visfatin_dataset.xlsx.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The protocol of this study was reviewed and approved by the Institutional Review Board (IRB) of Kaohsiung Medical University (KMUH-IRB-980567) and informed consent was taken from all patients.
Funding
This work was supported by grants from the Ministry of Science and Technology (MOST 104-2320-B-037-013-MY3 and MOST 103-2221-E-151-029-MY3), the National Sun Yat-sen University-KMU Joint Research Project (#NSYSU-KMU 107-p001), the Kaohsiung Medical University Hospital (KMUH105-5M24), the Kaohsiung Medical University (KMU-M106028), and the Health and welfare surcharge of tobacco products, the Ministry of Health and Welfare, Taiwan, Republic of China (MOHW106-TDU-B-212-144007, MOHW105-TDU-B-212-134007, MOHW104-TD-B-111-05, and MOHW104-TDU-B-212-124-003).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding authors
Additional file
Additional file 1.
Logistic regression analysis of progression risk factors in breast cancer. This table provides the univariate and multivariate logistic regression analysis of risk factor associated with breast cancer progression.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Moi, SH., Lee, YC., Chuang, LY. et al. Cumulative receiver operating characteristics for analyzing interaction between tissue visfatin and clinicopathologic factors in breast cancer progression. Cancer Cell Int 18, 19 (2018). https://doi.org/10.1186/s12935-018-0517-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12935-018-0517-z