Abstract
Background
Primary biliary cholangitis (PBC) and primary sclerosing cholangitis (PSC) are forms of hepatic autoimmunity, and risk for both diseases has a strong genetic component. This study aimed to define the genetic architecture of PBC and PSC within the Polish population.
Methods
Subjects were 443 women with PBC, 120 patients with PSC, and 934 healthy controls recruited from Gastroenterology Departments in various Polish hospitals. Allelotyping employed a pooled-DNA sample-based genome-wide association study (GWAS) approach, using Illumina Human Omni2.5-Exome BeadChips and the following novel selection criteria for risk loci: blocks of at least 10 single nucleotide polymorphisms (SNPs) in strong linkage disequilibrium, where the distance between each adjacent SNP pair in the block was less than 30 kb, and each SNP was associated with disease at a significance level of P < 0.005. A selected index SNP from each block was validated using TaqMan SNP genotyping assays.
Results
Nineteen and twenty-one SNPs were verified as associated with PBC and PSC, respectively, by individual genotyping; 19 (10/9, PBC/PSC) SNPs reached a stringent (corrected) significance threshold and a further 21 (9/12, PBC/PSC) reached a nominal level of significance (P < 0.05 with odds ratio (OR) > 1.2 or < 0.83), providing suggestive evidence of association. The SNPs mapped to seven (1p31.3, 3q13, 6p21, 7q32.1, 11q23.3, 17q12, 19q13.33) and one (6p21) chromosome region previously associated with PBC and PSC, respectively. The SNP, rs35730843, mapping to the POLR2G gene promoter (P = 1.2 × 10-5, OR = 0.39) demonstrated the highest effect size, and was protective for PBC, whereas for PSC respective SNPs were: rs13191240 in the intron of ADGRB3 gene (P = 0.0095, OR = 0.2) and rs3822659 (P = 0.0051, OR = 0.236) along with rs9686714 (P = 0.00077, OR = 0.2), both located in the WWC1 gene.
Conclusions
Our cost-effective GWAS approach followed by individual genotyping confirmed several previously identified associations and discovered new susceptibility loci associated with PBC and/or PSC in Polish patients. However, further functional studies are warranted to understand the roles of these newly identified variants in the development of the two disorders.
Similar content being viewed by others
Background
Primary biliary cholangitis (PBC) and primary sclerosing cholangitis (PSC) are hepatobiliary autoimmune diseases with strong genetic risk components [1]. PBC is characterized by progressive immune-mediated destruction of interlobular biliary ductules, and PSC by inflammatory and fibrotic processes affecting the intrahepatic and extrahepatic biliary tree; both diseases lead to liver cirrhosis [1–4]. PBC occurs more frequently in women than men and primarily in middle-age, with prevalences ranging from 40 to 400 patients per million and incidences ranging from 0.7 to 49 per million [5–8]. PSC affects 9 to 13 patients per million annually with a male-to-female ratio of 2:1 [3]. In Western countries, 60–80% of PSC cases are associated with inflammatory bowel disease (IBD), while PSC is present in 3–8% of all patients with ulcerative colitis and 1–3% of patients with Crohn’s disease [2, 9, 10]. Both PBC and PSC are classic polygenic disorders, with a genetic load represented by common, mostly non-protein-coding single nucleotide polymorphisms (SNPs), exhibiting similar small effect sizes [1].
Standard genome-wide association studies (GWASs) use high throughput SNP microarray technologies to discover SNPs associated with disease. Generally, the higher the sample size of a GWAS, the higher the number of the associations that reach the genome-wide significance threshold of P < 5 × 10-8 [2]. By contrast, studies with small sample sizes typically fail to reach GWAS statistical significance. The largest genetic association study for IBDs employed over 75,000 patients and controls and uncovered 163 IBD susceptibility loci [3]. However, studies of the heritable component of PBC and PSC by GWAS have been rather limited, primarily because of the lower prevalence of hepatobiliary autoimmunity, particularly PSC. While several GWASs have been performed using well-characterized PBC patient cohorts from North America, Europe, or Japan, only a few have included PSC patients mainly from northern Europe [4]; however, all of these GWASs had relatively small sample sizes [2]. Despite this, in addition to multiple PSC and PBC associations within the HLA complex, and with non-HLA genes mapping to the chromosome 6p21 major histocompatibility complex (MHC) locus, several associations have been identified at non-MHC susceptibility loci with genome-wide significance [6–17].
Many of these are associated with other immune-mediated diseases, including multiple sclerosis, celiac disease, and type 1 diabetes (T1D) [17, 18]. However, while larger GWAS cohorts, combining patients from different populations, may miss some sub-population-specific risk variants, smaller GWASs generally suffer from lack of statistical power. As a consequence, in GWASs limited to hundreds of patients, few or no associations at the accepted genome-wide significance level have been identified.
To identify susceptibility loci for PBC and PSC in the Polish population, we employed a pooled-DNA GWAS approach, together with a new method for identifying SNP associations. Considering the limited sizes of the cohorts investigated in our GWAS, this approach was effective in identifying novel PBC and/or PSC susceptibility loci. Despite the fact that “index SNPs” were selected at P-values much lower than the standard genome-wide significance threshold, the majority were validated by individual TaqMan SNP genotyping assays.
Methods
Studied subjects
Between 2010 and 2014, 443 women with PBC (389 antimitochondrial antibodies positive) and 120 PSC patients (37 females and 83 males) were recruited at nine recruitment centers. All enrolled patients and controls were Polish Caucasians. Diagnosis of PBC was based on standard clinical, biochemical, serological, and histological criteria, and PSC was diagnosed according to standard clinical, biochemical, cholangiographic, and in some patients - histological criteria according to the European Association for the Study of Liver (EASL) [19]. Blood samples were also obtained from 934 healthy individuals (512 females and 422 males). Sample sizes and age distribution for each group are shown in Table 1.
GWAS allelotyping
A pooled-DNA sample-based GWAS was performed as described previously [20]. Genomic DNA was extracted from whole blood treated with EDTA using a QIAamp DNA Mini Kit. DNA sample concentrations were measured by a Quant-iTTM PicoGreen dsDNA Kit (Invitrogen, United Kingdom). DNA integrity was verified by 1% agarose gel analysis. Those DNA samples that passed quality control tests were combined according to diagnosis at equimolar concentrations to obtain two sets of DNA pools. The first microarray set consisted of 21, 6 and 30 DNA pools combining 20–24 DNA samples from PBC patients, PSC patients and healthy controls, respectively, whereas the second set consisted of 11, 3 and 10 DNA pools which were respectively combined from 37 DNA samples of PBC, PSC and controls. Pooled-DNA samples were adjusted to a final concentration of 50 ng/ml in Tris-EDTA buffer (pH = 8) and were assayed independently on Illumina Human Omni2.5-Exome BeadChips by the external AROS Applied Biotechnology A/S (Aarhus, Denmark) service.
Individual genotyping
For validating the GWAS findings and the SNP typing replication study, individual patients and controls were genotyped with TaqMan SNP Genotyping Assays (Thermo, USA) using a TaqMan Universal Master Mix II (Thermo, USA) and a 7900HT Real-Time PCR system (Thermo, USA).
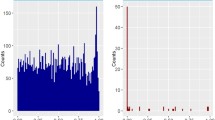
Statistical analyses – allelotyping GWAS
For each SNP, on each microarray, the relative allele signal (RAS) was calculated as described previously [20]. RAS was used as an approximation of the allele ratio. The Student’s t-test (Welch variant) was used to compare allele ratios between groups. Due to a lack of the call-rate statistic for pooled samples, quality was assessed by visual inspection of first four principal components. A representative example is shown in Additional file 1: Figure S1. Six/two control pools were removed as outliers from the first/second microarray set, respectively. No probe filtering was performed. P-values were corrected for multiple hypothesis testing with the Bonferroni algorithm. Manhattan plotting was performed using the qqman R package [21]. All computations were performed according to R environment [22]. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL http://www.R-project.org/).
Statistical analyses – individual genotyping
Associations were examined using the Fisher-exact test implemented in R (version 3.1.1). The odds ratios (ORs) and 95% confidence intervals (CIs) were estimated by normal approximation using the EpiTools R package [23].
Functional analyses
Symbols of genes to which SNPs mapped (in case of intergenic position symbols of both flanking genes) were used to assign functional overrepresentation using DAVID tool [24] and Swiss-Prot Protein Information Resource (SP-PIR) vocabulary.
Results
For association screening, we adopted a cost-effective pooled-DNA GWAS design [20], which involved two separate hybridizations. Individual DNA samples from the same patient cohorts, that passed quality control, were combined in equimolar amounts, according to patient diagnosis, to obtain two sets of DNA pools from the same patients groups; the first set represented 420 PBC patients and 120 PSC patients and the second set, 407 and 111 of these two patient groups, respectively. In contrast, two different cohorts of 724 and 370 controls were employed. Selected SNPs, identified by GWAS, were genotyped using individual DNA samples from the same cohorts of 443 PBC patients, 120 PSC patients, and 934 control subjects in TaqMan SNP genotyping assays.
The method of selecting loci for validation is crucial for a successful GWAS. Our relatively small patient cohorts, particularly the PSC cohort, were statistically unpowered to detect SNPs associated at the standard threshold for genome-wide significance (P < 5 × 10-8). Therefore, assuming that an “index SNP” at a given locus is usually not independent of neighboring SNPs, we focused on loci forming blocks of at least 10 SNPs in strong allele linkage disequilibrium, defined by the following criteria: the distance between each pair of adjacent SNPs in the block was < 30 kb, and each SNP was associated with a disease at a significance level of P < 0.005. Among blocks meeting such criteria, we selected “index SNPs” associated with disease at P < 10-4, which were subsequently subjected to TaqMan SNP genotyping assays using individual PBC and PSC patient DNA samples. Although no extensive optimization of the number of required loci, P-value threshold, or window size was performed, the algorithm used was effective.
Primary biliary cholangitis
Two rounds of GWAS led to the selection of 22 SNPs from 18 blocks of SNPs for validation as associated with PBC. Of the 22 SNPs, all but one were selected from the first GWAS, and only one of the seven SNPs selected from the second GWAS was not also identified in the first round. Among 22 “index SNPs” subjected to the genotyping assays, 19 were validated as associated with PBC, of which 10 reached the significance level determined by Bonferroni correction for multiple testing (P < 0.0023; 0.05/22), while the remaining nine demonstrated at least suggestive evidence for association, reaching a nominal level of significance (P < 0.05, with OR > 1.2 or < 0.83) (Additional file 2: Table S1). All 19 had the same direction of effect as observed in GWAS. In addition, two SNPs (rs3745516 and rs9303277) that were found to associate with PBC in previous studies [14, 16] were also confirmed to be associated in our PBC cohort. For 14 SNPs, the minor allele was associated with increased disease risk, while for the remaining five SNPs the minor allele showed a protective effect. The most significant PBC association (in terms of OR) as determined by genotyping assay was observed with the POLR2G locus (rs35730843; OR = 0.39; P = 1.2 × 10-5; SNP located in the gene promoter).
Primary sclerosing cholangitis
Two rounds of GWAS led to selection of 29 SNPs originating from 22 blocks of SNPs for validation as associated with PSC; 18 and 12 SNPs were selected from the first and second GWAS rounds, respectively, and only one SNP was shared between both rounds. From the 29 SNPs, 21 were defined as associated with PSC after validation by genotyping assays, of which nine SNPs reached the level of significance determined by Bonferroni correction for multiple testing (P < 0.0017; 0.05/29) and 12 reached a nominal level of significance (P < 0.05 with OR > 1.2 or < 0.83) (Additional file 2: Table S2). Again, all 21 validated SNPs had the same effect direction as observed in GWAS. For 10 SNPs, the minor allele was associated with an increased risk, and for the other 11 the minor allele showed a protective effect. The most significant PSC association outside MHC region, as determined by genotyping assays, were observed at the WWC1 gene (rs9686714; OR = 0.20; P = 0.00077; intronic location and rs3822659; OR = 0.24, P = 0.0051) and at the ADGRB3 intron (rs13191240; OR = 0.2; P = 0.0095).
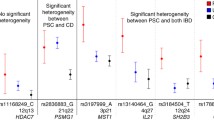
In addition, TaqMan SNP genotyping assays were used to test 18 and 3 SNPs associated with IBD and celiac disease, respectively, in a previous Polish study [25]. Of these, eleven and two SNPs were also found to associate with PBC and PSC, respectively, and another four SNPs with both PBC and PSC (Table 2). Finally, to assess which SNPs associated with PBC are shared loci for susceptibility to PSC and vice versa, all SNPs that had been subjected to validation in PBC were also genotyped in PSC, and those validated in PSC were genotyped in PBC. Altogether, 28 and 18 SNPs were unique to PBC and PSC, respectively, and eleven SNPs were shared between PBC and PSC. Of the latter, three had the same direction of effect in both types of hepatobiliary autoimmunity.
Functional analysis of the merged validated SNP list for PBC and PSC revealed significant over-representation of genes associated with immune responses (HLA-DQB1, HLA-DRB5, HLA-C, HLA-B, HLA-DPB1, HLA-DQA2, HLA-DQA1, and HLA-DRA; P = 0.023; Additional file 2: Table S3).
Discussion
GWASs provide information about common variants associated with disease susceptibility. Although GWASs allow the identification of disease risk alleles without prior knowledge of their position or biological function, they require large study cohorts to identify associations at the genome-wide significance threshold (5 × 10-8). By contrast, smaller GWASs using the same threshold may generate false-negative results. For association screening, we performed pooled-DNA GWASs and applied novel selection criteria that took into account strong allele linkage disequilibrium. We selected SNP blocks, defined by a distance of less than 30 kb between each pair of at least 10 SNPs associated with disease at P < 5 × 10-3, with an “index SNP” in the block for which the association was significant at P ≤ 10-4. All of the associations identified using this approach would have been missed using the standard genome-wide significance threshold. Of 22 and 29 associations with PBC and PCS, respectively, selected for validation, 19 and 21 SNPs were verified using TaqMan SNP genotyping assays of individual patient and control samples. In total, 19 SNPs reached the stringent (corrected) significance threshold, while the other 21 reached a nominal level of significance (P < 0.05 with OR > 1.2 or < 0.83), demonstrating at least suggestive evidence for association (Table 2). However, the expected number of false-positive results for 50 independent tests, with a significance threshold of 0.05, is < 3, while appropriate correction for multiple comparisons would reduce this to < 1. In our validation studies, correction for multiple testing reduced the number of associations at the nominal level of significance from 40 to 19, thus likely generating a large number of false-negative results and only slightly reducing the expected number of false-positive results.
This study identified 57 SNPs associated with either PBC or PSC or both disorders, which represent 38 genetic regions (Table 2). As expected, there were higher numbers of associations with HLA and non-HLA loci mapping to the MHC region (chromosome 6p21). Of 13 SNPs from this region, two, five, and six SNPs were associated with PBC, PSC, and both disorders, respectively. Of the SNPs shared between PBC and PSC, only two exhibited the same direction of effect.
As both PBC and PSC are hepatobiliary autoimmune diseases with low prevalence, the largest GWASs of these diseases have recruited individuals from different populations, which has certainly introduced a level of heterogeneity into the results, arising from the different genetic backgrounds of the geographically distinct populations. Consequently, these large cohort studies may have missed some subtle, sub-population-specific risk variants that may account for missing heritability. Conversely, studies with smaller sample sizes typically reveal a smaller fraction of the heritability of a complex disease, as they fail to detect associations because any found do not reach statistical significance thresholds [26]. The relative homogeneity of the Polish population may explain, at least in part, why our investigation identified so many SNPs significantly associated with PBC and/or PSC.
A GWAS including 536 North American PBC patients uncovered disease associations for several gene variants in the HLA class II region and coding variants in the interleukin-12a (IL12A) and IL12 receptor b2 (IL12RB2) genes [11]. Further GWASs have replicated these findings in a European population, and identified additional risk genes overlapping with other autoimmune diseases [17, 18]. In six GWASs, 27 non-HLA risk loci associated with PBC were identified [4]. Most have also been implicated in other autoimmune diseases, highlighting different immunoregulatory pathways. Our findings indicated the possible involvement of six previously described regions (1p31.3, rs3790567 [11]; 3q13 [13, 16]; 7q32.1, rs10488631 [12, 14]; 11q23.3 [13, 16]; 17q12, rs9303277 [18]; and 19q13.33, rs3745516 [14]) and the HLA-containing 6p21 locus in the development of PBC in Polish patients (Table 2).
Genomic studies of PSC have uncovered 18 associated genetic regions: 1p36 (TNFRSF14, MMEL1); 2q13 (BCL2L1); 2q33 (CD28); 2q35 (GPBAR1); 2q37.3 (GPR35); 3p21 (USP4, MST1); 4q27 (IL2, IL21); 6q15 (BACH2); 6p21 (HLA region); 10p15 (IL2RA); 11q23 (SIK2); 12q13 (HDAC7); 12q24 (SH2B3, ATXN2); 13q31 (GPC5/6); 18q21.1 (TCF4); 18q22 (CD226); 19q13 (PRKD2, STRN4); and 21q22 (PSMG1) [5, 6, 8, 27, 28]. Of these, only the MHC region was replicated in our PSC patients (Table 2).
The MHC region, which contains more than 224 genes and is highly polymorphic, is known to be associated with more than 100 different autoimmune and infectious diseases [29–31]. In European-based GWASs, the most pronounced MHC associations with PSC were with class I (HLA-B and -C) rather than class II (HLA-DRB1 and -DQB1) loci [27]. A meta-analysis of three independent PBC cohorts identified HLA class II alleles (HLA-DRB1, HLA-DQA1, and HLA-DQB1) achieving genome-wide significance levels, with similar allele frequencies in Canadian, US, and Italian PBC cohorts [15]. Outside of the MHC region, our investigation confirmed six and zero genetic regions uncovered by previous GWASs as associated with PBC and PSC, respectively [27]. Of 30 chromosomal regions representing novel susceptibility loci, 13, 9, and 8 were associated with PBC, PSC, and both disorders, respectively. Of these, 17 SNPs have a shared genetic association with IBD, three with rheumatoid arthritis, two with lupus erythematosus, and single SNPs with psoriasis, lateral sclerosis, T1D, and intrahepatic cholestasis of pregnancy.
While well-designed GWASs should be conducted with groups of at least 1,000 patients and 1,000 controls, the appropriate level of statistical power to test for genetic associations (at P < 5 × 10-8) often relates to higher effect sizes [32]. However, since loci with a high effect size have generally been efficiently removed from the human population by natural selection, the identification of a common polymorphic susceptibility locus strongly associated with disease, with an OR > 2 or < 0.5, is unlikely [33]. Instead, a large number of previously identified loci associated with different disorders exhibit relatively small effect sizes, with ORs < 1.3. The present study uncovered only one SNP (rs35730843, POLR2G, P = 1.2 × 10-5, OR = 0.393) strongly associated with PBC and 11 SNPs strongly associated with PSC (rs3822659, coding in WWC1, P = 0.0051, OR = 0.236; rs9686714, intron of WWC1, P = 0.00077, OR = 0.195; rs13191240, intron of ADGRB3, P = 0.0095, OR = 0.2; rs7454108, intergenic between LOC100294145 and C4B_2, P = 0.0013, OR = 0.326; rs2524163, intron of HLA-B, P = 5.9 × 10-7, OD = 2.02; rs2187668, intron of HLA-DQA1, P = 1.5 × 10-7, OR = 2.47; rs3130484, intron of MSH5-SAPCD1, P = 5.1 × 10-11, OR = 3.23; rs1264377, intergenic between PSORS1C3 − MIR877, P = 8 × 10-8, OR = 2.39; rs3130626, intron of PRRC2A, P = 1.5 × 10-6, OR = 2.10; rs419788, intron of SKIV2L, P = 1.2 × 10-6, OR = 2.03; and rs34708188, intergenic close to SENCR, P = 0.0056, OR = 2.27). Of these, nine SNPs map to the MHC region (6p21), while POLR2G, WWC1, and ADGRB3 are located in other genomic regions.
Our results indicated that a rare variant in the POLR2G gene promoter is associated with decreased risk of PBC, with a high effect size in the Polish population. POLR2G encodes one of the subunits in the polymerase 2 RNA complex, which is responsible for transcribing protein coding genes, miRNAs, and some classes of non-coding RNAs [34] and maps to the 11q12.3 locus, within which variants associated with chronic obstructive pulmonary disease [35] and asthma [36] have been identified. We also identified a decreased risk for PCS (OR < 0.25) conferred by a single rare variant in the ADGRB3 gene and two rare variants (rs3822659 and rs9686714) in the WWC1 gene. ADGRB3 encodes transmembrane adhesion G protein-coupled receptor B3 (BAI3), which is broadly expressed in the brain and involved in the regulation of excitatory synapse connectivity [37]. Furthermore, BAI3 can promote myoblast fusion in vertebrates [38]. A previous GWAS identified SNPs at the ADGRB3 locus as associated with early-onset venous thromboembolism [39]. WWC1 encodes the KIBRA protein that plays versatile roles including in the regulation of cellular signaling, cell polarity, vesicular trafficking, and cell migration and division [40]. Specifically, KIBRA is a regulator of the Hippo signaling pathway, which controls tissue growth and tumorigenesis by inhibiting cell proliferation and promoting apoptosis [41]. Notably, WWC1 hypermethylation occurs in 70% of B-cell acute lymphocytic leukemias [42] and its epigenetic silencing is also associated with unfavorable prognostic parameters in chronic lymphocytic leukemia [43]. Interestingly, the triggering of IL-6 trans-signaling, a process of aggregation of extracellular soluble IL-6 receptor and IL-6 associated with rheumatoid arthritis [44] and IBD [45], significantly increased WWC1 expression in human airway smooth muscle cells [46], suggesting a link between its expression and inflammatory diseases. Importantly, rs3822659 is a missense variant (Ser735Ala) that alters the interaction of KIBRA with phosphatidylinositol 3-phosphate [47]. Other GWASs have implicated SNPs in WWC1 as associated with memory performance and cognition [48], as well as Alzheimer’s disease [49].
Conclusions
To the best of our knowledge, we have performed the first GWAS of PBC and PSC patients from the Polish population. Our cost-effective GWAS approach, followed by individual genotyping, allowed us to confirm several previously described associations and discover new susceptibility loci associated with both diseases. Although GWASs allow scanning of the entire genome to identify disease risk alleles without prior knowledge of their position or biological function, the use of statistical, rather than biological, criteria for selection of association findings greatly limits our understanding of the role of newly identified variants related to disease development. More importantly, the contribution of the genetic landscape in the context of environmental factors, and interactions between these two influences in conferring susceptibility to disease, has yet to be elucidated.
Abbreviations
- GWAS:
-
Genome-wide association study
- IBD:
-
Inflammatory bowel disease
- MHC:
-
Major histocompatibility complex
- OR:
-
Odds ratio
- PBC:
-
Primary biliary cholangitis
- PSC:
-
Primary sclerosing cholangitis
- SNP:
-
Single nucleotide polymorphism
References
Webb GJ, Hirschfield GM. Using GWAS to identify genetic predisposition in hepatic autoimmunity. J Autoimmun. 2016;66:25–39.
Sham PC, Purcell SM. Statistical power and significance testing in large-scale genetic studies. Nat Rev Genet. 2014;15:335–46.
Jostins L, Ripke S, Weersma RK, Duerr RH, McGovern DP, Hui KY, et al. Host-microbe interactions have shaped the genetic architecture of inflammatory bowel disease. Nature. 2012;491:119–24.
Gulamhusein AF, Juran BD, Lazaridis KN. Genome-Wide Association Studies in Primary Biliary Cirrhosis. Semin Liver Dis. 2015;35:392–401.
Karlsen TH, Franke A, Melum E, Kaser A, Hov JR, Balschun T, et al. Genome-wide association analysis in primary sclerosing cholangitis. Gastroenterology. 2010;138:1102–11.
Melum E, Franke A, Schramm C, Weismüller TJ, Gotthardt DN, Offner FA, et al. Genome-wide association analysis in primary sclerosing cholangitis identifies two non-HLA susceptibility loci. Nat Genet. 2011;43:17–9.
Folseraas T, Melum E, Rausch P, Juran BD, Ellinghaus E, Shiryaev A, et al. Extended analysis of a genome-wide association study in primary sclerosing cholangitis detects multiple novel risk loci. J Hepatol. 2012;57:366–75.
Ellinghaus D, Folseraas T, Holm K, Ellinghaus E, Melum E, Balschun T, et al. Genome-wide association analysis in primary sclerosing cholangitis and ulcerative colitis identifies risk loci at GPR35 and TCF4. Hepatology. 2013;58:1074–83.
Anderson CA, Boucher G, Lees CW, Franke A, D’Amato M, Taylor KD, et al. Meta-analysis identifies 29 additional ulcerative colitis risk loci, increasing the number of confirmed associations to 47. Nat Genet. 2011;43:246–52.
Janse M, Lamberts LE, Franke L, Raychaudhuri S, Ellinghaus E, Muri Boberg K, et al. Three ulcerative colitis susceptibility loci are associated with primary sclerosing cholangitis and indicate a role for IL2, REL, and CARD9. Hepatology. 2011;53:1977–85.
Hirschfield GM, Liu X, Xu C, Lu Y, Xie G, Lu Y, et al. Primary biliary cirrhosis associated with HLA, IL12A, and IL12RB2 variants. N Engl J Med. 2009;360:2544–55.
Hirschfield GM, Liu X, Han Y, Gorlov IP, Lu Y, Xu C, et al. Variants at IRF5-TNPO3, 17q12-21 and MMEL1 are associated with primary biliary cirrhosis. Nat Genet. 2010;42:655–7.
Mells GF, Floyd JAB, Morley KI, Cordell HJ, Franklin CS, Shin S-Y, et al. Genome-wide association study identifies 12 new susceptibility loci for primary biliary cirrhosis. Nat Genet. 2011;43:329–32.
Liu X, Invernizzi P, Lu Y, Kosoy R, Lu Y, Bianchi I, et al. Genome-wide meta-analyses identify three loci associated with primary biliary cirrhosis. Nat Genet. 2010;42:658–60.
Cordell HJ, Han Y, Mells GF, Li Y, Hirschfield GM, Greene CS, et al. International genome-wide meta-analysis identifies new primary biliary cirrhosis risk loci and targetable pathogenic pathways. Nat Commun. 2015;6:8019.
Nakamura M, Nishida N, Kawashima M, Aiba Y, Tanaka A, Yasunami M, et al. Genome-wide association study identifies TNFSF15 and POU2AF1 as susceptibility loci for primary biliary cirrhosis in the Japanese population. Am J Hum Genet. 2012;91:721–8.
Liu JZ, Hov JR, Folseraas T, Ellinghaus E, Rushbrook SM, Doncheva NT, et al. Dense genotyping of immune-related disease regions identifies nine new risk loci for primary sclerosing cholangitis. Nat Genet. 2013;45:670–5.
Liu JZ, Almarri MA, Gaffney DJ, Mells GF, Jostins L, Cordell HJ, et al. Dense fine-mapping study identifies new susceptibility loci for primary biliary cirrhosis. Nat Genet. 2012;44:1137–41.
European Association for the Study of the Liver. EASL Clinical Practice Guidelines: management of cholestatic liver diseases. J Hepatol. 2009;51:237–67.
Gaj P, Maryan N, Hennig EE, Ledwon JK, Paziewska A, Majewska A, et al. Pooled sample-based GWAS: a cost-effective alternative for identifying colorectal and prostate cancer risk variants in the Polish population. PLoS One. 2012;7, e35307.
Turner SD. qqman: an R package for visualizing GWAS results using Q-Q and manhattan plots. bioRxiv. 2014:005165
Team RC. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. 2013. ISBN 3-900051-07-0; 2014
Developer TJA, User MPF, User DW. epitools: Epidemiology Tools [Internet]. 2012 [cited 2015 Jan 24]. Available from: http://cran.r-project.org/web/packages/epitools/index.html
Huang DW, Sherman BT, Lempicki RA. Systematic and integrative analysis of large gene lists using DAVID bioinformatics resources. Nat Protoc. 2009;4:44–57.
Paziewska A, Cukrowska B, Dabrowska M, Goryca K, Piatkowska M, Kluska A, et al. Combination Testing Using a Single MSH5 Variant alongside HLA Haplotypes Improves the Sensitivity of Predicting Coeliac Disease Risk in the Polish Population. PLoS One. 2015;10, e0139197.
Jostins L, Barrett JC. Genetic risk prediction in complex disease. Hum Mol Genet. 2011;20:R182–8.
Zimmer V, Lammert F. Role of genetics in diagnosis and therapy of acquired liver disease. Mol Aspects Med. 2014;37:15–34.
Li F, Lu J, Cheng J, Wang L, Matsubara T, Csanaky IL, et al. Human PXR modulates hepatotoxicity associated with rifampicin and isoniazid co-therapy. Nat Med. 2013;19:418–20.
Parkes M, Cortes A, van Heel DA, Brown MA. Genetic insights into common pathways and complex relationships among immune-mediated diseases. Nat Rev Genet. 2013;14:661–73.
Shiina T, Hosomichi K, Inoko H, Kulski JK. The HLA genomic loci map: expression, interaction, diversity and disease. J Hum Genet. 2009;54:15–39.
Goyette P, Boucher G, Mallon D, Ellinghaus E, Jostins L, Huang H, et al. High-density mapping of the MHC identifies a shared role for HLA-DRB1*01:03 in inflammatory bowel diseases and heterozygous advantage in ulcerative colitis. Nat Genet. 2015;47:172–9.
Williams SM, Haines JL. Correcting away the hidden heritability. Ann Hum Genet. 2011;75:348–50.
Gibson G. Hints of hidden heritability in GWAS. Nat Genet. 2010;42:558–60.
Scruggs BS, Adelman K. The Importance of Controlling Transcription Elongation at Coding and Noncoding RNA Loci. Cold Spring Harb Symp Quant Biol. 2015;80:33–44.
Kim DK, Cho MH, Hersh CP, Lomas DA, Miller BE, Kong X, et al. Genome-wide association analysis of blood biomarkers in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2012;186:1238–47.
Laing IA, Hermans C, Bernard A, Burton PR, Goldblatt J, Le Souëf PN. Association between plasma CC16 levels, the A38G polymorphism, and asthma. Am J Respir Crit Care Med. 2000;161:124–7.
Sigoillot SM, Iyer K, Binda F, González-Calvo I, Talleur M, Vodjdani G, et al. The Secreted Protein C1QL1 and Its Receptor BAI3 Control the Synaptic Connectivity of Excitatory Inputs Converging on Cerebellar Purkinje Cells. Cell Rep. 2015.
Hamoud N, Tran V, Croteau L-P, Kania A, Côté J-F. G-protein coupled receptor BAI3 promotes myoblast fusion in vertebrates. Proc Natl Acad Sci USA. 2014;111:3745–50.
Antoni G, Morange P-E, Luo Y, Saut N, Burgos G, Heath S, et al. A multi-stage multi-design strategy provides strong evidence that the BAI3 locus is associated with early-onset venous thromboembolism. J Thromb Haemost. 2010;8:2671–9.
Zhang L, Yang S, Wennmann DO, Chen Y, Kremerskothen J, Dong J. KIBRA: In the brain and beyond. Cell Signal. 2014;26:1392–9.
Xiao L, Chen Y, Ji M, Volle DJ, Lewis RE, Tsai M-Y, et al. KIBRA protein phosphorylation is regulated by mitotic kinase aurora and protein phosphatase 1. J Biol Chem. 2011;286:36304–15.
Hill VK, Dunwell TL, Catchpoole D, Krex D, Brini AT, Griffiths M, et al. Frequent epigenetic inactivation of KIBRA, an upstream member of the Salvador/Warts/Hippo (SWH) tumor suppressor network, is associated with specific genetic event in B-cell acute lymphocytic leukemia. Epigenetics. 2011;6:326–32.
Shinawi T, Hill V, Dagklis A, Baliakas P, Stamatopoulos K, Agathanggelou A, et al. KIBRA gene methylation is associated with unfavorable biological prognostic parameters in chronic lymphocytic leukemia. Epigenetics. 2012;7:211–5.
Patel AM, Moreland LW. Interleukin-6 inhibition for treatment of rheumatoid arthritis: a review of tocilizumab therapy. Drug Des Devel Ther. 2010;4:263–78.
Rose-John S, Mitsuyama K, Matsumoto S, Thaiss WM, Scheller J. Interleukin-6 trans-signaling and colonic cancer associated with inflammatory bowel disease. Curr Pharm Des. 2009;15:2095–103.
Robinson MB, Deshpande DA, Chou J, Cui W, Smith S, Langefeld C, et al. IL-6 trans-signaling increases expression of airways disease genes in airway smooth muscle. Am. J. Physiol. Lung Cell Mol. Physiol. 2015;309:L129–38.
Duning K, Wennmann DO, Bokemeyer A, Reissner C, Wersching H, Thomas C, et al. Common exonic missense variants in the C2 domain of the human KIBRA protein modify lipid binding and cognitive performance. Transl Psychiatry. 2013;3, e272.
Papassotiropoulos A, Stephan DA, Huentelman MJ, Hoerndli FJ, Craig DW, Pearson JV, et al. Common Kibra alleles are associated with human memory performance. Science. 2006;314:475–8.
Corneveaux JJ, Liang WS, Reiman EM, Webster JA, Myers AJ, Zismann VL, et al. Evidence for an association between KIBRA and late-onset Alzheimer’s disease. Neurobiol Aging. 2010;31:901–9.
Acknowledgements
Not applicable.
Funding
This study was funded by the National Science Center, grant numbers 2011/01/B/NZ5/05291 (to AH) and 2011/02/A/NZ5/00339 (to JO).
Availability of data and materials
GWAS datasets described in the manuscript are available from the GEO database (GSE79094).
Authors’ contributions
Conception and design of the study: AH and JO; all authors participated in generation, collection, assembly, analysis, and interpretation of data; performed statistical analysis: KG; drafting of the manuscript: JO, AH, KG, and MM. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The study was approved by the ethics committee (decision 46/PW/2011) of the Medical Center for Postgraduate Education, Warsaw, Poland, and all participants provided written informed consent. The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki.
Author information
Authors and Affiliations
Corresponding author
Additional files
Additional file 1: Figure S1.
Plot of first four principal components (PC) for: full dataset (A) and dataset after removal of outlier samples (B). Arrows indicate samples removed from analyses. PBC, primary biliary cholangitis; PSC, primary sclerosing cholangitis. (DOCX 298 kb)
Additional file 2: Table S1-S3.
Table S1. A summary of significant primary biliary cholangitis (PBC) loci selected based on GWAS results replicated by individual patient TaqMan genotyping. Position - position of a given loci on chromosome (GRCh37); GENESYMBOL - symbol of a gene SNP is located in, provided SNP is located within gene; PRECEDESYMBOL/FOLLOWSYMBOL - symbol of genes flanking given SNP, p-value - result of TagMan replication assessed with Fisher’s exact test; OR - odds ratio; PBC vs control (1st/2nd analysis) - indication whether given SNP met selection criterion in GWAS analysis, 1 = YES. Yellow marks SNPs significant in ‘PSC vs control’ comparison. Table S2. A summary of primary sclerosing cholangitis (PSC) loci selected based on GWAS results replicated by individual patient TaqMan genotyping. Position - position of a given loci on chromosome (GRCh37); GENESYMBOL - symbol of a gene SNP is located in, provided SNP is located within gene; PRECEDESYMBOL/FOLLOWSYMBOL - symbol of genes flanking given SNP, p-value - result of TaqMan replication assessed with Fisher’s exact test; OR - odds ratio; PSC vs control (1st/2nd analysis) - indication whether given SNP met selection criterion in GWAS analysis, 1 = YES. Yellow marks SNPs significant in ‘PBC vs control’ comparison. Table S3. Swiss-Prot Protein Information Resource Terms significantly overrepresented among genes associated with PBC and PSC in this study. (XLSX 21 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Paziewska, A., Habior, A., Rogowska, A. et al. A novel approach to genome-wide association analysis identifies genetic associations with primary biliary cholangitis and primary sclerosing cholangitis in Polish patients. BMC Med Genomics 10, 2 (2017). https://doi.org/10.1186/s12920-016-0239-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12920-016-0239-9