Abstract
Background
The Digital X-ray Radiogrammetry (DXR) method measures the cortical bone thickness in the shafts of the metacarpals and has demonstrated its relevance in the assessment of hand bone loss caused by rheumatoid arthritis (RA). The aim of this study was to validate a novel approach of the DXR method in comparison with the original version considering patients with RA.
Method
The study includes 49 patients with verified RA. The new version is an extension of the BoneXpert method commonly used in pediatrics which has these characteristics: (1) It introduces a new technique to analyze the images which automatically validates the results for most images, and (2) it defines the measurement region relative to the ends of the metacarpals. The BoneXpert method measures the Metacarpal Index (MCI) at the metacarpal bone (II to IV). Additionally, the MCI is quantified by the DXR X-posure System.
Results
The new version correctly analyzed all 49 images, and 45 were automatically validated. The standard deviation between the MCI results of the two versions was 2.9% of the mean MCI. The average Larsen score was 2.6 with a standard deviation of 1.3. The correlation of MCI to Larsen score was −0.81 in both versions, and there was no significant difference in their ability to detect erosions.
Conclusion
The new DXR version (BoneXpert) validated 92% of the cases automatically, while the same good correlation to RA severity could be presented compared to the old version.
Similar content being viewed by others
Background
Conventional radiogrammetry measures distances in radiographs to estimate the thickness of the cortical bone partition. For over 50 years it has been used for the assessment of osteoporosis [1–3]. This method measures total width of a bone and the cortical thickness at the mid-point of the second metacarpal of the non-dominant hand. Based on the measured data the Metacarpal Index (MCI) as ratio of total bone width and cortical thickness can be calculated or the Barnett and Nordin Index as percentage cortical thickness [1]. Further investigations implement the Garn Index which characterised the cortical area [4] or the Exton-Smith index as the ratio of the cortical area to the total transverse area [5]. These indices of conventional radiogrammetry quantify the amount of cortical bone. Despite conventional radiogrammetry being relatively inexpensive and widely available, the technique has significant limitations regarding the imprecision due to the difficulty in identification of the endosteal margin and precise marking of the mid shaft location by the operator of the radiogrammetrical measurements [6].
Based on the conventional Radiogrammetry technique a digital version named as Digital X-ray Radiogrammetry (DXR) for the measurement of MCI at the metacarpal bones was developed and marketed as the X-posure System [7]. The DXR method measures MCI at the metacarpal bones II to IV with a high precision and in a highly reproducible way [8, 9]. The main field of application of the DXR is the quantification of periarticular metacarpal bone loss in patients with RA [10]. The periarticular bone loss as detected by the MCI is strongly associated with the disease activity in RA [11]. Cross-sectional studies have shown a strong association between reduced metacarpal index as measured by DXR and radiographically visible joint destruction [12–15], indicating that DXR-estimates function as surrogate marker of radiographic progression [10]. Longitudinal studies have also confirmed that early periarticular bone loss may be a predictor of subsequent radiographic joint damage [16–19].
Until now, the BoneXpert method has been used for the automatic determination of bone age in children [20–27]. A newly developed version of the BoneXpert-method is now available for the measurement of the MCI in adults. The BoneXpert-method is also able to quantify a new parameter, the Bone Health Index (BHI).
The aim of this study was to evaluate the new automated BoneXpert method in comparison with the original version of DXR in RA patients. The comparison focused on the agreement of their measurements to estimate MCI and on the correlation to the RA severity as estimated by the Larsen Score. Additionally, the potential of BHI in the quantification of periarticular bone loss was evaluated.
Methods
Study population
We included 49 patients (38 females and 11 males, mean (±SD) age: 66.7 years ± 5.7 years) suffering from verified RA diagnosed according to the revised criteria of the American College of Rheumatology in 1987 [28]. The median disease duration was 2.4 ± 2.5 years. The mean C-reactive protein was 11.3 mg/l and/or the mean Erythrocyte Sedimentation Rate 1st hour was 25 mm. No pre-selection regarding severity of RA or steroid therapy was performed. All patients were treated with disease-modifying antirheumatic drugs (Methotrexat n = 37, Leflunomide n = 12) (details see Table 1).
For all patients, radiographs of the hand were performed under standardized technical conditions (tube voltage 42 kV, exposure level 6 mAs, film focus distance 100 cm, film Agfa cruix).
Methods
Scoring of hand radiographs
Each radiograph of the RA-cohort was scored by two radiologists blinded to each other using the modified Larsen Score which evaluates 32 joints of the feet and hands (total sum of points: 160): score 0 = normal joint; score 1 = periarticular demineralization, soft tissue affection, initial reduction of the joint space width; score 2 = initial erosions and reduction of the joint space width; score 3 = multiple erosions and advanced reduction of the joint space width; score 4 = partial ankylosis; score 5 = ankylosis or mutilation [29] (see Fig. 1). The individual sum of scoring points was then divided by the evaluated joints. In cases of ambiguity, a third highly experienced radiologist reviewed the radiographs for a final decision.
a Normal hand X-ray without signs of RA b Demineralisation of the metacarpal bone, joints space narrowing of the metacarpophalangeal joint I to V (asterix) and erosions of the metacarpophalangeal joint (arrows) c Severe demineralisation of the metacarpal bones as well as advanced joint space narrowing of the carpus and metacarpophalangeal joint I to V (asterix) with total loss of joint space at the metacarpophalangeal joint II and III, erosive destruction of the metacarpophalangeal joint III and subluxation of the metacarpophalangeal joint I
The X-Posure System
The X-posure System (XP, Pronosco X-Posure System™, Version 2.0; Sectra; Linköping, Sweden, see Fig. 2) was applied to estimate cortical thickness (TXP), metacarpal bone width (WXP) and Metacarpal Index (MCIXP), requiring conventional or digital radiographs of the hand in an anterior-posterior projection [7].
The radiographs were digitised (Scanner UMAX Power Look 1100) in resolution 300 dots per inch by the XP-system. XP performed a continuous self-checking of the scanning process to maintain an optimal quality of the digital X-ray imaging; the analysis process is halted, if the X-ray imaging becomes inferior during the contour finding process (e. g. false identification of bone structures).
After digitalization of the hand radiographs, the method automatically defined regions of interest around the narrowest bone parts of the metacarpals II, III and IV and subsequently determined the outer and inner cortical edges of the identified cortical bone parts. There is no operator interaction in the XP-measurements. The XP-parameters were calculated as follows:
-
A.
MCIXP is a dimensionless parameter calculated as the ratio of cortical thickness to outer metacarpal width [30, 31]:
$$ \mathrm{M}\mathrm{C}{\mathrm{I}}_{\mathrm{XP}} = 2\ {\mathrm{T}}_{\mathrm{XP}}/\ {\mathrm{W}}_{\mathrm{XP}}. $$ -
B.
Cortical thickness TXP is computed as the mean over the three bones.
-
C.
The outer bone diameter WXP was measured as the entire width of the second, third and fourth metacarpal bones including the two cortical regions and the medullary cavity. WXP was calculated as the mean over the three bones [7].
BoneXpert adult
The BoneXpert system (BX, Version 2.1, Visiana, Holte, Denmark) is a medical device for analysis of pediatric hand X-rays for automated determination of bone age. It also includes an implementation of the DXR method for determination of bone health index in children [32]. In this study we use a new version of BX, called BX Adult (Version 2.3), which extends the DXR method to adults up to age of 90 y.
The new DXR analysis applies more advanced image analysis compared to the original implementation. Instead of locating marks only on the shafts of the metacarpals, the new method locates 32 marks all around each metacarpal II-V. This means the whole of the bones are recognised by the method and if the bones do not appear as a likely instance of such bones, it is a sign that the analysis is not reliable. In this way, the method is able to know when there is an error, in other words, it is able to validate its own recognition of the bones.
Two of the 32 marks identify the proximal and distal ends, which define the bone axis and the bone length LBX. A region of interest (ROI) is placed with its centre at 44% of LBX from the proximal end, and the length of the ROI is 25% of LBX. The original method placed the ROIs at the location where the metacarpals are narrowest. We consider placing the ROIs relative the ends of the metacarpals to be anatomically more correct, and it is also more robust.
In each ROI, the outer border of the cortex is defined at the location of maximum gradient, while the inner border is at the maximum radio-opacity. The average cortical thickness TBX and the bone width WBX are determined in each ROI, and from these, the cortical area is defined as
Four bone indices are computed from this. Here we mention the Bone Health Index and the metacarpal index
These computations are done in each metacarpal, and the final indices are formed as averages over the three bones.
BoneXpert Adult validates the analysis automatically, or rejects the analysis automatically. However, a certain fraction of the images fall in an in-between category of “questionable images” where the analysis can neither be automatically accepted nor rejected. These are presented to the clinician for verification. The idea of this design is that there should as few questionable images as possible, but this feature has not previously been validated for RA patients. In this study we visually inspect all the BoneXpert analyses to verify that those automatically validated are indeed valid, and to determine the percentage of questionable images which are valid.
Statistical analysis
The statistical analysis included the following elements
-
I.
Evaluation of the BoneXpert self-validation.
-
II.
For the comparison of the XP and BX methods, we define a variant of MCI for BX, because BX uses the definition MCIBX = ABX/WBX 2, while X-posure uses the definition MCIXP = 2 TXP/WXP. Therefore MCIBX-naive = 2 TBX/WBX was defined . Furthermore, since the ROI is in general larger (around 30% on average) in XP than the 25% used in BX, BX finds on average larger MCI values. Therefore, a correction factor is defined to adjust for this, and an adjusted MCI is defined as MCIBX-adj = MCIBX-naive/1.084, where the factor was derived from the data in this study.
-
III.
The relation of XP- and BX-parameters to Larsen-Score 1 and 5 is assessed by the correlation, and we test for significant difference in correlation by a boot-strapping method, i.e. using resampling of the data with replacement, reference: Armitage page 298 an onwards, https://archive.org/details/StatisticalMethodsInMedicalResearch.
-
IV.
The relation of XP- and BX-parameters to occurrence of erosion is assessed by the correlation, and again we test for significant differences by a boot-strapping method.
The significance level was set to p < 0.05.
Results
Self-validation of the BoneXpert
BX was able to analyse all 49 images, and 45 were automatically validated. The 4 images flagged for visual clearance were all found to be correctly analysed by BX. Three of these “questionable” radiographs had Larsen Score 5 and one had Larsen Score 4. The XP method requires visual clearance of all images, and all were found to be correctly analysed. So both methods were able to analyse cases with extensive joint involvement caused by RA. Some examples are shown in Fig. 3.
Examples of BoneXpert analyses of three images with relatively advanced RA showing how the borders of metacarpals have been located. These three cases were “self-validated” by BoneXpert. a strong erosion at caput 5, b Strong erosion at caput 5 and a slight segmentation error at caput 2 and 4, c Strong erosions at all four caputs, but despite this, a rater accurate segmentation of the metacarpal bones
Comparison of the Metacarpal Index between both techniques
The comparison of XP and BoneXpert MCI is shown in Fig. 4. It reveals a good agreement: The SD between them is 2.9% of the mean MCI. The coefficient of correlation between MCIXP and MCIBX-naive was r = 0.987 (p < 0.001). Comparable results were documented for TXP and TBX (r = 0.991, p < 0.01).
The association between Metacarpal Index and severity of rheumatoid arthritis
The relation between MCI determined by BX and the Larsen Score is shown in Fig. 5. The coefficient of correlation is r = −0.811 for BX. It is r = −0.807 for the X-posure system. The bootstrapping method showed that this difference is not statistically significant – it would need to be at least 0.026 to be significant; here it is 0.004.
The association between Metacarpal Index and erosions
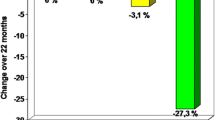
Figure 6 shows histograms of MCI for cases with and without erosions.
To test whether one method is better than the other in separating these two groups, we computed the correlation between MCI and a 0–1 variable indicating erosions. The correlations were r = −0.828 for the X-posure system and −0.807 for BoneXpert. The bootstrapping method showed than this difference is not significant.
Furthermore, the patients with erosions presented a significantly reduced MCI for both techniques (MCIXP: −24.1%; MCIBX-naive: −19.2%).
The Bone Health Index for the quantification of periarticular bone loss in rheumatoid Arthritis
The BHI presented a negative coefficient of correlation (r = 0.595, p < 0.01) to the Larsen Score. In this context, a reduction of BHI between the Larsen Score 1 to Larsen Score 5 was verified with 29.5% (p < 0.05). RA-patients with erosions revealed a significant lower BHI with −24.0% compared to the RA-patients without erosions.
Discussion
The BoneXpert-technique is a new developed automated Digital X-ray Radiogrammetry method for the measurement of the Metacarpal Index. The objective of this study was the comparison of the BoneXpert technique to the established X-posure system considering the agreement of their measurements of the MCI as well as their correlation to the Larsen score and erosions.
Correct placement of ROIs
The RA-related destructions of the metacarpal bone, especially at the metacarpal joints [33] could present a challenge for a method like BoneXpert which relies on locating the metacarpal ends.
Likewise, the X-posure System could place the ROIs on the wrong bones or obviously wrong (too distal or too proximal), perhaps due to artefacts of the radiographs or abnormal bone shapes.
The new BoneXpert method includes a method for self-validation of the analysis. In this study 45 hand radiographs of the patients with RA and with different stages of radiographic destruction were automatically accepted by the self-validation process of the BoneXpert technique. The remaining 4 cases required visual verification and were found to be analysed correctly. These results show that BX works reliably in this patient group. XP was also found to work reliable on all images.
A potential advantage of the new BX method is its ability to self-validate the image analysis, which could lead to a better workflow and a more reliable result. More studies are required to demonstrate such an advantage, for instance including images of poorer quality which challenge the methods more. In this study all images were analysed correctly by both methods, and this is suspected not to be true in general.
A potential advantage of the new BX method is its more appropriate definition of measurement ROI, which adjust its size to the patient size. It also allows the method to be used consistently on images with unknown magnification. However, the comparison with RA severity in this study showed no advantage of BX. Larger studies are required to clarify this issue.
Comparison of Metacarpal Index estimated by the X-posure System and the BoneXpert
A direct comparison of the absolute MCI values is not possible, based on different procedures of the ROI positioning and configuration by the BX- and XP-techniques. But the study revealed a high correlation (r = 0.983, r 2 = 0.966, p < 0.001) of the MCI between the X-posure System and the BoneXpert. The XP-System centres the ROI at the narrowest point of the metacarpal shaft of the metacarpal bones II to IV. And it used a fixed size of the ROI. The BX-technique centres the ROI 44% from the proximal end of the metacarpal bone and the ROI scaled 25% to the bone length. The ROI location of the BX allows a more anatomically correct location of the metacarpal bone.
Quantification of Metacarpal Index
Using the Larsen Score, MCIBX (r = −0.811) and MCIXP (r = −0.807) presented a significant correlation to the severity of RA. A study of Böttcher et al. (2006) also revealed a high correlation with different radiographic scoring methods in RA [34]. In this context, the MCI as surrogate marker for the periarticular demineralization could be reliably quantified by XP and BX. Periarticular demineralization of the metacarpals has been implemented as a diagnostic feature to classify bone involvement in RA, both in the Steinbroker Score as well as by the Larsen Score [35, 36]. Periarticular loss at the metacarpal bones has obviously functioned as the first radiological sign of RA considered by the scoring methods, and may be found before erosions or joint space narrowing occurs. Additionally, different cross-sectional studies have observed a strong relationship between reduced periarticular cortical bone mass as measured by DXR and radiographic joint destruction [12, 17, 34].
The relation of erosions and Metacarpal Index
We also explored BX and XP for their diagnostic impact in the assessment of erosions. Our data revealed a significant reduced BX-MCI and XP-MCI in RA-patients with erosions. These results clearly demonstrate that periarticular osteoporosis as quantified by MCI is a predictive value in the detection of erosions.
The Bone Health Index as a new parameter of the quantification of periarticular demineralization
We have presented data for two indices of cortical bone: MCI and BHI. They differ by using different ways to adjust for the size of the patient. The MCI is dimensionless, so it so to speak makes a complete compensation for the size, and it has the advantage that its measurement is invariant to a magnification of the X-ray image. The BHI makes a different adjustment to the dimensions of the patient, including the bone width as well as the bone length. When the BHI was introduced [32] it was conjectured that its particular adjustment was clinically more relevant than the one used in other indices, including the MCI, but it remains a hypothesis. In the data we have presented here, there is no significant difference in the performance or clinical relevance of BHI and MCI.
In this context, periarticular demineralisation, which is a characteristic feature of inflammatory bone involvement in RA, may be more valuable in the early diagnosis of RA as joint space narrowing and erosions. As demineralisation is difficult to ascertain by simple visualization of radiographs [36], BX and XP offer the benefit of a reliable quantification of periarticular bone mass in an observer-independent and highly reproducible manner [8].
One limitation of the study is based on the size of the study cohort, which reflected the proof of concept of the study. In this context, longitudinal studies were necessary to evaluate the diagnostic performance of the BX-technique, especially under consideration of therapeutic regimes in RA.
Conclusion
In conclusion, the development of Digital X-ray Radiogrammetry has promoted the precise quantification of Metacarpal Index [37] and hand bone mass calculated by BX and XP. The clinical use of the BX-technology also allows the measurement of MCI as the traditional XP-system in patients suffering from RA. Consequently, BX-MCI is able to function as a characteristic surrogate marker for RA progression which also may improve the planning of appropriate individual therapeutic strategies.
Abbreviations
- ABX :
-
Cortical area in mm2 as estimated by BoneXpert
- BHI:
-
Bone Health Index estimated by BoneXpert
- BX:
-
BoneXpert method
- DXR:
-
Digital X-ray Radiogrammetry
- LBX :
-
Length of the metacarpal bone in mm as measured by BoneXpert
- MCIBX :
-
Metacarpal Index as measured by BoneXpert
- MCIBX-adj :
-
MCIBX-naïve / 1.084
- MCIBX-naïve :
-
Metacarpal Index as measured by BoneXpert with a definition similar to the one used in X-posure
- MCIXP :
-
Metacarpal Index as measured by X-Posure System
- RA:
-
Rheumatoid arthritis
- ROI:
-
Region of interest
- TB :
-
Cortical thickness of the metacarpal bone in mm as measured by BoneXpert
- TXP :
-
Cortical thickness of the metacarpal bone in cm as measured by X-Posure System
- WBX :
-
Average width of the metacarpal bone in mm as measured by BoneXpert
- WXP :
-
Average width of the metacarpal bone in cm as measured by X-Posure System
- XP:
-
X-posure System
References
Barnett E, Nordin B. The radiological diagnosis of osteoporosis: a new approach. Clin Radiol. 1960;11:166–74.
Meema H. The occurrence of cortical bone atrophy in old age and osteoporosis. J Can Assoc Radiol. 1962;13:27–32.
Meema H, Meema S. Measuable roentgenologic changes in some peripheral bones in senile osteoporosis. J Am Geriatr Soc. 1963;11:1170–82.
Garn S, Poznanski A, Nagy J. Bone measurement in the differential diagnosis of osteopenia and osteoporosis. Radiology. 1971;100:509–18.
Exton-Smith A, Millard P, Payne P, Wheeler E. Method of measuring quantity of bone. Lancet. 1969;2:1153–7.
Böttcher J, Pfeil A, Schäfer ML, Petrovitch A, Seidl BE, Mentzel HJ, Lehmann G, Malich A, Heyne JP, Hein G, Wolf G, Kaiser WA. Normative data for digital X-ray radiogrammetry from a female and male German cohort. J Clin Densitom. 2006;9:341–50.
Rosholm A, Hyldstrup L, Baeksgaard L, Grunkin M, Thodberg HH. Estimation of bone mineral density by digital X-ray radiogrammetry: theoretical background and clinical testing. Osteoporos Int. 2001;12:961–9.
Böttcher J, Pfeil A, Rosholm A, Malich A, Petrovitch A, Heinrich B, Lehmann G, Mentzel HJ, Hein G, Linss W, Kaiser WA. Influence of image-capturing parameters on digital X-ray radiogrammetry. J Clin Densitom. 2005;8:87–94.
Pfeil A, Renz DM, Fröber R, Hansch A, Lehmann G, Sommerfeld J, Malich A, Wolf G, Böttcher J. Influence of angulation on metacarpal bone mineral density measurements using digital X-ray radiogrammetry. Int J Comput Assist Radiol Surg. 2015;10:587–92.
Pfeil A, Haugeberg G, Hansch A, Renz DM, Lehmann G, Malich A, Wolf G, Böttcher J. The value of digital X-ray radiogrammetry in the assessment of inflammatory bone loss in rheumatoid arthritis. Arthritis Care Res (Hoboken). 2011;63:666–74.
Böttcher J, Pfeil A, Mentzel HJ, Kramer A, Schäfer ML, Lehmann G, Eidner T, Petrovitch A, Malich A, Hein G, Kaiser WA. Peripheral bone status in rheumatoid arthritis evaluated by Digital X-ray Radiogrammetry (DXR) and compared with multi-site Quantitative Ultrasound (QUS). Calcif Tissue Inter. 2006;78:25–34.
Haugeberg G, Lodder MC, Lems WF, Uhlig T, Ørstavik RE, Dijkmans BAC, Kvien T, Woolf AD. Hand cortical bone mass and its associations with radiographic joint damage and fractures in 50–70 year old female patients with rheumatoid arthritis: cross sectional Oslo-Truro-Amsterdam (OSTRA) collaborative study. Ann Rheum Dis. 2004;63:1331–4.
Böttcher J, Malich A, Pfeil A, Petrovitch A, Lehmann G, Heyne JP, Hein G, Kaiser WA. Potential clinical relevance of digital radiogrammetry for quantification of periarticular bone demineralization in patients suffering from rheumatoid arthritis depending on severity and compared with DXA. Eur Radiol. 2004;14:631–7.
Böttcher J, Pfeil A, Rosholm A, Schäfer ML, Malich A, Petrovitch A, Mentzel HJ, Hein G, Kaiser WA. Computerized digital imaging techniques provided by Digital Radiogrammetry as new diagnostic tool in rheumatoid arthritis. J Digit Imaging. 2006;19:279–88.
Forslind K, Boonen A, Albertsson K, Hafstrom I, Svensson B. Hand bone loss measured by digital X-ray radiogrammetry is a predictor of joint damage in early rheumatoid arthritis. Scand J Rheumatol. 2009;38:431–8.
Hoff M, Haugeberg G, Ødegård S, Syversen S, Landewé R, van der Heijde D, Kvien TK. Cortical hand bone loss after 1 year in early rheumatoid arthritis predicts radiographic hand joint damage at 5-year and 10-year follow-up. Ann Rheum Dis. 2009;68:324–9.
Böttcher J, Pfeil A, Rosholm A, Petrovitch A, Seidl BE, Malich A, Kramer A, Lehmann G, Hein G, Kaiser WA. Digital X-Ray Radiogrammetry combined with semi-automated analysis of joint space distances as a new diagnostic approach in rheumatoid arthritis – A cross-sectional and longitudinal study. Arthritis Rheum. 2005;52:3850–9.
Böttcher J, Pfeil A. Diagnosis of periarticular osteoporosis in rheumatoid arthritis using Digital X-ray Radiogrammetry. Arthritis Res Ther. 2008;10:103.
Hoff M, Haugeberg G, Kvien TK. Hand bone loss as an outcome measure in established rheumatoid arthritis: 2-year observational study comparing cortical and total bone loss. Arthritis Res Ther. 2007;9:R81.
Thodberg HH, Kreiborg S, Juul A, Pedersen KD. The BoneXpert method for automated determination of skeletal maturity. IEEE Trans Med Imaging. 2009;28:52–66.
van Rijn RR, Lequin MH, Thodberg HH. Automatic determination of Greulich and Pyle bone age in healthy Dutch children. Pediatr Radiol. 2009;39:591–7.
Martin DD, Deusch D, Schweizer R, Binder G, Thodberg HH, Ranke MB. Clinical application of automated Greulich-Pyle bone age determination in children with short stature. Pediatr Radiol. 2009;39:598–607.
Thodberg HH, Jenni OG, Caflisch J, Ranke MB, Martin DD. Prediction of adult height based on automated determination of bone age. J Clin Endocrinol Metab. 2009;94:4868–74.
Martin DD, Sato K, Sato M, Thodberg HH, Tanaka T. Validation of a new method for automated determination of bone age in Japanese children. Horm Res Paediatr. 2010;73:398–404.
Thodberg HH, Neuhof J, Ranke MB, Jenni OG, Martin DD. Validation of bone age methods by their ability to predict adult height. Horm Res Paediatr. 2010;74:15–22.
Thodberg HH, Sävendahl L. Validation and reference values of automated bone age determination for four ethnicities. Acad Radiol. 2010;17:1425–32.
Thodberg HH, Jenni OG, Ranke MB, Martin DD. Standardization of the Tanner-Whitehouse bone age method in the context of automated image analysis. Ann Hum Biol. 2012;39:68–75.
Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fies FJ, Cooper NS. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988;31:315–24.
Larsen A, Thoen J. Hand radiography of 200 patients with rheumatoid arthritis repeated after an interval of one year. Scand J Rheumatol. 1987;16:395–401.
Hyldstrup L, Nielsen SP. Metacarpal index by digital X-ray radiogrammetry: normative reference values and comparison with dual X-ray absorptiometry. J Clin Densitom. 2001;4:299–306.
Jorgensen JT, Andersen PB, Rosholm A, Bjarnason NH. Digital X-ray radiogrammetry: a new appendicular bone densitometric method with high precision. Clin Physiol. 2000;20:330–5.
Thodberg HH, van Rijn RR, Tanaka T, Martin DD, Kreiborg S. A paediatric bone index derived by automated radiogrammetry. Osteoporos Int. 2010;21:1391–400.
Pfeil A, Oelzner P, Bornholdt K, Hansch A, Lehmann G, Renz DM, Wolf G, Böttcher J. Joint damage in rheumatoid arthritis: assessment of a new scoring method. Arthritis Res Ther. 2013;15:R27.
Böttcher J, Pfeil A, Rosholm A, Sörös P, Petrovitch A, Schaefer ML, Seidl BE, Malich A, Hansch A, Wolf G, Kaiser WA. Computerized quantification of joint space narrowing and periarticular demineralization in patients with rheumatoid arthritis based on digital x-ray radiogrammetry. Invest Radiol. 2006;41:36–44.
Steinbroker O, Traeger CH, Batterman RC. Therapeutic criteria in rheumatoid arthritis. JAMA. 1949;140:659–62.
Larsen A, Dale K, Eek M. Radiographic evaluation of rheumatoid arthritis and related conditions by standard reference films. Acta Radiol Diagn. 1977;18:481–91.
Pfeil A, Oelzner P, Renz DM, Hansch A, Wolf G, Böttcher J. Is there a role for Digital X-ray Radiogrammetry as surrogate marker for radiological progression and imaging of structural integrity in rheumatoid arthritis? BMC Musculoskelet Disord. 2015;16:155.
Acknowledgements
The authors thank Thomas Lehmann (PhD) for the statistical advice. The authors also thank Monika Arens (managing director, Arewus GmbH) and Jacob Algulin (Sectra, Sweden) for the use of the X-posure system. There is no funding support for this study.
Funding
There is no funding regarding the study.
Availability of data and material
Data will not be shared as it contains clinical patient data from the Jena University Hospital which were not allowed to share by the law. Additionally, the patients have been asked to publicly share their data, and thus they have not consented to sharing their data freely to any scientists.
Authors’ contributions
AP designed the study, collected the data, analysed the radiographs, performed the statistical analysis and wrote the manuscript. HH performed the BX-measurements and participated on the statistical analysis, manuscript editing as well as on the study design. DR: performed the scoring of the radiographs and the DXR-measurements. LR performed the data collection and participated on the statistical analysis. PO performed the clinical data collection and edited the manuscript. GW wrote and edited the manuscript. JB participated on the study design, performed the scoring of the hand X-ray and wrote the manuscript. All authors read and approved the final manuscript.
Competing interest
HHT is the owner of Visiana, which develops and markets the BoneXpert medical device. The other authors declare that they have no conflict of interest.
Consent for publication
Not applicable.
Ethical approval and consent to participate
All examinations were performed in accordance with the rules and regulations of the local Human Research and Ethics Committeé of the Friedrich-Schiller-University Jena. The study is retrospective analysis of pre-existing clinical data. Based on the regulations of the ethics committee of the Friedrich-Schiller-University Jena a separate consent from any patient was not necessary in the analysis of retrospective analysis of pre-existing clinical data. As a special note, the authors emphasize that all radiographs used for the BoneXpert- and DXR-calculations were performed as part of routine clinical care; no additional radiographs were obtained only for study purposes.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Pfeil, A., Thodberg, H.H., Renz, D.M. et al. Metacarpal bone loss in patients with rheumatoid arthritis estimated by a new Digital X-ray Radiogrammetry method – initial results. BMC Musculoskelet Disord 18, 6 (2017). https://doi.org/10.1186/s12891-016-1348-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-016-1348-5