Abstract
Background
The maximal expiratory flow at 50 % of the forced vital capacity (MEF50) is the flow where half of forced vital capacity (FVC) remains to be exhaled. A reduced MEF50 has been suggested as a surrogate marker of small airways disease. The diagnostic and prognostic utility of this easy to assess spirometric variable in persons with respiratory symptoms, but without COPD is unclear.
Methods
We used data from the UHFO-COPD cohort in which 405 community-dwelling persons aged 65 years or over, and a general practitioner’s diagnosis of chronic obstructive pulmonary disease (COPD) underwent pulmonary function testing and echocardiography. In total 161 patients had no COPD according to the spirometric GOLD criteria. We considered MEF50 as reduced if < 60 % of predicted.
Results
Of the 161 patients without COPD (mean age 72 ± 5.7 years; 35 % male; follow-up 4.5 ± 1.1 years), 61 (37.9 %) had a reduced MEF50. They were older, had more pack-years of smoking, more respiratory symptoms, and used more frequently inhaled medication than the remaining 100 subjects. A reduced MEF50 was nearly twice as often associated with newly detected heart failure (HF) at assessment (29.5 % vs. 15.6 %, p = 0.045). In age-and sex-adjusted Cox regression analysis, a reduced MEF50 was significantly associated with episodes of acute bronchitis (hazard ratio 2.54 95 % confidence interval (1.26; 5.13) P = 0.009), and in trend with pneumonia (2.14 (0.98; 4.69) P = 0.06) and hospitalizations for pulmonary reasons (2.28 (0.93; 5.62) P = 0.07).
Conclusions
In older community-dwelling persons with pulmonary symptoms but without COPD, a reduced MEF50 may help to uncover unrecognized HF, and identify those at a higher risk for episodes of acute bronchitis, pneumonia and hospitalizations for pulmonary reasons. Echocardiography and close follow-up should be considered in these patients.
Similar content being viewed by others
Background
The maximal expiratory flow at 50 % of the forced vital capacity (MEF50) is the flow where half of forced vital capacity (FVC) remains to be exhaled [1]. It corresponds to the forced expiratory flow at 50 % (FEF50) and correlates highly with the maximum mid-expiratory flow (FEF25-75 %) [2]. As such, MEF50 indicates obstruction of small airways and may be used as a surrogate of early small airways disease defined by an abnormally low mid-expiratory flow in the presence of normal forced expiratory volume in 1 second (FEV1), FVC, and FEV1/FVC ratio [3].
The usefulness of forced expiratory flows to diagnose small airways disease is, however controversial, as intra-individual variability is high, even in healthy subjects [4, 5]. Especially in the presence of central obstructive ventilatory disorders such as COPD or asthma, forced expiratory flow parameters lack reproducibility and do not correlate well with other variables related to airway obstruction (as forced vital capacity, FVC and residual volume-total lung capacity index, (RV/TLC) [6, 7]. However, in absence of central obstructive disorders, e.g. in patients with symptoms suggestive of COPD but in whom COPD has been excluded spirometrically, a low maximal expiratory flow and small airways disease may strongly suggest an alternative diagnosis, e.g. primary bronchiolar disorders (bronchiolitis) or interstitial lung diseases with bronchiolar involvement [8]. Moreover, a low maximum expiratory flow might also direct differential diagnosis towards a non-pulmonary condition causing respiratory symptoms such as heart failure, either known or latent [9].
The aim of our analysis was to assess the prevalence and the potential prognostic value of a low post-dilatory MEF50, in older community-dwelling individuals with pulmonary symptoms of airways obstruction, but without COPD.
We assessed the relation of a low post-dilatory MEF50 with hitherto unknown heart failure, first episode of either acute bronchitis, pneumonia, hospitalizations for pulmonary reason, or all-cause mortality.
Methods
Study design and population
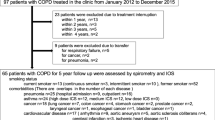
We made use of a data set derived from a prospective cohort study (UHFO-HF) investigating 405 patients aged ≥65 years with a clinical diagnosis of COPD in primary care. Population and study characteristics have been described in detail previously [10]. Patients clinically suspect of COPD but without spirometrically verified obstruction were recruited from 51 primary care practices and assessed in the outpatient clinic of the University Medical Center Utrecht, Netherlands. A standardized clinical examination, extensive pulmonary function testing (PFT), chest radiography, and echocardiography were performed in all participants [10]. Exclusion criteria comprised an already established diagnosis of heart failure, severe psychiatric disorder, immobility, and terminal illness with short life expectancy precluding study participation [10].
In 244 of 405 (60 %) patients from the original cohort COPD defined as a post-bronchodilator ratio of FEV1/FVC <0.7 according to the GOLD criteria could be spirometrically verified [11].
The present analysis refers to the remaining 161 patients with exclusion of a COPD diagnosis in spirometry. The study complied with the Declaration of Helsinki, and the Medical Ethics Committee of the University Medical Center Utrecht approved the study protocol. All participants gave their written informed consent.
Missing values
In four patients post-bronchodilator MEF50 values were missing. In these patients pre-bronchodilator measurements were used (two subjects with a MEF50 < 60 %, and two with a MEF50 > 60 % of predicted). Thus, the present study analyzes 161 patients without COPD.
Pulmonary function tests and definition of low MEF50
Pre-and post-bronchodilator pulmonary function testing was performed with a fixed-volume bodyplethysmograph (Masterlab Jaeger, Würzburg, Germany). The post-bronchodilator test was assessed 30 minutes after inhalation of 40 μg of ipratropium bromide.
There are no published guidelines regarding normal values for MEF50. We used 60 % of post-dilatory MEF50 predicted as cut-off in the presence of a post-dilatory FEV1/FVC ≥ 0.7 for defining low MEF50 [6]. Following the recommendations of the European Respiratory Society we used age, gender, and height for the calculation of the predicted values of all lung function parameters [12].
Blood test results
Laboratory results such as white blood cell count, haemoglobin, haematocrit, and serum aminoterminal pro-hormone B-type natriuretic peptide (NT-proBNP) were measured as part of the study assessment.
Echocardiography and definition of heart failure
Echocardiography was performed by two experienced cardiac sonographers using a Philips Sonos 5500 imaging system (Andover, MA, USA) and interpreted by a single cardiologist, who was blinded to clinical data [10]. Left ventricular ejection fraction (LVEF) was derived using Simpson’s biplane or, when not possible, by single plane area–length method [13].
Left atrial volume was calculated by the biplane area–length method from apical four-and two-chamber views and indexed to the body surface area [14]. Mitral inflow and pulmonary venous inflow were measured with pulsed-wave Doppler echocardiography. Tissue Doppler was used to assess the sub-mitral movement of the septal wall, and a composite of abnormalities in diastolic function was employed to define diastolic dysfunction [15].
Presence or absence of heart failure was established by an expert panel consisting of two cardiologists, a pulmonologist, and a general practitioner using all available diagnostic information, including echocardiography and pulmonary function tests [10]. Heart failure was classified by the panel in line with the recommendations of the ESC guidelines on heart failure. The definition required presence of signs and symptoms suggestive of heart failure and additional criteria that led to the following subtypes: a) “heart failure with a reduced ejection fraction” when LVEF was reduced (arbitrarily defined as ≤45 %); b) “heart failure with preserved ejection fraction” when echocardiographically determined diastolic dysfunction was present and LVEF >45 %; of note, symptoms and/or signs should not, or insufficiently, be explained by co-incident pulmonary disease; and c) “right-sided heart failure” (cor pulmonale) when LVEF was >45 %, and the calculated pulmonary artery pressure >40 mmHg [10].
Follow-up and outcomes ascertainment
Patients included in the study were followed from April 2001 to June 2007 during a mean period of 4.3 (standard deviation 1.1) years. The follow-up data collection mode was described before [16]. In brief, the general practitioner’s (GP) electronic medical files were scrutinized to obtain information on patient’s drug prescription, pulmonary hospitalizations and survival status. Acute bronchitis was defined as an episode with bronchial wheezing and rhonchi for which the GP prescribed antibiotics and/or pulse prednisolon for 7 to 10 days.
Most episodes of pneumonia were diagnosed clinically by the GP and only occasionally confirmed by chest X-ray or sputum culture.
Data analysis
Continuous data were expressed as mean (standard deviation, SD) or median (quartiles). Group comparisons between patients with and without a MEF50 < 60 % of predicted were performed using Fisher’s exact test or Mann–Whitney U-test, as appropriate (Tables 1 and 2). Correlations between MEF50 with other pulmonary function parameters were calculated with the Spearman rank order correlation coefficient (r). The strength of the correlation was graded using the following guide for the absolute value of r: 0.00-0.19 very weak; 0.20-0.39 weak; 0.40-0.59 moderate; 0.60-0.79 strong; 0.80-1.0 very strong.
Univariate, and age and sex adjusted multivariable Cox regression models were calculated for different outcomes (acute bronchitis, pulmonary hospitalizations, pneumonia, and all-cause mortality) and reported as hazard ratios (HR) with 95 % confidence intervals (CI). P values <0.05 were considered statistically significant. Data analysis was performed with SPSS 21 (IBM, Munich, Germany).
Results
Demographics of the patients with COPD according to the GOLD criteria
Patients excluded from our analysis (244 individuals with a GOLD diagnosis of COPD) were more often male (68 vs. 35 %, P < 0.001), and slightly older (73 [70; 77]) vs. 72 [67; 76] years P = 0.016) than the 161 patients included. All but one of the 243 patients with GOLD-COPD and available information on MEF had a post-dilatory MEF50 < 60 % of predicted confirming that a MEF50 below the chosen threshold is common in COPD.
Demographics of the patients without COPD according to the GOLD criteria
Table 1 lists the baseline characteristics of the 161 individuals under study, stratified by MEF50 </≥ 60 % of predicted. Patients with a low MEF50 (38 %) were older, had more pack-years of smoking, suffered more often from respiratory complaints, used more often inhaled medication (especially anticholinergics), and had higher leucocyte counts than subjects with a MEF50 ≥ 60 %. Twenty-two of the 63 patients (35 %) with a low MEF50 < 60 % of predicted had a FEV1 and/or FVC % of predicted below 80 %. The remaining 41 participants (65 %) had normal values of FEV1 and FVC % of predicted.
Correlation between MEF50 and other pulmonary function test results
Patients with a low MEF50 had a normal total lung capacity (TLC), while the carbon monoxide (CO) diffusion capacity was lower than in those with a MEF50 ≥ 60 % of predicted. Patients with a low MEF50 also had higher levels of total resistance, higher residual volume (RV) and larger RV/TLC ratio than subjects with a ‘normal’ MEF50 (Table 2). Reversibility of airway obstruction, defined as an increase of FEV1 levels > 200 ml and >12 % to baseline, did not differ between </≥ MEF50 60 % of predicted.
Table 3 presents Spearman rank-order correlation coefficients for the association between MEF50 and other continuous pulmonary function test parameters. MEF50 correlated moderately to strongly with all pulmonary function test results, except for TLC (no correlation) and RV (very weak correlation).
Association of low expiratory flow with newly detected heart failure
In total, N = 33 patients (20.5 %) were newly diagnosed with heart failure; N = 16 with heart failure with reduced ejection fraction, N = 17 with heart failure with preserved ejection fraction, and N = 0 isolated right-sided heart failure. A MEF50 < 60 % was associated with a new diagnosis of heart failure at the assessment: The incidence of newly diagnosed heart failure was 29.5 % in those with MEF50 < 60 % compared to 15.6 % in persons with a MEF50 ≥ 60 % of predicted (P = 0.045, Table 1).
Patients with a novel diagnosis of heart failure also had lower post-dilator MEF75 % of predicted (84 % [64; 103 %] vs. 97 % [86; 119 %], P = 0.03) than the 128 patients without heart failure, whereas peak expiratory flow and post-dilator MEF25 % were not different between these two groups. Patients with heart failure had more often FEV1 values below 80 % of predicted than subjects without heart failure (27 % vs. 12 %, P = 0.05). The corresponding FVC values were also numerically but not statistically different (FVC below 80 % of predicted 21 vs. 11 %, P = 0.15).
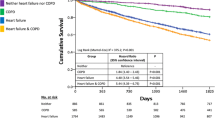
Association of low MEF50 with prognosis
During follow-up, 34 patients experienced acute bronchitis and 27 patients a pneumonia, 21 patients were hospitalized for a pulmonary reason (pneumonia, bronchitis, acute exacerbation of newly diagnosed COPD), and 17 patients died (Table 4). In age-and sex-adjusted Cox regression analysis, a low MEF50 was significantly associated with acute bronchitis (2.54 (1.26; 5.13) P = 0.009) but not with pneumonia (2.14 (0.98; 4.69) P = 0.06), hospitalizations (2.28 (0.93; 5.62) P = 0.07, Table 5) or death (1.84 (0.68; 4.99) P = 0.23). If patients with heart failure (n = 33) were excluded from the analysis the associations became significant for all outcome measures except total mortality (Table 5).
Discussion
In this retrospective analysis of 161 older community-dwelling individuals with a clinical diagnosis of COPD but without spirometrically verified airways obstruction, we found that low maximum mid-expiratory flow (i.e., MEF50 < 60 % of predicted) was prevalent in 38 %. These patients had increased pulmonary resistance and residual volumes, and a higher RV/TLC index than subjects with a MEF50 ≥ 60 %. Further, a low MEF50 was associated with incident heart failure and predicted a higher risk for acute bronchitis during follow-up.
Small airways disease is frequently found in patients with airways obstruction as asthma or COPD [6]. In the present study we did not see differences in the prevalence of low MEF50 in patients with and without a history of asthma. However, since our patients were selected according to a GP’s diagnosis of COPD, the prevalence of patients with a history of asthma was low (12 % in the total cohort). Reduced MEF is a characteristic feature of COPD [4]: in the original cohort of patients with verified COPD (244/405, data not shown) according to the GOLD criteria, a MEF50 < 60 % of predicted was detected in 242 out of 243 persons (data not shown). In the remaining patient, MEF values were not available. The prognostic capacity of low MEF is thus not meaningful in patients with established airways obstruction.
Lower MEF values may also be found in the absence of airways obstruction, in primary bronchiolar disorders or interstitial lung disease, but also in systemic inflammatory diseases such as rheumatoid arthritis [8]. A low MEF is easily detectable with spirometry and relates to inflammation of the small non-cartilaginous bronchioles with an internal diameter of <2 mm and may well be an indicator of small airways disease or be considered as a precursor stage of COPD [6, 17, 18]. However, to determine the underlying pathophysiological substrate, histological investigation of lung biopsies or high resolution computer tomography scans would be needed, procedures that are not part of the routine assessment in clinical practice and thus were not available for this study [8, 19].
Expiratory flow volumes have previously been proposed as a tool for diagnosing extra-pulmonary restrictive disease [9]. Heart failure is such a condition as increased heart size and pulmonary congestion may simply reduce lung volumes [20]. In addition, pulmonary fluid overload in heart failure may cause or aggravate external bronchial obstruction with subsequent compromise of FEV1 [20, 21]. Thus, clinically and spirometrically, heart failure frequently mimics COPD. Indeed, in congestive heart failure, it has been repeatedly be shown that FEV1 values may be more reduced than corresponding FVC values, yielding FEV1/FVC ratios <0.70 in the absence of COPD [22, 23]. Importantly, this finding (i.e., pseudo-COPD) is not reproducible when the same individuals are re-assessed after recompensation under euvolemic conditions, calling for a more conscious use of spirometry in these cases [21, 24, 25]. Additionally, expiratory flow measurements may be more susceptible to heart failure than FEV1 or FEV1/FVC: in 29.5 % of the cases with a MEF50 < 60 % of predicted, previously unrecognized heart failure was detected. This is more than three times as high as might be expected in the general population aged > 65 years (estimated prevalence of heart failure in this age group 7-10 %) [26] and also higher than the percentage of newly detected cases of heart failure in the 244 patients with a GOLD-COPD diagnosis (prevalence 21 %) from the original cohort [10, 27]. Further 18 out of 33 patients (55 %) with previously unrecognized heart failure had a MEF50 < 60 % predicted, whereas only 9 (27 %) had a reduced FEV1 < 80 % predicted.
Although our study convincingly related a reduced MEF50 to clinically relevant outcomes, we acknowledge that the causality of these associations is not stringent. Some studies found that MEF50 was below average in subgroups of healthy never smokers [4, 5], or asymptomatic subjects [28]. Further, higher body mass index levels may attenuate MEF [29], but we observed no relation between body mass index levels and low MEF50 (Table 1).
Study limitations
The extensive pulmonary function testing with spirometry, bodyplethysmography, and CO diffusion measurements was performed only once at baseline, thus, time-dependent effects could not be addressed. Because histological investigations or chest CT scans were not available in the GP setting of the current study, we were unable to assess small airways disease on a more pathophysiological basis. Further restrictive disorders might also account for MEF reduction. Patients with pulmonary restriction were not excluded in this study however, the prevalence in total cohort was low (3.1 %, N = 5) and there was no between group difference between patients with and without a MEF50 < 60 %.
Conclusions
In older community-dwelling patients with pulmonary symptoms but without central airway obstruction a low maximum MEF, easily obtained by spirometry, showed clinical utility to identify patients with previously undiagnosed heart failure and patients at risk for pulmonary events. Thus, MEF50 values should also be evaluated when obtaining spirometry in persons aged >65 years with shortness of breath.
Abbreviations
- CI:
-
Confidence intervals
- COPD:
-
Chronic Obstructive Pulmonary Disease
- DLCO:
-
Diffusion capacity of carbon monoxide
- FEV1:
-
Forced expiratory volume in 1 second
- FVC:
-
Forced vital capacity
- GOLD:
-
Global Initiative for Chronic Obstructive Lung Disease
- GP:
-
General practitioner
- HF:
-
Heart failure
- HR:
-
Hazard ratios
- LVEF:
-
Left ventricular ejection fraction
- MEF50:
-
Maximal expiratory flow at 50 % of the forced vital capacity
- NT-proBNP:
-
N-terminal pro-hormone B-type natriuretic peptide
- PEF:
-
Peak expiratory flow
- PFT:
-
Pulmonary function testing
- RV:
-
Residual volume
- Rtot:
-
Total resistance
- SD:
-
Standard deviation
- TLC:
-
Total lung capacity
References
Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of spirometry. Eur Respir J. 2005;26:319–38.
Bar-Yishay E, Amirav I, Goldberg S. Comparison of maximal midexpiratory flow rate and forced expiratory flow at 50 x% of vital capacity in children. Chest. 2003;123:731–5.
McFadden Jr ER, Linden DA. A reduction in maximum mid-expiratory flow rate. A spirographic manifestation of small airway disease. Am J Med. 1972;52:725–37.
Pellegrino R, Viegi G, Brusasco V, Crapo RO, Burgos F, Casaburi R, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005;26:948–68.
Quanjer PH, Stanojevic S, Cole TJ, Baur X, Hall GL, Culver BH, et al. Multi-ethnic reference values for spirometry for the 3-95-yr age range: the global lung function 2012 equations. Eur Respir J. 2012;40:1324–43.
Burgel PR. The role of small airways in obstructive airway diseases. Eur Respir Rev. 2011;20:23–33.
Sorkness RL, Bleecker ER, Busse WW, Calhoun WJ, Castro M, Chung KF, et al. Lung function in adults with stable but severe asthma: air trapping and incomplete reversal of obstruction with bronchodilation. J Appl Physiol (1985). 2008;104:394–403.
Burgel PR, Bergeron A, De Blic J, Bonniaud P, Bourdin A, Chanez P, et al. Small airways diseases, excluding asthma and COPD: an overview. Eur Respir Rev. 2013;22:131–47.
Zanen P, Folgering H, Lammers JW. Flow-volumes indices as means to discriminate between intra-and extrapulmonary restrictive disease. Respir Med. 2005;99:825–9.
Rutten FH, Cramer MJ, Grobbee DE, Sachs AP, Kirkels JH, Lammers JW, et al. Unrecognized heart failure in elderly patients with stable chronic obstructive pulmonary disease. Eur Heart J. 2005;26:1887–94.
Vestbo J, Hurd SS, Agusti AG, Jones PW, Vogelmeier C, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187:347–65.
Quanjer PH, Tammeling GJ, Cotes JE, Pedersen OF, Peslin R, Yernault JC. Lung volumes and forced ventilatory flows. Report Working Party Standardization of Lung Function Tests, European Community for Steel and Coal. Official Statement of the European Respiratory Society. Eur Respir J Suppl. 1993;16:5–40.
Schiller NB, Shah PM, Crawford M, DeMaria A, Devereux R, Feigenbaum H, et al. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am Soc Echocardiogr. 1989;2:358–67.
Tsang TS, Barnes ME, Gersh BJ, Bailey KR, Seward JB. Left atrial volume as a morphophysiologic expression of left ventricular diastolic dysfunction and relation to cardiovascular risk burden. Am J Cardiol. 2002;90:1284–9.
Garcia MJ, Thomas JD, Klein AL. New Doppler echocardiographic applications for the study of diastolic function. J Am Coll Cardiol. 1998;32:865–75.
Boudestein LC, Rutten FH, Cramer MJ, Lammers JW, Hoes AW. The impact of concurrent heart failure on prognosis in patients with chronic obstructive pulmonary disease. Eur J Heart Fail. 2009;11:1182–8.
Shaw RJ, Djukanovic R, Tashkin DP, Millar AB, Du Bois RM, Orr PA. The role of small airways in lung disease. Respir Med. 2002;96:67–80.
Mirsadraee M, Boskabady MH, Attaran D. Diagnosis of chronic obstructive pulmonary disease earlier than current Global Initiative for Obstructive Lung Disease guidelines using a feasible spirometry parameter (maximal-mid expiratory flow/forced vital capacity). Chron Respir Dis. 2013;10:191–6.
Hansell DM. Small airways diseases: detection and insights with computed tomography. Eur Respir J. 2001;17:1294–313.
Guder G, Brenner S, Stork S, Hoes A, Rutten FH. Chronic obstructive pulmonary disease in heart failure: accurate diagnosis and treatment. Eur J Heart Fail. 2014;16:1273–82.
Brenner S, Guder G, Berliner D, Deubner N, Frohlich K, Ertl G, et al. Airway obstruction in systolic heart failure–COPD or congestion? Int J Cardiol. 2013;168:1910–6.
Puri S, Dutka DP, Baker BL, Hughes JM, Cleland JG. Acute saline infusion reduces alveolar-capillary membrane conductance and increases airflow obstruction in patients with left ventricular dysfunction. Circulation. 1999;99:1190–6.
Guder G, Rutten FH. Comorbidity of heart failure and chronic obstructive pulmonary disease: more than coincidence. Curr Heart Fail Rep. 2014;11:337–46.
Guder G, Rutten FH, Brenner S, Angermann CE, Berliner D, Ertl G, et al. The impact of heart failure on the classification of COPD severity. J Card Fail. 2012;18:637–44.
Hawkins NM, Petrie MC, Jhund PS, Chalmers GW, Dunn FG, McMurray JJ. Heart failure and chronic obstructive pulmonary disease: diagnostic pitfalls and epidemiology. Eur J Heart Fail. 2009;11:130–9.
Tiller D, Russ M, Greiser KH, Nuding S, Ebelt H, Kluttig A, et al. Prevalence of Symptomatic Heart Failure with Reduced and with Normal Ejection Fraction in an Elderly General Population-The CARLA Study. PLoS One. 2013;8, e59225.
Hogg K, Swedberg K, McMurray J. Heart failure with preserved left ventricular systolic function; epidemiology, clinical characteristics, and prognosis. J Am Coll Cardiol. 2004;43:317–27.
Held M, Mittnacht M, Karl S, Kolb M, Jany B. Pulmonary and Cardiac Function in asymptomatic Obese Subjects and Changes following a Structured weight reduction Program: a Prospective Observational Study. PLoS One. 2014;9(9):e107480.
Lazarus R, Sparrow D, Weiss ST. Effects of obesity and fat distribution on ventilatory function: the normative aging study. Chest. 1997;111:891–8.
Funding
We thank the participating patients, GP, and their assistants, including the general practices connected to the General Practice Network Utrecht (HNU). The original study was supported by a grant (number 904-61-144) from the Netherlands Organization for Scientific Research.
Analysis of this work was further supported by grants from the German Ministry of Education and Research (BMBF), Berlin, Germany [BMBF 01GL0304–Competence Network Heart Failure Germany; BMBF 01GI0205; BMBF 01EO1004–Comprehensive Heart Failure Center Würzburg]. GG was supported by a fellowship grant from the Medical Faculty of the University of Würzburg (Habilitationsstipendium). This publication was funded by the German Research Foundation (DFG) and the University of Würzburg in the funding programme Open Access Publishing.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
GG analysed and interpreted the data and wrote the manuscript. SB, MH, BB and JL contributed significant intellectual content to the manuscript. AH helped to set up and design the study, and was instrumental in grant application, and contributed significant intellectual content to the manuscript. SS supervised data analysis and contributed significant intellectual content to the manuscript. FR designed the study, recruited patients, interpreted the data and wrote the manuscript. All authors read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Güder, G., Brenner, S., Störk, S. et al. Diagnostic and prognostic utility of mid-expiratory flow rate in older community-dwelling persons with respiratory symptoms, but without chronic obstructive pulmonary disease. BMC Pulm Med 15, 83 (2015). https://doi.org/10.1186/s12890-015-0081-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-015-0081-4