Abstract
Background
Preventing childhood obesity is a public health challenge of the twenty-first century and it must be a priority. Governments play a major role in creating and supporting a healthy school environment and should prioritise actions to improve children’s health. Sintra Grows Healthy aims to promote healthy lifestyles to prevent childhood obesity and improve children’s health-related quality of life and social and emotional skills, through the development of a school evidence-based and sustainable model.
Methods
This protocol describes a quasi-experimental design and community-based participatory research. The participants included in the study are the school community of Portuguese public primary schools from the municipality of Sintra. Data will be collected on demographic and socio-economic characterization, nutritional status, eating habits and behaviours, physical activity, sedentary behaviours and sleep, health-related quality of life, and social and emotional skills.
Discussion
There is evidence to support interventions in school settings as strategies for obesity prevention. Up-to-date homogeneous and community-based interventions for preventing childhood obesity are lacking, therefore Sintra Grows Healthy intends to fill this gap. Furthermore, Sintra Grows Healthy aims to contribute with relevant scientific findings that will allow the development of better strategies for policymakers and society to manage this major public health problem.
Similar content being viewed by others
Background
Childhood obesity is one of the most serious global public health challenges of the twenty-first century. In just 40 years the number of schoolchildren and adolescents with obesity has increased more than ten-fold [1]. It is recognised that obesity is a complex system of distinct and interconnecting factors including food consumption and physical activity patterns, genetic factors, environmental structures, cultural values, social inequalities, social class differences, economic factors, social gradients, and stress [2]. Current literature indicates that obesity prevalence is higher amongst adolescent boys [3], particularly those from ethnic minorities [4]. Ethnicity is associated with differences in food habits and behaviours and cultural influences may contribute to higher obesity prevalence among children from minority populations [5]. Also, evidence suggests that children from lower socioeconomic status tend to have poorer dietary habits and lower levels of physical activity [6].
Childhood obesity increases the likelihood of obesity in adulthood and is strongly associated with the development of non-communicable diseases such as cardiovascular disease [7] and diabetes [8]. Preventing obesity has direct benefits for children’s health and wellbeing in childhood and subsequently in adulthood [9]. Also, as reported by the Organisation for Economic Co-operation and Development (OECD), preventing obesity is extremely beneficial for the economic system [10]. In Portugal, the prevalence of obesity and pre-obesity in children under 10 years old is, respectively, 7.7 and 17.3% [11]; 12% of children aged between 6 and 8 years are obese and 29.6% are overweight [12]. In the primary schools of Sintra’s municipality, the prevalence estimates change to 12.6% obese and 23% pre-obesity [13].
The United Nations Convention on the Rights of the Child establishes the children’s rights of protection, education, health, and health care, shelter, and adequate nutrition [14]. Rome Declaration on Nutrition reinforces that collaboration between governments, the private sector, civil society, and communities are crucial for improving nutrition [15]. Therefore, governments play a major role in creating and supporting a healthy environment and should prioritise actions to improve children’s healthy preference learning and to ensure adequate availability of healthy food [16]. Regarding schools, governments should set food standards, and provide healthy eating education, influencing a cultural shift towards healthier food preferences [16]. International guidelines state that municipalities are promising spaces for improving the nutritional status of children and that they must assume a leading role in fighting childhood obesity [17]. In Portugal, the city council is responsible for “support social, cultural, educational, sporting, recreational or other activities of interest to the municipality, including those that contribute to health promotion and disease prevention” [18] including “to participate in programmes to promote public health, community health, and healthy living habits” [19]. Governments can take various actions to create a healthy school environment namely setting physical activity standards [20, 21] and nutritional standards for school meals and minimising the exposure to advertisements of foods and beverages high in fat, sugar and salt [9].
Childhood is one of three sensitive periods of the life-course identified as critical points of intervention that can influence obesity risk in the context of the encompassing obesogenic environment [22]. Schools constitute an important setting for promoting physical, social, cognitive, and mental health and establishing healthy behaviour [23], protect and support good nutrition in children and their families and communities [24, 25]. Tackling nutrition issues in childhood requires coherent action in the school setting, namely through the development of food and nutrition policies [24]. Schools are also considered to be an important context to promote active lifestyles [20, 21]. Regular practice of physical activity can have multiple benefits [26] but most children fail to meet the recommended 60 min of moderate-to-vigorous physical activity daily [27, 28] and present low levels of basic motor competences [29].
Health promotion must have five essential interrelated actions as established by the Ottawa Charter for Health Promotion: building healthy public policy, creating supportive environments, strengthening community action, developing personal skills and reorienting health services [30]. Those concepts must also be applied in nutrition education [31] and health-promoting schools [32]. The health-promoting school (HPS) model has been a notable international health initiative [33]. There is evidence to sustain that this model is effective in improving certain areas of health, namely reducing children’s BMI and increasing children’s physical activity [34,35,36]. An HPS is a school that implements a structured and systematic plan for the health, well-being, and the development of social capital of all pupils and teaching and non-teaching staff [37]. HPS also creates an environment that encourages personal and social development, leading to better health [38].
Comprehensive school-based nutrition programmes involve the school community and address multiple components (curriculum, quality, and quantity of meals served and other actions addressing the school environment, such as vending machines and areas to practise physical activity) [25]. In what concerns the promotion of physical activity, a comprehensive multi-component approach that includes physical education, physical activity during school (e.g., recess), physical activity before and after school (e.g., active travel, school sports intramurals), staff involvement, and family and community engagement has also been recommended and implemented [35]. Interventions at school settings are strategies for obesity prevention [36]. Although childhood obesity may offer many opportunities to intervene, the heterogeneity present in some interventions, set in different contexts across the globe, does not account for a global mechanism for stakeholders to implement [22]. Nevertheless, multifaceted interventions that combine diet and physical activity are particularly associated with a range of positive outcomes, including healthier weight, diet, and levels of physical activity among schoolchildren [9, 36]. Also, diet combined with physical activity interventions may be effective to reduce the risk of obesity in children aged 6 to 12 years [36]. Evidence shows that interventions to improve child nutrition and physical activity are more effective if they involve the whole community (students, teachers, school staff, and parents) [22]. Moreover, it is known that multi-component strategies [36, 37], implemented in collaboration with school community elements over sustained periods [39, 40], and initiated in early age [22] are likely to have the greatest impact. The intensity and duration of the intervention are characteristics that must necessarily be considered when planning it. Extended programmes with frequent interventions seem to be more successful than shorter durations or with time-spaced activities [39, 40]. Additionally, social and emotional skills have established links to mental health and health-related behaviour, affecting physical health [41]. Today’s children will need a balanced set of cognitive, social, and emotional skills to succeed in modern life and to meet the challenges of the twenty-first century [42].
Up-to-date homogenous prevention strategies for childhood overweight and obesity are lacking and more community-environment-based preventive approaches are necessary [43, 44]. Also, future research should focus on intervention sustainability [45] and impact evaluation [46]. In Portugal, impact evaluation of interventions is missing, therefore, it is crucial to provide their effectiveness in behaviour change [46]. Thus, a school-based intervention named Sintra Grows Healthy (SGH) was developed to contribute to a community-environment-based preventive approach. SGH will develop and evaluate the effectiveness of an evidence-based and sustainable school intervention model that could be reproducible in similar contexts. SGH aims to improve children’s health-related quality of life by promoting key dietary and physical activity behaviours and simultaneously enhancing social and emotional skills, preventing the increase of childhood obesity prevalence. Considering that the third United Nations Sustainable Development Goal (good health and well-being) involves a broad range of social determinants covered by the remaining goals [47], SGH also intends to contribute as an integrated response to the 2030 Agenda for Sustainable Development [48].
Therefore, this study protocol aimed to describe the design and methodology of the Sintra Grows Healthy.
Methods
Design
This protocol reports a community intervention with a quasi-experimental design and community-based participatory research. The study was developed by the municipality of Sintra (the project owner) with a partnership between health and academic entities as stakeholders: Sintra Health Centres Group, College of Communication and Media Studies (Polytechnic Institute of Lisbon), Lisbon School of Health Technology (Polytechnic Institute of Lisbon), Nutrition Laboratory of Faculty of Medicine (University of Lisbon), Faculty of Human Kinetics (University of Lisbon). Furthermore, SGH has the institutional support of organisations such as Ministry of Health, Portuguese National Programme for the Promotion of Healthy Eating, Portuguese National Programme for the Promotion of Physical Activity, Ministry of Education, Portuguese Council of Nutritionists, Portuguese Order of Psychologists, Food and Agriculture Organisation of the United Nations (FAO) – Portugal, NOVA National School of Public Health (NOVA University Lisbon) and Food, Farming & Forestry College (F3) (University of Lisbon).
Participants
Sintra is the second Portuguese municipality with the largest number of inhabitants, considering children and young people [49] (62.834 under 15 years old in 2018 [50]), and is characterised by a multicultural population representing 8.7% of the total population of the municipality, more than double the percentage registered in Portugal [49]. Sintra’s School Network includes 20 public school clusters with a total of 96 kindergartens and primary schools. The study includes the respective subgroup of 83 primary schools from the municipality of Sintra (approximately 13,100 children). Firstly, we are recruiting 16 schools and our goal is to reach within 5 years the entire population - the 83 primary schools from the municipality of Sintra. The sample is selected by the schools’ convenience and split into an intervention group and a control group, guaranteeing the sample size required to reach the minimum difference of proportions between groups of 3–5% with at least 80% statistical power. Any children who meet the inclusion criteria (attend the primary schools belonging to the project and give written freely given, enlightened, informed consent for participation with children’s legal guardian approval and signature) and do not meet the exclusion criteria (to have a motor and/or intellectual disabilities and/or not present a valid consent for participation) are eligible (census procedure). As mentioned in the informed consent this study does not represent any risk, cost, or harm to the participants.
Procedure
SGH aims to develop a sustainable model of intervention to promote healthy lifestyles in a school environment and to evaluate its impact. To achieve it, SGH community-based intervention focuses on community actors and prioritises three axes: 1) food and nutrition curricula named Health at the Table, 2) school food environment and 3) physical activity. Throughout the process, a specialised team will design a set of communication tools to inform, engage and motivate all the stakeholders involved in the process, from the institutional partners, to the local community, to children, families, teachers and other actors who play an important role in the school environment. The intervention follow-up will occur during each school year from the first to fourth grade. Also, SGH researchers will assure continuous monitoring and disclosure of a quarterly report for all intervention axes to the schools, to communicate and verify the school community engagement.
Axis 1 – health at the table
This axis is focused on providing children a nutrition curriculum by integrating weekly sessions of food and nutrition education. To achieve a sustainable model those sessions will be developed by the responsible teacher of each class. Also, Health at the Table is a response to a mandatory curriculum component established in Portuguese law, called “the complementary offer” [51]. Complementary offer is considered a new mandatory attendance subject (not covered in the basic curricular matrices) that has its own identity and curriculum documents [51]. Through curricular flexibility and articulation, the complementary offer allows the curriculum to be enriched with the knowledge, skills and attitudes that contribute to achieving the competencies provided in the Profile of Students after Leaving Compulsory Education [52]. To ensure that nutrition education content is properly given to children, SGH developed a 50-h training that all teachers need to attend to be able to lecture those sessions. The training contents are based on scientific evidence related to the topics covered namely i) Food and culture, ii) Food, nutrition, and health, iii) Food and emotions, iv) Food cycle: from the producer to the consumer, v) Safe cooking and vi) Food sustainability. It also includes practical exercises, such as choosing a snack, consulting nutrition labelling, checking the adequacy to children’s energy and nutritional needs or presenting solutions to reduce food waste at school. SGH has also developed a reference manual that provides the contents organised for each schooling level and which also allows connection with the basic curricula subjects (Maths, Science and Portuguese). This manual comprises those six main areas, previously identified by the Portuguese Health Education Reference [53].
This axis will be monitored through a weekly submission in an SGH platform for each food and nutrition education sessions applied by the teachers. In this submission, teachers will fill in a form regarding the application of each session and will answer several questions, (e.g. date of application, improvement opportunities, children’s competencies achieved and activity adequacy).
Axis 2 – school food environment
The municipality of Sintra has already developed several policies to provide children with a healthier school food environment such as assuring the quality of school meals, being all menus established by registered nutritionists/dietitians. In primary schools, a salt control policy has been implemented at school lunches. Moreover, Sintra assures professional ongoing training of cooks, family dinners at schools, and monthly healthy culinary workshops for families.
To continue that work, SGH will implement and monitor a healthy snacks policy. The construction of this policy is developed in a community-based participatory approach, co-designed, and includes different moments explained below.
-
Snacks Diagnosis – Qualitative and quantitative evaluation of foods consumed by children in both morning and afternoon snacks.
-
Snacks Assembly – Within the scope of health at the table, children will organise an assembly to discuss the quality of theirs snacks: what is a healthy snack, which causes lead to the consumption of unhealthy snacks by the class, and what they could implement to improve their snacks. At the end, children build a document, signed by the entire class, with the main conclusions of their debate to be discussed in an assembly with the school community.
-
School Community Assembly – SGH research team will present the snacks diagnosis. Based on the document prepared by the children at the snacks assembly and on Directorate-General for Education guidance for school buffets [54], the school community will afterwards construct a healthy snacks policy. After construction and approval of the healthy snacks policy, it will be incorporated into the school regulation, assuring SGH sustainability.
-
Healthy Snacks Policy Monitoring – To monitor policy compliance a self-regulation map based on the nutritional quality of snacks will be completed by the children daily. Children, supervised by their teachers, will categorise their snacks in a colour system: green (foods to be promoted), yellow (foods to limit) or red (foods not to be available at school) as established by the Directorate-General for Education guidance for school buffets [54].
Axis 3 – physical activity
Physical education is a unique context where all children can have access to quality physical activity experiences guided by a teacher. Physical education has been shown to provide an effective means to promote physical activity inside and outside of school [55]. However, in Portugal, despite being compulsory, physical education often lacks implementation in many primary schools (grades 1 to 4). Some of the main reasons are related to the low perceived status of the subject compared to Language and Mathematics, lack of time and resources, general teacher’s perceived lack of competence to teach physical education, and, lack of continuous and contextualised professional development opportunities [56, 57]. The Directorate-General of Education [51] specified that physical education (and arts education) in primary school should be taught up to 5 h a week and that the collaboration of general teachers with specialist teachers in this field is a possibility. Thus, in this axis, the priority of the intervention was given to provide at least one weekly physical education session (45–60 min) - developed, implemented, and evaluated by the collaborative participation of general and specialist teachers – to children. The contents for physical education classes are the basic motor skills, such as running, jumping, rolling, kicking, grabbing and throwing, gymnastic exercises, and pre-sports games. To ensure SGH sustainability, a previously training (25 h) aimed at general and specialist teachers in the scope of the development of children’s basic motor competences and physical activity was conducted. Children’s basic motor competences (objectively measured) and physical activity levels in different contexts (reported by legal guardian) were measured in the beginning and at the end of the year (pre and post-intervention). Table 1 summarises the information regarding research questions, intervention axes, and expected results and outcomes.
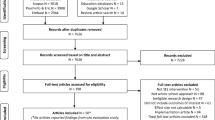
Figure 1 presents the SGH framework of action. This reinforces the importance of community-based participatory research and the crucial role of whole-of-government and whole-of-society to succeed in all intervention axes and achieve the expected results and outcomes.
Data collection
Data collection will be based on structured questionnaires applied to children, children’s legal guardians, teachers, and school staff. The questionnaires evaluate the following dimensions: 1) sociodemographic and health-related data, 2) eating habits and behaviours, 3) movement behaviours: physical activity, sedentary behaviour and sleep 4) health-related quality of life, 5) social and emotional skills and 6) process evaluation. Children’s 7) anthropometric measurements, 8) snacks evaluation, and 9) basic motor competences will be collected by trained researchers to avoid deviations. To ensure that procedures are carried out strictly, teachers will receive specific training regarding the snack’s evaluation.
-
1)
Sociodemographic and Health-Related Data
Child’s data (sex, date of birth, schooling level, previous chronic illnesses or health conditions), number of individuals in the household and children’s legal guardians data (age, nationality, professional status, education, professional activity, weight, height, family income) will be collected.
-
2)
Eating Habits and Behaviours
An instrument will be applied to evaluate the adequacy of Mediterranean dietary patterns in children, reported by children’s legal guardian: KIDMED, a 16-item instrument with an index that ranges from zero to twelve Questions denoting a negative connotation concerning the Mediterranean diet are assigned a value of minusone, and those with a positive aspect plusone. The classification is divided into three levels: ≥8 optimal Mediterranean diet; four to seven, improvement needed to adjust intake to Mediterranean patterns; ≤three very low diet quality [58]. Also, a validated instrument for rapidly assessing the adherence to the Mediterranean dietary patterns in adulthood will be applied to the legal guardian. It is a 14-item scale and the answer to each of the items is scored with one in the case of fulfilling the criteria defined as a characteristic of this pattern or zero if it does not meet. Classification ≥ten is considered to be good adherence [59].
Children food preferences will be collected based on 40 common foods consumed in Portugal, using a 4-item scale (“likes very much”, “neither likes nor dislikes”, “does not like”, “I do not know”) applied to the legal guardian. Children’s involvement in family food choices and food preparation (e.g. how often they helped make family meal choices, how often they helped make family food purchases choices, how often they helped prepare or cook food at home) [60] and basic food skills proposed by age (e.g. measure ingredients, prepare sandwiches and simple snacks, read and follow recipes) [24] will be collected and treated as proxies for children food skills, reported by the legal guardian.
Parents’ food skills will be collected, namely, by meal planning habits, meal preparation practices (e.g. “Are you capable of cooking with leftovers?”), mechanical skills (e.g. cutting, peeling, baking from a recipe), ranked by the respondent on a scale ranging from “very limited” to “very good” [61, 62]. Besides, cooking attitudes will be also collected using a 5-item Likert scale (e.g. “I do not like cooking”, “I pretend to teach my child how to cook”, “My child does not need to know how to cook”).
-
3)
Movement Behaviours: Physical Activity, Sedentary Behaviour, and Sleep
Total physical activity will be assessed by the question “In the last seven days, how many days did your child practised physical activity for at least 60 minutes?”. This is a valid and reliable question assessing physical activity [63] and it has been used in several international and national studies [28, 64]. Participation in organised physical activity (e.g. sports activities guided by a teacher/trainer outside of school), unorganized physical activity (e.g. non-guided activities outside of school) and school sports (e.g. activities systematically conducted in the context of school sport context) will also be collected by the questions “How many times a week does your child take part in… (1) organised physical activity? (2) unorganised physical activity? (3) school sports?”. Active travel to school will be assessed by the question: “How do you usually, travel from home to school?”. The response options will be walking, cycling, by public transportation, by car, and by motorcycle. For each option, the legal guardian will be asked the time of travelling. All these questions are reliable and valid and have been used in several studies [65,66,67]. Questionnaires are important to assess physical activity because they help to understand the context in which it occurs. However, the questionnaires do not allow to determine the intensity of the activity practised regularly. Besides, children also have difficulty reporting the intensity of activities accurately. Therefore, accelerometers are important to understand the levels of intensity of physical activity practised. To determine the physical activity intensity, children will wear an accelerometer for at least two weekdays and one weekend.
Child sedentary behaviours (e.g. time spent watching television, playing console, reading, or listening to music) [68] and sleep behaviours (number of hours of sleep per day at the weekday and the weekend) will be reported by a legal guardian. These questions are reliable and valid and have already been used in the Portuguese context using national representative samples [66, 69] …
-
4)
Health-Related Quality of Life
The child self-report and parent-report versions of the KIDSCREEN-10 will be applied [70, 71]. Based on the definition of quality of life as a multidimensional construct covering five dimensions (physical, emotional, mental, social, and behavioural components of well-being and functioning), contains 10 items. Each item is answered on a 5-point response scale. Higher values indicate a better health-related quality of life. The KIDSCREEN-10 instrument, version for children and adolescents and version for parents, was adapted and validated for the Portuguese language [71].
-
5)
Social and Emotional Skills
An instrument granted by OECD - Study on Social and Emotional Skills (SSES) - will be applied to evaluate self-regulation, resilience, and adaptability. Children’s legal guardians and children will answer the 32-item (e.g. “the child is not easily annoyed” and “I am not easily annoyed.” respectively) self-report questionnaire using a 5-item Likert scale. Children’s questionnaires will be appliedby the teacher in the classroom and instructions will be readaloud. Teachers will answer the 12-item questionnaire (e.g. “The child can control his/her actions.”), using a 5-item Likert scale.
-
6)
Process Evaluation
The process evaluation will be aimed at all school community members. It will be applied both in close and open-ended questions to children’s legal guardians, teachers, and school staff. The close-ended questions, on a Likert scale, will include global project-related questions (e.g. “How important is the SGH in children’s education?”) and specific questions related to each intervention axis (e.g. “How important is the healthy snacks policy at school?”). The adequacy of the questionnaires applied will also be evaluated (e.g. “Were the questions accessible to answer?”). The open-ended question will aim to collect suggestions and improvement opportunities. Children will answer a self-reported questionnaire, using a three-choice scale, namely how much they liked participating in the curricula health at the table, how much theylearnt, and how much their eating habits became healthier.
-
7)
Anthropometric Data
Weight, height, and waist circumference will be measured objectively, according to standardised procedures [72] and classified according to World Health Organization [73]. Children will be wearing minimal clothing and no shoes to assess height and weight. Height will be assessed using a portable stadiometer to the nearest 0.1 cm (SECA 213®) in the vertical position, with feet together and the head in the Frankfort plan [72]. Weight will be assessed through a portable calibrated scale (SECA 813®), expressed up to 0.1 kg. Waist circumference will be directly measured on the skin to the nearest 0.1 cm, according to the method of Cameron, with a non-extensible and flexible tape (SECA 201®).
-
8)
Snacks Evaluations
During the morning and afternoon snacks, a qualitative and quantitative evaluation will be assessed. A qualitative evaluation grid, containing the foods mentioned in the Directorate-General for Education guidance for school buffets [54], will be applied by the responsible teacher in a random moment at the beginning and the end of the school year. At the same moments, trained researchers will conduct a quantitative and qualitative detailed evaluation of children’s snacks. This assessment will be carried out by direct observation, in random classrooms of each leveland recorded in specific registration grids. For the quantitative analysis, snacks’ nutritional composition will be calculated using a database created by SGH accordingly to the reference values established in the Portuguese Food Composition Table [74].
-
9)
Basic Motor Competences
The MOBAK protocol [75] assesses eight basic motor qualifications, assigned to two areas of motor competence: object-movement (object-movement throwing, catching, bouncing, and dribbling) and self-movement (self-movement balancing, rolling, jumping, and moving sideways). Each score ranges between zero and two points, up to a maximum of eight points in each area, and a maximum score of 16 points for the overall score. A total motor competence category was created (maximum of 16 points) [76].
There will be two different data collection moments per year, one at the beginning and another at the end of each school year (SY). Table 2 describes the information collected at each moment.
Data management and statistical analysis
SGH study data will be centralized by the project executive responsible who will hold the participant individuals’ coded key. All individuals involved in the study will be assigned a single anonymised code that will be used to link the respective data across all the existing databases/tables. Each of the performed surveys will have its own database/table with the participant individuals anonymised code.
Regular reporting will be performed using RStudio Notebooks that collect information from the several available databases/tables. This procedure ensures data monitoring, verification, and cleaning. The iterative process of automatic generation of data reporting identifies errors, originated by OCR transposition of paper questionnaires to digital databases/tables, that propel data correction and revision.
The SGH protocol promotes extensive data collection with baseline data points and follow-up points, and with individuals entering and exiting the study during its expected implementation. Overall, this represents a great challenge for the study data management and analysis. For baseline and specific momentary data, statistical characterisation will be performed using descriptive statistics (absolute and relative frequencies for qualitative variables and mean and standard-deviations or median and IQRs for quantitative variables according to verification normality distribution assumption using the Shapiro-Wilk test). Bivariate relations with the main socioeconomic characteristics will be tested using chi-square tests or Fisher exact test (when both variables will be qualitative); Pearson or Spearman’s correlation coefficients (when both variables will be quantitative); and t-, ANOVA or Mann-Whitney and Kruskal-Wallis tests (when one variable will be quantitative and the other qualitative, whether parametric test use will be met or not and according to the discrepancy of sample size between groups). For the comparison of two moments of the same quantitative variable, the paired-samples t-test or the Wilcoxon signed-rank test will be used. For multivariable analyses, the Generalized Linear Models family will be used (it includes Multiple Linear Regression, Multiple Logistic regression, Poisson Regression, and Negative Binomial regression among other models).
Discussion
Even though there has been a trend towards a decrease in children’s overweight national prevalence since 2008, child obesity remains a major public health concern [12]. Although Portugal has recognised obesity as a chronic disease since 2004 [77], obesity stigma contributes to its underestimation and non-recognition as a serious disease, despite its huge consequences [78]. This stigma might compromise the effectiveness of obesity interventions [78]. Up-to-date community-based interventions for preventing childhood obesity are lacking [43]. Evidence regarding interventions to prevent childhood obesity indicates that multi-component approaches [36, 37], whole community approaches [43], sustained over time [39, 40] and sustainable models [45] are more likely to succeed. Several guidelines reinforce the crucial role of whole-of-government, whole-of-society, and health-in-all-policies approaches in taking action on childhood obesity [9, 79, 80]. Thus, SGH aims to contribute with relevant research to obtain evidence-based practices, providing significant knowledge for policymakers and health and education professionals’ actions.
SGH is aware of its limitations such as scarce research funding opportunities, response rates lower than expected due to low socioeconomic status, namely legal guardians’ education level, intrinsic motivation of the community in the study. SGH community-based participatory research protocol, with its study design and methodology, will ensure better community engagement, associated with partnership effectiveness [81], the sustainability and future reproduction of good practices, through the empowerment of the school community, preventing the increase of childhood obesity prevalence, and improving children’s social and emotional skills and health-related quality of life.
Overall, SGH will innovate by its consistent monitoring and scientific evaluation to establish a sustainable and effective intervention model to prevent childhood obesity. Quality control and assurance of procedures through training of researchers, data collection protocols, processes of internal data quality verification will be taken. To support further policy actions, an annual report addressed to policymakers will be developed. Also, there will be strategic thinking about all the issues concerning the institutional communication of the intervention, as well as social behaviour change communication. Furthermore, SGH scientific dissemination of findings will be assured through a shared publication policy with SGH consortium.
It is crucial to reinforce public investment in health, namely through the presence of more health professionals in local governments and schools, prioritsing the measurement of the impact of their interventions, through partnerships with academic researchers. In addition to having evidence-based practices, it is also essential to obtain more evidence based on practices. Implementing this study protocol will bring relevant scientific findings regarding different factors related to childhood obesity, allowing the development of better strategies to manage this major health problem.
Availability of data and materials
Not applicable.
Abbreviations
- HPS:
-
Health promoting school
- SGH:
-
Sintra Grows Healthy
References
Abarca-Gómez L, Abdeen ZA, Hamid ZA, Abu-Rmeileh NM, Acosta-Cazares B, Acuin C, et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390:2627–42. https://doi.org/10.1016/S0140-6736(17)32129-3.
Blundell JE, Baker JL, Boyland E, Blaak E, Charzewska J, de Henauw S, et al. Variations in the prevalence of obesity among European countries, and a consideration of possible causes. Obes Facts. 2017;10:25–37. https://doi.org/10.1159/000455952.
World Health Organization. Adolescent obesity and related behaviours : trends and inequalities in the WHO region 2002-2014; 2017. https://doi.org/10.4103/0972-5229.178178.
Development Initiatives. 2020 global nutrition report: action on equity to end malnutrition. Bristol, UK; 2020. https://doi.org/10.2499/9780896295841.
Manios Y, Costarelli V, Ahrens W. Epidemiology of obesity in children and adolescents. New York, NY: Springer New York; 2011. https://doi.org/10.1007/978-1-4419-6039-9.
Goisis A, Martinson M, Sigle W. When richer doesn’t mean thinner: Ethnicity, socioeconomic position, and the risk of child obesity in the United Kingdom. Demogr Res. 2019;41(September):649–78. https://www.demographic-research.org/volumes/vol41/23/.
Litwin SE. Childhood obesity and adulthood cardiovascular disease. J Am Coll Cardiol. 2014;64:1588–90. https://doi.org/10.1016/j.jacc.2014.07.962.
Reilly JJ, Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int J Obes. 2011;35:891–8. https://doi.org/10.1038/ijo.2010.222.
World Health Organization. Taking Action on Childhood Obesity report. Geneva; 2018. https://www.who.int/end-childhood-obesity/publications/taking-action-childhood-obesity-report/en/. Accessed 11 Apr 2020.
OECD. The heavy burden of obesity. In: OECD health policy studies, editor. Paris: OECD Publishing; 2019. https://doi.org/10.1787/b53ed5f9-fr.
Lopes C, Torres D, Oliveira A, Severo M, Alarcão V, Guiomar S, et al. Inquério Alimentar Nacional e de Atividade Física, IAN-AF 2015–2016: Relatório de resultados: Universidade do Porto; 2017. www.ian-af.up.pt. Accessed 22 Apr 2020.
Instituto Nacional de Saúde Dr. Ricardo Jorge. Childhood Obesity Surveillance Initiative COSI Portugal - 2019. Preliminary data [Internet]. 2019. https://alimentacaosaudavel.dgs.pt/activeapp2020/wp-content/uploads/2020/01/COSI2019_FactSheet.pdf. Accessed 22 Apr 2020.
Ferreira RJ, Marques-Vidal PM. Prevalence and determinants of obesity in children in public schools of Sintra. Portugal Obesity. 2008;16:497–500. https://doi.org/10.1038/oby.2007.74.
UN General Assembly. Universal Declaration of Human Rights. 1948. https://www.refworld.org/docid/3ae6b3712c.html. Accessed 21 Nov 2019.
Food and Agriculture Organisation of the United Nations, World Health Organization. Conference Outcome Document: Rome Declaration on Nutrition. In: Second International Conference on Nutrition. 2014. p. 19–21. https://doi.org/10.1044/leader.PPL.19102014.18.
Hawkes C, Smith TG, Jewell J, Wardle J, Hammond RA, Friel S, et al. Smart food policies for obesity prevention. Lancet. 2015;385:2410–21. https://doi.org/10.1016/S0140-6736(14)61745-1.
World Health Organization/Regional Office for Europe. Vienna Declaration on Nutrition and Noncommunicable Diseases in the Context of Health 2020. In: WHO European ministerial conference on nutrition and noncommunicable diseases in the context of health 2020. Vienna; 2013. p. 5. https://doi.org/10.1136/bmj.f4417.
Assembleia da República. Lei n.o 75/2013. Diário da República no 176. 2013;:5688–724. https://dre.pt/application/conteudo/500023.
Assembleia da República. Lei n.o 50/2018. Diário da República no 157. 2018;:4102–8. https://dre.pt/application/conteudo/500023.
UNESCO. Quality physical education: guidelines for policy-makers. Paris, France: United Nations Educational, Scientific and Cultural Organization. United Nations Educational, Scientific and Cultural Organization; 2015.
Expert Group on Health-enhancing physical activity Recommendations. Recommendations to encourage physical education in schools, including motor skills in early childhood, and to create valuable interactions with the sport sector, local authorities and the private sector. 2015. https://www4.dcu.ie/shhp/downloads/CSPPA.pdf. Accessed 20 May 2020.
World Health Organization. Consideration of the evidence on childhood obesity for the Commission on Ending Childhood Obesity: report of the ad hoc working group on science and evidence for ending childhood obesity, Geneva, Switzerland. Geneva, Switzerland.: World Health Organization; 2016. https://apps.who.int/iris/handle/10665/206549.
World Health Organization. Promoting intersectoral and interagency action for health and well-being in the WHO European Region: working together for better health and well-being. Paris, France; 2017. http://www.euro.who.int/en/media-centre/events/events/2016/12/paris-high-level-conference/documentation/promoting-intersectoral-and-interagency-action-for-health-and-well-being-in-the-who-european-region-working-together-for-better-health-and-well-being-2. Accessed 28 Apr 2020.
World Health Organization Regional Office for Europe. Food and nutrition policy for schools: A Tool for the Development of School Nutrition Programmes in the European Region. WHO Regional Office for Europe. Copenhagen; 2006. http://www.euro.who.int/pubrequest. Accessed 28 Apr 2020.
World Health Organization. Global nutrition policy review 2016–2017: country progress in creating enabling policy environments for promoting healthy diets and nutrition. Geneve: World Health Organization; 2018. https://www.who.int/publications-detail/9789241514873.
Warburton DER, Bredin SSD. Health benefits of physical activity. Curr Opin Cardiol. 2017;32:541–56. https://doi.org/10.1097/HCO.0000000000000437.
World Health Organization. Global recommendations on physical activity for health. Geneva; 2010.
Guthold R, Stevens GA, Riley LM, Bull FC. Global trends in insufficient physical activity among adolescents: a pooled analysis of 298 population-based surveys with 1·6 million participants. Lancet Child Adolesc Heal. 2020;4:23–35.
Barnett LM, Lai SK, Veldman SLC, Hardy LL, Cliff DP, Morgan PJ, et al. Correlates of gross motor competence in children and adolescents: a systematic review and meta-analysis. Sports Med. 2016;46:1663–88.
World Health Organization. Ottawa Charter for Health Promotion: First International Conference on Health Promotion. Ottawa; 1986. https://www.healthpromotion.org.au/images/ottawa_charter_hp.pdf.
Food and Agriculture Organization of the United Nations. Nutrition education in primary schools. Food and Agriculture Organization of the United Nations; 2006. http://www.fao.org/3/a-a0333e.pdf. Accessed 22 Apr 2020.
Buijs GJ. Better schools through health: networking for health promoting schools in Europe. Eur J Educ. 2009;44:507–20. https://doi.org/10.1111/j.1465-3435.2009.01410.x.
Clift S, Jensen BB. The health promoting school : international advances in theory, evaluation and practice. 1st edition. Copenhagen: European Network of Health Promoting Schools by Danish University of Education Press The; 2005. www.dpu.dk/forlag. Accessed 28 Apr 2020.
Langford R, Bonell CP, Jones HE, Pouliou T, Murphy SM, Waters E, et al. The WHO health promoting school framework for improving the health and well-being of students and their academic achievement. Cochrane Database Syst Rev. 2014;2014. https://doi.org/10.1002/14651858.CD008958.pub2.
Centers for Disease Control and Prevention. Comprehensive School Physical Activity Programs: A Guide for Schools. GA: U.S. Department of Health and Human Services; 2013. http://www.shapeamerica.org/cspap/index.cfm. Accessed 20 May 2020.
Brown T, Moore TH, Hooper L, Gao Y, Zayegh A, Ijaz S, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2019. https://doi.org/10.1002/14651858.CD001871.pub4.
Schools for Health in Europe. Better Schools Through Health: the Third European Conference on Health Promoting Schools. Vilnius, Lithuania; 2009. https://www.schoolsforhealth.org/resources/conference-statements/vilnius-resolution. Accessed 29 Apr 2020.
World Health Organization. First Conference of the European Network of Health Promoting Schools “The Health Promoting School-an investment in education, health and democracy.” Thessaloniki-Halkidiki, Greece; 1997. https://apps.who.int/iris/handle/10665/107850. Accessed 28 Apr 2020.
Guerra PH, da Silveira JAC, Salvador EP. Physical activity and nutrition education at the school environment aimed at preventing childhood obesity: evidence from systematic reviews. J Pediatr (Rio J). 2016;92:15–23.
World Health Organization. Population-based approaches to childhood obesity prevention. Geneva, Switzerland: World Health Organization; 2012.
OECD. Skills for social Progress: the power of social and emotional skills. Paris: OECD; 2015.
OECD. Social and Emotional Skills Well-being, connectedness and success. 2015.
Weihrauch-Blüher S, Kromeyer-Hauschild K, Graf C, Widhalm K, Korsten-Reck U, Jödicke B, et al. Current guidelines for obesity prevention in childhood and adolescence. Obes Facts. 2018;11:263–76. https://doi.org/10.1159/000486512.
Khambalia AZ, Dickinson S, Hardy LL, Gill T, Baur LA. A synthesis of existing systematic reviews and meta-analyses of school-based behavioural interventions for controlling and preventing obesity. Obes Rev. 2012;13:214–33. https://doi.org/10.1111/j.1467-789X.2011.00947.x.
Pearson M, Chilton R, Wyatt K, Abraham C, Ford T, Woods H, et al. Implementing health promotion programmes in schools: a realist systematic review of research and experience in the United Kingdom. Implement Sci. 2015;10:149. https://doi.org/10.1186/s13012-015-0338-6.
Filipe J, Godinho CA, Graça P. Intervenções comportamentais de prevenção da obesidade infantil: Estado da arte em portugal. Psychol Community Heal. 2016;5:170–84. https://doi.org/10.5964/pch.v5i2.175.
Borowy I. Sustainable health: the need for new developmental models. Bull World Health Organ. 2014;92:699. https://doi.org/10.2471/BLT.14.145219.
United Nations. Transforming Our World: The 2030 Agenda for Sustainable Development 2015.
Instituto Nacional de Estatística. Censos 2011 Resultados Definitivos - Região Lisboa. Lisboa; 2012. https://censos.ine.pt/ngt_server/attachfileu.jsp?look_parentBoui=148313382&att_display=n&att_download=y. Accessed 29 Apr 2020.
PORDATA - População residente: total e por grandes grupos etários. https://www.pordata.pt/Municipios/População+residente+total+e+por+grandes+grupos+etários-390. Accessed 27 May 2020.
Assembleia da República. Lei n.o 55/2018. Diário da República no 129. 2018;:29228–2943. https://dre.pt/home/-/dre/115652962/details/maximized. Accessed 11 Apr 2020.
Martins G d’Oliveira, Gomes CAS, Brocardo J, Pedroso JV, Camilo JLA, Silva LMU, et al. Perfil dos alunos à saída da Escolaridade Obrigatória. 2017.
A. Carvalho; C. Matos; C. Minderico C de A et. al. Referencial de Educação para a Saúde. 2017. http://www.dgidc.min-edu.pt/index.php?s=noticias¬icia=443. Accessed 16 Mar 2019.
Direção - Geral da Educação. Bufetes Escolares Circular n.o 11/DG1DC/2007. 2007;:28. https://www.dge.mec.pt/sites/default/files/Esaude/orientacoes_bufetes_final.pdf.
Chen S, Kim Y, Gao Z. The contributing role of physical education in youth’s daily physical activity and sedentary behavior. BMC Public Health. 2014;14:110. https://doi.org/10.1186/1471-2458-14-110.
Lander N, Eather N, Morgan PJ, Salmon J, Barnett LM. Characteristics of teacher training in school-based physical education interventions to improve fundamental movement skills and/or physical activity: a systematic review. Sport Med. 2017;47:135–61.
Morgan PJ, Hansen V. Classroom teachers’ perceptions of the impact of barriers to teaching physical education on the quality of physical education programs. Res Q Exerc Sport. 2008;79:506–16.
Serra-Majem L, Ribas L, Ngo J, Ortega RM, García A, Pérez-Rodrigo C, et al. Food, youth and the Mediterranean diet in Spain. Development of KIDMED, Mediterranean diet quality index in children and adolescents. Public Health Nutr. 2004;7:931–5. https://doi.org/10.1079/PHN2004556.
Martínez-González MA, García-Arellano A, Toledo E, Salas-Salvadó J, Buil-Cosiales P, Corella D, et al. A 14-item Mediterranean diet assessment tool and obesity indexes among high-risk subjects: the PREDIMED trial. PLoS One. 2012;7:e43134. https://doi.org/10.1371/journal.pone.0043134.
Blanchet R, Loewen OK, Godrich SL, Willows N, Veugelers P. Exploring the association between food insecurity and food skills among school-aged children. Public Health Nutr. 2020.
Slater JJ, Mudryj AN. Self-Perceived Eating Habits and Food Skills of Canadians. J Nutr Educ Behav [Internet]. 2016;48(7):486–95.e1. https://linkinghub.elsevier.com/retrieve/pii/S1499404616305164.
Slater J, Mudryj AN. Nurturing Future Generations: Household Food Practices of Canadian Children and Family Meal Participation. Can J Diet Pract Res [Internet]. 2016;77(3):113–8. https://dcjournal.ca/doi/10.3148/cjdpr-2015-050.
Prochaska JJ, Sallis JF, Long B. A physical activity screening measure for use with adolescents in primary care. Arch Pediatr Adolesc Med. 2001;155:554–9.
Martins J, Marques A, Loureiro N, Da Costa FC, Diniz J, De Matos MG. Trends and age-related changes of physical activity among Portuguese adolescent girls from 2002-2014: highlights from the health behavior in school-aged children study. J Phys Act Health. 2019;16:281–7.
Ledent M, Cloes M, Telama R, Almond L, Diniz J, Piéron M. Participation des jeunes Européens aux activités physiques et sportives. Sport. 1997;159/160:61–71.
Matos MG de, Equipa Aventura Social. A saúde dos adolescentes portugueses: Relatório do estudo HBSC 2010. 2012. www.researcherid.com/rid/H-3824-2012. Accessed 20 May 2020.
Carreiro da Costa F, Marques A. Promoting Active and Healthy Lifestyles at School: Views of Students, Teachers, and Parents in Portugal; 2011.
Marshall SJ, Biddle SJH, Sallis JF, McKenzie TL, Conway TL. Clustering of sedentary behaviors and physical activity among youth: a cross-national study. Pediatr Exerc Sci. 2002;14:401–17.
Lopes C, Torres D, Oliveira A, Severo M, Alarcão V, Guiomar S, et al. Inquérito Alimentar Nacional e de Atividade Física IAN-AF, 2015-2016: Relatório metodológico. Vol. 112, U. Porto. Universidade do Porto; 2017.
Ravens-Sieberer U, Herdman M, Devine J, Otto C, Bullinger M, Rose M, et al. The European KIDSCREEN approach to measure quality of life and well-being in children: development, current application, and future advances. Qual Life Res. 2014;23:791–803. https://doi.org/10.1007/s11136-013-0428-3.
Gaspar T, Gaspar de Matos M. Qualidade de vida em crianças e adolescentes: versão portuguesa dos instrumentos kidscreen-52. 2008. www.aventurasocial.com. Accessed 29 Apr 2020.
Rito A, Breda JCI. Guia de Avaliação do Estado Nutricional Infantil e Juvenil. Lisboa: Ministério da Saúde; 2011.
World Health Organization - Department of Nutrition for Health and Development. WHO Child Growth Standards Length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age Methods and development Department of Nutrition for Health and Development. 2006. https://www.who.int/childgrowth/standards/Technical_report.pdf%0A; http://www.who.int/childgrowth/standards/Technical_report.pdf?ua=1.
Instituto Nacional de Saúde Dr. Ricardo Jorge (INSA). Tabela da Composição de Alimentos. 2016. http://www2.insa.pt/sites/INSA/Portugues/AreasCientificas/AlimentNutricao/AplicacoesOnline/TabelaAlimentos/Paginas/TabelaAlimentos.aspx.
Herrmann C, Gerlach E, Seelig H. Development and validation of a test instrument for the assessment of basic motor competencies in primary school. Meas Phys Educ Exerc Sci. 2015;19:80–90.
Quitério A, Martins J, Onofre M, Gerlach E, Scheur C, Herrmann C. MOBAK 1 assessment in primary physical education : exploring basic motor competences of Portuguese 6-year-olds; 2018.
Direção-Geral da Saúde. A Obesidade como doença crónica - Circular Normativa no 03/DGCG de 17/03/2005. 2005;:1–2. https://www.dgs.pt/directrizes-da-dgs/normas-e-circulares-normativas/circular-normativa-n-03dgcg-de-17032005-pdf.aspx. Accessed 30 Apr 2020.
Phelan SM, Burgess DJ, Yeazel MW, Hellerstedt WL, Griffin JM, van Ryn M. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes Rev. 2015;16:319–26. https://doi.org/10.1111/obr.12266.
World Health Organization Regional Office for Europe. European Food and Nutrition Action Plan 2015-2020. 2015. http://www.euro.who.int/pubrequest. Accessed 29 Apr 2019.
European Union. EU action plan on childhood obesity 2014–2020. 2014. http://www.who.int/dietphysicalactivity/childhood_consequences/en. Accessed 5 Apr 2020.
Oetzel JG, Wallerstein N, Duran B, Sanchez-Youngman S, Nguyen T, Woo K, et al. Impact of participatory Health Research: a test of the community-based participatory research conceptual model. Biomed Res Int. 2018;2018:1–12. https://doi.org/10.1155/2018/7281405.
Acknowledgments
Not applicable.
Funding
This research is funded by the Municipality of Sintra and co-funded by Gulbenkian Academies for Knowledge, Calouste Gulbenkian Foundation. The Sintra Grows Healthy is promoted by the Municipality of Sintra. The Gulbenkian Academies for Knowledge, Calouste Gulbenkian Foundation, supports the Municipality of Sintra assigning a subsidy in order to promote social and emotional skills but played no role in the study design. The Municipality of Sintra provides financial support to Faculty of Medicine, University of Lisbon, for this institution to undertake the technical and scientific leadership, including the study design validation, development and dissemination of Sintra Grows Healthy, in its various actions.
Author information
Authors and Affiliations
Contributions
RJF, TN, JS, RB, AR, JM, MO, AM, AR, AQ and AP contributed to the initial study design protocol and the final research protocol. RJF and TN coordinate the study implementation, fieldwork, data collection and methodological and operational adjustments. JM coordinates the physical activity axis. PN and AMP coordinate statistical analyses plan and database management. AR coordinates the institutional communication. TN coordinates the impact evaluation of the study. JS coordinates scientific supervision. VDS and MP drafted and critically revised the manuscript. All authors contributed to further discussion and critically revised the manuscript. All authors read and approved the final manuscript.
Authors’ information
Not applicable.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study is conducted according to the guidelines laid down in the Declaration of Helsinki and it is obtained written informed consent from the children’s legal guardian. Lisbon Academic Medical Centre ethics committee (401/17), the National Data Protection Commission (11468/2017) and the Ethics Boards of each participating school approved the study. Permission from the relevant rights holders of each questionnaire applied was obtained.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ferreira, R.J., Nogueira, T., Dias da Silva, V. et al. A school-based intervention for a better future: study protocol of Sintra Grows Healthy. BMC Public Health 20, 1615 (2020). https://doi.org/10.1186/s12889-020-09715-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-020-09715-0