Abstract
Background
Number of opiate users worldwide has doubled over the past decade, but not all of them are diagnosed with opioid use disorder. We aimed to identify the prevalence and risk factors for OUD after ten years of follow-up.
Methods
Among 8,500 chronic opiate users at Golestan Cohort Study baseline (2004–2008), we recalled a random sample of 451 subjects in 2017. We used three questionnaires: a questionnaire about current opiate use including type and route of use, the drug use disorder section of the Composite International Diagnostic Interview lifetime version, and the validated Kessler10 questionnaire. We defined opioid use disorder and its severity based on the DSM-5 criteria and used a cutoff of 12 on Kessler10 questionnaire to define psychological distress.
Results
Mean age was 61.2 ± 6.6 years (84.7% males) and 58% were diagnosed with opioid use disorder. Starting opiate use at an early age and living in underprivileged conditions were risk factors of opioid use disorder. Individuals with opioid use disorder were twice likely to have psychological distress (OR = 2.25; 95%CI: 1.44–3.52) than the users without it. In multivariate regression, former and current opiate dose and oral use of opiates were independently associated with opioid use disorder. Each ten gram per week increase in opiate dose during the study period almost tripled the odds of opioid use disorder (OR = 3.18; 95%CI: 1.79–5.63).
Conclusions
Chronic opiate use led to clinical opioid use disorder in more than half of the users, and this disorder was associated with psychological distress, increasing its physical and mental burden in high-risk groups.
Similar content being viewed by others
Introduction
The United Nations Office on Drugs and Crime (UNODC) reported that the number of opiate users has doubled over the past decade [1]. In 2019, 61.6 million people used opioids worldwide, of whom 30.8 million used minimally-processed products (i.e. opiates such as heroin and opium), with the remainder using synthetic or semi-synthetic preparations [1]. Although all opiate users are at risk of adverse health conditions, not all of them fulfil the criteria for dependence or abuse, and they should be evaluated individually with clinical criteria for opioid use disorder (OUD) [2]. Between 1990 and 2016, the prevalence of OUD increased by 47·3%, making it the most common drug use disorder in the world [3]. History of opioid-related poisoning, the opioid dose used, polysubstance use, a diagnosis of psychiatric disorders, and the influences of the social environment are currently known risk factors for opioid use disorder [4,5,6]. However, diagnosing psychiatric disorders is not feasible in a large scale study of the general population [7, 8]. For these reasons, information on risk factors of OUD and patterns of long-term use in the general population is relatively scarce.
Consumption of minimally-processed opium is a known carcinogen [9] and is associated with an increased overall risk of cancer [10] cardiovascular diseases [11], and mortality [12]. Afghanistan produces more than 80% of the total illicit opium in the world [13], and UNODC has predicted a rise in illicit cultivation in Afghanistan due to the economic crisis following the COVID pandemic [1]. Iran is a transit route for trafficking opium and its derivatives from Afghanistan to the rest of the world and accounts for 42% of worldwide consumption of opium [14]. Opium consumption in Iran dates back thousands of years and opium abuse surged in this country in the late 15th century [15]. Long-term use of opium and its derivatives are still common in Iran [16], and it is sometimes regarded as a “soft drug” due to its widespread use [17]. The 2011 Iranian Mental Health Survey showed an OUD prevalence of 2.23% in the 15- to 64-year-old population [18]. This is while the global age-standardized rate of opioid dependence was 0.51% (510 per 100,000 people) in the year 2017 [19].
The current study used baseline and follow-up data from the Golestan Cohort Study (GCS), accrued from the population of Golestan Province in northeastern Iran. GCS started in January 2004, in the context of an international collaboration, initially intending to identify risk factors for upper gastrointestinal cancers due to the high incidence of esophageal cancer in this area, as detailed before [20]. Among more than 50,000 participants, 8487 (17%) reported long-term use of opium at baseline based on a validated structured questionnaire [12]. In 2017, we used the GCS infrastructure to recall a group of these individuals. This nested study is the first longitudinal study aiming to determine the prevalence and potential risk factors of OUD including demographics, habitual history, psychological distress, and opiate use characteristics in long-term opium users after ten years of follow-up.
Materials and methods
Participants
Informed consent was obtained from all participants. All procedures were performed in compliance with relevant laws and institutional guidelines and that the National Institutes of Health (NIH) IRB has approved this study (protocol number: 07CN120). The GCS originally recruited 50,045 individuals, aged 40–75, from the general population of Golestan Province in northeastern Iran between 2004 and 2008. In the GCS, individuals were randomly selected through systematic clustering based on household numbers and invited by telephone contact. Details of the GCS have been published before [20]. In 2017, about 13 years after GCS baseline enrolment, we administered a repeat comprehensive opiate and tobacco use questionnaire, along with validated psychological tools detailed below, to investigate the psychological correlates of long-term opiate use. We invited a random sample of 500 participants who reported chronic opium use at baseline, stratified by sex and tobacco use history. To select this random sample, we complied the list of all participants who were alive and reported opiate use at baseline and categorizing them into 4 strata defined by current tobacco use and sex. Since these two factors are important determinants of opiate use, from each stratum we selected a number of individuals proportional to their prevalence among all GCS participants, to ensure representativeness. Data from 451 subjects who accepted to participate were analyzed for the present study. This was more than the required sample size of 385 calculated based on a type 1 error of 0.05, a 50% prevalence of OUD among users and a 5% error margin.
Measurements
The baseline information was derived from demographic and lifestyle data collected by trained interviewers in the GCS. The lifestyle questionnaire included questions about substance and tobacco use. The questionnaire included history of substance use over a person’s life, dates of starting and stopping, types of drugs used, routes, and self-reported doses of opiate use in grams. In this province, the main substance of abuse is opium which is used in two forms: teriak (raw opium) and shireh (a refined product extracted by boiling opium pipe residue in water, with or without adding teriak), which are taken by oral or smoking routes. The quantity measure for opium use has been previously shown to be valid against urinary codeine and morphine with 93% sensitivity and 89% specificity [21]. History of any lifetime alcohol use was also obtained from all participants. Alcohol consumption is relatively uncommon in this population (ever use less than 5%), and most ever users have had a limited number of drinks for a short period of time. There were no current alcohol drinkers in our study sample, and we defined the consumption of 1 drink or more per week at any period during a person’s life as a history of ever alcohol use.
We used three different questionnaires in this study: [1] a detailed questionnaire asking about current opiate type, dose and route, [2] to define OUD we used the validated L section of the Farsi translation Composite International Diagnostic Interview (CIDI 2.1-lifetime version) [22, 23], and [3] the validated Farsi version of the Kessler 10 (K10) questionnaire [7, 8] to define psychological distress. The questionnaires were administered by two trained interviewers after a workshop and a pilot phase supervised by two investigators who were involved in the development and validation of the Farsi version of the substance use and K10 questionnaires [24].
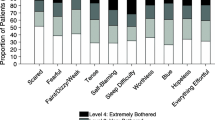
We defined lifetime OUD based on the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), which is based on having at least two of the following eleven criteria: hazardous use, social or interpersonal problems related to use, neglected significant roles due to use, withdrawal, tolerance, use of more significant amounts, repeated attempts to quit or control use, much time spent using, physical or psychological problems related to use, activities given up using the drug, and craving. The severity of OUD was further classified into mild (2–3 criteria), moderate (4–5 criteria), and severe (6 or more criteria).
Psychological distress was measured by a standard K10 questionnaire. The K10 questionnaire includes 10 questions to screen for mental distress. It is a simple screening tool which is not used for making a diagnosis. Each response in the K10 questionnaire was rated on a 5-point Likert scale from 0 as “never” to 4 as “always”, with the total K10 scores ranging from 0 to 40. Based on the population and purpose of the study, different cutoffs have been proposed. We used a cutoff of 12 to define mild to severe psychological distress based on the K10 score validated for Iranian population, which has an area under the curve of 0.92 for detecting severe mental illness, with a sensitivity of 86% and a specificity of 83% [25,26,27,28].
Statistical analysis
Opiate dose, frequency, type and route were analyzed at two time periods: “prior use” was reported on the baseline questionnaire administered in 2004–2008 (depending on the exact enrolment date), and “current use” was based on the new questionnaire administered in 2017. The doses were reported using a local using called “nokhod” which is almost equal to 0.2 grams [29]. For each time period (prior and current), we used the last reported daily use and number of days a person used during the week to calculate grams per week and categorized prior and current doses into quartiles. We also calculated dose change between the baseline interview and 2017, which were separated by 10–13 years. We. We also categorized the change of route of use into 4 groups: continued smoking, continued oral use, switch from smoking to oral use, and change from oral use to smoking. In 38 and 40 participants, dose and route change could not be calculated, respectively, due to missing data at either period. Age, sex, marital status, place of residence, education, BMI, and socioeconomic Status (SES) were extracted from the baseline questionnaire [30].
The descriptive statistics are presented as raw numbers, percentages, mean, and standard deviation or median and interquartile range whichever was appropriate. Univariate analysis of factors associated with OUD was done using Chi-square test for categorical variables and t-test for continuous variables. We used univariate ordered logistic regression to analyze the trends of these variables across categories of OUD severity (from mild to severe).
We investigated the independent role of opiate use patterns on OUD and OUD severity as the outcomes of interest, adjusted for potential confounders, using three different models: one for prior use, another for current use, and the third for the change between the two time periods. The models with OUD as an outcome of interest were examined through multivariate logistic regression (present/absent). In the models with OUD severity as an outcome we excluded those without an OUD diagnosis and used ordered logistic regression since the outcome had three levels (mild/moderate/severe). The odds ratio in ordered logistic regression reflects the odds of a one-step increase in the three levels of severity associated with the independent variables (opiate use pattern). All models were adjusted for age, age of starting opiate use, sex, place of residence (rural/urban), socioeconomic status (quartiles) and psychological distress K10 score. Stata statistical software, version 17 (StataCorp, College Station, TX) was used to perform analyses, and a p-value less than 0.05 was considered statistically significant.
Results
Among 451 subjects (mean age 61.2 ± 6.6 years, 84.7% males), all used raw (teriak) or refined opium (shireh), and 261 (57.9%) were diagnosed as having opioid use disorder (OUD) in their lifetime based on DSM-5 criteria. Among opiate users with and without OUD, the most common DSM-5 criteria were withdrawal symptoms (94.3% and 48.4%, respectively), repeated attempts to quit or control use (73.5% and 49.5%, respectively), and craving (57.1% and 15.8%, respectively). OUD was mild in 144 (55.7%) of the individuals with OUD, moderate in 71 (27.2%) and severe in 46 (17.6%). As expected, the frequency of all criteria increased in people with more severe OUD. The details of DSM-5 criteria by OUD diagnosis and its severity are presented in Table 1.
Individuals with OUD were significantly younger (60.6 ± SD vs. 62.1 ± SD years old) than those without OUD, were more likely to live in rural area, had lower socioeconomic status, lower BMI, and higher psychological distress (Table 2). There were no statistically significant differences in sex, marital status, education, cigarette use, and history of ever alcohol use between the two groups. However, cigarette smoking, in addition to younger age and higher education and psychological distress were significantly associated with OUD severity (Supplementary Table 1). The K10 scale for psychological distress was positive in 31.7% of the study participants. Individuals with OUD had higher scores of psychological distress, and were more likely to have a score of equal to or above the cut-off of 12 (p < 0.01). In subjects with OUD, the odds of positive K10 scores were more than two times the odds in those without it (OR = 2.25; 95%CI: 1.44–3.52, p < 0.001). Similar, but stronger associations were found among individuals with severe OUD. These associations changed slightly after adjustment for current and prior opiate dose and route and their changes between these periods (Supplementary Table 2).
Table 3 compares the patterns of opiate use between those with and without OUD and by OUD severity. Individuals with OUD started opiate use at an earlier age (35.1 ± 12.4 vs. 38.8 ± 12.6 years). As OUD severity increased, the start age decreased to 30.2 (SD = 10.0) in severe cases. Prior and current opiate doses were both significantly associated with the presence and severity of OUD (Table 3). Among individuals whose dose change during the follow-up could be calculated, 228 (55.2%) increased their dose, 66 (16.0%) and 107 (25.9%) reported unchanged and decreasing opiate doses, respectively, and 12 (2.9%) quit using opiates. As a result, average weekly dose increased from 3.6 ± 3.9 g at baseline to 4.6 ± 4.3 g. Individuals with OUD were more likely to have increased their opiate dose compared to those without OUD (59.8% vs. 48.8%, respectively) and reported a significantly higher average increase in dose (mean increase: 1.7 vs. 0.13 g per week, p < 0.01). Individuals with OUD were more likely to consume opium orally, both currently and more than 10 years prior, however the change in route was not associated with OUD severity. There were no significant differences between the types of current and prior opiates used by those with and without OUD.
Table 4 presents the results of multivariate models assessing the associations between current and prior opiate use patterns and OUD presence and severity, adjusted for age, opiate start age, sex, place of residence, socioeconomic status, and K10 score. Prior opiate dose was independently associated with the presence of OUD and OUD severity (p for trend < 0.05), however current opiate dose was associated with OUD presence and not its severity. Each ten grams per week increase in opiate dose during the study period almost tripled the odds of OUD presence (OR = 3.18; 95%CI: 1.79–5.63) without a significant effect on OUD severity. The odds of OUD and severe OUD increased up to three times in people who currently used opiates by both oral and smoking routes, i.e. dual use (OR = 2.96; 95%CI: 1.11–7.92, and OR = 2.65; 95%CI: 1.07–6.54, respectively). Prior route of use did not significantly predict OUD and its severity. Individuals who previously used oral opiates and still had the same habit at the time of follow-up had the highest odds of OUD (OR = 2.97; 95%CI:1.55–5.71) compared to subjects who continued smoking opiates. The change from smoking to oral route had the second highest odds ratios for OUD (OR = 1.87; 95%CI: 1.10–3.17). The change in route was not associated with OUD severity.
Discussion
More than half (57.9%) of the people who had used opiates for a long time in our study were diagnosed with an opiate use disorder. Opiate users with an OUD diagnosis were relatively younger than those without OUD and had started using at an earlier age. Other factors associated with OUD included living in rural areas, having low socioeconomic status and having a lower BMI. Younger and more educated opiate users, and those who smoked cigarettes, were more likely to have severe OUD. Individuals with OUD had higher psychological distress scores compared with opiate users without such diagnosis. Patterns of opiate use were also different between individuals with and without OUD: opiate users with OUD used higher doses and were more likely to increase their dose during the follow-up, and OUD diagnosis was more common in those using opiates orally instead of smoking.
Our study confirms that the widespread consumption of opiates has led to OUD and is a major health problem in this population. In the U.S., the prevalence of OUD has been estimated at around 0.7% in people aged 25 years and above [31], and in the Netherlands, the prevalence of opioid use disorder other than heroin was reported 0.0056% [32, 33]. The results of the 2011 Iranian Mental Health Survey which showed a prevalence of 3.02% for opiate use in the past year, and 2.23% for OUD [18]. We believe that the overall rate of OUD in our study population is higher than these estimates, as we studied lifetime prevalence which is naturally higher compared with the past year definition used in the survey. Also the prevalence of opiate use in Iran follows a geographic pattern and the provinces in the south and northeast (where our study was conducted) have higher rates compared to other regions of the country. Finally, we investigated people between 40 and 75 years, while the 2011 national study was conducted on 15 to 64 years group, and lifetime prevalence of OUD increases overtime.
In Iran, opium is sometimes considered a “soft drug” due to its widespread use, but the fact that almost three out of five long-term opium users were clinically diagnosed as having an OUD is in contrast with this notion. OUD is associated with poor mental health and a number of important psychological comorbidities. Opiate use increases the risk of mood disorders, suicide attempts, and violent behavior [34,35,36]. Other substance uses and severe mental disorders are commonly associated with OUD [37]. Mood and anxiety disorders may precede the substance use and may even be the cause of abuse, making the diagnosis and treatment even more complex [34, 38]. People with psychological comorbidities are more prone to seek a substance to resolve their undesirable psychological symptoms [39]. Our study did not include an assessment of these mental comorbidities, but we screened for psychological distress using a validated questionnaire. K10 were first developed to screen for more recent non-specific symptoms of serious mental disorders, i.e. anxiety disorders, mood disorders, and psychotic disorders [25, 40]. People with higher psychological distress are more likely to seek outpatient mental health care, be under psychological treatment in the future, and have higher mortality [26, 27]. Nearly 32% of opiate users in this study had psychological distress, and individuals with OUD were twice more likely to have psychological distress after adjusting for opiate use patterns. In a study from Nepal, half of all kinds of substance users in drug rehabilitation centers had psychological distress [41]. Similar findings have also been reported for cannabis and nonmedical use of prescription opioids [42, 43]. Our cross-sectional analysis would not allow us to conclude a causal relationship, since it is not clear if the psychological distress preceded the OUD diagnosis or occurred because of it. However, the high prevalence of this comorbidity underlines the importance of appropriate psychosocial support for opiate users, especially those with OUD.
Opium consumption is a known carcinogen [9], and recent studies have found that it can increase the risk of premature mortality from different causes [12, 44,45,46]. These risks increase with the dose and duration of use, putting users with OUD at an even greater risk. Opium users have also been shown to be exposed to very high levels of lead, probably as a result of opium adulterations to increase weight. Lead exposure among users is dose-dependent and is seen mainly among those who used opium orally [47]. Lead is a probable carcinogen and a risk factor for cardiovascular diseases, and users with OUD are more likely to have high blood lead levels due to their longer and higher use. Moreover, in our study people with OUD were more likely to take opium orally in both periods and keep their habit of eating opiates. Oral consumption is easier than inhalation, and enables the heavy user to consume opiates regardless of time and location. These hazards are aggravated by the fact that the most common OUD symptoms in our population of opiate users were withdrawal symptoms and repeated (failed) attempts to quit or control use, meaning that a large proportion of these long-term users will continue using for a long time, maybe for the rest of their lives.
Certain groups of opiate users were at increased risk of developing OUD in our study. Opiate users with OUD were on average younger than those without it, because they may live shorter, and had started using at an earlier age. In the U.S., National Epidemiologic Study on Alcohol and Related Conditions reported similar finding and suggested implementing programs to prevent the initiation of opioid use with an emphasis on younger age groups [48]. A comparative study on three cohorts of Millennials (1979-96), Generation X (1964-79), and Baby Boomers (1949-64) reported higher odds of nonmedical prescription opioid use and use disorder in Millennials [49, 50]. Younger individuals become dependent to a substance faster than the older age groups [51]. Besides, coping with social and psychological challenges is one of the proposed reasons for the higher frequency of OUD among younger age groups [52]. Prioritizing younger and long-time users for opiate use treatment consultations can slow the upward trend of opiate use disorder in the future.
We showed that rural users and those in lower SES levels were more likely to have OUD than urban users with higher SES scores. Our finding on socioeconomic status was in line with the Iranian household Mental Health survey, in which subjects with higher SES were at lower risk of opioid dependence than those at lower levels [17]. Also, the U.S. National Epidemiologic Study on Alcohol and Related Conditions reported incomes at or above 40,000 U.S. dollars as a protective factor for OUD [48]. Opium is inexpensive, which makes it affordable for people with low income even in rural areas.
Limitations
We studied a sizeable number of opiate users and evaluated clinical OUD by DSM-5 criteria in a non-clinical setting using a validated questionnaire. The availability of detailed data on the lifetime pattern of opiate use and other lifestyle variables in the context of a prospective cohort study is another strength of this study. Comparing these data in the baseline and after more than 10 years of follow-up enabled us to investigate the impact of changes in opiate use on OUD. However, the OUD questionnaire was only available at the follow-up visit, and we had not assessed OUD at the baseline, which is the main limitation of our study. Assessment of psychological distress was also done at the follow-up. Another limitation of this study was insufficient information on other comorbidities such as depression and anxiety for further adjustment. However, we used Kessler score for evaluating psychologic distress and found it quite useful in a study of a high-risk group. Also, we were not able to investigate some previously proposed OUD risk factors like personal and psychological traits due to lack of data.
Conclusions
In conclusion, we found that more than half of the subjects with a history of long-term opiate use had OUD, which means that it is probably one of the most common mental disorders in this population. In addition to the known long-term health hazards, we showed that OUD was associated with psychological distress. Identifying groups at high risk of OUD, such as those who start using at an earlier age, live in underprivileged conditions, and use higher doses and increase their dose is important in planning appropriate prevention strategies to lower the physical and mental burden of OUD.
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
World Drug. Report 2021 (United Nations publication, Sales No. E.21.XI.8).
Degenhardt L, Grebely J, Stone J, Hickman M, Vickerman P, Marshall BDL, et al. Global patterns of opioid use and dependence: harms to populations, interventions, and future action. Lancet Lond Engl. 2019;394(10208):1560–79.
GBD 2016 Alcohol and Drug Use Collaborators. The global burden of Disease attributable to alcohol and drug use in 195 countries and territories, 1990–2016: a systematic analysis for the global burden of Disease Study 2016. Lancet Psychiatry. 2018;5(12):987–1012.
Liu YS, Kiyang L, Hayward J, Zhang Y, Metes D, Wang M et al. Individualized prospective prediction of opioid Use Disorder. Can J Psychiatry Rev Can Psychiatr. 2022;7067437221114094.
Cragg A, Hau JP, Woo SA, Kitchen SA, Liu C, Doyle-Waters MM, et al. Risk factors for misuse of prescribed opioids: a systematic review and Meta-analysis. Ann Emerg Med. 2019;74(5):634–46.
Webster LR. Risk factors for opioid-use disorder and Overdose. Anesth Analg. 2017;125(5):1741–8.
Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, et al. Screening for serious mental Illness in the general population. Arch Gen Psychiatry. 2003;60(2):184–9.
Hajebi A, Motevalian A, Amin-Esmaeili M, Rahimi-Movaghar A, Sharifi V, Hoseini L, et al. Adaptation and validation of short scales for assessment of psychological distress in Iran: the persian K10 and K6. Int J Methods Psychiatr Res. 2018;27(3):e1726.
IARC Monographs Vol 126 group. Carcinogenicity of opium consumption. Lancet Oncol. 2020;21(11):1407–8.
Mansouri M, Naghshi S, Parsaeian M, Sepanlou G, Poustchi S, Momayez Sanat H. Opium Use and Cancer Risk: a comprehensive systematic review and Meta-analysis of Observational studies. Int J Clin Pract. 2022;2022:5397449.
Nakhaee S, Ghasemi S, Karimzadeh K, Zamani N, Alinejad-Mofrad S, Mehrpour O. The effects of opium on the cardiovascular system: a review of side effects, uses, and potential mechanisms. Subst Abuse Treat Prev Policy. 2020;15(1):30.
Khademi H, Malekzadeh R, Pourshams A, Jafari E, Salahi R, Semnani S, et al. Opium use and mortality in Golestan Cohort Study: prospective cohort study of 50,000 adults in Iran. BMJ. 2012;344:e2502.
United Nations Office on Drugs and Crime. World drug report 2020. Vienna: United Nations., 2020. https://wdr.unodc.org/wdr2020/field/WDR20_Booklet_3.pdf (accessed Oct 6, 2020).
Rahimi-Movaghar A, Gholami J, Amato L, Hoseinie L, Yousefi-Nooraie R, Amin-Esmaeili M. Pharmacological therapies for management of opium withdrawal. Cochrane Database Syst Rev. 2018;6:CD007522.
Raeis Dana F. The Drug Market in Iran. Soc Welf Q. 2003;3(9):243–62.
Noorbala AA, Saljoughian A, Bagheri Yazdi SA, Faghihzadeh E, Farahzadi MH, Kamali K, et al. Evaluation of drug and alcohol abuse in people aged 15 years and older in Iran. Iran J Public Health. 2020;49(10):1940–6.
Amin-Esmaeili M, Rahimi-Movaghar A, Sharifi V, Hajebi A, Radgoodarzi R, Mojtabai R, et al. Epidemiology of illicit Drug Use Disorders in Iran: prevalence, correlates, comorbidity and service utilization results from the Iranian Mental Health Survey. Addict Abingdon Engl. 2016;111(10):1836–47.
Amin-Esmaeili M, Rahimi-Movaghar A, Sharifi V, Hajebi A, Radgoodarzi R, Mojtabai R, et al. Epidemiology of illicit Drug Use Disorders in Iran: prevalence, correlates, comorbidity and service utilization results from the Iranian Mental Health Survey. Addiction. 2016;111(10):1836–47.
Degenhardt L, Grebely J, Stone J, Hickman M, Vickerman P, Marshall BDL, et al. Global patterns of opioid use and dependence: harms to populations, interventions, and future action. The Lancet. 2019;394(10208):1560–79.
Pourshams A, Khademi H, Malekshah AF, Islami F, Nouraei M, Sadjadi AR, et al. Cohort Profile: the Golestan Cohort Study–a prospective study of oesophageal cancer in northern Iran. Int J Epidemiol. 2010;39(1):52–9.
Abnet CC, Saadatian-Elahi M, Pourshams A, Boffetta P, Feizzadeh A, Brennan P, et al. Reliability and validity of opiate use self-report in a population at high risk for Esophageal cancer in Golestan, Iran. Cancer Epidemiol Biomark Prev Publ Am Assoc Cancer Res Cosponsored Am Soc Prev Oncol. 2004;13(6):1068–70.
Arabgol F, Alaghband Rad J, Sharifi V, Hakim-shoushtari M, Shabani A, Davari-Ashtiani R et al. Reliability of a persian translation of the Composite International Diagnostic interview (CIDI), section for substance use disorders: in a multi-center study in Iran. Adv Cogn Sci. 2005;7.
Wittchen HU. Reliability and validity studies of the WHO–Composite International Diagnostic interview (CIDI): a critical review. J Psychiatr Res. 1994;28(1):57–84.
Hajebi A, Motevalian A, Amin-Esmaeili M, Rahimi‐Movaghar A, Sharifi V, Hoseini L et al. Adaptation and validation of short scales for assessment of psychological distress in Iran: The Persian K10 and K6. Int J Methods Psychiatr Res [Internet]. 2018 Sep [cited 2023 Jan 11];27(3). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6877187/.
Kessler RC, Green JG, Gruber MJ, Sampson NA, Bromet E, Cuitan M, et al. Screening for serious mental Illness in the general population with the K6 screening scale: results from the WHO World Mental Health (WMH) survey initiative. Int J Methods Psychiatr Res. 2010;19(Suppl 1):4–22.
La P. Serious psychological distress, as measured by the K6, and mortality. Ann Epidemiol [Internet]. 2009 Mar [cited 2022 Jun 14];19(3). Available from: https://pubmed.ncbi.nlm.nih.gov/19217003/.
Olfson M, Wang S, Wall M, Marcus SC, Blanco C. Trends in Serious Psychological Distress and Outpatient Mental Health Care of US adults. JAMA Psychiatry. 2019;76(2):152–61.
Sampasa-Kanyinga H, Zamorski MA, Colman I. The psychometric properties of the 10-item Kessler Psychological Distress Scale (K10) in Canadian military personnel. PLoS ONE. 2018;13(4):e0196562.
Mohebbi E, Kamangar F, Rahimi-Movaghar A, Haghdoost AA, Etemadi A, Amirzadeh S, et al. An Exploratory Study of Units of Reporting Opium Usein Iran: implications for epidemiologic studies. Arch Iran Med. 2019;22(10):541–5.
Islami F, Kamangar F, Nasrollahzadeh D, Aghcheli K, Sotoudeh M, Abedi-Ardekani B, et al. Socio-economic status and oesophageal cancer: results from a population-based case–control study in a high-risk area. Int J Epidemiol. 2009;38(4):978–88.
(2019). Key substance use and mental health indicators in the United States: Results from the 2018 National Survey on Drug Use and Health (HHS Publication No. PEP19-5068, NSDUH Substance Abuse and Mental Health Services Administration, Series H-. 54). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Retrieved from https://www.samhsa.gov/data/.
Kalkman GA, Kramers C, van Dongen RT, van den Brink W, Schellekens A. Trends in use and misuse of opioids in the Netherlands: a retrospective, multi-source database study. Lancet Public Health. 2019;4(10):e498–505.
W H, Dp EB, E FGD. F, T H, Is Europe also facing an opioid crisis?-A survey of European Pain Federation chapters. Eur J Pain Lond Engl [Internet]. 2021 Sep [cited 2022 Nov 2];25(8). Available from: https://pubmed.ncbi.nlm.nih.gov/33960569/.
Rahimi-Movaghar A, Amin-Esmaeili M, Sharifi V, Hajebi A, Radgoodarzi R, Hefazi M, et al. Iranian mental health survey: design and field proced. Iran J Psychiatry. 2014;9(2):96–109.
Najafipour H, Masoumi M, Amirzadeh R, Rostamzadeh F, Foad R, Shadkam Farrokhi M. Trends in the prevalence and Incidence of Opium Abuse and its association with coronary artery risk factors in Adult Population in Iran: findings from Kerman coronary artery Disease risk factors study. Iran J Med Sci. 2022;47(4):328–37.
Najafipour H, Banivaheb G, Sabahi A, Naderi N, Nasirian M, Mirzazadeh A. Prevalence of anxiety and depression symptoms and their relationship with other coronary artery Disease risk factors: a population-based study on 5900 residents in Southeast Iran. Asian J Psychiatry. 2016;20:55–60.
Jones CM, McCance-Katz EF. Co-occurring substance use and mental disorders among adults with opioid use disorder. Drug Alcohol Depend. 2019;197:78–82.
Lai HMX, Cleary M, Sitharthan T, Hunt GE. Prevalence of comorbid substance use, anxiety and mood disorders in epidemiological surveys, 1990–2014: a systematic review and meta-analysis. Drug Alcohol Depend. 2015;154:1–13.
Jané-Llopis E, Matytsina I. Mental health and alcohol, Drugs and Tobacco: a review of the comorbidity between mental disorders and the use of alcohol, Tobacco and illicit Drugs. Drug Alcohol Rev. 2006;25(6):515–36.
Kessler RC, Ustün TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic interview (CIDI). Int J Methods Psychiatr Res. 2004;13(2):93–121.
Gyawali B, Choulagai BP, Paneru DP, Ahmad M, Leppin A, Kallestrup P. Prevalence and correlates of psychological distress symptoms among patients with substance use disorders in drug rehabilitation centers in urban Nepal: a cross-sectional study. BMC Psychiatry. 2016;16(1):314.
Chan K, Moller M, Marsack-Topolewski C, Winston P, Jennings R, Prifti A. Age differences in non-medical prescription opioid use and psychological distress. Subst Use Misuse. 2020;55(11):1808–16.
Danielsson AK, Lundin A, Allebeck P, Agardh E. Cannabis use and psychological distress: an 8-year prospective population-based study among Swedish men and women. Addict Behav. 2016;59:18–23.
Nalini M, Shakeri R, Poustchi H, Pourshams A, Etemadi A, Islami F, et al. Long-term opiate use and risk of cardiovascular mortality: results from the Golestan Cohort Study. Eur J Prev Cardiol. 2021;28(1):98–106.
Rahmati A, Shakeri R, Khademi H, Poutschi H, Pourshams A, Etemadi A, et al. Mortality from Respiratory Diseases associated with opium use: a population-based cohort study. Thorax. 2017;72(11):1028–34.
Malekzadeh MM, Khademi H, Pourshams A, Etemadi A, Poustchi H, Bagheri M, et al. Opium Use and Risk of Mortality from Digestive Diseases: a prospective cohort study. Off J Am Coll Gastroenterol ACG. 2013;108(11):1757–65.
Etemadi A, Hariri S, Hassanian-moghaddam H, Poustchi H, Roshandel G, Shayanrad A, et al. Lead Poisoning among asymptomatic individuals with a long-term history of opiate use in Golestan Cohort Study. Int J Drug Policy. 2022;104:103695.
Schepis TS, Hakes JK. Age of initiation, psychopathology, and other substance use are associated with time to use disorder diagnosis in persons using opioids nonmedically. Subst Abuse. 2017;38(4):407–13.
Wall M, Cheslack-Postava K, Hu MC, Feng T, Griesler P, Kandel DB. Nonmedical prescription opioids and pathways of drug involvement in the US: generational differences. Drug Alcohol Depend. 2018;182:103–11.
Han B, Compton WM, Jones CM, Cai R. Nonmedical prescription opioid Use and Use disorders among adults aged 18 through 64 years in the United States, 2003–2013. JAMA. 2015;314(14):1468–78.
Alvanzo AAH, Storr CL, La Flair L, Green KM, Wagner FA, Crum RM. Race/ethnicity and sex differences in progression from drinking initiation to the development of alcohol dependence. Drug Alcohol Depend. 2011;118(2–3):375–82.
World Drug Report. 2018 (United Nations publication, Sales No. E.18.XI.9).
Acknowledgements
Not applicable.
Funding
Open Access funding provided by the National Institutes of Health (NIH). This work was supported by Tehran University of Medical Sciences [grant No: 81/15]; Cancer Research UK [grant No: C20/A5860]; the Intramural Research Program of the NCI, National Institutes of Health; and various collaborative research agreements with IARC.
Open Access funding provided by the National Institutes of Health (NIH)
Author information
Authors and Affiliations
Contributions
All authors are responsible for this reported research. R.Malekzadeh, and M. Amin-Esmaeili conceptualized the study. V. Sharifithe study, A. Rahimi-Movaghar, A.Etemadi, and F. Kamangar designed the study. S.Alvand, and G. Roshandel4 conducted the statistical analyses. H.Poustchi, and Y. Sadeghi, S. M. Dawsey, N. D. Freedman, C. C. Abnet visualized and validated the data. S. Alvand drafted the original manuscript. All authors critically reviewed and revised the manuscript. The authors approved the final manuscript as submitted.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Informed consent was obtained from all participants. All procedures were performed in compliance with relevant laws and institutional guidelines and that the National Institutes of Health (NIH) IRB has approved this study (number: IRB07CN120) and was conducted in accordance with the Declaration of Helsinki – Ethical Principles for Medical Research Involving Humans Subjects.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Alvand, S., Amin-Esmaeili, M., Poustchi, H. et al. Prevalence and determinants of opioid use disorder among long-term opiate users in Golestan Cohort Study. BMC Psychiatry 23, 958 (2023). https://doi.org/10.1186/s12888-023-05436-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-023-05436-x