Abstract
Background
Generally, the loss rate of human endothelial cells (HCEC) in routine cataract surgery is 8.5%. When the corneal endothelial cells density (ECD) drops, the HCEC may decompensate to keep cornea dehydration which leads to corneal edema. Granulomatosis with polyangiitis (GPA) is an uncommon autoimmune disease involving multiple organs including eyes such as conjunctivitis, scleritis, uveitis, and corneal ulcer. In this study, we report two cases of GPA whose corneal ECD decreased significantly after phacoemulsification cataract surgery.
Case presentation
In the first case of 69-year-old male with GPA, the ECD dropped 39.6% (OD) four months after phacoemulsification and 38.1% (OS) six months postoperatively respectively. At the final follow-up, the residual ECD was only 55% in the right eye in the 49th month, and 56% remained in the left eye in the 39th month. In the second case of 54-year old female, left ECD dropped 63.9% at the 4th month after surgery and 69.6% ECD remained at the 15th month postoperatively while similar ECD of right eye before and after left eye surgery.
Conclusion
Extensive preoperative ophthalmic evaluation and meticulous postoperative inflammation control should be applied to prevent severe loss of HCEC in GPA patients.
Similar content being viewed by others
Background
Granulomatosis with polyangiitis (GPA) is a systematic autoimmune disease with prevalence of 0.003% in America [1, 2], with 50–60% patients presenting with ocular manifestation lifetime [3]. The suspected etiology is activated dendritic cells that present autoantigen and prime type 1 T helper cells inducing macrophage migration, maturation and causing granuloma and tissue destruction. Chronic T cells activation promotes B cells secretion of antineutrophil cytoplasmic antibodies (ANCAs) targeting proteinase 3 (PR3) or myeloperoxidase (MPO) which trigger neutrophil activation and lead to vasculitis [4]. The clinical manifestations include flu-like symptoms, hearing loss, otitis media, bloody rhinorrhea, sinusitis, pulmonary disease, renal, cutaneous, neurologic problems and also conjunctivitis, scleritis, corneal ulceration, or uveitis [5, 6]. Importantly, most patients with GPA and ocular comorbidity are visually or systemically impaired [3].
Physiologically, the corneal endothelium consists of a monolayer of human corneal endothelial cells (HCEC), which remain contact-inhibited or non-proliferative, and endothelial cell density (ECD) diminishes gradually since birth until death [7]. The average ECD is around 2500 cells/mm2 in older adults [8]. When the ECD falls below 400–700 cells/mm2, the HCEC fail to pump the water out the cornea which ends up with corneal edema [9]. Pathologically, the loss rate of HCEC in routine cataract surgery is 8.5% [10], while that in patients with low ECD ranges from 5.1% to 12.1% [11, 12]. By contrast in the diabetic population, phacoemulsification-induced HCEC loss ranges from 6.2% up to 29.7% [13].
Here, we report a 69-year-old man with GPA suffering from significantly declined ECD up to 45% after phacoemulsification in the following-up of 49 months. Additionally, we report a 54-year-old woman with GPA suffering from declined ECD to 36.1% four months after cataract surgery, whose ECD recovered to 69.6% of the original level with ascorbate drops for 11 months.
Case presentation
Case 1
A 69-year-old Taiwanese Han male with GPA presented to our ophthalmologic clinic with redness, foreign body sensation, and pain in the right eye for two months. Before this episode, multiple sinusectomy was done for chronic aspergillus rhinosinusitis three months ago.
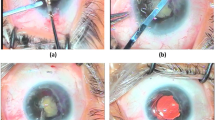
Ophthalmologic examination revealed visual acuity of 20/250 (OD) and 20/100 (OS), with bilateral congestion and an arcuate corneal ulceration between the 9 and 12 o’clock positions, as well as a 5-mm superior conjunctival ulceration in the right eye (Fig. 1a and b). Prednisolone (1%) eye drops and lubricant were prescribed to ameliorate impending perforation of the corneal ulcer, resulting in reduced reaction in the anterior chamber. Oral methylprednisolone 16 mg/day was also given initially to decrease the disease activity to facilitate subsequent conjunctival biopsy, which only showed necrosis and acute inflammation, but failed to show multinucleated giant cells, granuloma, or microangiopathy.
Serial external eye photography of Patient 1 before and after diagnosis of granulomatosis with polyangiitis (GPA). a. Initial presentation of superior nasal conjunctiva congestion (OD) with a 5-mm superior conjunctival ulceration and a 9 to 12 o’clock peripheral ulcerative keratitis was noted with visual acuity (VA) was 0.09. The insert shows fluorescein staining of some tiny epithelial defects and diffuse superficial punctate staining of the cornea. b. Initial presentation of superior conjunctival congestion and limbo-corneal neovascularization (OS) was noted with VA of 0.1. The insert shows fluorescein staining of mild superficial punctate staining of the cornea. c.d. Six months after initial presentation (i.e. 4 months after right eye cataract surgery), resolution in conjunctiva congestion (OU), peripheral ulcerative keratopathy (OD) and limbo-corneal neovascularization (OS) was noted with VA of 0.6 (OD) and 0.2 (OS) respectively
Hydroxychloroquine 400 mg was also added for 2 months under the suggestion of a rheumatologist, which was later shifted to prednisone 10 mg/day. One month later, visual acuity recovered to 20/60 (OU), and the PUK resolved. Free from further ocular symptoms and signs for one-year under the control of prednisolone 10 mg/day and methotrexate 7.5 mg/week, visual acuity decreased to finger counting (OD), which was caused by cataract after screening. In addition to grade 3 nuclear sclerosis and cortical opacity, dense posterior subcapsular cataract was also noticed probably due to long-term corticosteroid use. To prevent possible autoimmune-related corneal complications from intraocular surgery, we kept topical prednisolone acetate 1% and artificial tears in addition to planned medical treatment. Blood tests for immune activity were also relatively low before cataract surgery. No perioperative complication, increasing intraocular pressure nor postoperative inflammation were noted. The anterior chamber was deep and clear after surgery. There was mild arcuate neovascularization around the phacoemulsification wound and gradually subsided (Fig. 1c and d).
His visual acuity improved to 20/30 (OD). Ten months after right eye cataract surgery, his left eye visual acuity became 0.01 due to nuclear sclerosis and cortical opacification. The VA (OS) improved to 20/25 after cataract surgery. As right cataract surgery, no perioperative complication, increasing IOP nor postoperative inflammation were noted. The anterior chamber was deep and clear while slight arcuate neovascularization around the phacoemulsification wound was noted for few weeks.
The cataract surgeries (OU) were performed by an experienced surgeon (Chen HC) using standard techniques [14, 15]. Total ultrasound (US) power and time was 28.1 mJ and 94 s for the right eye, and 24.5 mJ and 76 s for the left eye using continuous and torsional energy power setting named Ozil with Alcon Laboratory #9056 Micro Tip Kelman 45 Degree phaco tip. The wound size was 2.65 mm. Preoperatively, ECD (OD = 2638 cells/mm2, OS = 2695 cells/mm2) was within normal range (Fig. 2a and b). After the right cataract surgery, the ECD dropped 39.6% in the 4th month (Fig. 2c) and recovered to only 29.9% cell loss in the 7th month (Fig. 2d), while the left ECD was still around its baseline. After the left cataract surgery, we found the ECD decreased to similar level of his right eye (Fig. 2e), approximately 44% loss binocularly in the 39 months following up (Fig. 2h).
Serial imaging of the corneal endothelium before and after cataract surgery in the right eye (a-d) and after cataract surgery in the left eye (e–h) of Patient 1. Specular microscopy showed changes in endothelial cell density (ECD), coefficient of variation (CV), percentage of hexagonal cells (HEX), and central corneal thickness (CCT) at the following time points. a. Fourteen months prior to cataract surgery (OD). b. Two weeks prior to cataract surgery (OD). c. Four months after cataract surgery (OD). d. Seven months after cataract surgery (OD). e. Six weeks after cataract surgery (OS), i.e. 12 months after cataract surgery (OD). f. 6 months after cataract surgery (OS), i.e. Seventeen months after cataract surgery (OD). g. Fourteen months after cataract surgery (OS), i.e. 25 months after cataract surgery (OD) h. Thirty-nine months after cataract surgery (OS), i.e. 49 months after cataract surgery (OD)
Case 2
A 54-year-old Taiwanese Han female with hypertension under medications control for 20 years and GPA with steroid and Imuran control for 3 years presented progressively blurred vision (OS) for several years.
Ophthalmologic examination revealed visual acuity of 20/28.5 (OD) and 20/200 (OS) without remarkable abnormalities in the anterior and posterior segments, except for grade 1 nuclear cataract assessed by the Lens Opacities Classification System III (LOCS III). Ten months later, her nuclear cataract became grade 2 and phacoemulsification and intraocular lens (OS) was performed in another 6 months later. The patient’s anterior chamber was shallow and clear before and after surgery. No obvious postoperative inflammation nor increasing IOP was noted compared with her baseline condition.
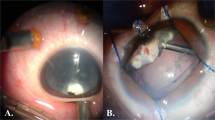
The cataract surgery was performed by an experienced surgeon (Chen HC). Total US power and time was 15.05 mJ and 50.2 s with the same facility and model in case 1. Tobramycin 0.3% + dexamethasone 0.1% suspension and oral mefenamic acid 1 g were prescribed for prophylactic use and pain control. Her ECD was 2645 cells/mm2 (OD) and 3067 cells/mm2 (OS) 1 month before left cataract surgery which was in normal range (Fig. 3a). Her ECD became 2659 cells/mm2 (OD) and 1041 cells/mm2 (OS) which was only 34.0% remained at the 1st month after surgery (OS) (Fig. 3b) and following ECD were 2772, 2902, 2909, 2876 cells/mm2 (OD) and 1108, 1155, 1891, 2134 cells/mm2 (OS) at the 4th, 7th, 9th and 15th month (Fig. 3d-f).
Serial imaging of the corneal endothelium before and after cataract surgery in the left eye (a-f) of Patient 2. Specular microscopy showed changes in endothelial cell density (ECD), coefficient of variation (CV), percentage of hexagonal cells (HEX), and central corneal thickness (CCT) at the following time points.a. One month prior to cataract surgery (OS). b. One month after cataract surgery (OS). c. Four months after cataract surgery (OS). d. Seven months after cataract surgery (OS), i.e. 3 months after topical use of ascorbic acid (OS). e. Nine months after cataract surgery (OS), i.e. 5 months after topical use of ascorbic acid (OS). f. Fifteen months after cataract surgery (OS), i.e.11 months after topical use of ascorbic acid (OS)
We tried to find possible strategy to rescue the loss HCEC and studies showed ascorbic acid might help [16]. Topical ascorbic acid (10 mg/mL, qid) was administered since 4th month after surgery for her left eye. At the last follow-up at the 15th month, ECD totally lost 30.4% with visual acuity of 20/25(OD) and 20/100 (OS) and unremarkable ocular examination results which rescued 32.0% of ECD loss than that in the 4th month.
Discussion and conclusions
Previously known as Wegener's granulomatosis, GPA is an ANCA-associated autoimmune disease involving multi-organ damage and is fatal without treatment. In this report, the patients had most classic manifestations of GPA and gradually developed to hypertension, and even cataract due to long-term use of steroid. Besides, PUK was also presented concurrently in one patient [17].
For a patient with GPA, long-term use of corticosteroid may accelerate the formation of posterior subcapsular cataract, with several theories [18]. Thorough systemic review, close follow-up, and control of local inflammation are mandatory before intraocular surgery because autoimmune-related corneal melting can occur spontaneously or after cataract extraction [19, 20]. There is also research aiming to discover specific antibodies in patients with autoimmune diseases that are responsible for corneal melting [21]. When the auto antibodies bind to specific corneal antigen forming immune complex, the classical pathway of complement was activated. Inflammatory cells are driven to peripheral cornea and produce cytokines inducing stromal keratocytes to release matrix metalloproteinases which subsequently dissolve the cornea [22,23,24].
In this case, we observed an abnormal pattern of corneal endothelial cell loss after cataract surgery, even though that one patient had concomitant diabetes under stable metformin therapy and a long-term serum HbA1c level of 6.0 to 6.5%. In addition, his inflammatory status was relatively stable based on preoperative examinations of serum C reactive protein (CRP) quantity and erythrocyte sedimentation rate (ESR) which were controlled around 10 mg/L and 25 mm/hour one month after the right cataract surgery.
Though this is only a case report, the patient’s binocular ECD decreased approximately 40% four months postoperatively and ended up around 44% in the forty months follow-up and another patient’s ECD decline 38.3% nine months after surgery which was apparently higher than that of 1.4% to 18.4% in non-diabetic and 6.2% to 29.7% in diabetic patients three months postoperatively shown in a meta-analysis study [13]. We speculate that the patient’s corneal endothelial cells were more susceptible to intraocular surgery than those in the normal population and even the diabetic patients owing to underlining GPA. In other word, the marked ECD decline was less likely related to autoimmune reaction aroused by cataract surgery per se since there was no severe postoperative local inflammation and no significant ECD decline in the left eye after the right cataract surgery. Also, no right eye ECD decreased in the second patient after left cataract surgery for 15 months. In the second case, tropical ascorbate sodium was given since the 4th month after phacoemulsification which showed gradually increasing ECD to the last follow up at the 15th month. Perioperative topical ascorbic acid (AA) has been shown preventive effects of corneal endothelial dysfunction in high-risk patients undergoing phacoemulsification [16]. AA has shown promoting proliferation effects in other human cells [25, 26]. In vitro evidence also shed light on the proliferative effects of AA on corneal endothelial cells [27]. Besides, there is clinical evidence of protective effect of AA on HCEC recently [16].
We have illustrated two rare cases of an old-aged male patient with GPA and PUK and a middle-aged female with GPA undergoing uneventful phacoemulsification but with marked loss of corneal endothelial cells. In the long-term follow-up, ECD decline was even more the that in the general population and diabetic group [13]. Collectively, we advocate extensive preoperative ophthalmic evaluation and meticulous postoperative inflammatory control to prevent severe corneal endothelial cell loss in such patients.
Availability of data and materials
All data generated during this case report are included in this published article.
Abbreviations
- AA:
-
Ascorbic acid
- ANCAs:
-
Antineutrophil cytoplasmic antibodies
- CRP:
-
C reactive protein
- ECD:
-
Endothelial cells density
- ESR:
-
Erythrocyte sedimentation rate
- GPA:
-
Granulomatosis with polyangiitis
- HCEC:
-
Human corneal endothelial cells
- MPO:
-
Myeloperoxidase
- PR3:
-
Proteinase 3
References
Pakalniskis MG, Berg AD, Policeni BA, Gentry LR, Sato Y, Moritani T, et al. The Many Faces of Granulomatosis With Polyangiitis: A Review of the Head and Neck Imaging Manifestations. Am J Roentgenol. 2015;205(6):W619–29.
Galor A, Thorne JE. Scleritis and peripheral ulcerative keratitis. Rheum Dis Clin N Am. 2007;33(4):835–vii.
Pakrou N, Selva D, Leibovitch I. Wegener’s Granulomatosis: Ophthalmic Manifestations and Management. Semin Arthritis Rheum. 2006;35(5):284–92.
Bosch X, Guilabert A, Espinosa G, Mirapeix E. Treatment of Antineutrophil Cytoplasmic Antibody-Associated VasculitisA Systematic Review. JAMA. 2007;298(6):655–69.
Jayne D. The diagnosis of vasculitis. Best Pract Res Cl Rh. 2009;23(3):445–53.
Harper SL, Letko E, Samson CM, Zafirakis P, Sangwan V, Nguyen Q, et al. Wegener’s granulomatosis: the relationship between ocular and systemic disease. J Rheumatol. 2001;28(5):1025.
Bourne WM. Biology of the corneal endothelium in health and disease. Eye. 2003;17:912.
Müller A, Craig JP, Grupcheva CN, McGhee CNJ. The effects of corneal parameters on the assessment of endothelial cell density in the elderly eye. Br J Ophthalmol. 2004;88(3):325–30.
Mishima S. Clinical Investigations on the Corneal Endothelium. Ophthalmology. 1982;89(6):525–30.
Walkow T, Anders N, Klebe S. Endothelial cell loss after phacoemulsification: relation to preoperative and intraoperative parameters. J Cataract Refract Surg. 2000;26(5):727–32.
Hayashi K, Yoshida M. Manabe S-i, Hirata A: Cataract surgery in eyes with low corneal endothelial cell density. J Cataract Refract Surg. 2011;37(8):1419–25.
Yamazoe K, Yamaguchi T, Hotta K, Satake Y, Konomi K, Den S, et al. Outcomes of cataract surgery in eyes with a low corneal endothelial cell density. J Cataract Refract Surg. 2011;37(12):2130–6.
Tang Y, Chen X, Zhang X, Tang Q, Liu S, Yao K. Clinical evaluation of corneal changes after phacoemulsification in diabetic and non-diabetic cataract patients, a systematic review and meta-analysis. Sci Rep. 2017;7(1):14128.
Su W-W. Chen PY-F, Hsiao C-H, Chen HS-L: Primary phacoemulsification and intraocular lens implantation for acute primary angle-closure. PLoS ONE. 2011;6(5):e20056–e20056.
Ho Y-J, Sun C-C, Chen H-C. Cataract surgery in patients with corneal opacities. BMC Ophthalmol. 2018;18(1):106–106.
Lee C-Y, Chen H-T, Hsueh Y-J, Chen H-C, Huang C-C, Meir Y-JJ, et al. Perioperative topical ascorbic acid for the prevention of phacoemulsification-related corneal endothelial damage: Two case reports and review of literature. World J Clin Cases. 2019;7(5):642–9.
Ebrahimiadib N, Modjtahedi BS, Roohipoor R, Anesi SD, Foster CS. Successful Treatment Strategies in Granulomatosis With Polyangiitis-Associated Peripheral Ulcerative Keratitis. Cornea. 2016;35(11):1459–65.
James ER. The Etiology of Steroid Cataract. J Ocul Pharmacol Ther. 2007;23(5):403–20.
Jang JH, Ko YJ, Lee SW. A Case of Bilateral Peripheral Ulcerative Keratitis in a Patient with Rheumatoid Arthritis after Cataract Extraction. J Korean Ophthalmol Soc. 2013;54(5):808–12.
Movahedan A, Djalilian AR. Cataract surgery in the face of ocular surface disease. Curr Opin Ophthalmol. 2012;23(1):68–72.
John SL, Morgan K, Tullo AB, Holt PJL. Corneal autoimmunity in patients with peripheral ulcerative keratitis (PUK) in association with rheumatoid arthritis and Wegener’s granulomatosis. Eye. 1992;6:630.
Yagci A. Update on peripheral ulcerative keratitis. Clinical ophthalmology. 2012;6:747–54.
Smith VA, Hoh HB, Easty DL. Role of ocular matrix metalloproteinases in peripheral ulcerative keratitis. Br J Ophthalmol. 1999;83(12):1376–83.
Brejchova K, Liskova P, Cejkova J, Jirsova K. Role of matrix metalloproteinases in recurrent corneal melting. Exp Eye Res. 2010;90(5):583–90.
Kouakanou L, Xu Y, Peters C, He J, Wu Y, Yin Z et al: Vitamin C promotes the proliferation and effector functions of human γδ T cells. Cell Mol Immunol 2019.
Zhang P, Li J, Qi Y, Zou Y, Liu L, Tang X, et al. Vitamin C promotes the proliferation of human adipose-derived stem cells via p53–p21 pathway. Organogenesis. 2016;12(3):143–51.
Shima N, Kimoto M, Yamaguchi M, Yamagami S. Increased Proliferation and Replicative Lifespan of Isolated Human Corneal Endothelial Cells with l-Ascorbic acid 2-phosphate. Invest Ophthalmol Vis Sci. 2011;52(12):8711–7.
Acknowledgements
None.
Financial Disclosure
None.
Funding
This study was supported by Chang Gung Memorial Hospital, Linkou with an award number of CMRPG3G0021-3 and CMRPG3G0031-3 and by the Ministry of Science and Technology, Taiwan with an award number of MOST 107–2314-B-182A-088-MY3. The funders did not involve in the direction and the result of this work.
Author information
Authors and Affiliations
Contributions
Conception of the work: HTC, HCC. Design of the work: FCH, HTC, HCC. Acquisition of data: FCH, KJC, HCC. Analysis of data: KJC, YJH, YJJM, TTL, CMC, WCW. Interpretation of data: FCH, HTC, HCC. Drafted the work: FCH, HCC. Substantively revised the work: FCH, HCC. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This retrospective study was approved by the Institutional Review Board of the Chang Gung Medical Foundation. All procedures that were performed on the patient were in accordance with the Declaration of Helsinki. The cases were retrospectively reviewed, and this case report describes the course of the diagnostics and therapy but does not include data that can identify the patient.
Consent for publication
Written informed consent for publication of their clinical details and clinical images was obtained from the patients. A copy of the consent forms is available for review by the Editor of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
All authors meet the ICMJE authorship criteria.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hsiao, FC., Chen, HT., Chen, KJ. et al. Accelerated corneal endothelial cell loss in two patients with granulomatosis with polyangiitis following phacoemulsification. BMC Ophthalmol 20, 480 (2020). https://doi.org/10.1186/s12886-020-01752-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-020-01752-y