Abstract
Background
The lymphocyte-to-monocyte ratio (LMR) has been used as a parameter reflecting systemic inflammation in several tumors, and is reportedly associated with prognosis in cancer patients. In this study, we evaluated the predictive value of LMR for progression and chemosensitivity in breast cancer patients treated with preoperative chemotherapy.
Methods
LMR was evaluated in 239 patients with breast cancer treated with neoadjuvant chemotherapy (NAC) with 5-fluorouracil, epirubicin, and cyclophosphamide, followed by weekly paclitaxel with or without trastuzumab, and subsequent curative surgery. The correlations between LMR and clinicopathological features, prognosis, and pathological complete response (pCR) rate of NAC were evaluated retrospectively. We also evaluated the predictive value of neutrophil-to-lymphocyte ratio (NLR), and compared the predictive values of LMR and NLR.
Results
We set 6.00 as the cut-off level for LMR based on the receiver operating characteristic (ROC) curve. A total of 119 patients (49.8%) were classified in the high-LMR group and 120 (50.2%) were classified in the low-LMR group. The low-LMR group had significantly worse disease-free survival rate (DFS) in all patients (p = 0.005) and in triple-negative breast cancer patients (p = 0.006). However, there was no significant correlation between LMR and pCR. Multivariate analysis showed that low LMR was an independent risk factor for DFS (p = 0.008, hazard ratio = 2.245). However, there was no significant difference in DFS (p = 0.143, log-rank) between patients in the low- and high-NLR groups.
Conclusions
LMR may be a useful prognostic marker in patients with breast cancer.
Similar content being viewed by others
Background
Breast cancer is the most common type of cancer in women. Although neoadjuvant chemotherapy (NAC) increases the options for breast-conserving surgery and reduces the risk of postoperative recurrence in patients with resectable breast cancer [1,2,3,4], recurrence and metastasis still remain major problems, especially in patients with advanced-stage disease [5]. The tumor node metastasis (TNM) staging system and its associated phenotypes are important and useful tools for predicting prognosis [6, 7]. In breast cancer, molecular subtypes also affect the prognosis. Patients with triple-negative breast cancer (TNBC) or human epidermal growth factor receptor-2 (HER2)-enriched breast cancer have high recurrence rates and poor prognosis [8]. However, it has been reported that not only the tumor characteristics but also the host inflammatory response are important for cancer progression [9].
Inflammation affects cancer progression, and a chronic systemic inflammatory response is involved in poor outcome in breast cancer patients [10]. Furthermore, the host immune system has been found to influence the clinical response to chemotherapy, and should thus be taken into account even during conventional chemotherapy treatment [11]. Systemic inflammatory markers such as neutrophil to lymphocyte ratio (NLR) and platelet lymphocyte ratio (PLR) have been reported as prognostic factors in various cancers [12, 13]. Furthermore, the lymphocyte-to-monocyte ratio (LMR), which also reflects the degree of systemic inflammation, has recently been reported to correlate with survival in various types of malignancies, such as diffuse large B cell lymphoma, colon cancer, esophageal carcinoma, lung cancer [14,15,16,17]. In this single-center, retrospective study, we aimed to evaluate LMR and NLR as a possible marker for predicting the outcome of NAC in a consecutive series of patients with breast cancer treated with a standardized protocol.
Methods
Patient background
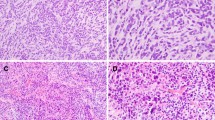
A total of 239 patients with resectable, early-stage breast cancer diagnosed as stage IIA (T1, N1, M0 or T2, N0, M0), IIB (T2, N1, M0 or T3, N0, M0), or IIIA (T1–2, N2, M0 or T3, N1–2, M0) were treated with NAC between 2007 and 2015. Tumor stage and T and N factors were stratified based on the TNM Classification of Malignant Tumors, UICC Seventh Edition [18]. Breast cancer was confirmed histologically by core needle biopsy and staged by systemic imaging studies using computed tomography, ultrasonography, and bone scintigraphy. Tumors were classified into subtypes according to the immunohistochemical expression of estrogen receptor, progesterone receptor, HER2, and Ki67. The cut-offs for estrogen receptor and progesterone receptor positivity were both > 0% positive tumor cells with nuclear staining. Tumors with 3+ HER2 on immunohistochemical staining were considered to show HER2 overexpression, tumors with 2+ HER2 were analyzed further by fluorescence in situ hybridization, and tumors with HER2/Centromere (CEP) 17 ≥ 2.0 were also considered to exhibit HER2 overexpression [19, 20]. A Ki67-labeling index ≥14% tumor cells with nuclear staining was determined to be positive [21].
All patients received a standardized NAC protocol consisting of four courses of FEC100 (500 mg/m2 fluorouracil, 100 mg/m2 epirubicin, and 500 mg/m2 cyclophosphamide) every 3 weeks, followed by 12 courses of 80 mg/m2 paclitaxel administered weekly [22, 23]. Sixty-eight patients had HER2-positive breast cancer and were additionally administered weekly (2 mg/kg) or tri-weekly (6 mg/kg) trastuzumab during paclitaxel treatment [24]. All patients underwent chemotherapy as outpatients. Therapeutic anti-tumor effects were assessed according to the Response Evaluation Criteria in Solid Tumors (RECIST) criteria [25]. Pathological complete response (pCR) was defined as the complete disappearance of the invasive compartment of the lesion with or without intraductal components, including the lymph nodes [1]. Patients underwent mastectomy or breast-conserving surgery after NAC. All patients who underwent breast-conserving surgery were administered postoperative radiotherapy to the remnant breast. Overall survival (OS) time was the period from the surgery to the time of death from any cause. Disease-free survival (DFS) was defined as freedom from all local, loco-regional, and distant recurrences. All patients were followed up by physical examination every 3 months, ultrasonography every 6 months, and computed tomography and bone scintigraphy annually. The median follow-up period for the assessment of OS was 3.7 years (range, 0.2–6.0 years) and for DFS was 3.4 years (range, 0.1–6.0 years).
Ethics statement
This study was conducted at Osaka City University Graduate School of Medicine, Osaka, Japan, according to the Reporting Recommendations for Tumor Marker Prognostic Studies (REMARK) guidelines and following a retrospectively written research, pathological evaluation, and statistical plan [26]. This research conformed to the provisions of the 2013 Declaration of Helsinki. All patients were informed of the investigational nature of this study and provided their written informed consent. The Ethics Committee of Osaka City University approved the study protocol (#926).
Blood sample analysis
Peripheral blood samples were obtained at the time of diagnosis, before the initiation of NAC. These were taken only once. The numbers of white blood cells were determined using a hemocytometer. The percentages of different cell types were determined using a Coulter LH 750 Hematology Analyzer (Beckman Coulter, Brea, CA, USA). LMR was calculated from the pretreatment blood sample by dividing the absolute lymphocyte count by the absolute monocyte count. NLR was calculated from the pretreatment blood sample by dividing the absolute neutrophil count by the absolute lymphocyte count. All patients had no self-reported acute infections or hematologic disorders.
Statistical analysis
Statistical analysis was performed using the JMP11 software program (SAS Institute, Cary, NC, USA). Receiver operating characteristic (ROC) curve analysis was performed to select the most appropriate cut-off values for LMR and NLR, to stratify patients at high risk of malignancy-related recurrences. The optimal cut-off value was established by means of Youden’s index. Associations between LMR, NLR, and clinicopathological variables, and the significance of different prognostic markers were analyzed using χ2 or Fisher’s exact test or Mann-Whitney U test, as appropriate. OS and DFS were estimated using the Kaplan–Meier method and compared using the log-rank test. Univariate and multivariate hazard ratios (HRs) were computed for the study parameters with 95% confidence intervals (CIs) using a Cox proportional hazards model, and used in a backward stepwise method selecting lymph node status, pathological response, and LMR for variable selection in multivariate analyses. A p value < 0.05 was considered significant.
Results
Clinical responses (pCR + partial response) were observed in 209 patients (87.5%, 209/239). NAC-related pCR was observed in 91 patients (38.1%, 91/239). The pCR rates were 48.2% (40/83) and 32.7% (51/156) in patients with TNBC and non-TNBC, respectively (Table 1). Among all cases, DFS was significantly better in the pCR group compared with the non-pCR group (p = 0.040) (Additional file 1: Figure S1a), while OS tended to be better in the pCR group (p = 0.058) (Additional file 1: Figure S1b).
LMR was determined in every sample and ranged from 1.8–15.2 (mean, 6.2; median, 5.9; standard deviation, 2.3). The LMR cut-off value for DFS was 6.00 (area under the curve (AUC): 0.57; sensitivity: 61.3%; specificity: 59.2%) (Additional file 2: Figure S2a). We therefore classified patients into low-LMR (n = 120, 50.2%) and high-LMR (n = 119, 49.8%) groups according to a cut-off value of 6.0 (Fig. 1). LMR was significantly correlated with age (p = 0.004), menopausal status (p = 0.008), and tumor size (p = 0.036). There was no significant correlation between LMR and any other tested clinicopathological parameter, including pCR (Table 2). In continuous variables, older age (p < 0.001), menopause (p < 0.001), and higher Ki-67 (p = 0.016) were significantly associated with higher LMR (Additional file 3: Figure S3). NLR was also determined in every sample, and ranged from 0.5–10.6 (mean, 2.3; median, 2.0; standard deviation, 1.3). The NLR cut-off value for DFS was 1.63 (AUC: 0.56; sensitivity: 75.6%; specificity: 36.7%) (Additional file 2: Figure S2b). We therefore classified patients into low-NLR (n = 74) and high-NLR (n = 165) groups according to a cut-off value of 1.63 (Fig. 1). NLR was significantly correlated with age (p < 0.001) and menopausal status (p < 0.001), but there was no significant correlation between NLR and any other tested clinicopathological parameter, including pCR. In continuous variables, older age (p = 0.011) and menopause (p = 0.008) were significantly associated with lower NLR (Additional file 4: Figure S4).
DFS was significantly worse in the low- compared with the high-LMR group (p = 0.005) (Fig. 2a), while OS tended to be worse in the low-LMR group (p = 0.059) (Fig. 2b). Among 83 TNBC patients, DFS was significantly longer (p = 0.006) in the high- compared with the low-LMR group (Fig. 2c), but OS was not significantly different (p = 0.191) (Fig. 2d). Among 156 non-TNBC patients, there was no significant difference between the low- and high-LMR groups in terms of DFS (p = 0.170) (Fig. 2e) or OS (p = 0.176) (Fig. 2f). There were no significant differences between the low- and high-NLR groups in terms of DFS or OS for all breast cancers (p = 0.143 and p = 0.359, respectively) (Fig. 3a,b), TNBC (p = 0.150 and p = 0.416, respectively) (Fig. 3c,d), and non-TNBC patients (p = 0.376 and p = 0.191, respectively) (Fig. 3e,f).
Survival was analyzed according to LMR. DFS was significantly worse in the low- compared with the high-LMR group (p = 0.005) (a). OS tended to be worse in the low- compared with the high-LMR group (p = 0.059) (b). Among 83 TNBC patients, DFS was significantly longer (p = 0.006) in the high- compared with the low-LMR group (c), but OS was not significantly different (p = 0.059) (d). Among 156 TNBC patients, there was no significant difference between the low- and high-LMR groups for DFS (p = 0.170) (e) or OS (p = 0.176) (f)
The correlations between DFS and the various clinicopathological factors in 239 all breast cancers are shown in Table 3. According to the results of univariate analysis, DFS exhibited significant relationships with lymph node status (p = 0.020), complete response to chemotherapy (p = 0.034), and LMR (p = 0.005). In contrast, NLR was not a prognostic factor for DFS (p = 0.116). Multivariate analysis indicated that lymph node status (HR = 2.826, 95 %CI: 1.281–7.474, p = 0.008), and LMR (HR = 2.245, 95 %CI: 1.237–4.233, p = 0.008) were independent prognostic factors for survival (Table 3). Additionally, in 83 TNBC patients, multivariate analysis revealed that pathological response (HR = 2.921, 95 % CI: 1.015–10.470, p = 0.047) and LMR (HR = 4.675, 95 % CI: 1.500–20.445, p = 0.006) were significantly correlated with RFS (Additional file 5: Table S1).
Discussion
Inflammation and cancer show a strong association, and pretreatment levels of peripheral inflammatory cells, including neutrophils, lymphocytes and monocytes are reported as prognositic factors in various cancers [27,28,29]. Lymphocytes play an important role in host tumor immunity (for example, in cytotoxic cell death and inhibition of tumor cell proliferation and migration) [30,31,32,33]. Decreased lymphocyte numbers are therefore considered to be responsible for an insufficient immunologic reaction to the tumor, thus promoting tumor progression and metastasis [15]. Monocytes are known to infiltrate tumors and differentiate into tumor-associated macrophages, which are involved in tumor proliferation, invasion, metastasis, neovascularization, and recurrence [34, 35]. Increased levels of monocytes thus reflect a high tumor burden in patients with cancer. In such a mechanism, LMR is believed to reflect the host immune status and the degree of tumor progression. Given that both a low lymphocyte count and high monocyte count reflect insufficient anti-tumor immunity and an elevated tumor burden, a low LMR is therefore associated with a poorer prognosis.
In this study, we evaluated the predictive value of pre-NAC LMR and NLR for progression and chemosensitivity in breast cancer, and compared the predictive values of these systemic inflammatory markers, and showed that LMR was significantly associated with DFS in all breast cancer patients who received NAC. This result suggests that LMR may be one of the criteria for deciding whether to perform adjuvant chemotherapies with active regimens from the beginning.
There are many publications concerning the prognostic value of LMR or NLR in breast cancer [36,37,38,39,40,41,42,43,44]. The appropriate cut-off values for LMR and NLR were set by ROC curve in most studies, and were not unified. Recently, Ethier et al. conducted meta-analysis on the relationship between NLR and prognosis of breast cancer, and reported that the median cut-off value for NLR was 3.0 [45]. However, to our knowledge, no meta-analysis on the relationship between LMR and prognosis of breast cancer has been conducted. In addition, some studies evaluated the predictive value of LMR or NLR for progression and chemosensitivity in breast cancer patients treated with NAC, however, there are few reports to investigate the prognostic value of both LMR and NLR in breast cancer patients following NAC. Marín et al. analysed 150 breast cancer patients treated with NAC and reported that patients with high LMR and low NLR were associated with good DFS [44]. On the other hand, our study reported that only LMR was significantly correlated with prognosis. There are two possible reasons for this inconsistent result. First, the appropriate cut-off values for LMR and NLR differed in each study. Second, the standardized protocol of NAC differed in each study. In Marín’s study, NAC regimen was based on anthracyclines and taxanes ± trastuzumab, and pCR rate was 17.6%. In our study, NAC regimen was based on FEC100 followed by weekly paclitaxel ± trastuzumab, and pCR rate was higher than Marín’s study, 38.1%. 5-fluorouracil is shown to increase the sensitivity of cancer cells to killing by cytotoxic T cells (CTLs). In addition, a DNA alkylating agent cyclophosphamide can lead to improved T cell effector functions and stimulate an immunogenic death. Moreover, CTLs are effective against paclitaxel-treated tumor cells and induce tumor cell apoptosis [46, 47]. In other words, our regimen plays a role in enhancing the immune response.
Moreover, the present study is the first to evaluate the prognostic value of both LMR and NLR in different molecular subtypes of breast cancer following NAC. Weijuan et al. reported that decreased LMR was significantly associated with a poor prognosis for TNBC subtype in a study of 1570 patients [38]. The present study found no relationship between LMR and intrinsic subtype, but did reveal significant differences in DFS among all 239 patients, and among 83 TNBC patients stratified by LMR. TNBC is known to exhibit poor clinical outcomes compared with non-TNBC, and a recent study suggested that TNBC may be more strongly influenced by systemic inflammatory function [41].
Recently, it is becoming evident that the surrounding cancer microenvironment greatly influences cancer cells and plays a role in the development of characteristic cancer features [48]. Lymphocytes play not only as systemic inflammatory markers but also as tumor-infiltrating lymphocytes (TILs) that evaluate tumor immune responses [49,50,51], and monocytes also relate to tumor-associated macrophages. Matsumoto et al. reported that high levels of tumor-infiltrating CD8+ T-cells may reflect an improved prognosis in terms of chemotherapy sensitivity in TNBC, and that tumor-associated macrophages were associated with a relatively poor outcome in patients with TNBC [52]. We also examined the prognostic significance of TILs before NAC in same breast cancer patients [53]. As in present study, DFS was significantly longer in the high TILs group than in the low TILs group among all breast cancer and TNBC patients. These results suggested that local immune tumor microenvironment and systemic inflammation had relationship. From now on, by further evaluating tumor-infiltrating lymphocytes or tumor-associated macrophages, along with systemic inflammatory markers such as LMR or NLR, more accurate identification of patient-specific immune mechanisms and prediction of prognosis may be possible.
As a potential limitation, this study is a single-center retrospective study, and the sample size is small, and the numbers of TNBC patients are thus even smaller. Further prospective multicenter studies are therefore needed to identify the strengths and weaknesses of our findings.
Conclusions
The findings of this study indicate that pretreatment LMR is a useful prognostic marker in patients with breast cancer.
Abbreviations
- CI:
-
Confidence interval
- CTLs:
-
Cytotoxic T cells
- DFS:
-
Disease-free survival
- HER2:
-
Human epidermal growth factor receptor-2
- HR:
-
Hazard ratio
- LMR:
-
Lymphocyte-to-monocyte ratio
- NAC:
-
Neoadjuvant chemotherapy
- NLR:
-
Neutrophil-to-lymphocyte ratio
- OS:
-
Overall survival
- pCR:
-
Pathological complete response
- RECIST:
-
Response Evaluation Criteria in Solid Tumors
- REMARK:
-
Reporting Recommendations for Tumor Marker Prognostic Studies
- ROC:
-
Receiver operating characteristic
- TILs:
-
Tumor-infiltrating lymphocytes
- TNBC:
-
Triple-negative breast cancer
- TNM:
-
Tumor node metastasis
References
Wolmark N, Wang J, Mamounas E, Bryant J, Fisher B. Preoperative chemotherapy in patients with operable breast cancer: nine-year results from National Surgical Adjuvant Breast and bowel project B-18. J Natl Cancer Inst Monogr. 2001;30:96–102.
van der Hage JA, van de Velde CJ, Julien JP, Tubiana-Hulin M, Vandervelden C, Duchateau L. Preoperative chemotherapy in primary operable breast cancer: results from the European Organization for Research and Treatment of Cancer trial 10902. J Clin Oncol. 2001;19(22):4224–37.
Mayer EL, Carey LA, Burstein HJ. Clinical trial update: implications and management of residual disease after neoadjuvant therapy for breast cancer. Breast Cancer Res. 2007;9(5):110.
Sachelarie I, Grossbard ML, Chadha M, Feldman S, Ghesani M, Blum RH. Primary systemic therapy of breast cancer. Oncologist. 2006;11(6):574–89.
Carlson RW, Allred DC, Anderson BO, Burstein HJ, Edge SB, Farrar WB, Forero A, Giordano SH, Goldstein LJ, Gradishar WJ, et al. Metastatic breast cancer, version 1.2012: featured updates to the NCCN guidelines. J Natl Compr Cancer Netw. 2012;10(7):821–9.
Carey LA, Perou CM, Livasy CA, Dressler LG, Cowan D, Conway K, Karaca G, Troester MA, Tse CK, Edmiston S, et al. Race, breast cancer subtypes, and survival in the Carolina breast Cancer study. JAMA. 2006;295(21):2492–502.
Singletary SE, Allred C, Ashley P, Bassett LW, Berry D, Bland KI, Borgen PI, Clark G, Edge SB, Hayes DF, et al. Revision of the American joint committee on Cancer staging system for breast cancer. J Clin Oncol. 2002;20(17):3628–36.
Kohler BA, Sherman RL, Howlader N, Jemal A, Ryerson AB, Henry KA, Boscoe FP, Cronin KA, Lake A, Noone AM, et al. Annual Report to the Nation on the Status of Cancer, 1975–2011, Featuring Incidence of Breast Cancer Subtypes by Race/Ethnicity, Poverty, and State. J Natl Cancer Inst. 2015;107(6):djv048.
Lu H, Ouyang W, Huang C. Inflammation, a key event in cancer development. Mol Cancer Res. 2006;4(4):221–33.
Iyengar NM, Hudis CA, Dannenberg AJ. Obesity and inflammation: new insights into breast cancer development and progression. Am Soc Clin Oncol Educ Book. 2013;33:46–51.
Menard C, Martin F, Apetoh L, Bouyer F, Ghiringhelli F. Cancer chemotherapy: not only a direct cytotoxic effect, but also an adjuvant for antitumor immunity. Cancer Immunol Immunother. 2008;57(11):1579–87.
Shibutani M, Maeda K, Nagahara H, Noda E, Ohtani H, Nishiguchi Y, Hirakawa K. A high preoperative neutrophil-to-lymphocyte ratio is associated with poor survival in patients with colorectal cancer. Anticancer Res. 2013;33(8):3291–4.
Neofytou K, Smyth EC, Giakoustidis A, Khan AZ, Cunningham D, Mudan S. Elevated platelet to lymphocyte ratio predicts poor prognosis after hepatectomy for liver-only colorectal metastases, and it is superior to neutrophil to lymphocyte ratio as an adverse prognostic factor. Med Oncol. 2014;31(10):239.
Li YL, Pan YY, Jiao Y, Ning J, Fan YG, Zhai ZM. Peripheral blood lymphocyte/monocyte ratio predicts outcome for patients with diffuse large B cell lymphoma after standard first-line regimens. Ann Hematol. 2014;93(4):617–26.
Stotz M, Pichler M, Absenger G, Szkandera J, Arminger F, Schaberl-Moser R, Samonigg H, Stojakovic T, Gerger A. The preoperative lymphocyte to monocyte ratio predicts clinical outcome in patients with stage III colon cancer. Br J Cancer. 2014;110(2):435–40.
Huang Y, Feng JF. Low preoperative lymphocyte to monocyte ratio predicts poor cancer-specific survival in patients with esophageal squamous cell carcinoma. Onco Targets Ther. 2015;8:137–45.
Hu P, Shen H, Wang G, Zhang P, Liu Q, Du J. Prognostic significance of systemic inflammation-based lymphocyte- monocyte ratio in patients with lung cancer: based on a large cohort study. PLoS One. 2014;9(9):e108062.
Greene FL, Sobin LH. A worldwide approach to the TNM staging system: collaborative efforts of the AJCC and UICC. J Surg Oncol. 2009;99(5):269–72.
Wolff AC, Hammond ME, Hicks DG, Dowsett M, McShane LM, Allison KH, Allred DC, Bartlett JM, Bilous M, Fitzgibbons P, et al. Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline update. J Clin Oncol. 2013;31(31):3997–4013.
Wolff AC, Hammond ME, Hicks DG, Dowsett M, McShane LM, Allison KH, Allred DC, Bartlett JM, Bilous M, Fitzgibbons P, et al. Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline update. Arch Pathol Lab Med. 2014;138(2):241–56.
Goldhirsch A, Wood WC, Coates AS, Gelber RD, Thurlimann B, Senn HJ, Panel m. Strategies for subtypes—dealing with the diversity of breast cancer: highlights of the St. Gallen international expert consensus on the primary therapy of early breast Cancer 2011. Ann Oncol. 2011;22(8):1736–47.
Mauri D, Pavlidis N, Ioannidis JP. Neoadjuvant versus adjuvant systemic treatment in breast cancer: a meta-analysis. J Natl Cancer Inst. 2005;97(3):188–94.
Mieog JS, van der Hage JA, van de Velde CJ. Preoperative chemotherapy for women with operable breast cancer. Cochrane Database Syst Rev. 2007;2:CD005002.
Buzdar AU, Valero V, Ibrahim NK, Francis D, Broglio KR, Theriault RL, Pusztai L, Green MC, Singletary SE, Hunt KK, et al. Neoadjuvant therapy with paclitaxel followed by 5-fluorouracil, epirubicin, and cyclophosphamide chemotherapy and concurrent trastuzumab in human epidermal growth factor receptor 2-positive operable breast cancer: an update of the initial randomized study population and data of additional patients treated with the same regimen. Clin Cancer Res. 2007;13(1):228–33.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–47.
McShane LM, Altman DG, Sauerbrei W, Taube SE, Gion M, Clark GM. Statistics subcommittee of the NCIEWGoCD: reporting recommendations for tumor marker prognostic studies. J Clin Oncol. 2005;23(36):9067–72.
Tibaldi C, Vasile E, Bernardini I, Orlandini C, Andreuccetti M, Falcone A. Baseline elevated leukocyte count in peripheral blood is associated with poor survival in patients with advanced non-small cell lung cancer: a prognostic model. J Cancer Res Clin Oncol. 2008;134(10):1143–9.
Schmidt H, Bastholt L, Geertsen P, Christensen IJ, Larsen S, Gehl J, von der Maase H. Elevated neutrophil and monocyte counts in peripheral blood are associated with poor survival in patients with metastatic melanoma: a prognostic model. Br J Cancer. 2005;93(3):273–8.
Wilcox RA, Ristow K, Habermann TM, Inwards DJ, Micallef IN, Johnston PB, Colgan JP, Nowakowski GS, Ansell SM, Witzig TE, et al. The absolute monocyte count is associated with overall survival in patients newly diagnosed with follicular lymphoma. Leuk Lymphoma. 2012;53(4):575–80.
Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454(7203):436–44.
Terzic J, Grivennikov S, Karin E, Karin M. Inflammation and colon cancer. Gastroenterology. 2010;138(6):2101–14 e2105.
Lin EY, Pollard JW. Role of infiltrated leucocytes in tumour growth and spread. Br J Cancer. 2004;90(11):2053–8.
Hoffmann TK, Dworacki G, Tsukihiro T, Meidenbauer N, Gooding W, Johnson JT, Whiteside TL. Spontaneous apoptosis of circulating T lymphocytes in patients with head and neck cancer and its clinical importance. Clin Cancer Res. 2002;8(8):2553–62.
Noy R, Pollard JW. Tumor-associated macrophages: from mechanisms to therapy. Immunity. 2014;41(1):49–61.
Qian BZ, Pollard JW. Macrophage diversity enhances tumor progression and metastasis. Cell. 2010;141(1):39–51.
Rimando J, Campbell J, Kim JH, Tang SC, Kim S. The pretreatment neutrophil/lymphocyte ratio is associated with all-cause mortality in black and white patients with non-metastatic breast Cancer. Front Oncol. 2016;6:81.
He J, Lv P, Yang X, Chen Y, Liu C, Qiu X. Pretreatment lymphocyte to monocyte ratio as a predictor of prognosis in patients with early-stage triple-negative breast cancer. Tumour Biol. 2016;37(7):9037–43.
Jia W, Wu J, Jia H, Yang Y, Zhang X, Chen K, Su F. The peripheral blood neutrophil-to-lymphocyte ratio is superior to the lymphocyte-to-monocyte ratio for predicting the long-term survival of triple-negative breast Cancer patients. PLoS One. 2015;10(11):e0143061.
Liu C, Huang Z, Wang Q, Sun B, Ding L, Meng X, Wu S. Usefulness of neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in hormone-receptor-negative breast cancer. Onco Targets Ther. 2016;9:4653–60.
Ni XJ, Zhang XL, Ou-Yang QW, Qian GW, Wang L, Chen S, Jiang YZ, Zuo WJ, Wu J, Hu X, et al. An elevated peripheral blood lymphocyte-to-monocyte ratio predicts favorable response and prognosis in locally advanced breast cancer following neoadjuvant chemotherapy. PLoS One. 2014;9(11):e111886.
Asano Y, Kashiwagi S, Onoda N, Noda S, Kawajiri H, Takashima T, Ohsawa M, Kitagawa S, Hirakawa K. Predictive value of neutrophil/lymphocyte ratio for efficacy of preoperative chemotherapy in triple-negative breast Cancer. Ann Surg Oncol. 2016;23(4):1104–10.
Ji H, Xuan Q, Yan C, Liu T, Nanding A, Zhang Q. The prognostic and predictive value of the lymphocyte to monocyte ratio in luminal-type breast cancer patients treated with CEF chemotherapy. Oncotarget. 2016;7(23):34881–9.
Chen Y, Chen K, Xiao X, Nie Y, Qu S, Gong C, Su F, Song E. Pretreatment neutrophil-to-lymphocyte ratio is correlated with response to neoadjuvant chemotherapy as an independent prognostic indicator in breast cancer patients: a retrospective study. BMC Cancer. 2016;16:320.
Marin, Hernandez C, Pinero Madrona A, Gil Vazquez PJ, Galindo Fernandez PJ, Ruiz Merino G, Alonso Romero JL, Parrilla Paricio P. Usefulness of lymphocyte-to-monocyte, neutrophil-to-monocyte and neutrophil-to-lymphocyte ratios as prognostic markers in breast cancer patients treated with neoadjuvant chemotherapy. Clin Transl Oncol. 2017;20(4):476–83.
Ethier JL, Desautels D, Templeton A, Shah PS, Amir E. Prognostic role of neutrophil-to-lymphocyte ratio in breast cancer: a systematic review and meta-analysis. Breast Cancer Res. 2017;19(1):2.
Ramakrishnan R, Gabrilovich DI. Mechanism of synergistic effect of chemotherapy and immunotherapy of cancer. Cancer Immunol Immunother. 2011;60(3):419–23.
Vacchelli E, Galluzzi L, Fridman WH, Galon J, Sautes-Fridman C, Tartour E, Kroemer G. Trial watch: chemotherapy with immunogenic cell death inducers. Oncoimmunology. 2012;1(2):179–88.
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–74.
Adams S, Gray RJ, Demaria S, Goldstein L, Perez EA, Shulman LN, Martino S, Wang M, Jones VE, Saphner TJ, et al. Prognostic value of tumor-infiltrating lymphocytes in triple-negative breast cancers from two phase III randomized adjuvant breast cancer trials: ECOG 2197 and ECOG 1199. J Clin Oncol. 2014;32(27):2959–66.
Denkert C, von Minckwitz G, Brase JC, Sinn BV, Gade S, Kronenwett R, Pfitzner BM, Salat C, Loi S, Schmitt WD, et al. Tumor-infiltrating lymphocytes and response to neoadjuvant chemotherapy with or without carboplatin in human epidermal growth factor receptor 2-positive and triple-negative primary breast cancers. J Clin Oncol. 2015;33(9):983–91.
Savas P, Salgado R, Denkert C, Sotiriou C, Darcy PK, Smyth MJ, Loi S. Clinical relevance of host immunity in breast cancer: from TILs to the clinic. Nat Rev Clin Oncol. 2016;13(4):228–41.
Matsumoto H, Koo SL, Dent R, Tan PH, Iqbal J. Role of inflammatory infiltrates in triple negative breast cancer. J Clin Pathol. 2015;68(7):506–10.
Asano Y, Kashiwagi S, Goto W, Takada K, Takahashi K, Hatano T, Takashima T, Tomita S, Motomura H, Ohsawa M, et al. Prediction of treatment response to neoadjuvant chemotherapy in breast Cancer by subtype using tumor-infiltrating lymphocytes. Anticancer Res. 2018;38(4):2311–21.
Acknowledgements
We thank Yayoi Matsukiyo and Tomomi Okawa (Department of Breast and Endocrine Surgery, Osaka City University Graduate School of Medicine) for helpful advice regarding data management.
Funding
This study was supported in part by Grants-in Aid for Scientific Research (KAKENHI, Nos. 25461992, 26461957, and 17 K10559) from the Ministry of Education, Science, Sports, Culture and Technology of Japan.
Availability of data and materials
The datasets supporting the conclusions of this article is included within the article.
Author information
Authors and Affiliations
Contributions
All authors were involved in the preparation of this manuscript. WG collected the data, and wrote the manuscript. SK, YA, KTakada, KTakashashi, TH and TT performed the operation and designed the study. WG, SK and ST summarized the data and revised the manuscript. HM, KH and MO made substantial contribution to the study design, performed the operation, and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Written informed consent was obtained from all subjects. This research conformed to the provisions of the Declaration of Helsinki in 2013. All patients were informed of the investigational nature of this study and provided their written, informed consent. The study protocol was approved by the Ethics Committee of Osaka City University (#926).
Consent for publication
Written informed consent was obtained from all patients.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:
Figure S1. Survival was analyzed according to pCR. Among breast cancer cases, DFS was significantly better in the pCR group compared with the non-pCR group (p = 0.040) (a) and OS tended to be better in the pCR group (p = 0.058) (b). (TIF 118 kb)
Additional file 2:
Figure S2. ROC curve analyses of the LMR and NLR in breast cancer patients. The LMR cut-off value for DFS was 6.00 (AUC: 0.57335, sensitivity: 61.3%, specificity: 59.2%) (a). The NLR cut-off value for DFS was 1.63 (AUC: 0.56064, sensitivity: 75.6%, specificity: 36.7%) (b). (TIF 167 kb)
Additional file 3:
Figure S3. Correlation between clinicopathological features and LMR in 239 all breast cancers in continuous variables. Older age (p < 0.001), menopause (p < 0.001), and higher Ki-67 (p = 0.016) were significantly associated with higher LMR. (TIF 141 kb)
Additional file 4:
Figure S4. Correlation between clinicopathological features and NLR in 239 all breast cancers in continuous variables. Older age (p = 0.011) and menopause (p = 0.008) were significantly associated with lower NLR. (TIF 128 kb)
Additional file 5
Table S1. Univariate- and multivariate analysis with respect to disease-free survival in 83 triple-negative breast cancer. (DOCX 21 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Goto, W., Kashiwagi, S., Asano, Y. et al. Predictive value of lymphocyte-to-monocyte ratio in the preoperative setting for progression of patients with breast cancer. BMC Cancer 18, 1137 (2018). https://doi.org/10.1186/s12885-018-5051-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-018-5051-9