Abstract
Background
Preterm birth, a leading cause of neonatal death, is more common in multiple births and thus there has being an increasing call for reducing multiple births in ART. However, few studies have compared risk factors for preterm births amongst ART and non-ART singleton birth mothers.
Methods
A population-based study of 393,450 mothers, including 12,105 (3.1%) ART mothers, with singleton gestations born between 2007 and 2009 in 5 of the 8 jurisdictions in Australia. Univariable and multivariable logistic regression models were conducted to evaluate socio-demographic, medical and pregnancy factors associated with preterm births in contrasting ART and non-ART mothers.
Results
Ten percent of singleton births to ART mothers were preterm compared to 6.8% for non-ART mothers (P < 0.01). Compared with non-ART mothers, ART mothers were older (mean 34.0 vs 29.7 yr respectively), less socio-economically disadvantaged (12.4% in the lowest quintile vs 20.7%), less likely to be smokers (3.8% vs 19.4%), more likely to be first time mothers (primiparous 62.4% vs 40.5%), had more preexisting hypertension and complications during pregnancy. Irrespective of the mode of conception, preexisting medical and pregnancy complications of hypertension, diabetes and antepartum hemorrhages were consistently associated with preterm birth. In contrast, socio-demographic variables, namely young and old maternal age (<25 and >34), socioeconomic disadvantage (most disadvantaged quintile Odds Ratio (OR) 0.95, 95% Confidence Interval (CI): 0.77–1.17), smoking (OR 1.12, 95%CI: 0.79–1.61) and priminarity (OR 1.19, 95% CI: 1.05–1.35, AOR not significant) shown to be associated with elevated risk of preterm birth for non-ART mothers were not demonstrated for ART mothers, even after adjusting for potential confounders. Nonetheless, in multivariable analysis, the association between ART and the elevated risk for singleton preterm birth persisted after controlling for all included confounding medical, pregnancy and socio-economic factors (AOR 1.51, 95% CI: 1.42–1.61).
Conclusions
Preterm birth rate is approximately one-and-a-half-fold higher in ART mothers than non-ART mothers albeit for singleton births after controlling for confounding factors. However, ART mothers were less subject to the adverse influence from socio-demographic factors than non-ART mothers. This has implications for counselling prospective parents.
Similar content being viewed by others
Background
Preterm birth (gestation of <37 weeks) is a global public health problem [1],[2]. More than one-third of neonatal deaths (death in the first four weeks of life) are directly attributable to preterm birth in 2010 [2],[3]. Survivors of preterm birth are at increased risk of neonatal morbidity [4],[5] and long-term adverse health outcomes including cerebral palsy, cognitive impairment [6], neurosensory deficits [3] and pulmonary disease [3]. Further, the cost to the health sector of preterm infants is substantial [7], and the hospital cost increases exponentially with decreasing gestational age [8].
Assisted reproductive technology (ART), defined by the World Health Organization and the International Committee Monitoring Assisted Reproductive Technologies as treatment that involves the handling of human oocytes (eggs) and sperms or embryos in a laboratory to establish pregnancies [9], has increasingly been used to treat infertility. It was estimated that ART has contributed to the birth of over 5 million liveborn babies worldwide [10]. ART has been associated with a significantly higher rate of multiple gestational pregnancies which are associated with increased risk of preterm birth [11]. However, elevated risk of preterm birth following ART has also been found for singleton pregnancies compared with non-ART singleton pregnancies [12]-[14].
International studies have shown that the socio-demographic characteristics, pregnancy-related complications and medical conditions of women giving birth after ART differ from non-ART mothers [15],[16]. However, few studies have investigated whether preterm birth, a multifactorial condition [17], is associated with varied sets of risk factors in these two groups.
Australia has one of the highest rates of ART utilisation as well as the practice of single embryo transfer in the world [18]-[20]. In 2011, 61,158 ART treatment cycles were undertaken in Australia, representing 12.9 cycles per 1,000 women of reproductive age (15–44 years) [21]. National data shows that over 17% of ART babies were preterm, which was markedly higher than the proportion of preterm babies (8.3%) born in Australia in 2010 [22],[23]. It is therefore timely to examine the association of ART and preterm birth.
Since 2007, the National Perinatal Data Collection (NPDC) which collects information on all births in Australia, has included information on use of ART [24]. The present study is the first large population-based study to investigate the association between ART and the risk of singleton preterm birth. The aims of this study were to: (1) Compare the socio-demographic, medical and pregnancy characteristics of ART and non-ART mothers; (2) Investigate the association between ART and preterm birth; and (3) Identify and compare risk factors associated with preterm birth for ART and non-ART mothers.
Methods
Data source
Perinatal data were provided on an annual basis by the health authorities in all Australian states and territories and compiled into the NPDC [24]-[26]. The NPDC includes national information on the pregnancy and childbirth of all Australian mothers, and the characteristics and outcomes of their babies. Namely NPDC includes maternal demographic factors; mothers’ medical conditions prior to pregnancy; complications during pregnancy; ART status; labour, mode of birth and perinatal outcomes. A birth is defined as a stillbirth or live birth of at least 20 weeks of gestation or at least 400 grams birthweight.
Data quality
All singleton births during the study period between 1 January 2007 to 31 December 2009 from 5 of the 8 states and territories where data on ART use was available (Victoria, Queensland, Western Australia, Tasmania and Australian Capital Territory) were extracted from NPDC. Of these, 19,118 records that did not state ART status (4.6%) and 59 records that did not state gestational age (<0.1%). The data quality statement for the NPDC was published in reports Australia’s mothers and babies 2007, 2008 and 2009 [24]-[26].
Data about most variables was with minor missings. However, maternal pre-pregnancy body mass index (BMI) and smoking during pregnancy were not required data items in the NPDC, so BMI was available for women in only one jurisdiction between 2008 and 2009 (N = 119,257), accounting for 30.31% of all women in the study population. Whether a woman smoked during pregnancy was indicated for women in two jurisdictions between 2007 and 2009, and one jurisdiction between 2008 and 2009 (N = 253,444), accounting for 64.42% of all women in the study population. Maternal pre-existing medical conditions including essential hypertension, diabetes mellitus and epilepsy were available in all but one jurisdiction in 2009 (N = 387,256), accounting for 98.43% of the study population.
Study population
The inclusion criteria for the study population consisted of singleton births during the study period from the 5 jurisdictions. The 19,118 records that did not state ART status and 59 records that did not state gestational age were excluded.
The final study population consisted of 393,450 women who gave birth to singleton babies, accounting for 45.6% of all singleton births in Australia during the three-year period.
Variables
The main outcome variable was preterm birth, this dichotomous variable was defined as < 37 completed weeks of gestation. The other outcome variable is gestational age, a continues variable.
The exposure variable was a dichotomous variable of ART status (yes or no). Other risk factors were selected based on published literature and were classified into three conceptual groups; (1) Demographic factors including maternal age, country of birth (Australia or overseas); smoking status during pregnancy (yes, no and not stated); pre-pregnancy BMI; remoteness (major cities, inner regional, outer regional, remote, very remote or other); health insurance type (public, private cover or other), Socio-Economic Indexes for Areas (SEIFA) (categorised into quintiles) [27]; and parity (grouped as primiparous and multiparous); (2) Maternal pre-existing medical conditions including essential hypertension, diabetes mellitus and epilepsy; and (3) Complications arising in pregnancy including hypertensive disorders in pregnancy, gestational diabetes and antepartum haemorrhage. The socio-economic status was measured by Socio-economic Indexes for Areas (SEIFA). The Index of Relative Socio-Economic Disadvantage (IRSD). The indexes ranked geographic areas across Australia in terms of their socio-economic characteristics. The SEIFA indexes were created by combining information collected in the five-yearly Census of Population and Housing in Australia [26].
Statistical analysis
Descriptive statistics were generated to compare maternal characteristics and outcomes between ART and non-ART mothers; student t-test was used for continuous variables; and Pearson’s χ2-test was used for categorical variables.
The odds of singleton preterm births in ART and non-ART mothers were compared using univariable and multivariable logistic regression models. The multiple logistic regression model was adjusted for maternal age, country of birth, smoking status during pregnancy, SEIFA, parity, health insurance type, remoteness, essential hypertension, diabetes mellitus, epilepsy, hypertensive disorders in pregnancy, gestational diabetes and antepartum haemorrhage. Such analysis was conducted within the total study population and within populations stratified by women’s parity.
Univariable and stepwise multivariable logistic regression analyses were conducted separately in the ART and non-ART mothers to calculate crude and adjusted odds ratios for each risk factor in relation to preterm birth.
Missing and not applicable data were included in regression models as a separate group. Items with less than 20 cases in any category were excluded from the model. Data analysis was performed using IBM Statistical Package for Social Sciences (SPSS), version 20. Findings with a P-value <0.05 or a CI not including 1 were considered statistically significant.
Ethics approval
Ethics approval was received for the study from the Human Research Ethics Committee of the University of New South Wales (HREC Ref: # HC11024) and Australian Institute of Health and Welfare (HREC Ref: # EC2011/1/5).
Results
Characteristics of women who gave birth to singletons by ART status
Of the 393,450 women who had singleton births, 12,105 (3.1%) gave birth following ART treatment, and 381,345 (96.9%) did not use ART.
The socio-demographic characteristics of mothers who underwent ART treatment were significantly different to those of mothers who did not have ART treatment (Table 1). The average age of ART mothers was significantly higher than for non-ART mothers (34.0 years versus 29.7 years, P < 0.01), and ART mothers were more likely to be aged ≥35 years (47.1% versus 21.4%, P < 0.01) at the time of delivery. ART mothers were more likely to be first-time mothers (62.4%) compared with non-ART mothers (40.5%; P < 0.01). Further, compared with non-ART mothers, higher proportions of ART mothers were born in Australia, were non smokers, had a higher socioeconomic status (SES), were non-obese, resided in major cities and had private health insurance (Table 1). However, of the three pre-existing medical conditions examined, only essential hypertension was significantly more prevalent among ART mothers (1.2% versus 0.9%, P = 0.01) (Table 2). The obstetric characteristics differed according to mothers’ mode of conception. The prevalence of hypertensive disorders in pregnancy, gestational diabetes and antepartum haemorrhage were significantly higher among ART mothers than non-ART mothers (6.1% versus 4.4% P < 0.01, 7.5% versus 5.0% P < 0.01, and 5.0% versus 2.8% P < 0.01 respectively) (Table 2).
The proportion of preterm births in ART mothers (10.1%) was significantly higher compared with non-ART mothers (6.8%) (P < 0.01); and the average length of gestation was shorter in ART pregnancies compared with non-ART pregnancies (38.4 weeks versus 38.9 weeks, P < 0.01) (Table 3).
Association between ART and preterm birth
Table 4 shows a positive association between ART treatment and preterm birth (OR 1.54; 95% CI: 1.45–1.63); the risk of preterm birth was only marginally reduced after multiple potential confounders were adjusted (AOR 1.51; 95% CI: 1.42–1.61). Sub-group analysis on data from the jurisdiction where BMI was available indicates the odds of preterm birth for ART mothers were 59% higher than for non-ART mothers (AOR 1.59; 95% CI: 1.42–1.77).
Compared with non-ART singletons, ART singletons were at 44% (AOR 1.44, 95% CI: 1.33–1.56) and 60% (AOR 1.60, 95% CI: 1.43–1.78) of increased odds of being preterm among primiparous and multiparous mothers respectively.
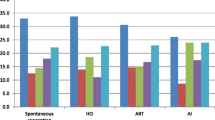
Risk factors for preterm birth by ART status
The differences in characteristics of ART and non-ART mothers suggest there may be variations in risk factors for preterm birth between the two groups. Therefore, risk factors relating to preterm birth were analysed separately among non-ART and ART mothers (Tables 5 and 6).
All of the factors examined, except for the mother’s country of birth, were associated with preterm births among non-ART mothers (Table 5). The most pronounced demographic factor associated with preterm birth following non-ART treatment was smoking during pregnancy (AOR 1.55, 95% CI: 1.50–1.61) (Table 5).
However, sociodemographic factors, including maternal age, parity, smoking during pregnancy, socioeconomic status, remoteness and patients’ insurance type, previously seen to play a role in predisposing preterm birth among non-ART mothers were no longer associated with preterm birth among ART mothers (Table 6).
ART and non-ART mothers share some common risk factors for preterm birth: the pre-existing maternal medical conditions and complications arising during pregnancy, including pre-existing hypertension (AOR 2.16 (1.39–3.36) and 2.05 (1.86–2.27)), diabetes mellitus (2.74 (1.61–4.67) and 4.13 (3.75–4.56)), hypertensive disorders in pregnancy (3.21 (2.67–3.87) and 2.94 (2.81–3.08)), gestational diabetes (1.43 (1.17–1.76) and 1.27 (1.20–1.34)) and antepartum haemorrhage (4.83 (4.01–5.82) and 7.11 (6.80-7.43)) (Tables 5 and 6).
Antepartum haemorrhage showed the strongest association with preterm birth in both ART (AOR 4.83, 95%CI: 4.01–5.82) and non-ART (AOR 7.11, 95% CI: 6.80–7.43) mothers, although the association was stronger in the non-ART group (Tables 5 and 6). Diabetes mellitus and hypertensive disorders in pregnancy were identified as the second strongest risk factors among ART and non-ART mothers respectively (Tables 5 and 6).
Discussion
As Australia was an early adopter of single embryo transfer in clinical practise, it is timely to investigate whether ART is independently associated with preterm birth and whether risk factors related to preterm birth vary by the mode of conception. There were three main findings of this study: (1) The characteristics of women who gave birth to singleton babies in Australia varied by the mode of conception; (2) The odds of singleton preterm birth among women who gave birth after ART in Australia was approximately one-and-a-half-fold compared with non-ART mothers; and (3) Risk factors associated with preterm birth differ between ART and non-ART mothers.
Findings from this study suggest that ART is independently associated with singleton preterm birth. Notwithstanding the inability to control for the number of embryos transferred, the odds of preterm birth in women with singleton birth following ART treatment is 1.51-fold (95% CI: 1.42–1.61) compared to non-ART mothers. This finding was consistent with the 1.54-fold in a recent systematic review (95% CI: 1.47–1.62) [28]; but was comparatively lower than the approximately two-fold risk of preterm birth found in three earlier systematic reviews published in 2004 [12]-[14]. The reduction in risk may be partially explained by increased use of single embryo transfer resulting in fewer preterm births among singletons as shown by our group [29]-[31].
The characteristics of women giving birth after ART in Australia were markedly different to their non-ART counterparts, this finding is consistent with two earlier international studies from the US [15],[16], ART mothers were older, more socioeconomically privileged and more likely to be first-time mothers; the proportion of essential hypertension and complications in pregnancy were also higher in this group. The differences in characteristics between the two groups suggest that risk factors associated with preterm birth in the ART group may differ from those for non-ART mothers. An array of socio-demographic factors was found to be associated with preterm birth among non-ART mothers. Interestingly, the important demographic factors predisposing preterm birth among non-ART mothers, namely age, socioeconomic status, smoking and parity were no longer found to be associated with preterm birth among ART mothers. This may be due to the relative homogeneity of the ART group. This result is consistent with Tepper’s study which is, to our knowledge, the only previous study that investigated risk factors associated with singleton preterm birth by the use of ART. The US study also found that socioeconomic factors had weaker associations with preterm birth among the ART mothers than among non-ART mothers [15].
In addition to gestational hypertension and diabetes in pregnancy identified by Tepper and colleagues [15], the present study found that essential hypertension, diabetes mellitus and antepartum haemorrhage were, independently associated with increased odds of preterm birth regardless of the mode of conception. Prevention and proper management of these conditions before and during pregnancy for both ART and non-ART mothers are important.
The current study revealed socioeconomic inequity related to the use of ART in Australia. Although Australia is one of the few countries in the world that have ART services meeting the level of demand [32], the utilisation of these services varied according to one’s socioeconomic background. More than two-thirds of ART mothers were covered by private health insurance, while the majority of the non-ART group were public patients. There also is a positive association between elevated risk of preterm birth and low SES among non-ART mothers. This finding is comparable with international studies that used maternal educational attainment and neighbourhood income as indicators of SES [33]-[35]. The current study demonstrated that mothers from the lowest SES quintile had a 14% excess risk of preterm birth compared with mothers from the highest quintile (AOR 1.14, 95% CI: 1.09–1.19). This result is very similar to the finding in a Canadian study (AOR 1.14, 95% CI: 1.10–1.17) [35]. A low SES is associated with unintended/unwanted pregnancies, which were shown to play a role in increasing the risk of preterm birth [36],[37].
The absence of socio-demographic and economic risk factors among mothers who gave birth after ART may be related to their overall high SES. In a Massachusetts study, Schieve and colleagues [16] demonstrated that ART mothers tended to receive more adequate antenatal care initiated from an earlier stage of pregnancy compared with non-ART mothers. Adequate antenatal care was shown to be protective against preterm birth [38]-[40]. A Finnish study also attributed the improved perinatal outcomes after IVF treatment over time to the more intense care received by ART mothers [41]. Furthermore, unintended pregnancies do not play a role in predisposing preterm birth in ART mothers because all pregnancies following ART are planned. The more adequate antenatal care received by ART mothers may at least in part compensate for the adverse effects resulting from giving birth at an advanced age and being primiparous.
Similar to the age distribution of ART mothers in Massachusetts [15], the current study found that 47.1% of ART mothers were over 35 years old; in comparison, approximately 21.4% of non-ART mothers were over 35 years old. Further, as also found in Tepper and colleagues’ study, the association between maternal age and preterm birth was present among non-ART mothers but was absent among ART mothers. However, the absence of such association should be interpreted with caution as advancing maternal age remains an important risk factor associated with declining success rate of clinical pregnancy after an IVF procedure [42]. Additionally, women aged more than 35 are more likely to have double embryo transfer [43], a practice leading to the high incidence of multiple gestation which can result in vanishing twin and singletons that are preterm [44]. Finally, other unfavourable obstetric complications, such as chromosomal abnormality, increase markedly with advancing maternal age [45]. Therefore, women should not postpone their motherhoods albeit that age is not a significant risk factor for preterm birth after ART treatment.
Compared with non-ART mothers, the proportion of ART mothers who smoked during pregnancy was significantly less (3.8% versus 19.4%, P < 0.01). Infertile couples seeking ART treatment tend to experience higher level of anxiety upon losing the pregnancy [46], it is therefore understandable that ART women were more mindful of factors such as cigarette smoking that predisposes miscarriage [47]. As shown by Tepper and colleagues, the percentage of smoking decreased from 5.6% prior conception to 1.7% after conception among ART women, while this decrement was milder among non-ART women (from 17.0% to 9.8%) [15].
As anticipated, smoking was found to be a risk factor predisposing preterm births among mothers who did not use ART. Surprisingly, the current study did not demonstrate an association between smoking and preterm birth among mothers who gave birth after ART treatment. A possible type II error may be caused by the small number of preterm birth among ART mothers who smoke (35 in total). Given that there is a dose–response relationship between the quantity of cigarettes smoked and preterm birth [48], if ART mothers who smoke were exposed to smaller quantities of cigarettes compared with non-ART mothers, the statistical model might fail to detect the effect of smoking on preterm birth among ART mothers. Notwithstanding, couples should be counselled to cease smoking during pregnancy to minimise risk to the unborn fetus.
The strength of the current study is that it is a population-based study containing validated, singleton birth records for five out of eight Australian jurisdictions. Up to 0.4 million mothers were included in the study population, accounting for approximately 45% of all singleton births in the three-year period. The age of mothers and the prevalence of preterm birth among singleton infants following ART treatment included in the study resume the entire Australian and New Zealand. The average age of women at the time of delivery was 34.0 ± 4.8 in this study, comparable with 34.8 in 2007 [49] and 35.0 in 2008 and 2009 [20],[50] based on data from The Australian and New Zealand Assisted Reproduction Database. The 10.1% preterm birth prevalence in the current study is also similar to the levels in Australia and New Zealand, where the prevalence of singleton preterm birth following ART treatment was 10.5% in 2007 [49], 10.7% in 2008 [50] and 9.9% in 2009 [49]. Therefore the results can be generalised to the nation with the unique socio-demographic and economic context of each State and Territory taken into consideration, especially in Northern Territory that has the highest percentage of Indigenous women who give birth and second highest smoking rate [24]-[26]. With more than twelve thousand ART mothers included in the study, the diminished associations between multiple sociodemographic factors and preterm birth were unlikely to be due to reduced population size.
We acknowledge some limitations of the current study. Data were not available on the number of embryos transferred. Data for smoking during pregnancy and BMI were missing in some states and territories during the study period. Nevertheless, the quality of data from jurisdictions that provided BMI and smoking information were good, accounting for approximately 30% and 64% of the study population respectively. Sub-group analysis on data where BMI was available showed similar result to the AOR produced for the whole study population.
Although caesarean section is an obstetric precursor for preterm birth [17], this association was not investigated in this study. A caesarean section could result from emergency or various clinical complications, however in the data collection it was not possible to identify if an elective caesarean section was indeed planed or not and its indications. Future studies could examine this link.
The current study did not include information on previous obstetric history, such as whether the pregnancy was subsequent to a prior preterm birth, which has been shown in the literature to be independently associated with preterm birth [51],[52]. A South Australian study restricted the study population to women in their first singleton pregnancy so as to remove the confounding effect of multiple pregnancies, parity and previous preterm birth [53]. In the current study, adjustment was made for parity in the regression model instead of stratifying for primiparous women. Sub-group analysis showed a comparable association between preterm birth and ART for both primiparous and multiparous women.
As a cross sectional data collection, the NPDC dataset does not provide information regarding to separate deliveries for a same woman. Future studies using longitudinal data would consider linking deliveries for the same women.
From a clinical perspective, couples in Australia who are considering using ART should be informed about the potential of increased risk of preterm birth even for singleton births. Antenatal care guidelines should include consideration of a woman’s mode of conception reflecting the variation in risk factors for ART and non-ART mothers, and the excess risk of preterm birth for ART mothers.
The findings of this study underscore the possibility that the mechanism causing preterm birth following ART treatment is different from preterm birth in the general population even after elimination the confounding factor of multiple gestation. The literature has postulated that the underlying causes of infertility may explain the elevated risk of preterm births among ART mothers [54],[55]. Further research is required. In addition, further studies may focus on determining whether there are variations in risk factors for other adverse birth outcomes, such as very preterm birth (<32 weeks of gestation), by the use of ART.
Conclusions
The current study identified ART as an independent risk factor for preterm birth in an Australian setting and that there are variations of risk factors associated with preterm birth for ART and non-ART mothers. Couples should be informed about the elevated risk of preterm birth associated with ART, and criteria for ART mothers should be developed that identify individuals who are at high risk of preterm birth. Further studies may focus on assessing the associations between the stated risk factors and other adverse perinatal outcomes in ART mothers.
Abbreviations
- AIHW:
-
Australian Institute of Health and Welfare
- AOR:
-
Adjusted odds ratio
- ART:
-
Assisted reproductive technology
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- IVF:
-
In vitro fertilisation
- NPDC:
-
National perinatal data collection
- OR:
-
Odds ratio
- SEIFA:
-
Socio-economic indexes for areas
- SES:
-
Socioeconomic status
- SPSS:
-
Statistical package for social sciences
References
Beck S, Wojdyla D, Say L, Betran AP, Merialdi M, Requejo JH, Rubens C, Menon R, Van Look PF: The worldwide incidence of preterm birth: a systematic review of maternal mortality and morbidity. Bull World Health Organ. 2010, 88: 31-38. 10.2471/BLT.08.062554.
Liu L, Johnson HL, Cousens S, Perin J, Scott S, Lawn JE, Rudan I, Campbell H, Cibulskis R, Li M: Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet. 2012, 379: 2151-2161. 10.1016/S0140-6736(12)60560-1.
Howson ECP, Kinney MV, Lawn JE: Born Too Soon: The Global Action Report on Preterm Birth. 2012, World Health Organization, Geneva
Shapiro-Mendoza CK, Tomashek KM, Kotelchuck M, Barfield W, Nannini A, Weiss J, Declercq E: Effect of late-preterm birth and maternal medical conditions on newborn morbidity risk. Pediatrics. 2008, 121: e223-e232. 10.1542/peds.2006-3629.
McIntire DD, Leveno KJ: Neonatal mortality and morbidity rates in late preterm births compared with births at term. Obstet Gynecol. 2008, 111: 35-41. 10.1097/01.AOG.0000297311.33046.73.
Moster D, Lie RT, Markestad T: Long-term medical and social consequences of preterm birth. N Engl J Med. 2008, 359: 262-273. 10.1056/NEJMoa0706475.
Petrou S, Sach T, Davidson L: The long-term costs of preterm birth and low birth weight: results of a systematic review. Child Care Health Dev. 2001, 27: 97-115. 10.1046/j.1365-2214.2001.00203.x.
Gilbert WM, Nesbitt TS, Danielsen B: The cost of prematurity: quantification by gestational age and birth weight. Obstet Gynecol. 2003, 102: 488-492. 10.1016/S0029-7844(03)00617-3.
Zegers-Hochschild F, Adamson GD, de Mouzon J, Ishihara O, Mansour R, Nygren K, Sullivan E, Vanderpoel S: International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) revised glossary of ART terminology, 2009. Fertil Steril. 2009, 92: 1520-1524. 10.1016/j.fertnstert.2009.09.009.
Adamson G, Tabangin M, Macaluso M, de Mouzon J: The number of babies born globally after treatment with the assisted reproductive technologies (ART). Fertil Steril. 2013, 100: S42-10.1016/j.fertnstert.2013.07.1807.
Blondel B, Kaminski M: Trends in the occurrence, determinants, and consequences of multiple births. Semin Perinatol. 2002, 26: 239-249. 10.1053/sper.2002.34775.
Jackson RA, Gibson KA, Wu YW, Croughan MS: Perinatal outcomes in singletons following in vitro fertilization: a meta-analysis. Obstet Gynecol. 2004, 103: 551-563. 10.1097/01.AOG.0000114989.84822.51.
Helmerhorst FM, Perquin DA, Donker D, Keirse MJ: Perinatal outcome of singletons and twins after assisted conception: a systematic review of controlled studies. BMJ. 2004, 328: 261-10.1136/bmj.37957.560278.EE.
McGovern PG, Llorens AJ, Skurnick JH, Weiss G, Goldsmith LT: Increased risk of preterm birth in singleton pregnancies resulting from in vitro fertilization-embryo transfer or gamete intrafallopian transfer: a meta-analysis. Fertil Steril. 2004, 82: 1514-1520. 10.1016/j.fertnstert.2004.06.038.
Tepper NK, Farr SL, Cohen BB, Nannini A, Zhang Z, Anderson JE, Jamieson DJ, Macaluso M: Singleton preterm birth: risk factors and association with assisted reproductive technology. Matern Child Health J. 2012, 16: 807-813. 10.1007/s10995-011-0787-8.
Schieve LA, Cohen B, Nannini A, Ferre C, Reynolds MA, Zhang Z, Jeng G, Macaluso M, Wright VC: A population-based study of maternal and perinatal outcomes associated with assisted reproductive technology in Massachusetts. Matern Child Health J. 2007, 11: 517-525. 10.1007/s10995-007-0202-7.
Goldenberg RL, Culhane JF, Iams JD, Romero R: Epidemiology and causes of preterm birth. Lancet. 2008, 371: 75-84. 10.1016/S0140-6736(08)60074-4.
Maheshwari A, Griffiths S, Bhattacharya S: Global variations in the uptake of single embryo transfer. Hum Reprod Update. 2011, 17: 107-120. 10.1093/humupd/dmq028.
Chambers GM, Illingworth PJ, Sullivan EA: Assisted reproductive technology: public funding and the voluntary shift to single embryo transfer in Australia. Med J Aust. 2011, 195: 594-598. 10.5694/mja10.11448.
Wang Y, Macaldowie A, Hayward I, Chambers G, Sullivan E: Assisted Reproductive Technology in Australia and New Zealand 2009. 2011, AIHW, Canebrra
Macaldowie A, Wang Y, Chambers G, Sullivan E: Assisted Reproductive Technology in Australia and New Zealand 2011. 2013, National Perinatal Epidemiology and Statistics Unit, the University of New South Wales, Sydney
Li Z, Zeki R, Hilder L, Sullivan EA: Australia’s Mothers And Babies 2010. Perinatal Statistics Series no. 27. Cat. no. PER 57. 2012, AIHW National Perinatal Epidemiology and Statistics Unit, Canberra
Macaldowie A, Wang Y, Chambers G, Sullivan E: Assisted Reproductive Technology in Australia and New Zealand 2010. 2012, AIHW, Canberra
Laws P, Sullivan EA: Australia’s mothers and babies 2007. 2009, AIHW National Perinatal Statistics Unit, Sydney
Laws P, Li Z, Sullivan E: Australia’s Mothers and Babies 2008. 2010, AIHW, Canberra
Li Z, McNally L, Hilder L, Sullivan EA: Australia’s Mothers and Babies 2009. 2011, AIHW National Perinatal Epidemiology and Statistics Unit, Sydney
Pink B: Information Paper: An Introduction to Socio-economic Indexes for Areas (SEIFA), 2006. 2008, Australian Bureau of Statistics, Canberra
Pandey S, Shetty A, Hamilton M, Bhattacharya S, Maheshwari A: Obstetric and perinatal outcomes in singleton pregnancies resulting from IVF/ICSI: a systematic review and meta-analysis. Hum Reprod Update. 2012, 18: 485-503. 10.1093/humupd/dms018.
Wang YA, Macaldowie A, Hayward I, Chambers GM, Sullivan EA: Assisted Reproductive Technology in Australia and New Zealand 2009: Assisted Reproduction Technology Series no. 15: Cat. no. PER 51. 2011, AIHW, Canberra
Wang YA, Chambers GM, Sullivan EA: Assisted Reproductive Technology in Australia and New Zealand 2008. Assisted Reproduction Technology Series: Cat. no. PER 49. 2010, AIHW, Canberra
Wang YA, Chambers GM, Dieng M, Sullivan EA: Assisted Reproductive Technology in Australia and New Zealand 2007. Assisted reproduction technology series: no.13. Cat. no. PER 47. 2009, AIHW, Canberra
Chambers GM, Sullivan EA, Ishihara O, Chapman MG, Adamson GD: The economic impact of assisted reproductive technology: a review of selected developed countries. Fertil Steril. 2009, 91: 2281-2294. 10.1016/j.fertnstert.2009.04.029.
Thompson JM, Irgens LM, Rasmussen S, Daltveit AK: Secular trends in socio-economic status and the implications for preterm birth. Paediatr Perinat Epidemiol. 2006, 20: 182-187. 10.1111/j.1365-3016.2006.00711.x.
Petersen CB, Mortensen LH, Morgen CS, Madsen M, Schnor O, Arntzen A, Gissler M, Cnattingius S, Nybo Andersen AM: Socio-economic inequality in preterm birth: a comparative study of the Nordic countries from 1981 to 2000. Paediatr Perinat Epidemiol. 2009, 23: 66-75. 10.1111/j.1365-3016.2008.00977.x.
Luo ZC, Wilkins R, Kramer MS: Effect of neighbourhood income and maternal education on birth outcomes: a population-based study. CMAJ. 2006, 174: 1415-1420. 10.1503/cmaj.051096.
Shah PS, Balkhair T, Ohlsson A, Beyene J, Scott F, Frick C: Intention to become pregnant and low birth weight and preterm birth: a systematic review. Matern Child Health J. 2011, 15: 205-216. 10.1007/s10995-009-0546-2.
Orr ST, Miller CA, James SA, Babones S: Unintended pregnancy and preterm birth. Paediatr Perinat Epidemiol. 2000, 14: 309-313. 10.1046/j.1365-3016.2000.00289.x.
Barros H, Tavares M, Rodrigues T: Role of prenatal care in preterm birth and low birthweight in Portugal. J Public Health Med. 1996, 18: 321-328. 10.1093/oxfordjournals.pubmed.a024513.
Krueger PM, Scholl TO: Adequacy of prenatal care and pregnancy outcome. J Am Osteopath Assoc. 2000, 100: 485-492.
Vintzileos AM, Ananth CV, Smulian JC, Scorza WE, Knuppel RA: The impact of prenatal care in the United States on preterm births in the presence and absence of antenatal high-risk conditions. Am J Obstet Gynecol. 2002, 187: 1254-1257. 10.1067/mob.2002.127140.
Klemetti R, Gissler M, Hemminki E: Comparison of perinatal health of children born from IVF in Finland in the early and late 1990s. Hum Reprod. 2002, 17: 2192-2198. 10.1093/humrep/17.8.2192.
Wang YA, Healy D, Black D, Sullivan EA: Age-specific success rate for women undertaking their first assisted reproduction technology treatment using their own oocytes in Australia, 2002–2005. Hum Reprod. 2008, 23: 1633-1638. 10.1093/humrep/den135.
Reproductive Technology Accreditation Committee, Code of practice for assisted reproductive technology units. [], [http://www.fertilitysociety.com.au/wp-content/uploads/RTAC-COP-Final-20141.pdf]
Pinborg A, Lidegaard O, Freiesleben N, Andersen AN: Consequences of vanishing twins in IVF/ICSI pregnancies. Hum Reprod. 2005, 20: 2821-2829. 10.1093/humrep/dei142.
Cleary-Goldman J, Malone FD, Vidaver J, Ball RH, Nyberg DA, Comstock CH, Saade GR, Eddleman KA, Klugman S, Dugoff L: Impact of maternal age on obstetric outcome. Obstet Gynecol. 2005, 105: 983-990. 10.1097/01.AOG.0000158118.75532.51.
Hjelmstedt A, Widstrom A, Wramsby HM, Collins A: Patterns of emotional responses to pregnancy, experience of pregnancy and attitudes to parenthood among IVF couples: a longitudinal study. J Psychosom Obstet Gynecol. 2003, 24: 153-162. 10.3109/01674820309039669.
George L, Granath F, Johansson AL, Anneren G, Cnattingius S: Environmental tobacco smoke and risk of spontaneous abortion. Epidemiology. 2006, 17: 500-505. 10.1097/01.ede.0000229984.53726.33.
Shah NR, Bracken MB: A systematic review and meta-analysis of prospective studies on the association between maternal cigarette smoking and preterm delivery. Am J Obstet Gynecol. 2000, 182: 465-472. 10.1016/S0002-9378(00)70240-7.
Wang Y, Chambers G, Dieng M, Sullivan EA: Assisted Reproductive Technology in Australia and New Zealand 2007. 2009, AIHW, Canberra
Wang Y, Chambers G, Sullivan E: Assisted Reproductive Technology in Australia and New Zealand 2008. 2010, AIHW, Canmerra
McManemy J, Cooke E, Amon E, Leet T: Recurrence risk for preterm delivery. Am J Obstet Gynecol. 2007, 196: 571-576. 10.1016/j.ajog.2007.01.039.
Hsieh TT, Chen SF, Shau WY, Hsieh CC, Hsu JJ, Hung TH: The impact of interpregnancy interval and previous preterm birth on the subsequent risk of preterm birth. J Soc Gynecol Investig. 2005, 12: 202-207. 10.1016/j.jsgi.2004.12.004.
Freak-Poli R, Chan A, Tucker G, Street J: Previous abortion and risk of pre-term birth: a population study. J Matern Fetal Neonatal Med. 2009, 22: 1-7. 10.1080/14767050802531813.
Halliday J: Outcomes of IVF conceptions: are they different?. Clin Obstet Gynecol. 2007, 21: 67-81.
Wang JX, Norman RJ, Kristiansson P: The effect of various infertility treatments on the risk of preterm birth. Hum Reprod. 2002, 17: 945-949. 10.1093/humrep/17.4.945.
Acknowledgements
This research is based on data made available by the Australian Institute of Health and Welfare (AIHW). The authors acknowledge the AIHW for funding the NPDC and midwives and neonatal nurses for collecting data for the NPDC.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
XX was involved in the study design, methods investigation, data analysis and preparing the manuscript. YW, ZL, KL and ES were involved in the study design, methods investigation and revision of the manuscript. All authors have contributed to the conducting of this study. The manuscript has been seen and approved by all authors; the order of authorship was agreed by all authors.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Xu, X.K., Wang, Y.A., Li, Z. et al. Risk factors associated with preterm birth among singletons following assisted reproductive technology in Australia 2007–2009–a population-based retrospective study. BMC Pregnancy Childbirth 14, 406 (2014). https://doi.org/10.1186/s12884-014-0406-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-014-0406-y