Abstract
Background
World Health Organization recommended community-based ART (CBART) approaches to improve access to antiretroviral treatment (ART) and treatment outcomes among key populations living with (KPLHIV). Key populations (KP) are female sex workers, men who have sex with men, persons who inject drugs, and transgender people. How CBART for KP (KP-CBART) worked and why, for whom and in what circumstances it worked within KP communities or at community sites, are yet to be described. The aim of this study is to describe the different KP-CBART approaches or models in Nigeria, identifying the context conditions and mechanisms that are likely to produce the desired outcomes.
Method
Building on our previous study eliciting an initial programme theory for KP-CBART, we used a multiple case design and cross-case analysis to evaluate 3 KP-CBART approaches, namely: One Stop Shop clinic; community drop-in centre; and outreach venue. Between 2021 and 2023, we conducted a retrospective cohort study, 99 indepth interviews and 5 focused group discussions with various actors. Using realist evaluation, we synthesised context-mechanism-outcome configurations (CMOCs) and developed programme theory for each of the cases and an overall theory.
Result
The analysis showed the central importance of decentralizing ART service delivery to a safe place within the community for KPLHIV. The provision of ART in a KP friendly environment triggered a feeling of safety and trust in the healthcare workers among KPLHIV, resulting in KP-CBART acceptance and improved ART uptake, medication adherence and retention on ART. KP community engagement in ART delivery, peer support through support group meetings, and linkages with KP-led organizations improved self-efficacy, fostered solidarity and a sense of belonging among KP. These resources encouraged and motivated clients to engage with the KP-CBART model. However, fear of disclosure of HIV and KP status, and lack of trust between KP groups, demotivated and discouraged KPLHIV from initiating ART and continuing their treatment in KP-CBART.
Conclusion
To optimise access to ART and treatment outcomes for KPLHIV, policy makers and health practitioners should ensure the provision of a safe place for ART service delivery that can be trusted by the clients and the KP communities.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
In 2021, seventy percent of new HIV infections reported globally were among KP and their sexual partners [1]. They accounted for 51% of new HIV infections in Sub-Saharan Africa (SSA) and 94% of new infections outside of SSA [1]. KP include sex workers and their clients, men who have sex with men (MSM), persons who inject drugs (PWID), and transgender people (TG). According to the 2022 UNAIDS report, female sex workers (FSW) and transgenders respectively have 30 and 14 times more risk of acquiring HIV compared to other adult women. MSM have a 28 times higher risk compared to adult men while PWID have a 35 times higher risk than adults who do not inject drugs [1]. KP are disproportionately affected by HIV and yet, they are underrepresented in HIV treatment programmes [2]. In Nigeria, antiretroviral treatment (ART) coverage among KP is low when compared to the general population. As of 2021 in the country, ART coverage among adults and children was 90% while ART coverage for FSW, PWID, TG, and MSM was 23.7%, 25%, 19.5%, and 26.3% respectively [1, 3]. Factors accounting for suboptimal access to ART among KP include stigma and discrimination when accessing facility-based services, criminalization, and violence [4, 5].
The World Health Organization recommended the use of differentiated service delivery (DSD) models to improve treatment outcomes among KP [4, 6]. Evidence from studies in Sub-Saharan Africa have shown that involvement of KP communities and organization in service delivery and task shifting of ART refill visits to KP peers improved treatment outcomes. DSD models that facilitate ART delivery within KP communities or at community sites where KP feel safe and comfortable, and models that reduce the frequency of clinical review visits have been advocated for in the literature and guidelines [2, 4, 7, 8].
The KP-CBART programme in Benue State, Nigeria
In Benue State, Nigeria, a community-based ART (CBART) programme was established to serve KPLHIV. CBART for KP (KP-CBART) is a type of differentiated care model that adapts HIV care and treatment services to meet the specific health needs of key populations living with HIV (KPLHIV). Only KP and their sexual partners can access ART through this ART service delivery model. KP-CBART provides tailored ART services to KPLHIV in a safe place within the community without stigma or discrimination, relying on healthcare workers and KP peers for ART services. KP-CBART involves 3 approaches to ART service delivery namely one stop shop clinics (OSS), community drop-in-centres (DIC), and community outreach venues (OV). The full description of the KP-CBART programme can be found in our previous publication about the development of the initial programme theory (IPT) for the programme [9] and under the description of KP-CBART in the result section of this paper. There is limited evidence on the effect of this type of KP-CBART on HIV treatment outcomes in Nigeria. A KP-CBART study in Nasarawa state reported 73.2% ART retention and 88% viral load suppression at 7 months on ART among KP clients [10]. A similar study in community-based HIV clinics in Abuja and Lagos reported that 50.1% of MSM living with HIV initiated ART, 72.3% completed six months and 70.6% of them were virally suppressed [11]. How KP-CBART works for KPLHIV, why, for whom, and in what circumstances has not been studied. Therefore, addressing this knowledge gap is crucial to the understanding of barriers and facilitators of KP-CBART at individual, service delivery, and health system levels.
The realist evaluation methodology
Because the KP-CBART programme is a complex intervention, we adopted the realist evaluation (RE) methodology to appraise the effectiveness of the programme. RE is part of the theory-driven evaluation school [12] that is suitable for complex health interventions. Interventions can be considered complex because of “properties of the intervention itself, such as the number of components involved; the range of behaviours targeted; expertise and skills required by those delivering and receiving the intervention; the number of groups, settings, or levels targeted; or the permitted level of flexibility of the intervention or its components’’ [13]. RE was developed by Pawson and Tilley in 1997 as an evaluation methodology to develop useful knowledge for policy-makers and policy practice. RE develops theories about generative causation and its objective is to go beyond the evaluation of effectiveness of interventions to better understand why a complex intervention will work or not in a specific context.
RE allows researchers to unpack the black box of mechanisms that explain why interventions (programmes or policies) work differently in different settings; for whom it works and under what circumstances it works. In RE theories are presented using a heuristic, the Context-Mechanism-Outcome causal configurations (CMOc), which explains how contextual conditions are interacting with the intervention mechanisms to generate outcomes. Table 1 below defines the key terminology in RE.
In a previous paper, we developed the IPT for the KP-CBART model (Table 2). This was achieved by conducting a scoping review of publications on KP-CBART in SSA, a desk review of programme and policy documents, and key informant interviews with programme managers [9]. The following question guided our research: how, why, for whom, and in what circumstances do community-based ART models of service delivery contribute to observed clinical outcomes (i.e. ART uptake, medication adherence, and retention in care) among key populations?
Study objective
The focus of this current paper is to confirm or refute, and refine the IPT of the KP-CBART in Benue State, Nigeria [9]. Using empirically tested context–mechanism–outcome configurations (CMOc), we will answer practice-oriented questions, such as ‘what works and why?’, what works for whom? ‘in what circumstances, and how?’ We will describe different cases of KP-CBART models and their CMOc, synthesizing findings across cases (cross case analysis), to develop a refined programme theory, identifying the context conditions and mechanisms that are likely to produce the desired outcome(s).
Methods
Study design
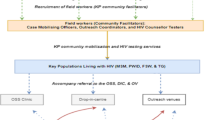
We used a multiple case design and cross-case analysis to confirm or disconfirm and /or modify (refine) the IPT of KP-CBART [16]. The cases are the various KP-CBART approaches which are OSS, DIC and OV (Table 3). Each case involved a mixed method design; the qualitative arm consisted of in-depth interviews and focus group discussions on the contextual factors (including barriers and facilitators) influencing the delivery of CBART. The quantitative arm was a retrospective cohort study of KPLHIV initiated on ART within the community. The analysis, including cross case synthesis, was conducted between January 2022 and April 2023. The overall study flow is shown in Fig. 1 below.
Study flow of the realist evaluation of community-based ART for key populations KP-CBART in Benue State. (IPT-initial programme theory, EMR-electronic medical record, HMIS-health management information system, FSW-female sex worker, MSM-men who have sex with men, PWID-persons who inject drugs, HCW- healthcare worker, SSA-sub-Saharan Africa, KP-CBART- community-based ART for key populations)
Study setting
Benue state has the second highest HIV prevalence in Nigeria with an estimated 184,745 PLHIV and a prevalence of 4.8% among adults (15–64 years), 6.3% among females and 3.5% among males [17]. KP experience the highest burden of HIV in the state. 2020 Integrated Behavioural and Biological Surveillance Surveys (IBBSS) reported a HIV prevalence of 20.2% among FSW, 23.4% among PWID, 21% among MSM and 12.1% among TG [18]. Diagnosis of HIV among KP and linkage to ART is still a challenge in Benue state. Therefore, donor agencies (PEPFAR) and implementing partners (NGOs) partner with the Benue State Ministry of Health, the State Agency for the Control of HIV/AIDS to provide HIV care and treatment services to PLHIV through its various public and private healthcare facilities.
KPLHIV can access ART through the CBART programme or in KP-friendly health facilities in the state. However, due to criminalization, stigma and discrimination, the majority of KPLHIV prefer community-based ART (CBART) service delivery approaches or models to receive HIV care and treatment services. The CBART approach to ART service delivery for KP is the focus of this evaluation and our study sites are located in 6 out of the 23 local government areas (LGA). These LGA are Makurdi, Gboko, Vandekya, Gwer West, and Oturpo. These LGAs have the highest number of KP and are the only ones with CBART structure for KP in the state. Other LGA are reached via HTS and ART outreaches and referral to KP friendly public health facilities.
Study population
Adult KPLHIV that were enrolled and initiated on ART in the KP-CBART programme between January 2016 and December 2019 were eligible for the quantitative study. For the qualitative arm, the study participants comprised of MSM, FSW, and PWID living with HIV, clinical HCWs (ART clinicians, triage nurses, and medical laboratory scientists) and non-clinical HCWs (adherence counsellors, data entry clerks, and KP peer educators, and community mobilizing officers). The majority of the non-clinical staff are working for KP-led or KP-friendly community-based organizations (CBOs).
The quantitative arm of the study, being a retrospective cohort, used an exhaustive sample. All KP clients enrolled on the programme and initiated ART within the study period were included into the study. The large study population size and large number of patients with an adverse treatment outcome (attrition and virological non-suppression, in different analyses) allowed achieving the study aim of estimating factors associated with these adverse outcomes [19]. For the qualitative study, we started with a preliminary sample size, inviting for IDI at least 6 persons per KP group per KP-CBART approach. For FGD we invited a homogenous group of 6–8 persons, including either health workers or KP volunteers working with KP-friendly or KP-led CBOs in Benue State. We then continued recruiting participants until we achieved maximum variation and data saturation.
The cases of KP-CBART examined
Table 3 presents the cases of KP-CBART that were examined in this study. We conducted 3 case studies of KP-CBART, comprising of 3 different service delivery channels, to understand the contextual conditions and generative mechanisms responsible for client outcomes in the programme. The KP-CBART programme is considered a case while the approach/type to KP-CBART implementation is the unit of analysis. Within each case we tested the IPT to obtain a refined programme theory explaining how and why KP-CBART works.
The common focus across the cases is the provision of ART in a safe place for KPLHIV within the community and involvement of KP peers in HIV service delivery. These cases are selected for theory refining in that they provide different contexts from which the programme can be examined in terms of service delivery structure, location, and available human and material resources.
Data collection methods
The qualitative data were collected using in-depth interviews (IDI) and focus group discussions (FGD) guides (Supplementary file). We engaged 2 local research assistants who are familiar with the study settings to facilitate the interviews and discussions. The first author trained the research assistants for a day before the interviews. Research assistants were trained on the use of IDI and FGD guides, and how to conduct qualitative interviews and take informed consents in writing. The first author and the two research assistants conducted all the interviews and group discussions. We purposively selected KP clients receiving ART through KP-CBART and health care providers for IDI and FGD. Study participants were selected based on their experience in the program (since enrolment at least 6 months in HIV care, retained in care, and history of poor or good adherence to ART). A line list of eligible HIV-infected FSW, MSM, and PWID who met the inclusion criteria was generated by the Data Entry Clerks from the electronic medical record (EMR). This line list forms the sampling frame for the study. Study participants were sampled from the line list until data saturation was reached when no new information or theme was gotten from the interviews. We conducted 99 IDI and 5 FGDs. For the IDI, we interviewed 84 beneficiaries, 8 professional HCWs (ART clinicians, Nurses, Medical laboratory scientist, and Pharmacist) and 5 lay HCWs. Lay HCWs are KP volunteers (Peer educators or navigators) working with KP-focussed CSOs. Lay HCWs are trained to mentor and counsel KP clients to adhere to clinical and drug refill appointments. They track clinic defaulters or LTFU clients to return back to treatment.
We also interviewed both lay HCW (working for KP-led CBOs) and professional HCW while we maintained homogenous groups for FGDs. We conducted 2 FGDs with professional HCWs and 3 FGDs with KP community volunteers. There was no FGD with the beneficiaries The selection of study participants aimed at ensuring optimal representation of stakeholders (beneficiaries and service providers) and interviewing participants with diverse knowledge and lived experiences of KP-CBART. Interviews were held at the service delivery points (OSS, DIC, and OV) and in the offices of KP-led CBO. KP peers and other community facilitators working for the KP-led CBOs assisted with the selection and invitation of KP clients for interviews. The location for interview was decided in consultation with the clients, KP-led CBOs, and HCWs. We ensured that all locations were safe for KP with assurance of privacy and confidentiality. Each interview and group discussion lasted between 30 – 50 min. Table 4 below showed the number of study partipants who participated in the IDI and FGD.
For the quantitative study, we extracted client-level data from the electronic medical records and health medical records available in the facilities. The study population are KPLHIV who initiated ART in the KP-CBART programme between January 1, 2016 and December 31, 2019 and followed up until January 31, 2021 in Benue State Nigeria. Data extracted include demographic information, clinical and laboratory profiles, and treatment outcomes. The detailed description of the quantitative study method is has been published in an open access journal: https://doi.org/https://doi.org/10.1371/journal.pone.0260557
Data analysis and synthesis
We adopted the confirmatory theory building approach to analyse the cases and to refine the programme theory [16, 20]. First of all, we conducted a mixed method study of the three KP-CBART cases, synthesised CMOCs and developed programme theory for each of the cases using a retroductive (form of reasoning). Retroductive inferencing within a realist evaluation refers to a logic in which outcomes are considered to follow from the alignment of a specific combination of attributes or elements of the realist heuristic tool [16, 21].
After obtaining the programme theories from the cases, the conjectured CMOCs from each of the cases were compared and contrasted to develop an overall programme theory. We applied the process of analytical generalisation across the cases to refine the PT. Figure 2 shows the processes of the analytical generalization to refine programme theory [16]. Analytical techniques such as retroduction (mechanism centred theorising), analytical generalisation and concretization of the theorized mechanisms were used for the data analysis [16, 20]. Using these analytic techniques allow us to move from the specificics of individual cases to a theory that is more abstract.
In-case analysis
For each of the cases, a retrospective cohort study and a qualitative study were done. We conducted a quantitative study to determine the clinical outcomes and associated factors among KP enrolled in KP-CBART. We determined retention on ART and viral load suppression, per KP group and KP-CBART case. Variables that were extracted from EMR included demographic data (age, sex, education, occupation, residence), clinical variables (HIV status, date of HIV diagnosis, linkage to care, ART status, WHO stage, tuberculosis (TB) status, viral load suppression) and treatment outcomes (lost-to-follow up (LTFU), dead, transferred out, active in care). Baseline characteristics were summarised and stratified by KP-CBART approach. Proportions were calculated for categorical variables while medians and interquartile ranges were calculated for continuous variables. We determined retention on ART and viral load suppression, per KP group and KP-CBART case. Attrition referred to those who died or were LTFU. LTFU was defined as no clinical contact or drug refill from any of the KP-CBART approaches for more than 28 days since the last expected contact. Retention in care on ART was defined as the proportion of patients that are active in care and on ART, among those who commenced ART and those transferred out to another HIV programme or facility. Virological non-suppression was defined as having a last viral load higher than 1000 copies/mL. Cox regression and logistic regression were used to assess the risk factors for attrition and virological non-suppression respectively. Survival analysis was used to assess retention on ART [19]. Kaplan–Meier techniques were employed to estimate retention by KP-CBART approach and the Log-rank test was used to estimate the differences in Kaplan–Meier curves between subgroups’’ [19]. The full description of the quantitative study and findings can be found in https://doi.org/https://doi.org/10.1371/journal.pone.0260557
For the qualitative study, we explored the perspectives of the stakeholders concerning the implementation of KP-CBART, the barriers, facilitators, and recommendations. Audio recordings were transcribed verbatim and we verified data accuracy and completeness by reading the interview transcripts multiple times. For study respondents who could not understand or speak English, we conducted interviews and FGD in their local languages (TIV and Idoma) or ‘’pidgin English’’ with them. The topic guides were translated by the trained data assistants (native speakers) and to ensure correct translation, we also asked indigenous HCWs to confirm the correctness of the translation. The data assistants also transcribed the audio recordings and translation of the audio recordings (in verbatim) into the English language. The interview transcripts were imported into Nvivo software for coding. Primary content analysis was used to identify the overarching patterns emerging from the data. Use of retroductive reasoning based on the CMOs identified during the elicitation/development of the KP-CBART IPT. We used the qualitative study to complement and explain the quantitative findings.
Cross-case analysis
The objective of the cross-case analysis was to refine the programme theories obtained from all the KP-CBART cases while the objective of the within-case analysis was to contrast the cases, developing causal configurational patterns per case in depth and in a way ‘contrasting CMOs’ [16]. Using within case analysis, we charted the key contextual factors for each of the cases, and the generative mechanisms that explained the outcomes. Then through an iterative process and discussion with research participants and team, we charted common CMO patterns across the cases and developed the refined programme theory.
Comparing CMOc from all cases and from the initial programme theory provided evidence to confirm or disconfirm CMOCs and to refine the programme theory. To compare and contrast cases, we identified active mechanisms and their related outcomes (M–O links), then we search for the context in which the M–O link was contingent [16]. CMOCs with negative outcomes from the cases were used to confirm or disconfirm CMOC chains in the IPT. We identified the association between negative or failed outcomes between the ‘’missing mechanisms’’ and negative ‘contexts’. The negative CMOs reinforces the construction of positive ones[16].
Findings
The findings from this study are presented in three parts. The first part summarises the quantitative findings and presents the CMOc and programme theory for each of the cases. The second part presents the refined programme theory while the third part explains the mechanisms that are common to all the KP-CBART cases and their key enabling and constraining factors.
Case studies of KP CBART
Findings from the quantitative study [19]
Between January 2016 and December 2019, 3495 KPLHIV were initiated on ART in KP-CBART. An estimated 51.8% (n = 1812) of these clients were enrolled in OSS, 28.1% (n = 982) in DIC, and 20.1% (n = 701) through the outreach venues. The majority of participants were FSW—54.2% (n = 1896) while 15.8% (n = 551), 29.8% (n = 1040), and 0.2% (n = 8) were PWID, MSM, and TG respectively [19].
Overall, retention in care was 63.5%, 55.4%, 51.2%, and 46.7% at 1 year, 2 years, 3 years, and 4 years on ART (Table 5). Out of 1650 clients with attrition, 41 (2.5%) were reported as having died, while 97.5% (n = 1609) were LTFU [19]. Supplementary file 2 include tables that show the characteristcs of KPLHIV enrolled into the KP-CBART and predictors of attrition and viral load suppression [19].
Mutivariate analysis showed that KP-CBART approach did not predict attrition among KPLHIV initiated on ART in the programme (supplementary file 2), having adjusted for other factors such as age, sex, place of residence, year of ART enrolment, WHO clinical stage, type of KP group, and KP-CBART approach. MSM were at a higher risk of attrition (vs FSW; adjusted hazard ratio (aHR) 1.27; 95%CI: 1.14 – 1.42). Of 3495 patients, 48.4% (n = 1691) had a viral load (VL) test. Of those, 97.8% (n = 1654) were virally suppressed.
Virological coverage and non-suppression
Out of 3495 eligible patients for a VL test, only 48.4% (n = 1691) had a VL test done (Table 6). Of 1691 with a VL test result, 97.8% (n = 1654) had a viral load < 1000 copies/mL.
In the multivariate logistic regression model (supplementary file 2_table 2.2), we adjusted for sex, place of residence, duration on ART, WHO Stage at ART enrolment, KP group type, and KP-CBART approach [19]. Virological non-suppression was associated with WHO Stage II (adjusted odds ratio (aOR) 3.76, 95%CI: 1.45 – 9.75) compared to WHO stage I [19]. The type of KP population group and the KP-CBART approach were not associated with virological non-suppression [19] ( supplementary file 2_table 2.3).
Qualitative findings
Because retention rates were low in the KP-CBART, we asked study participants for their views and perspectives on the barriers and facilitators of linkage to ART and retention on ART in the KP-CBART. Several factors were identified as the cause of sub-optimal retention on ART within the KP-CBART compared to facility-based ART for the general population. From the client and HCW perspective, Table 7 presents the barriers and facilitators of retention on ART across the different cases of KP-CBART.
-
A
Case Study 1: One Stop Shop (OSS) clinic
The OSS clinic is a community-based ART centre established for KPLHIV. This community ART centre is designed only for KP individuals. Since establishment, the programme has initiated 3495 KPLHIV on ART in 3 different centres in the state. The 3 ART centres are located in Makurdi, Gboko, and Oturpo towns in Benue state. These centres are located in the capitals of their local government areas (sub-national unit), and at the outskirts of the residential neighbourhood where the majority of the city population lives. The OSS is hidden from the public because there are no sign posts or boards or any form of publicity to notify or inform the general public about the place. The OSS is fully equipped with medical and laboratory equipment (such as rapid test kits, sphygmanometer, stethoscope, weighing machine, examination couch, first aid box, ARV and other drugs, centrifuge) and recreational facilities (such as table tennis, ludo game, and cards). The OSS is the most preferred CBART model among KP because of the warm ambiance and friendly atmosphere for social interaction and ART service delivery. Majority of the study participants perceived OSS to be a KP-friendly environment, free of stigma and discrimination. Table 8 presents the CMOc obtained from the OSS in Benue state.
Healthcare professionals, such as doctors, nurse case managers, medical laboratory scientists, and a pharmacist provide HIV testing and treatment at the OSS. Other members of staff are lay HCWs, consisting of adherence counsellors/peer educators, data clerks and a receptionist. The OSS also has a mobile health team (or community ART team) which conducts ART outreach to serve locations without a KP-specific facility. On ART outreach days, clients’ waiting time may be prolonged depending on the inflow of clients and the number of staff available at the OSS. The staff of OSS usually liaise with lay HCW working for KP-led CBOs to ensure linkage of KPLHIV to ART and retention on ART. The majority of the CBO staff are members of KP and they are responsible for community-based outreach HIV testing and linkage to the OSS clinic, DIC, OV and other facility-based care. Their roles as volunteer lay health workers include community mobilisation, HIV testing, linkage to ART, client tracking for retention, organization of support group meetings, and referral to other services.
Porgramme theory for One Stop Shop In urban setting IF ART service delivery is conducted in a safe place for KPLHIV, within a friendly and non-stigmatizing environment with flexible consultation and/or ART refill appointments triggering a sense of safety and trust among clients, including recreation options enabling bonding, and there is provision of peer education/support through clients’ participation in support group meetings and linkages with KP-led organizations will bring about a sense of belonging, bonding, and increased self-efficacy; KP community engagement as lay HCWs ensures meaningful participation of KP in ART service delivery; and clients’ satisfaction and motivation from availability of quality and comprehensive HIV services; and capacity building/continuous technical support to empower HCW to provide quality KP friendly HIV services to KPLHIV. THEN the uptake of ART, medication adherence and retention on ART among KPLHIV in the model will improve BECAUSE KPLHIV will develop trust for HCWs and the programme, and will be empowered (self-efficacy), and motivated to engage with HIV care through the OSS HOWEVER, fear of HIV status and KP status disclosure, and lack of trust between KP groups through the OSS, will demotivate and discourage KPLIV from engaging and continuing their ART care |
-
B
Case Study 2: Community Drop in Centres
DIC are safe places, like mini-OSS, where KPLHIV can access their ART within the community. Benue state has two functional DIC located in Vandekya (Vandekya town) and Gwer East LGA (Aliade town). Both DIC were analysed in this case study.
The DIC do not have their own medical officer (ART clinician) but rely on the mobile health team and community health extension workers (CHEW) for clinical care. These facilities are led by CHEW and lay HCWs. With the support of the outreach team CHEW initiate KPLHIV on ART, refill ARV and collect samples for VL. The lay HCWs from the KP-led CBOs specifically provide adherence support to clients and ensure retention in care. Similar to the OSS, DIC offer comprehensive HIV services such as HIV-testing services, medication adherence counselling, condom distribution, ART initiation, ART refill and referral if needed. Unlike the OSS, there are no recreational facilities to draw KP for social engagement and linkage to HIV services. Table 9 presents the CMOc obtained from the DIC in Benue state.
One of the challenges confronting the DIC is that HCWs only provide ART services three days in a week and client visits are based on appointment. Another challenge is the issue of the openness of the DIC and inadequate privacy because DIC are located within an office space in a PHC setting (the one in Vandekya) or an abandoned hotel (in Aliade town) for its operation/activities. Moreover, support group meetings are organized infrequently for KPLHIV by the KP-led CBOs.
Programme theory for Drop in centre (In semi-urban areas) IF ART service delivery is decentralised to a primary healthcare setting or a building (i.e. a rented hall or an old hotel) that offers a safe, friendly and non-stigmatizing environment to KPLHIV and served by low-cadre HCWs (i.e. community health extension workers and lay HCWs) thereby enabling a sense of safety and trust among clients; and there is provision of peer education/support through clients’ participation in support group meetings and linkages with KP-led organizations will bring about a sense of belonging, bonding, and increased self-efficacy; KP community engagement as lay HCWs ensures meaningful participation of KP in ART service delivery; and clients’ satisfaction and motivation from availability of quality and comprehensive HIV services; and capacity building/continuous technical support to empower HCW to provide quality KP friendly HIV services to KPLHIV. THEN the uptake of ART, medication adherence and retention on ART among KPLHIV in the model will improve BECAUSE KPLHIV will develop trust for HCWs and the programme, and will be empowered (self-efficacy), and motivated to engage with HIV care through the model HOWEVER, if there is no timely client-bases access, lack of privacy and inadequate peer support then ART uptake, medication adherence, and retention will be sub-optimal because clients are dissatisfied, demotivated and discouraged from engaging with and remaining in HIV care |
-
III.
Case Study 3: Community Outreach Venue
The case study consists of two community outreach venues in Ushongo and Korinya towns. OVs are places within the town where ART is provided to KPLHIV. The OVs are served by the mobile health teams from the OSS. Ushongo and Korinyo OVs are served by the mHealth teams from the Makurdi OSS and Gboko OSS teams respectively. Both venues are public spaces, a room within an oldtown hall. HIV services such as HIV testing services, ART initiation and refill are offered to KPLHIV through this model of ART delivery. Other services offered to KP include viral load monitoring, referral for AHD and STI treatment, condoms distribution, support group meetings, PrEP, etc.
A mobile health team visits the outreach venues at least once in a month for ART initiation and/or refill. At times, the visit is organized once per month or per quarter to refill ART for PLHIV enrolled at the venue. Although this model brings ART closer to where people live, there is no flexibility in scheduling of visits and appointments. Clients cannot seek care for emerging health concerns in between consultations/visits to the OVs. The OV model relies on community facilitators (lay HCWs) to mobilise KP for ART refill at the OV. These community facilitators (CF) are engaged by KP-led/KP-friendly CBOs to provide HIV testing services, linkage to ART and other services, and client tracking to minimise IIT/LTFU. The majority of these CF are KP and they were trained by CSOs and APIN (implementing partner) to provide HIV services.
Table 10 presents the CMO configurations for community outreach venues. The community OV provides the opportunity for KPLHIV to receive ART where they live and at no travel cost. The convenience of receiving ART, cost savings (transportation cost), the technical competence of HCWs, and short waiting time are some of the factors motivating KP clients to enroll in the venue and be retained in care.
For OV locations that are very far from the OSS, clients expressed dissatisfaction with the quality of service delivery due to occasional late arrival of cART teams resulting in a long waiting time and short time for consultation. Clients also complained of lack of adequate privacy during service delivery because these locations are perceived to be open and other people (clients) can hear and observe proceedings at the venue.
Programme theory for Community outreach venue (In a rural or setting where there are no OSS or DIC) IF ART service delivery is conducted in an outreach venue or a place that is safe, friendly and non-stigmatizing to KPLHIV and clients are served by a mobile health team or a community ART team (comprising of a medical doctor, adherence counsellor, medical laboratory scientist, and pharmacist) who provide ART initiation and refill (and other services) and thus improving access by bringing ART or HIV services closer to where clients live and enabling psychological safety, motivation, and trust; provision of peer education/support through support group meetings and linkages with KP-led organization will bring about a sense of belonging, bonding, and increased self-efficacy; KP community engagement as lay HCWs ensures meaningful participation of KP in ART service delivery; and capacity building/continuous technical support to empower HCW to provide quality KP friendly HIV services to KPLHIV. THEN the uptake of ART, medication adherence and retention on ART among KPLHIV in the model will improve BECAUSE clients buy into the model and trust the community ART team to provide quality HIV services, also they feel safe, empowered, and motivated to engage and remain in HIV care/model HOWEVER, if there is no timely client-oriented / client-centric access (long waiting time, infrequent visits, inadequate/short consultation time) and lack of privacy during service delivery (because of the open space- a hall) then ART uptake, retention-in care, and medication adherence are going to be sup-optimal because clients are dissatisfied and demotivated from engaging with and remaining in HIV care |
The refined programme theory/ overall PT
Relying on analytical generalization and retroductive theorizing [16, 20]. CMOc from each of the cases were synthesised and summarised through cross-case analysis into a framework for KP-CBART (a refined theory) as shown in Figs. 3, 4, and 5 below. This refined theory explains how the KP-CBART model resulted in outcomes across the three cases. The findings from the case studies and cross synthesis confirmed the hypothesised CMOc and programme at the beginning of this theory. KP-CBART maybe more effective when it is designed and implemented for a specific KP-group.
To explain how and why the KP-CBART works, as shown in Figs. 3 and 4, we used retroductive theorizing and teased out the macro and meso context conditions into which the KP-CBART intervention was introduced, the actors, the mechanisms, and the outcomes. Then we explained how the actors perceived, interacted, and responded to the various components or interventiol modalities of the KP-CBART intervention through their reasoning (mechanisms). The actors’ response and reasoning generated the intended outcomes of the CBART intervention.
KP friendly services are provided through the three KP-CBART and services are comprehensive to include HIV prevention and treatment services. KP perceived the environment of service delivery in the three cases to be safe and free of stigma. Across the cases, KP peers support KP community mobilisation and facilitated service delivery through KP-led CBOS and support group meetings. Capacity buiding and technical support for staff are similar across cases and guidance documents are available. However, cases differ in terms of geographic access, cadre and number of staff, opening time, service delivery venue, flexibility of ART delivery (i.e. outreach venues), and availability of recreational space to socialise with peers. Across all the cases, clients felt safe and trusted the healthcare workers with their care/ART. Also, KP individuals were encouraged and motivated to engage with and remain in the model and adhere to their drugs. Through peer support, KP individual assumed greater responsibility for own health with improved self-efficacy.
We refined the programme theory for the KP-CBART as follows:
Refined programme theory • IF ART service delivery (ART initiation and refill) to a specific KP group (MSM or FSW or PWID) is organized in a safe place within a specific location in the community, together with meaningful involvement of the KP community in service delivery, provision of quality and comprehensive HIV services, training of HCW and law enforcement agents on KP sensitization, and advocacy to policy makers THEN access to antiretroviral treatment, utilisation of services, and retention-in-care among KPLHIV will improve BECAUSE of enhanced clients’ trust and feeling of safety in the programme. Resulting in better health outcomes and well-being for KP because they (KPLHIV) are encouraged and motivated to engage and remain in care. • IF ART service delivery, including ART initiation and/or refill, is organized in a safe and comfortable place for KP group(s) with HIV and within a specific location in the community, but there is no adequate privacy and confidentiality, minimal or no flexibility in appointment scheduling (difficulty accessing HCWs before and after appointments), long waiting time, and insufficient time for consultation, THEN ART uptake, medication adherence, and retention on ART will be sub-optimal BECAUSE KP clients are dissatisfied with the quality of services received and demotivated to engage and continue their HIV treatment. • IF KP community and lay health workers are involved in the design, planning, and implementation of ART service delivery (e.g. assisted referral (escort referral) for ART, medication adherence, ART refill, client tracing and etc), THEN KP clients will be encouraged to engage in KP-CBART BECAUSE they trust the healthcare providers and perceive HIV services to be KP-friendly and thus, resulting in sustained engagement of KPLHIV in HIV care and clinical outcomes (i.e. medication adherence and retention in care). |
Key mechanisms of the KP-CBART
In this section, we will explain the key mechanisms of the KP-CBART: we first describe the mechanisms, summarize its components in a table (the enablers and barriers) and then illustrate with citations from the IDI/FGD. Bringing the different components of the different KP-CBART cases together, we identified 4 key or prominent mechanisms that dominate other mechanisms and occur more frequently (i.e. partial or demi-regularities) through the process of abstraction and accentuation [14, 22]. These key mechanisms are privacy and confidentiality, trust, motivation, buy-in, and self-efficacy. We used these mechanisms to construct the configurational map or framework for KP-CBART (Figs. 3, 4 and 5) which explains the overall PT.
Mechanism one: privacy and confidentiality
Privacy and confidentiality is one of the key mechanisms that accounts for optimal engagement in HIV care and treatment among KPLHIV within the KP-CBART. We view privacy and confidentiality as the foundational element for building trust in the KP-CBART and it has a ripple effect on the development of other CMOCs [23]. It is the commitment to privacy and the development of trust that motivate KPLHIV to engage with the model and remain in HIV care. All the respondents prefered a ART service delivery point or a model that ensures optimal privacy and confidentiality. The level of privacy obtainable in a service delivery point and whether service delivery is KP-friendly or not, will determine the level of confidence KPLHIV will have in the KP-CBART and their openness to discuss personal and health issues with HCWs. The community outreach venue is somewhat open and offers less privacy compared to the DIC and OSS. Activities (i.e. clients consultation and drug refill) happening at the OV can be observed by other KP clients waiting for their turn to be attended to service and by curious pasers-by. Privacy is better at the DIC because consulation offices are located within a primary health care centre or an enclosed space in an old hotel. The OSS offers the best in terms of privacy and confidentiality as it is located at the outskirt of the community and it is hidden from the general public. There is no signpost or signboard indicating location of service delivery. Those living in the neighbouring houses or passers-by are not aware of clients’ visit or the purpose of their visit to the OSS.
Many of the respondents identified the fear of accidental disclosure of sexual orientation and HIV status through the KP-CBART as a threat and barrier to their linkage and retention on ART.
PWID receiving ART through OSS: - ‘’ …This OSS assures you of confidentiality… like take a look at this place …it's not everybody that knows what’s going on in this place…. it doesn't look like a hospital or a clinic. It looks more like an apartment…yeah, somebody’s home, …so they (KP clients) can assess care or treatment and their confidentiality will still be assured… will still be guaranteed to a very great extent. I think it's a lot of motivation, it's a great motivation’’ (IDI).
FSW receiving ART at the DIC: - I think like me…when I tested positive, I felt somehow because if these men find out that I am HIV positive they may not want to patronise me until…but when I came here and discovered that it is hidden and people will not find out what I come here to do… that put me at ease…. So….. I think other Ashawo (sex workers) are not coming to this place because they do not know what to expect ……. feel that way… but when they come, I am sure they will continue coming because some of them don't want people to know what they are doing’’ (IDI)
Mechanism two: enhanced trust and psychological safety
The level of trust KPLHIV have in the HCWs and the KP-CBART is one of the key mechanisms that influences clients’ decision to enrol in HIV care, initiate, adhere, and remain on ART. Nigeria government, including the Benue state government, criminalised homosexuality in 2014 by way of the Same Sex Marriage (Prohibition) Act, 2013 with a potential penalty of 14 years imprisonment and criminalization of sex work (Nigeria criminal/penal code). Therefore, it is key that KPLHIV are assured that they are safe and that the program is not a bait to lure them out for arrest and prosecution. As such, the provision of ART in a safe place, that is free of harassment from and arrest by law enforcement agents generated a feeling of safety and trust in the HCWs and the KP-CBART. A safe place is also free of stigma and discrimination from HCWs and other clients. Thus a safe place encouraged KPLHIV to accept and use the KP-CBART, initate and refill ART, and remain in care and achieve viral suppression.
The majority of the MSM and a number of PWID expressed dissatisfaction with the idea of receiving ART in the same place with individuals belonging to another KP group, and non-KP clients (i.e. sexual partners of KP). MSM respondents complained of cases of backbiting and discriminationfrom FSW and PWID. On the other hand, the majority of the FSW are comfortable with the PWIDS, and vice versa, because of the opportunity for friendship (dating) and transactional sex (exchange of drugs for sex). Table 11 presents factors that can enable (generate) or disable trust in the KP-CBART.
Generally, KPLHIV perceived the OSS, DIC, and OV as a safe place for drug delivery and HIV care. One of the clients interviewed commented that:
MSM from the OSS:- “When we talk about confidentiality, how to keep the secret of the clients here in OSS, these people (HCWs) are trained and they understand that they have to keep clients’ secret …..that's why we have that courage to come out. for example If you hear that a nurse working in the OSS tell someone that: “.. Hmm look… even this married man fucks nyash o (anal sex)….” immediately I hear of such,… that OSS is getting close(black listed) and I will not go there again’’….. but, I have never heard of such and that’s why I am still going to the OSS…. because of the confidentiality and the trust I have in them’’. Indepth interview
MSM from MSM-led CBO: - ‘’…I will also suggest and…. advise that it will be better if we have our own OSS as MSM- do you understand that? You know that there is a level to which I will open up to you if I know you are from my community (KP group) than I will open up to somebody I know is just a worker and is not a member of my community. But if we have our own OSS, and we know that our own people (KPs) are working here, we are comfortable telling you anything, opening up everything to you. So I will also suggest that it will be really nice if we have our own OSS’’. Focus group discussion
MSM from MSM-led CBO: - ‘’The male doctors too… they are not MSM …so they are also homophobic. Whether you are a male or female if you are not a MSM you are homophobic- yes, because you are a homophobic person, you cannot attend to an MSM because you feel….. you know….some of them feel irritated, it irritates them that you are coming …that you are going to fuck nyash (anus). So in fact MSM are facing issues’’. Focus group discussion
Mechanism three: motivation and encouragement
The majority of the KPLHIV confirmed that KP-CBART encouraged and motivated them to engage in HIV care and treatment. Study respondents identified both intrinsic or extrinsic motivational factors that are at play within the model. Intrinsic motivators include privacy and confidentiality, easy and convient access to ART, and the formation of group identity and mutual support and solidarity while extrinsic motivators are conducive and safe environment for ART delivery free health services, availability of recreational facilities, incentives such as condoms and lubricants, transport reimbursement, etc.
Disabling and enablers of motivation in the KP-CBART are captured in Table 12 below.
In a nutshell, KP-CBART being client -centered means that ART delivery is tailored to the needs of the clients, e.g. the delivery of ART is close to where clients live, there is ART drug refill by proxy, multi-month dispensing, etc. All these serve to motivate KP clients to engage in HIV care.
The citation below is about the utmost importance of privacy / confidentiality.
FSW at the outreach venue:- ‘’ I told you earlier that this place is very conducive, not everyone that has this virus wants someone to know that I'm coming to collect drugs. This is a place, a hall, of which they all know the use over twenty years, this hall is in a very secret place, it is open but no one can just walk in. First of all, when they come for support group we have a security that will stand at the gate despite the fact that this place is covered, ….not everybody is allowed… if you come with your card and they see that your card is there… you can come inside’’. Indepth interview
The following citation is about difficulty in accessing ART through the OV and importance of drug refill by proxy in bridging this gap:
MSM, lay HCW at the OV:- ‘’Yes, because you know, normally they give appointments …time for refill like in xyz, ….they do come once in a month and that is becoming an issue to other MSM member because you cannot expect everybody to be available on that appointment or particular day. So that, ….make many people miss their appointment but if you can, if you can have people that maybe will take drugs and be giving it to them that is by proxy …giving to these people their drusgs --house to house… like we normally we used to do ….before …that will help a lot because you know many people do have activities sometimes and that make them to miss their appointment. So if they miss their appointment for them to go to the OSS in towns become a problem for them’’. Indepth interview
Mechanism four: buy in
Stakeholders collaboration with KP-led CBOs and meaningful participation of KP in service delivery encouraged clients to buy into the model of HIV service delivery and to engage with the treatment programme. This collaboration also facilitated trust and feeling of safety among KP. The engagement of KP-led and KP-friendly CBOs provide opportunities to KP to have a say in issues or matters that affect them and it also provides employment opportunities to KPLHIV. For instance, volunteer lay HCWs receive stipends from the program to cover the cost of transport and phone calls). KP peers are recruited and trained to mobilise KPLHIV for HIV testing services and VL testing, link clients to ART through assisted referral/escort services, ART refill, and clients tracking to minimise LTFU. KP peer educators provide one-on-one adherence counselling to their peers and coordinate the community support group meetings. Although the roles of KP network/association and KP peer educators in the planning and evaluation of community-led monitoring activities and KP-CBART are ill-defined. The KP-led CBOs engaged community facilitators (KP peers) to provide peer counselling and treatment support to their peers. Factors that enabled or disabled stakeholders to buy into KP-CBART are as shown in Table 13.
The following citation demonstrates the distrust between MSM and FSW or PWIDs:
MSM at the OSS: ‘’Is actually a bad experience, because bringing these three KP categories into one environment is like bringing ….should I say when two elephant fight the bush suffers that is how it is because you see that… MSM and PWID though… they are sometimes together because some MSM also inject drugs, but they are not together,…. it's not too easy for MSM and PWID and also FSW to be in one environment because if they go outside they are still going to… some of them may still disclose another’s HIV status, because a PWID can get married but a MSM cannot easily get married. And again, should a PWID know a MSM's relative…. They can expose your sexuality or they can make your HIV status known. So it's not too easy to bring these kind of people together……if it is only MSM, purely MSM facility, it is better than bringing all of us together’’ Indepth interview
Mechanism five: self-efficacy
Peer support through participation in the community support group meetings provide an opportunity for KP individuals to bond and identify with the group. During the support group meetings, participants encouraged one another, and shared their coping strategies. Sessions on important skills, such as tailoring and soap making trainings, are routinely organized for group members by the KP-led CBOs. This type of continuous support and encouragement from peers has the potential to build the confidence of KP individuals and their self-efficacy.
Also capacity building for the healthcare workers (clinical and non-clinical HCWs) in the form of trainings on HIV/AIDS management, sensitization about KPLHIV, technical assistance to HCWs, and provision of guidelines and SOPs have increased staff confidence and technical competence in the delivery of quality HIV services/ART to KPLHIV. Law enforcement agents were sensitized through a training on key populations and provision of KP friendly health services. Those working in the local government areas or towns where KP-CBART is located were prioritized for training.
Factors that enabled or disabled the mechanism of self-efficacy are as shown in Table 14. Disabling factors included inadequate support for support group (SG) meetings, infrequent SG meetings, prioritizing naïve PLHIV for SG meetings (i.e. a situation whereby newly enrolled PLHIV are supported to attend the support group meetings more frequently than the old clients).
The following citations demonstrate peer support and solidarity in KP-CBART:
MSM at Outreeach venue :- ‘’One…..if I come to pick my drugs in xyz here and I don't have transport money , when I come they will pay for my transport back. And two, because this support group meeting when I come we talk about our drugs, they teach us how to take drugs, how to feel happy when you're taking those drugs, and I open up being an MSM, and I open up to my fellow members we talk and we know each others, ….so I'm happy coming to xyz to take my drugs’’ Indepth interview
MSM at the OSS : - ‘’The benefits, …..well talking about the benefits I will start from when I said the support group. ..It was very beneficial…. you understand? it was very beneficial because a lot of people when you come when you hear encouragement apart from the testimonies, you hear one or two persons standing up to tell you how they started how you understand, be telling you things about themselves that will motivate you and besides they are still giving you encouraging words so when you hear all those things it used go a long way to encourage you’’ Indepth interview
Discussion
This paper presents a refined programme theory based on evidence from the initial programme theory and three cases of the KP-CBART intervention in Nigeria. We described the dynamics between the contextual factors and the mechanisms that promote linkage to ART, medication adherence, and retention in care for KPLHIV within the community-based ART intervention for KP. Findings show that the provision of ART in a KP friendly environment will trigger a feeling of safety and trust in KPLHIV for healthcare workers, resulting in KP-CBART acceptance and improved ART uptake, medication adherence, and retention on ART. KP community engagement in ART delivery, peer support through support group meetings, and linkages with KP-led organizations will improve self-efficacy, foster solidarity, and a sense of belonging among KP. These resources will encourage and motivate clients to engage with the KP-CBART model. However, fear of disclosure of HIV and KP status, and lack of trust between KP groups, can demotivate and discourage KPLHIV from initiating ART and continuing their treatment in KP-CBART.
Findings from our study and similar studies in low and middle income countries show that in a setting where sex work, drug use, and homosexuality are prohibited or criminalised, members of KP find it difficult to access ART and achieve optimal treatment outcomes [9, 24, 25]. Many of these studies show sub-optimal performance for ART uptake or linkage to ART, retention in care, and viral load suppression when compared to the UNAIDS 95–95-95 target, or when compared to HIV programme outcomes in the general population [24, 26,27,28]. Based on these studies, we can infer that the current KP-CBART models are not sufficient to engage and retain KP clients on ART and achieve optimal viral load suppression. This calls for further differentiation of KP-CBART to improve both individual client and programme outcomes. In line with our findings in Nigeria, long-term retention in KP-CBART is high in Ivory Coast, impacting negatively on health outcomes and well-being [19, 29]. Across studies, we observed sub-optimal viral load coverage but good viral load suppression when compared to other vulnerable groups, such as children and adolescents [19, 29], meaning that viral load suppression is optimal among KP clients who were retained on ART in KP-CBART.
Having all the different KP groups receive ART in the same service delivery point and ART model could explain the low retention rates observed among KP enrolled in KP-CBART. The MSM group reported experiences of harassment from both FSW and PWID while a number of PWID expressed dissatisfaction with the model arrangement. To overcome this challenge, the national HIV programme may need to consider ART service delivery models for each KP group. A prospective cohort study in Nigeria, that initiated only MSM with HIV on ART in a community-based clinic, reported a retention rate of 72.3% at 6 months, while two studies on KP-specific CBART for FSW in Tanzania reported retention rates of 100% and 81.3% at 6 month and 18 months of ART initiation respectively [27, 30]. However, the feasibility of such a KP-specific service delivery will depend on the availability of resources and programme priorities.
We identified a common theme of confidentiality between our study and another study, a realist review, that explains when, why, and how implementation of ART adherence intervention work [31]. Evidence from this study show that PLHIV are more likely to enrol in interventions that protect their confidentiality and that foster trust between program beneficiaries and service providers. From patients’ perspectives, important skills to gain patient’s trust are technical ability, verbal communication skills and respect of patient's autonomy by the physician [32]. Therefore, the quality of HCWs engaged to provide ART outreach can boost the client’s confidence in KP-CBART and encourage them to access HIV care and treatment. Other factors that enable a feeling of safety and trust within the KP-CBART are collaboration with KP-led CBOs and involvement of KP community in ART service delivery. We note that privacy for KP clients at the DIC and OV is sub-optimal and requires improvement, especially in hostile and rural communities. These service delivery centres leverage a space within a primary health care clinic or a community town hall to provide ART services. Some of these service centres are open and will benefit from a change of location and facility re-design. We recommend the use of office environment of KP-led CBOs to serve as DIC or treatment centres for group-specific KP- ART service delivery model instead of townhalls and rooms in primary health care settings.
There is need to strengthen KP-CBART to increase access of KPLHIV to ART. All the 3 KP-CBART approaches should be prioritized and scaled up to all the local government areas (sub-national units) in the state. The choice of KP-CBART approaches to implement will depend on the specific health needs of the KP, size estimates and HIV prevalence in each of the LGA. The 3 different KP-CBART approaches are complementary and can remove or limit individual barriers to access and availability of ART. Designing a CBART model for each of the KP group is the most preferred approach—however, considering the resources required to set up CBART for KP, especially OSS, it may not be realistic to implement KP-specific CBART models for KP. Study participants recommended appointment blocking by KP group or a specific day during the week for consultation/ART refill per KP-group.
To ensure KP-CBART ownership and sustainability, there was KP-community engagement through collaboration with KP-led CBOs and KP networks. Community engagement is defined as a process of collaborative work with groups of people affiliated by geographic proximity, interest, or health issue, to address social and health challenges affecting those people [15, 33]. Within KP-CBART, KP individuals are recruited and trained to provide tailored ART services to their peers. They mobilise their peers for HIV testing services, link HIV positive KP to effective ART, and ART refill. Using this approach ensures meaningful participation of KP community in HIV service delivery.
From a realist perspective, community engagement can build trust and social relationships [15, 23]. Where community members can provide feedback and voice their concerns, and have these acknowledged and responded to, they may feel valued and respected and this may contribute to the establishment of trust. Also, respectful interaction and responsiveness to participants needs can trigger the mechanisms of trust, which increases motivation to participate [15].
Limitations, rigour, and trustworthiness
Selection bias was evident in the quantitative analysis of the KP-CBART and in the recruitment and sampling of study participants for the qualitative interviews and FGD. KP-led CBOs and staff of KP-CBART recommended study participants for interviews and group discussions. Although we purposively selected study participants with either good or bad record of retention on ART in the programme. Refusal rates were difficult to estimate and were not reported. For the retrospective cohort study, there was selection bias because of incomplete and missing data.
Evidence for theory testing and refinement was derived from a KP-CBART programme in one of the six geopolitical regions in Nigeria. These regions have their contextual differences and similarities. Therefore, our study should be interpreted with caution in terms of generalisation of findings. However, the identified mechanisms in the refined programme theory may be transferrable to similar settings (i.e. punitive laws against homosexuality and sex work, and weak health systems) in Nigeria and Sub-Saharan Africa.
A key strength of this RE is the mixed approach to theory development. The evaluation incorporates analysis of patient-level data, and multiple views and perspectives of stakeholders to provide deeper insight into the KP-CBART intervention. The case studies and cross-case helped to explore the different contextual factors and causal mechanisms of the KP-CBART. Mechanisms were clearly articulated by identifying the different enabling or disabling mechanisms in the KP-CBART intervention.
The refinement of this theory requires maximum variation of study participants to capture varied perspectives and lived experiences of the various actors interacting with the programme. We selected and interviewed participants from the different KP groups, KP-led CBOs, and KP-CBART approaches in Benue state. Some of the interviews were conducted in the local language for participants who cannot speak English. We read the transcripts of interviews multiple times to understand the responses before data coding. Also, we checked with selected study participants for feedback on the generated programme theories.
Recommendations and conclusion
Health needs of KP individuals and KP groups are different in Nigeria. Each KP group (FSW, MSM, PWID, and TG) has its own identity, health and psychological needs. Therefore to strengthen the KP-CBART, interventions should be adapted to meet specific KP group and individual client needs. Where feasible, a KP-CBART intervention per KP group type should be implemented. For KPLHIV who belong to two or more KP groups (i.e. MSM or FSW who inject or use drugs), little is known about their shared risks and health needs. Therefore, future research should explore the intersection of vulnerabilities for these individuals and how best to deliver HIV services to them.
To further strengthen the KP-CBART intervention, we recommend implementation research that includes a cycle of community approaches, process evaluation, and evidence-informed adaptation to ART service delivery using realist evaluation in Nigeria and other SSA countries. This will encourage cumulation of knowledge (theory-building) as described by Pawson and Tilley [14], and future development of a middle range theory for KP-CBART. Middle range theory are theories that are close to the actual observations and it is applicable across different settings or contexts.
For effective implementation of CBART for KP and optimal treatment outcomes (linkage to ART, medication adherence, retention on ART, and viral load suppression), there is need for KP-community participation in service delivery. Buy-in of the intervention by the KP-led community based organizations and networks are key to program ownership and sustainability. Also, policy makers and practitioners should ensure the provision of a safe place for ART service delivery that can be trusted by KP community, maintain privacy and confidentiality for clients, and build the capacity of healthcare workers and KP clients to achieve self-efficacy in the design and implementation of HIV programmes for KPLHIV.
Availability of data and materials
The dataset underlying the results and conclusions of this article are available as part of the article and supplementary file. If additional information is required, the raw data supporting the results of this study are available from the corresponding author on reasonable request.
Abbreviations
- ART:
-
Antiretroviral treatment or antiretroviral therapy
- CBART model:
-
Community-based antiretroviral therapy delivery model
- CMOc:
-
Context-mechanism-outcome configuration
- DIC:
-
Community drop in centre
- FSW:
-
Female sex workers
- IBBSS:
-
Integrated Behavioural and Biological Surveillance Surveys
- IPT:
-
Initial programme theory
- KP:
-
Key populations
- KP-CBART:
-
Community-based ART model of service delivery for key populations or CBART for key populations
- KPLHIV:
-
Key populations living with HIV
- MSM:
-
Men who have sex with men
- NAIIS:
-
National HIV/AIDS Indicator Survey
- OSS:
-
One Stop Shop
- OV:
-
ART outreach venue
- PLHIV:
-
People living with HIV
- PWID:
-
Persons who inject drugs
- TG:
-
Transgender people
References
Global HIV & AIDS statistics — Fact sheet | UNAIDS. Available from: https://www.unaids.org/en/resources/fact-sheet. Cited 2023 May 20.
Treatment | Differentiated service delivery. Available from: https://www.differentiatedservicedelivery.org/models/treatment/. Cited 2023 May 20.
UNAIDS. AIDSinfo | UNAIDS. Available from: https://aidsinfo.unaids.org/. Cited 2020 May 15.
WHO. Consolidated guidelines on HIV prevention, diagnosis, treatment and care for key populations. 2016. Available from: www.who.int. Cited 2019 Apr 27.
The GlobalFund. Key Populations - The Global Fund to Fight AIDS, Tuberculosis and Malaria. 2019. Available from: https://www.theglobalfund.org/en/key-populations/. Cited 2020 Apr 20.
Consolidated guidelines on HIV prevention, testing, treatment, service delivery and monitoring: recommendations for a public health approach. Available from: https://www.who.int/publications/i/item/9789240031593. Cited 2021 Aug 20.
Macdonald V, Verster A, Baggaley R. A call for differentiated approaches to delivering HIV services to key populations. J Int AIDS Soc. 2017;20(Suppl 4):28–31. Available from: https://doi.org/10.7448/IAS.20.5.21658. Cited 2019 Apr 22.
Ibiloye O, Akande P, Plang J, Emerenini F, Omole T, Osindero O, et al. Community health worker-led ART delivery improved scheduled antiretroviral drug refill among men who have sex with men in Lagos State. Nigeria Int Health. 2021;13(2):196–8. Available from: https://academic.oup.com/inthealth/article/13/2/196/5849427. Cited 2023 Jun 5.
Ibiloye O, Decroo T, van Olmen J, Masquillier C, Okonkwo P, Lynen L, et al. Initial programme theory for community-based ART delivery for key populations in Benue State, Nigeria: a realist evaluation study. BMC Public Heal. 2023;23(1):1–25. Available from: https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-023-15774-w. Cited 2023 May 16.
Ibiloye O, Decroo T, Eyona N, Eze P, Agada P. Characteristics and early clinical outcomes of key populations attending comprehensive community-based HIV care: Experiences from Nasarawa State, Nigeria Mugo. PM, editor. PLoS One. 2018;13(12):e0209477 http://www.ncbi.nlm.nih.gov/pubmed/30571744.
Ramadhani HO, Ndembi N, Nowak RG, Ononaku U, Gwamna J, Orazulike I, et al. Individual and Network Factors Associated With HIV Care Continuum Outcomes Among Nigerian MSM Accessing Health Care Services. J Acquir Immune Defic Syndr. 2018;79(1):e7-16. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29781881. Cited 2018 Nov 3.
Chen HT, Rossi PH. The theory-driven approach to validity. Eval Program Plann. 1987;10(1):95–103.
Craig P, Dieppe P, Macintyre S, Mitchie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ. 2008;337(7676):979–83 https://www.bmj.com/content/337/bmj.a1655.
Pawson R, Tilley N. Realistic evaluation. 1997. p. 235.
Adhikari B, Vincent R, Wong G, Duddy C, Richardson E, Lavery JV, et al. A realist review of community engagement with health research. Wellcome Open Res. 2019;4:87. Available from: https://pubmed.ncbi.nlm.nih.gov/31289754/. Cited 2023 May 20.
Mukumbang FC, Marchal B, Van Belle S, Van Wyk B. Unearthing how, why, for whom and under what health system conditions the antiretroviral treatment adherence club intervention in South Africa works: A realist theory refining approach. BMC Health Serv Res. 2018;18(1):1–15. Available from: https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-018-3150-6. Cited 2022 Jul 30.
NAIIS. Nigeria HIV/AIDS Indicator and Impact Survey. 2019. Available from: https://www.naiis.ng/resource/factsheet/NAIIS/PA/NATIONAL/FACTSHEET/FINAL.pdf. Cited 2019 Apr 27.
IBBSS 2020 – Wacphd. Available from: https://wacphd.org/projects/ibbss-2020/. Cited 2022 Jul 11.
Ibiloye O, Jwanle P, Masquillier C, Van Belle S, Jaachi E, Amoo O, et al. Long-term retention and predictors of attrition for key populations receiving antiretroviral treatment through community-based ART in Benue State Nigeria: A retrospective cohort study. PLoS One. 2021;16(11):e0260557. Available from: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0260557. Cited 2022 Apr 5.
Eastwood JG, Jalaludin BB, Kemp LA. Realist explanatory theory building method for social epidemiology: a protocol for a mixed method multilevel study of neighbourhood context and postnatal depression. Springerplus. 2014;3(1):12. Available from: https://doi.org/10.1186/2193-1801-3-12.
Mukumbang FC, Kabongo EM, Eastwood JG. Examining the Application of Retroductive Theorizing in Realist-Informed Studies. Int J Qual Methods. 2021;20:16. Available from: https://doi.org/10.1177/16094069211053516.
Gilmore B, McAuliffe E, Power J, Vallières F. Data Analysis and Synthesis Within a Realist Evaluation: Toward More Transparent Methodological Approaches: https://doi.org/10.1177/1609406919859754. 2019;18. Available from: https://journals.sagepub.com/doi/full/10.1177/1609406919859754. Cited 2022 Sep 5.
Jagosh J, Bush PL, Salsberg J, Macaulay AC, Greenhalgh T, Wong G, et al. A realist evaluation of community-based participatory research: partnership synergy, trust building and related ripple effects. BMC Public Health. 2015;15(1):725. Available from: https://doi.org/10.1186/s12889-015-1949-1.
Tenni B, Carpenter J, Thomson N. Arresting HIV: Fostering Partnerships between Sex Workers and Police to Reduce HIV Risk and Promote Professionalization within Policing Institutions: A Realist Review. PLoS ONE. 2015;10(10): e0134900.
Chang J, Shelly S, Busz M, Stoicescu C, Iryawan AR, Madybaeva D, et al. Peer driven or driven peers? A rapid review of peer involvement of people who use drugs in HIV and harm reduction services in low- and middle-income countries. Harm Reduct J. 2021;18(1). Available from: /pmc/articles/PMC7857348/. Cited 2024 Jun 15.
Cowan FM, Davey CB, Fearon E, Mushati P, Dirawo J, Cambiano V, et al. The HIV Care Cascade Among Female Sex Workers in Zimbabwe: Results of a Population-Based Survey From the Sisters Antiretroviral Therapy Programme for Prevention of HIV, an Integrated Response (SAPPH-IRe) Trial. J Acquir Immune Defic Syndr. 2017;74(4):375–82.
Tun W, Apicella L, Casalini C, Bikaru D, Mbita G, Jeremiah K, et al. Community-Based Antiretroviral Therapy (ART) Delivery for Female Sex Workers in Tanzania: 6-Month ART Initiation and Adherence. AIDS Behav. 2019;23(Suppl 2):142–52.
Olawore O, Astatke H, Lillie T, Persaud N, Lyons C, Kamali D, et al. Peer Recruitment Strategies for Female Sex Workers Not Engaged in HIV Prevention and Treatment Services in Cote d’Ivoire: Program Data Analysis. JMIR PUBLIC Heal Surveill. 2020;6(4):93–104 Available from: /pmc/articles/PMC7563635/.Cited 2021 Oct 6.
Vuylsteke B, Semdé G, Auld AF, Sabatier J, Kouakou J, Ettiègne-Traoré V, et al. Retention and risk factors for loss to follow-up of female and male sex workers on antiretroviral treatment in Ivory Coast: a retrospective cohort analysis. J Acquir Immune Defic Syndr. 2015;68:S99-106. Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00126334-201503011-00005. Cited 2017 Jun 6
Kerrigan D, Mbwambo J, Likindikoki S, Davis W, Mantsios A, Beckham SW, et al. Project Shikamana: Community Empowerment-Based Combination HIV Prevention Significantly Impacts HIV Incidence and Care Continuum Outcomes among Female Sex Workers in Iringa. Tanzania J Acquir Immune Defic Syndr. 2019;82(2):141–8.
Leeman J, Chang YK, Lee EJ, Voils CI, Crandell J, Sandelowski M. Implementation of antiretroviral therapy adherence interventions: a realist synthesis of evidence. J Adv Nurs. 2010;66(9):1915–30. https://doi.org/10.1111/j.1365-2648.2010.05360.x.
Hamelin ND, Nikolis A, Armano J, Harris PG, Brutus JP. Evaluation of factors influencing confidence and trust in the patient-physician relationship: A survey of patient in a hand clinic. Chir Main. 2012;31(2):83–90.
Clinical and Translational Science Awards: Foundations for Accelerated Discovery and Efficient Translation: Progress Report 2009–2011 — Principles of Community Engagement (Second Edition).Available from: https://ncats.nih.gov/ctsa_2011/ch5_v2.html. Cited 2023 May 20.
Acknowledgements
The authors would like to thank the respondents of the in-depth interview and focus group discussions, and the APIN Public Health Initiatives for providing the enabling environment for this study.
Funding
The first Author (OI) received a PhD scholarship grant from the Institute of Tropical Medicine, Antwerp supported by the Belgian Directorate General for Development (DGD). The funder had no role in the conceptualisation, study design, data collection, analysis, data interpretation, and in the writing of the manuscript.
Author information
Authors and Affiliations
Contributions
O.I., S.VB., and T.D. conceptualized the study. O.I., S.VB., C.M., and T.D. developed the interview guide. O.I., T.D., and S.VB. conducted data analysis, interpretation of data, writing, and review of the main manuscript. PO, JVO, TD, PJ, LL, and SVB supervised the study and reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was performed in accordance with the Declaration of Helsinki. The study was approved by the Institutional Research Board of APIN Public Health Initiatives (IRB022-FR), Benue State Ministry of Health and Human Services (MOH/STA/204/VOL1/154), and the Institute of Tropical Medicine Antwerp (1503/21). Written informed consent was obtained from all participants in the study. All data sources (coded voice recordings and transcripts) were de-identified and held in strict confidentiality by the researchers. Deidentification/coding occurred prior to audiorecording and immediately after informed consent was taken. Pseudonyms were used to identify study participants and audio files were deleted after validation of the pseudonymised transcription.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ibiloye, O., Decroo, T., Masquillier, C. et al. Realist evaluation of a community-based antiretroviral therapy (CBART) programme for key populations in Benue State in Nigeria. BMC Infect Dis 24, 892 (2024). https://doi.org/10.1186/s12879-024-09808-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09808-w