Abstract
Objective
To analyze the epidemic characteristics of common respiratory tract infection pathogens in children with respiratory tract infection, and provide scientific basis for the prevention and control of respiratory tract infection.
Methods
A retrospective collection of clinical data was conducted on 11,538 children with respiratory tract infections at Luoyang Maternal and Child Health Hospital from December 2022 to November 2023. The types of respiratory tract infections, including upper and lower respiratory tract infections, as well as five respiratory pathogens: influenza A virus (influenza A), influenza B virus (influenza B virus, adenovirus (ADV), respiratory syncytial virus (RSV), and Mycoplasma pneumoniae (MP) infections, were analyzed and compared for different genders, ages, temperatures, and air quality in different months; And the changes of five pathogens in children with respiratory tract infections of different disease severity.
Results
From December 2022 to November 2023, a total of 11,538 children with respiratory infections were included in the analysis, including 6436 males and 5102 females, with an age of 4.92 ± 2.03 years. The proportion of upper respiratory tract infections is as high as 72.17%, and lower respiratory tract infections account for 27.83%. Among them, 2387 were positive for Flu A antigen, with a positive rate of 20.69%, 51 cases were positive for Flu B antigen, and the positive rate was 0.4%, 1296 cases were positive for adv antigen, with a positive rate of 11.23%, 868 cases were positive for RSV antigen, with a positive rate of 7.52%, 2481 cases were positive for MP IgM antibody or MP antigen, and the positive rate was 21.50%. Flu B in male children The infection rate of ADV and MP was higher than that of female children (p < 0.05); Among children in different age groups, the older the age, the older the Flu A The higher the infection rate of MP (p < 0.05), the higher the positive rate of RSV in children with younger age (p < 0.05). The positive rate of ADV in children aged 3–6 years and > 6 years was higher than that in children aged 0–3 years (p < 0.05); Flu A and MP are popular throughout the year, and the positive rate peaks during the period of temperature rise and air quality decline from February to March, and during the period of temperature drop and air quality index rise from August to November, The positive rate of RSV peaked after the turning point of temperature rise from March to April. The infection rate was higher during the period of sharp decline in air quality from March to May and sharp decline in temperature in November, The positive rate of ADV was higher at the turning point of temperature rise from February to March, and then the infection rate decreased. During the period of sharp temperature drop from August to November, the positive rate increased sharply, and the peak of infection occurred; As the disease worsens, The positive rates of Flu A, Flu B, RSV, MP and combined infection with more than two pathogens were all increased (p < 0.05).
Conclusion
After the new coronavirus epidemic in 2022, Flu A and MP have the highest infection rate of respiratory pathogens in children, showing a peak growth in general, with epidemic characteristics changing with environmental temperature, air quality and seasons. The main disease type is upper respiratory tract infection, MP and adv infections were mainly in male children, Flu A, MP and ADV infections are more common in older children, RSV infection was more common in younger children; Flu A, Flu B, RSV and MP infection and the co infection of more than two pathogens may more easily lead to the occurrence of severe pneumonia.
Similar content being viewed by others
Introduction
Acute respiratory infection (ARI) can be divided into upper respiratory tract infections and lower respiratory tract infections based on the site of infection. Upper respiratory tract infections include the common cold, acute pharyngitis, laryngitis, acute tonsillitis, and other related conditions, while lower respiratory tract infections include acute pneumonia and bronchitis [1, 2].ARI is mostly caused by influenza A virus (Flu A), influenza B virus (Flu B), adenovirus (ADV), Mycoplasma pneumoniae (MP), and other pathogens that enter the human nasal cavity, throat, tonsils, and other parts, leading to inflammation. This can result in symptoms such as fever, throat discomfort, hoarseness, cough, expectoration, and others [3]. Some patients may also experience severe symptoms such as shortness of breath, chest pain, and hemoptysis, which can pose a serious threat to their health [4]. According to World Health Organization data, millions of children die each year due to complications caused by respiratory diseases, particularly in developing countries [5]. The trend of respiratory pathogens in children in China has changed before and after the pandemic. In early 2023, with the adjustment and appropriate relaxation of national epidemic prevention policies, multiple outbreaks of respiratory pathogens occurred in various regions [6]. There are also differences in the types and epidemic characteristics of pathogens across different areas and medical institutions [7, 8]. In this study, five common respiratory pathogens were detected in children with respiratory tract infections treated at Luoyang Maternal and Child Health Hospital from December 2022 to November 2023. The aim was to analyze the relevant epidemiological characteristics and provide a scientific basis for the prevention and treatment of respiratory tract infections in children in this region. This study holds significant value for doctors and public health departments in formulating more effective prevention strategies, optimizing resource allocation, and protecting children’s health.
Subjects and methods
Objective
A total of 11,538 children with respiratory tract infections admitted to Luoyang Maternal and Child Health Hospital from December 2022 to November 2023 were selected as the study subjects. The main symptoms included cough, sore throat, headache, fever, dyspnea, and other respiratory tract infection symptoms. Among them, 6,436 were male and 5,102 were female, with an average age of 5.93 ± 1.82 years (range, 0–16 years). The types of diseases included acute tonsillitis, acute laryngitis, acute angina, bronchopneumonia, acute tracheitis, community-acquired pneumonia, lobar pneumonia, and others.
Inclusion criteria
The diagnosis of respiratory tract infection meets the relevant standards outlined in Zhu Futang Practical Pediatrics (8th Edition).
The diagnosis of children in the severe pneumonia group met the diagnostic criteria for severe cases as per the Guidelines for the Diagnosis and Treatment of Mycoplasma Pneumoniae Pneumonia in Children (2023 Edition). The criteria include meeting any of the following conditions:
-
Continuous high fever (above 39 °C) for ≥ 5 days or fever for ≥ 7 days with no downward trend in peak temperature.
-
Presence of one or more of the following symptoms: wheezing, shortness of breath, dyspnea, chest pain, or hemoptysis.
-
Occurrence of extrapulmonary complications that do not meet the criteria for critical illness.
-
Pulse oxygen saturation ≤ 0.93 at rest while breathing room air.
-
Imaging findings of any of the following:
-
.Involvement of a single lobe ≥ 2/3 with uniform high-density consolidation, or two or more lobes with high-density consolidation (regardless of the size of the involved area), potentially accompanied by moderate to massive pleural effusion or localized bronchiolitis.
-
Diffuse or bilateral bronchiolitis involving ≥ 4/5 of lobes in one lung, possibly complicated by bronchitis and mucus plug formation leading to atelectasis.
-
Clinical symptoms that gradually worsen, with imaging showing lesion progression of more than 50% within 24–48 h.
-
Significant elevation of one or more of the following: C-reactive protein (CRP), lactate dehydrogenase (LDH), or D-dimer.
-
Exclusion criteria
-
Combined immunodeficiency disease.
-
Congenital organ dysfunction or hematopoietic dysfunction.
-
Patients with other infectious diseases who have been taking hormones, immunosuppressive drugs, or other medications in the past 7 days.
-
Patients with incomplete clinical data.
-
This study was approved by the medical ethics committee of the hospital.
Method
Data collection
The medical records of the children were retrieved through the hospital’s LIS system. General data, including gender, age, clinical symptoms, disease types, and laboratory test results from the respiratory tract panel, were collected. Positive results were defined as positive findings from the respiratory tract panel’s antigen (antibody) or nucleic acid tests.
Testing procedures
The five joint tests for respiratory tract infections included detection of the following: Flu A antigen, Flu B antigen, RSV antigen, ADV antigen, MP antigen, or MP IgM antibody. Upon admission, throat swabs from the patient’s posterior pharyngeal wall, tonsil crypts, lateral walls, and other areas were collected before medication and immediately sent for inspection.
The respiratory tract pentaplex test was performed using the colloidal gold method to detect antigens. The reagent used was a kit produced by Hangzhou Innovative Biological Detection and Control Technology Co., Ltd. For detecting IgM antibodies against Mycoplasma pneumoniae in children’s serum, the passive gel method was employed. Three milliliters of venous blood were drawn within 1–7 days after the onset of the disease, and the serum was collected by centrifugation (3500 rpm, 10 min). The detection was performed using a kit produced by Wantai Biopharmaceutical Co., Ltd.
Reverse transcription polymerase chain reaction (RT-PCR) was used to detect the nucleic acids of the five pathogens in the respiratory tract. The nucleic acid detection kit used was produced by Da’an Gene Co., Ltd. of Sun Yat-sen University, with a test result of > 1 × 103 copies/ml indicating a positive result.
Statistical analysis
SPSS 25.0 statistical software was used for data analysis. The number of cases (n) and percentages (%) of the categorical data were reported. The Chi-square test was employed for comparing rates, with a p-value of < 0.05 considered statistically significant.
Results
Detection of respiratory pathogens using a five-joint test in children with respiratory tract infections from December 2022 to November 2023 revealed that among 11,538 children, Flu A and Mycoplasma pneumoniae (MP) were the pathogens with the highest detection rates, with positive rates exceeding 20% (see Table 1).
Among all enrolled children, upper respiratory tract infections, which include diseases with acute inflammation of the nasal cavity, pharynx, or throat (such as tonsillitis, acute laryngitis, rhinitis, herpetic angina, and bacterial pharyngotonsillitis), were identified in 8,324 cases, accounting for 72.17%. Lower respiratory tract infections, involving the trachea, bronchus, and lungs (including acute tracheitis, pneumonia, and bronchopneumonia), were identified in 3,214 cases, accounting for 27.86%. The clinical diagnoses of all enrolled patients are shown in Table 2.
Among all enrolled children with respiratory tract infections, there were 5,102 females (44.22%) and 6,436 males (55.78%). The infection rates of Flu B, ADV, and MP were higher in males compared to females. There was no statistically significant difference in the infection rates of Flu A and RSV between the two groups, as shown in Table 3.
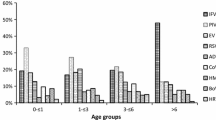
A comparison of the positive rates of five pathogens across different age groups revealed the following: Older children had a higher infection rate of Flu A and Mycoplasma pneumoniae (MP), while younger children had a higher positive rate of RSV. The positive rate of ADV was higher in the 3–6 year old and > 6 year old groups compared to the 0–3 year old group, but there was no significant difference between the 3–6 year old and > 6 year old groups. There was no significant difference in the positive rate of Flu B across different age groups (see Table 4).
Temperature and air quality changes in the region across different months affected the infection rates of five respiratory pathogens
Flu A and Mycoplasma pneumoniae (MP) were prevalent throughout the year, with positive rates peaking from February to March, when temperatures rise and air quality declines, and again from August to November, when temperatures decrease and the air quality index increases.
RSV had its highest positive rate after the temperature began to rise from March to April. The infection rate was notably higher during periods of sharp air quality decline from March to May and a sharp temperature drop in November.
ADV showed a higher positive rate at the temperature rise turning point from February to March, followed by a decrease in infection rate. During the sharp temperature drop from August to November, the positive rate sharply increased, reaching its peak.
These trends are illustrated in Fig. 1.
Infection of five respiratory pathogens by disease severity
There were 8,324 cases of upper respiratory tract infections, accounting for 72.14%, including acute suppurative tonsillitis, tonsillitis, acute laryngitis, and acute angina. There were 2,611 cases of non-severe pneumonia, accounting for 22.63%, and 603 cases of severe pneumonia, accounting for 5.22%.
As the severity of the disease increased, the positive rates of Flu A, Flu B, RSV, MP, and infections involving more than two pathogens also increased. The infection rate of ADV was highest in children with upper respiratory tract infections, with no significant difference compared to the severe pneumonia group (see Table 5).
Discussion
Acute respiratory infection (ARI) is a major health problem worldwide, with respiratory viruses being the primary source of infection. Common causes of ARI include rapid onset, low immune function, exposure to infectious sources, and environmental factors [9,10,11].Acute upper respiratory tract infections are typically characterized by mild disease and a short course, with a generally good prognosis for patients. In contrast, acute lower respiratory tract infections present with more severe symptoms. Without timely treatment, these infections can progress, especially in children, potentially leading to serious complications such as respiratory failure [12, 13]. Furthermore, ARI patients with infections from multiple pathogens are more likely to experience symptoms such as cough, sore throat, shortness of breath, and dyspnea compared to those with a single pathogen infection. Therefore, implementing targeted prevention and control strategies based on the epidemic characteristics of pathogens is essential for effective disease management.
The results of this study indicated that from December 2022 to November 2023, five types of respiratory pathogens were prevalent among children. Upper respiratory tract infections were the most common, with tonsillitis being the most frequent type. Flu A and Mycoplasma pneumoniae (MP) had the highest infection rates among the pathogens. Additionally, Flu B, ADV, and MP had higher infection rates in males compared to females [14]. Among different age groups, children older than 6 years had the highest infection rates of Flu A and MP, while the positive rate of RSV was highest in children aged 0–3 years. These findings are consistent with studies from other regions, where RSV is predominantly prevalent among younger children [15]. In contrast, Flu A and MP were primarily found in older children in this study, which aligns with results from neighboring areas. This may be due to the school environment, which facilitates the spread of pathogens among this age group. However, the study observed a predominance of infections in males, which differs from other studies and may be attributed to sample selection bias [16].
Different respiratory pathogens exhibit varying epidemiological patterns, typically showing seasonal epidemic characteristics influenced by factors such as environmental temperature, humidity, and air quality. This study, which began monitoring respiratory pathogen infections after the release of the national epidemic prevention policy in January 2023, found that the prevalence of Flu A, Mycoplasma pneumoniae (MP), ADV, and RSV increased significantly [6].
The positive rates for these pathogens peaked with rising temperatures in spring from March to April, remained high during the summer, but declined as air quality decreased. Specifically:
-
The positive rate of Flu A increased from 0.7% in December 2022 to 42.32% in March 2023, then decreased to 6.75% by July.
-
The positive rate of RSV rose from 0.28% in December 2022 to 39.34% in April 2023, and then fell to 1.72% by July.
-
The positive rate of ADV increased from 0.28% in December to 8.77% in March, decreased to 2.79% in June, but rose again to 23.88% in November.
-
Flu B remained prevalent at low levels throughout the study period, with Flu A and MP being the main prevalent pathogens.
Previous studies have indicated that RSV is prevalent from March to June in the Southern Hemisphere and from September to December in the Northern Hemisphere. This study observed that RSV was mainly prevalent from March to May in the Northern Hemisphere, suggesting an earlier prevalence than usual for the year following the epidemic [17,18,19]. After an initial peak in infection from March to April, ADV showed a high-level epidemic state from August to November. Flu A and MP exhibited continuous prevalence across all four seasons, with further outbreaks in spring and winter. ADV not only showed an early epidemic trend but also had a notable epidemic period in winter [20]. Comparative analysis of respiratory pathogen detection data before and after the COVID-19 epidemic reveals significant differences in trends, reflecting changes in epidemic characteristics. These findings provide valuable insights for the prevention and treatment of respiratory infectious diseases in children in this region.
In this study, the infection rates among three groups of children—those with upper respiratory tract infections, non-severe pneumonia, and severe pneumonia—were compared. The results showed a progressive increase in infection rates, with co-infection of two or more pathogens being most prevalent among children with severe pneumonia, reaching 63.68%. This indicates that a larger scope of infection and more severe pneumonia are associated with higher pathogen infection rates. Co-infection can severely impair immune function, leading to immune imbalance and extrapulmonary complications, which are highly detrimental to children [21]. Additionally, in clinical practice, bacterial and viral infections, as well as mixed infections, can present with similar symptoms of acute respiratory tract infection in children, making them difficult to distinguish. This often leads to empirical antibiotic use, particularly in infants. However, the misuse of antibiotics can drive pathogen variation and contribute to immune escape. Therefore, it is crucial to enhance pathogen detection capabilities, ensure early diagnosis and treatment, avoid antibiotic overuse, and prevent the occurrence of multiple infections and severe pneumonia [22].
Additionally, during the COVID-19 epidemic, the response to national epidemic prevention policies involved non-pharmacological interventions (NPIs), such as home isolation, reduced population contact, and prolonged mask-wearing [23]. These measures may have led to “immune debt”, potentially affecting children negatively once the pandemic is under control [24]. During the epidemic, some parents avoided hospital visits due to fear of infection, delaying treatment for other conditions. This delay could weaken children’s immune systems and contribute to immune debt. Furthermore, NPIs reduced exposure to viruses and bacteria, leading to less immune stimulation and training. This decrease in immune training and antibody levels increases children’s susceptibility to infections, making them more prone to diseases [25].Immune debt may partly explain the recent outbreaks of respiratory pathogens, such as Flu A, Flu B, ADV, and RSV, in children. Moreover, after the epidemic, previously prevalent viruses might exhibit new variants, posing additional challenges. This variation can decrease population immunity, potentially causing a resurgence in pediatric respiratory infections, which might contribute to multiple infections and severe pneumonia [26]. The decline in vaccination coverage and the potential rise in vaccine-preventable disease cases highlight the need for strengthened supplementary vaccination efforts by epidemic prevention departments [12]. Mathematical models suggest that the impact of immune debt could lead to more severe RSV and flu epidemics in the coming years. The results of this study align with this prediction, emphasizing the need to consider immune debt in post-epidemic disease prevention and control strategies [27]. Therefore, it is crucial to maintain personal protection measures and enhance immunity through vaccination and other preventive strategies.
To summarize, this study found that infection rates for various respiratory pathogens in children showed distinct epidemic characteristics after the epidemic. Upper respiratory tract infections were the most common, and co-infection with multiple pathogens increased the likelihood of developing severe pneumonia. Flu A, Mycoplasma pneumoniae (MP), ADV, and RSV exhibited high infection rates, with Flu A and MP showing a tendency to affect older age groups. These pathogens demonstrated seasonal epidemic patterns, with trends of advancing or delaying the epidemic period.
Preventive and protective measures are essential for infants and children of all ages, particularly those older than 3 years. Vaccination can help reduce infections and lower the risk of severe illness and death.
This study has some limitations. Due to the high outpatient workload and staff shortages during the epidemic outbreak season, the colloidal gold method was used for rapid screening of some respiratory pathogens. However, since the principle and sensitivity of the colloidal gold method differ from those of the PCR method, this may have led to missed detections [28]. Future research should address this limitation by optimizing the screening methods and conducting studies with a larger sample size and multiple centers.
Availability of data and materials
All data generated or analyzed during this study are included in this article.
Abbreviations
- Flu A:
-
Influenza A virus
- Flu B:
-
Influenza B virus
- ADV:
-
Adenovirus
- RSV:
-
Respiratory syncytial virus
- MP:
-
Mycoplasma pneumoniae
References
Ma H, Song YM. Analysis of factors associated with nosocomial-acquired lower respiratory tract infection complicating acute myeloid leukemia in induced remission. Chin J Pract Med. 2018;45(15):93–5. China.
Liu L, Ling J, Zhao F. Pathogenetic characterization of Mycoplasma pneumoniae and Chlamydia pneumoniae in children with acute respiratory tract infections. Chin J Pathog Biol. 2017;12(2):174–7, 181. China.
Chatzis O, Darbre S, Pasquier J, et al. Burden of severe RSV disease among immunocompromised children and adults: a 10 year retrospective study. BMC Infect Dis. 2018;18(1):111.
Zhou B. Analysis of serum IgM antibody detection of 8 respiratory pathogens in children with acute respiratory tract infection. J Clin Pulmonol. 2017;22(1):132–4. China.
Wang DY, Eccles R, Bell J, Chua AH, Salvi S. Management of acute upper respiratory tract infection: the role of early intervention. Expert Rev Respir Med. 2021;15(12):1517–23.
Notice on Printing and Distributing the Prevention and Control Plan for novel coronavirus Infection (Tenth Edition). Bulletin of the National Health Commission of the People's Republic of China, 2023, (01): 8–11.
Mok LY, Zhang JW. Analysis of respiratory viruses in hospitalized children with acute respiratory infections before and after the new coronary pneumonia epidemic. Zhejiang Clin Medi. 2023;25(9):1369–71. China.
LIANG Yimin, GU Yiwen, YE Zhonglv. Analysis of 9 respiratory pathogens in 11333 children with acute respiratory tract infection in Meizhou. Journal of Guangdong Medical University. 2022;40(2):198–201.China.
Ma Hui, Shen Yongming, Si Ping, et al. Analysis of IgM antibody detection of nine respiratory pathogens in children with acute respiratory tract infection and its correlation with air pollution. Chinese Journal of Immunology. 2018;34 (4): 576 -582.China.
KONG De-chuan, WU Huan-yu, ZHENG Ya-xu, et al. Epidemiologic and aetiologic characterization of acute respiratory tract infection cases among adults in Shanghai, 2015–2017. Chinese Journal of Epidemiology. 2019;40(8):904 -910.China.
Zhang Y, Wu S, Zhu J. Distribution of pathogenic bacteria and analysis of drug sensitivity test in pediatric acute respiratory tract infections. Chinese Journal of Practical Medicine. 2022;49(18):27 -30.China.
Ren X, Wang Z. Differential diagnostic value of white blood cell count C-reactive protein and calcitoninogen test for acute upper respiratory tract infection in children. China Drugs and Clinics. 2019;19(2):309 -310.China.
WEN Ya, HUANG Juan, DU Yanjia, et al. Study on the value of ring-mediated isothermal amplification technology in detecting pathogenic bacteria in 397 cases of chronic obstructive pulmonary disease with lower respiratory tract infection. Anhui Medicine. 2022;26(9 ): 1760 -1766.China.
CHEN Yunying, YE Xianfei, ZHOU Jun, et al. Analysis of influenza A and B virus test results and viral load in 2,357 children with influenza-like illness. Chinese Journal of Hospital Infection. 2020;30(2):278–282.China.
PENG Xianhua, LI Bingbing, LI Xiaolin, LEI Guofeng, MA Chunying, ZHENG Satellite.Epidemiological characteristics of Mycoplasma pneumoniae infection among children with respiratory tract infections in a hospital in 2021–2022. Chinese Journal of Hospital Infection. 2023;33(18):2851–2854.China.
LIN Jian, LI Wei, ZHOU Chao, TANG Jiaming, GUO Yajun, SHANG Shiqiang. Viral aetiology testing and epidemiologic characterization of pediatric patients with influenza-like illness. Chinese Journal of Laboratory Medicine. 2022;45(6):574–580.China.
Reeves RM, Hardelid P, Gilbert R, Warburton F, Ellis J, Pebody RG. Estimating the burden of respiratory syncytial virus (RSV) on respiratory hospital admissions in children less than five years of age in England, 2007–2012. Influenza Other Respir Viruses. 2017;11(2):122–9.
Nair H, Nokes DJ, Gessner BD, Dherani M, Madhi SA, Singleton RJ, et al. Global burden of acute lower respiratory infections due to respiratory syncytial virus in young children: a systematic review and meta-analysis. Lancet. 2010;375(9725):1545–55.
Tong S, Amand C, Kieffer A, Kyaw MH. Incidence of respiratory syncytial virus related health care utilization in the United States. J Glob Health 2020;10(2) [Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7568930/].
FU Zongqiang, LIU Doudou, ZHANG Huizheng, NIU Xiaobin, LI Yongwei. Prevalence characteristics of respiratory tract infection pathogens in patients hospitalized in a single center in Zhengzhou area. Henan Medical Research. 2020;29(1):1–5.China.
Cillóniz, Catia., Pericàs, Juan M., Pericàs, Juan M., Rojas, Jorge R., Torres, Antoni.. Severe Infections Due to Respiratory Viruses. Seminars in respiratory and critical care medicine, 2022, 43(1):60–74.
Guohong Z, Dan X, Yuanyuan Z, et al. Epidemiological characteristics of four common respiratory viral infections in children. Virology Journal. 2021;18(1):10–10.
Notice on Printing and Distributing the novel coronavirus Pneumonia Prevention and Control Program (8th Edition). Bulletin of the National Health Commission of the People's Republic of China, 2021, (05): 4–60
Cohen, Robert., Ashman, Marion., Taha, Muhamed-Kheir., Varon, Emmanuelle., Angoulvant, François.. Pediatric Infectious Disease Group (GPIP) position paper on the immune debt of the COVID-19 pandemic in childhood, how can we fill the immunity gap?. Infectious diseases now, 2021, 51(5).
Calvo C. Changes in the epidemiology of infections in children. Is there an immune debt? Only for respiratory viruses? An Pediatr (Engl Ed). 2023 Mar;98(3):155–156. https://doi.org/10.1016/j.anpede.2023.01.014. Epub 2023 Feb 23. PMID: 36828695; PMCID: PMC9946788.
Munro, Alasdair Ps., Jones, Christine E., Jones, Christine E.. Immunity debt and unseasonal childhood respiratory viruses. British journal of hospital medicine (London, England : 2005), 2022, .
Baker RE, Park SW, Yang W, Vecchi GA, Metcalf CJE, Grenfell BT. The impact of COVID-19 nonpharmaceutical interventions on the future dynamics of endemic infections. Proc Natl Acad Sci. 2020;117(48):30547–53.
Li W, Liu L, Chen L, Shang S. Evaluation of a Commercial Colloidal Gold Assay for Detection of Influenza A and B Virus in Children's Respiratory Specimens. Fetal Pediatr Pathol, 2019, 39(2).
Acknowledgements
Thanks to AP Shouting Lu of Luoyang Institute of Science and Technology for his support in the field of statistics for this paper. Meanwhile, we would like to thank our funders, esp. Luoyang Maternal and Child Health Hospital, for their kind and generous financial support towards achieving these study objectives.
Funding
Henan Provincial Department of Education Humanities and Social Sciences Research Project, 2023-ZDJH-529.
Author information
Authors and Affiliations
Contributions
All authors contributed equally to this work. Pingping Wang wrote the original draft. Jin Yao revised the manuscript. Zhanjun Zhang and Kenan Fang supervised the investigation. Shouting Lu performed the data analysis. Xiaorong Huang translated the draft. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Luoyang Maternal and Child Health Hospital (LWOPN 224020802.0). The ethical approval waived the need for informed consent, being that this study was Retrospective Study. All data collected were stripped of patient identifiers, with no possibility to track the data to an individual person’s identity.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, P., Zhang, Z., Fang, K. et al. Analysis of the epidemic characteristics of common respiratory pathogens infection in children in a 3A special hospital. BMC Infect Dis 24, 879 (2024). https://doi.org/10.1186/s12879-024-09784-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09784-1