Abstract
Background
Sepsis is a life-threatening organ dysfunction caused by an excessive host response to infection, manifested by elevated levels of inflammatory cytokines. At present, the use of hemoperfusion to remove inflammatory cytokines from the bloodstream has been expanding. Meanwhile, the pharmacokinetics and pharmacodynamics characteristics of antibiotics in critically ill patients may be impacted by hemoperfusion.
Case presentation
The patient was a 69-year-old male with poorly controlled type 2 diabetes. When admitted to the ICU, Multiple Organ Dysfunction Syndrome (MODS) appeared within 48 h, and he was suspected of septic shock due to acute granulocytopenia and significantly increased procalcitonin. Broad-spectrum antibiotics imipenem was administered according to Sepsis 3.0 bundle and hemoperfusion lasting 4 h with a neutron-macroporous resin device (HA-380, Jafron, China) five times was conducted to lower the extremely high value of serum inflammatory factors. Blood samples were collected to measure imipenem plasma concentration to investigate the effect of hemoperfusion quantitatively. This study showed that 4 h of hemoperfusion had a good adsorption ability on inflammatory factors and could remove about 75.2% of imipenem.
Conclusions
This case demonstrated the high adsorption capacity of hemoperfusion on imipenem in critically ill patients. It implies a timely imipenem supplement is required, especially before hemoperfusion.
Similar content being viewed by others
Background
Sepsis manifests as potentially fatal organ dysfunction with a high level of inflammatory cytokines due to the dysregulated host response to infection [1, 2]. It has raised a public health concern [1] as a leading cause of mortality worldwide [3, 4]. In mainland China, about one-fifth of patients admitted to the intensive care unit (ICU) were diagnosed with sepsis, with a 90-day mortality rate of 35.5% [5]. Effective antibiotic treatment is crucial and should be initiated as soon as possible [6]. Vincent et al. [7] demonstrated that Gram-negative bacterial infections accounted for 67% of severe infection patients. Carbapenems, such as imipenem, are commonly used as empirical therapy [8].
Hemoperfusion is a technique of blood purification relying on the interaction of target molecules with a sorbent [9]. There are various types of hemoperfusion cartridges targeting endotoxins or cytokines globally [9]. Though it benefits inflammatory cytokines absorption, hemoperfusion may affect the pharmacokinetic (PK) characteristics of antibiotics. Beyond complicating the hemodynamic state, hemoperfusion can also affect the concentration of antibiotics in the patient’s body, thus may partially affect the effectiveness of anti-infective treatment. Therefore, how does the PK of antibiotics change? How do we optimize the dosage regimen in septic patients undergoing hemoperfusion? Few studies [10] focused on imipenem absorption and dose adjustment during hemoperfusion. By estimating PK parameters before and after 4-hour hemoperfusion, we aim to describe the hemoperfusion absorption ability of imipenem and provide the optimized strategy for imipenem administration under hemoperfusion.
Case presentation
The patient was a 69-year-old male with poorly controlled type 2 diabetes. Following a cerebral hemorrhage and craniotomy, he developed severe pneumonia and acute respiratory distress syndrome (ARDS) within 24 h. We transferred him to the ICU on July 28th, 2020 (D1) after his second intubation. Multiple Organ Dysfunction Syndrome (MODS) appeared within 48 h. In addition, he had the complications of acute heart failure (left ventricular ejection fraction decreased from 61 to 30%, impaired diastolic function, N-terminal pro-B-type natriuretic peptide: 26700 pg/mL), acute kidney injury (serum creatinine: 332 µmol/L, with anuria), acute liver injury (elevated levels of aminotransferase [alanine aminotransferase: 187 U/L] and bilirubin [total bilirubin: 84.2 umol/L], coagulation disorder [fibrinogen: 7.16 g/L, fibrinogen and fibrin degradation products: 24.3 ug/mL, D-Dimer: 3.16 ug/mL] with hypoproteinemia [albumin: 20.9 g/L], dropped from Child-Pugh class A to B), granulocytopenia and thrombocytopenia (white blood cell count: 0.71 × 10^9/L, neutrophil count: 0.43 × 10^9/L, platelet count: 68 × 10^9/L). When admitted to the ICU, he was suspected of septic shock due to acute granulocytopenia and significantly increased procalcitonin (from 8 ng/mL to 74 ng/mL in 31 h).
Based on the Sepsis 3.0 bundle, we collected the patient’s blood, urine, sputum, and other body fluids for etiological examination (including smears, cultures, and metagenomics next-generation sequencing (mNGS), and the broad-spectrum antibiotics imipenem and cilastatin sodium (0.5 g/0.5 g, q6h, prolonged infusion to 2 h) were immediately administered, together with vancomycin. At the same time, we implanted PiCCO for hemodynamic parameters-guided fluid resuscitation. Dobutamine, mechanical ventilation, and continuous veno venous hemofiltration (CVVH, blood flow rate: 180 mL/min, replacement fluid rate for pre/post-dilution: 1200 mL/h, ultrafiltration rate: 35.2 mL/[h×kg]) were also used. The application indication of CVVH was septic shock with acute kidney injury. mNGS detected Klebsiella pneumoniae in sputum and blood samples, consistent with the subsequent culture results in the same samples. Meanwhile, such the extremely high value of serum inflammatory factors was detected, as interleukin-6 (IL-6), IL-8, and IL-10 being 3.31 × 10^10 pg/mL, 9.21 × 10^4 pg/mL, and 266.06 pg/ml respectively (Fig. 1A). Hemoperfusion was needed since CVVH can not remove macromolecular inflammatory cytokines. We then performed hemoperfusion with a neutron-macroporous resin device (HA-380, Jafron, China) five times from July 28th to August 1st (D1—D5) [11,12,13,14]. Hemoperfusion lasted 4 h each time, and CVVH treatment continued throughout the whole course (Fig. 1B). On August 4th, after five times of hemoperfusion, IL-6, IL-8, and IL-10 decreased to 40.16 pg/mL, 224.51 pg/mL, and 5.91 pg/mL, respectively (Fig. 1A), which indicates a good adsorption ability of hemoperfusion on inflammatory factors.
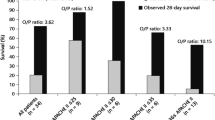
(A). Values of IL-6, IL-8 and IL-10 from 7/28/2020 to 8/4/2020. (This patient received hemoperfusion five times from July 28th to August 1st (D1—D5), and IL-6, IL-8, and IL-10, which were determined by flow cytometry, decreased gradually.); (B). The ideograph of hemoperfusion and CVVH. (The vena jugularis interna draws and returns blood. The red line represents the blood route, and the black line indicates the introduction of anticoagulants (sodium citrate). The red arrow represents the direction of blood flow. The dotted box indicates hemoperfusion for 4 h each time, which was withdrawn at the end. CVVH, continuous veno venous hemofiltration.) (C). The observed and predicted imipenem plasma concentration-time profiles of this patient. (“a” represents intravenous imipenem, and the infusion duration was 2 h. The sampling times were 15 min before administration, 30 min after the completion of the infusion, before hemoperfusion, and after hemoperfusion. Light gray area indicates CVVH treatment, and dark gray area indicates CVVH and hemoperfusion treatment. Solid square represents the observed value, and the solid line represents the observed curve. Solid dots represent predicted values, and the dotted lines represent predicted curves. It should be mentioned that the predicted values were obtained from the scenario assuming only CVVH without hemoperfusion therapy.)
To quantitatively investigate the effect of hemoperfusion on imipenem, blood samples were taken to measure the plasma concentration before and after hemoperfusion on August 1st (D5), five days following CVVH, hemoperfusion, and anti-infective therapy. As imipenem has a half-life of about 1 h, it was assumed the plasma concentration of imipenem had reached the steady state. Plasma was separated by centrifuge and stored at -80℃ until assayed. The plasma concentrations of imipenem were measured using a validated high-performance liquid chromatography (Shimadzu LC-30 A; Shimadzu, JP) coupled with tandem mass spectrometry (ABSciex 4000 + triple quadrupole system, ABSciex Corp., USA) method. The data was acquired and processed by Analyst 1.6.2 software (ABSciex Corp.). A 200 µL plasma sample was processed by protein precipitation. A total of four samples were collected. The sampling times were 15 min before administration (13:45), 30 min after the completion of the infusion (16:30, which was known as the peak concentration [15], and the infusion time was two hours), before hemoperfusion (17:00), and after hemoperfusion (21:00). The concentrations of imipenem in each time were 16.2 mg/L, 24 mg/L, 19.9 mg/L, and 3.47 mg/L correspondingly (Fig. 1C).
In addition, the PK parameters were calculated using the first-order conditional estimation method [16] through NONMEM version 7.2.0 software (ICON Development Solutions). One- and two-compartment models with first-order absorption and linear elimination were investigated to determine the optimal structural model. Because we only had one patient, the inter-individual variability was fixed at 0, and hemoperfusion was included as the covariate. Finally, the one-compartment model was chosen as it better described the data. The estimated PK parameters are summarized in Table 1. The clearance of this patient only during CVVH and during CVVH combined hemoperfusion was 4.25 L/h and 18.05 L/h, respectively. Besides, the PK model estimated the blood concentration of imipenem at 21:00 to be 13.99 mg/L assuming without hemoperfusion (Fig. 1C), and the actual concentration after hemoperfusion was 3.47 mg/L. That means 4-hour hemoperfusion cleared about 75.2% of imipenem. It suggests that 750 mg of imipenem at the beginning of hemoperfusion for this patient, estimated by the current PK model, would achieve enough imipenem concentration (10.08 mg/L), which is close to 13.99 mg/L. The various dosages simulated by the model and their predicted concentrations after hemoperfusion are shown in Table 2.
This patient underwent a tracheotomy once the infection was controlled (D10). After breathing and limb rehabilitation exercises, the patient was weaned off the ventilator (D75) and returned to carry out bed activities. He was transferred to a rehabilitation hospital on November 1st, 2020 (D97), and has partially recovered his independent living ability.
Discussion and conclusions
At present, an increasing number of studies show that hemoperfusion can effectively remove inflammatory cytokines in septic patients. Blocking or attenuating the impact of inflammatory cytokines offers protection in acute animal models of fulminant infections [14, 17]. Hemoperfusion can theoretically deliver non-specific treatment, based on several mediators’ plasma levels rather than targeting single cytokines, which has failed before [14, 18, 19]. With new biocompatible sorbent cartridges, the removal of humoral mediators and cytokines with different columns (CytoSorb®, Cytosorbents, NJ, USA, and HA380, Jafron, China, which the patients used) may be beneficial for the septic patients [14, 20]. In this case, inflammatory cytokines declined rapidly after hemoperfusion, which proved its great clearance ability.
Hemoperfusion may also remove antibiotics and affect the efficacy of anti-infective therapy. International Guidelines for Management of Sepsis and Septic Shock [6] recommended empiric broad-spectrum therapy with one or more antimicrobials for patients presenting with sepsis or septic shock to cover all likely pathogens, so carbapenems were usually the first choice. However, scarce evidence exists about how to adjust the antibiotics dosage regimen. A prospective PK study [21] was conducted at a tertiary hospital to evaluate the effect of direct hemoperfusion with polymyxin B immobilized cartridge (DHP-PMX) on meropenem PK in ICU patients with sepsis requiring CVVH. It demonstrated that DHP-PMX does not exhibit a significant effect on meropenem PK, and dose adjustment is unrequired. There are no related studies about imipenem, a very common carbapenem antibiotic in the Sepsis Bundle. Our study showed that 4 h of hemoperfusion could remove about 75.2% of imipenem, owing to the lower molecular weight of imipenem than meropenem (299.346 vs. 383.463 Dalton) or the differences of columns used in the hemoperfusion [14]. Given the central nervous system toxicity of imipenem, as well as to balance the effectiveness of imipenem and its safety, we suggest a 150% dose administration at the start of hemoperfusion.
There are three limitations of this study. Firstly, blood samples were collected only before and after hemoperfusion, resulting in missing details of the PK profile during hemoperfusion. Therefore, results estimated by mathematical methods still need to be further verified. In addition, since the patient received hemoperfusion and CVVH simultaneously, it was hard to measure the effect of hemoperfusion directly. Previous studies [22] have demonstrated that imipenem can be cleared by CVVH, but this patient has been receiving CVVH therapy before and after hemoperfusion, and the parameters of CVVH have not been changed. We may have concentrated on the relative difference in serum imipenem concentration between pre- and post-hemoperfusion, since this may indicated the adsorption capacity of hemoperfusion. Finally, only the concentration of imipenem was determined, and cilastatin was considered ineffective except for inhibiting renal clearance of imipenem by default as the patient was anuric. However, cilastatin absorption by hemoperfusion can’t be ignored for patients with urine as it may affect the activity of imipenem.
This case illustrated that about 75% of imipenem was removed after 4-hour hemoperfusion using HA380 resin hemoperfusion cartridge. It implies a timely imipenem supplement is required, especially before hemoperfusion, which can be beneficial to keep adequate antibiotic concentration during the hemoperfusion. As we only had one patient, future studies are needed to validate the conclusion.
Data availability
Data is provided within the manuscript.
Abbreviations
- ICU:
-
intensive care unit
- HP:
-
Hemoperfusion
- PK:
-
pharmacokinetic
- ARDS:
-
acute respiratory distress syndrome
- MODS:
-
multiple organ dysfunction syndrome
- mNGS:
-
metagenomics next-generation sequencing
- CVVH:
-
continuous veno venous hemofiltration
- IL:
-
interleukin
- DHP-PMX:
-
direct hemoperfusion with polymyxin B immobilized cartridge
References
Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus definitions for Sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):801.
Shankar-Hari M, Phillips GS, Levy ML, et al. Developing a new definition and assessing New Clinical Criteria for septic shock. JAMA. 2016;315(8):775.
Vincent JL, Marshall JC, Namendys-Silva SA, et al. Assessment of the worldwide burden of critical illness: the intensive care over nations (ICON) audit. Lancet Respir Med. 2014;2(5):380–6.
Fleischmann C, Scherag A, Adhikari NK, et al. Assessment of Global Incidence and Mortality of Hospital-treated Sepsis. Current estimates and limitations. Am J Respir Crit Care Med. 2016;193(3):259–72.
Xie J, Wang H, Kang Y, et al. The epidemiology of Sepsis in Chinese ICUs: a National Cross-sectional Survey. Crit Care Med. 2020;48(3):e209–18.
Evans L, Rhodes A, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021;47(11):1181–247.
Vincent JL, Sakr Y, Singer M, et al. Prevalence and outcomes of infection among patients in Intensive Care Units in 2017. JAMA. 2020;323(15):1478–87.
David NJ, Henry FC, George ME, et al. Antibiotic dose adjustment of adults with repaired renal function. The Sanford Guide to Antimicrobial Therapy 2018 (Chinese Version). Sperryville, VA, USA: Antimicrobial Therapy, Inc.; 2018.
Ronco C, Bagshaw SM, Bellomo R, et al. Extracorporeal blood purification and organ support in the critically ill patient during COVID-19 pandemic: Expert Review and Recommendation. Blood Purif. 2021;50(1):17–27.
Selig DJ, Reed T, Chung KK et al. Hemoperfusion with Seraph 100 Microbind Affinity Blood Filter unlikely to require increased antibiotic dosing: a simulations Study using a Pharmacokinetic/Pharmacodynamic Approach. Blood Purificat 2022:1–7.
Navas A, Ferrer R, Martínez ML, et al. Impact of hemoperfusion with polymyxin B added to hemofiltration in patients with endotoxic shock: a case-control study. Ann Intensive Care. 2018;8(1):121.
Zhou Z, Kuang H, Ma Y, et al. Application of extracorporeal therapies in critically ill COVID-19 patients. J Zhejiang Univ Sci B. 2021;22(9):701–17.
Burov AI, Abramov TA, Kostritca NS, et al. Observational case series: six neurosurgical patients with septic shock demonstrating clinical improvement after a combination of standard care and blood purification. Eur J Med Res. 2021;26(1):151.
Ricci Z, Romagnoli S, Reis T, et al. Hemoperfusion in the intensive care unit. Intensive Care Med. 2022;48(10):1397–408.
de Velde F, de Winter B, Neely MN, et al. Population Pharmacokinetics of Imipenem in critically ill patients: a Parametric and Nonparametric Model Converge on CKD-EPI estimated glomerular filtration rate as an Impactful Covariate. Clin Pharmacokinet. 2020;59(7):885–98.
Hooker AC, Staatz CE, Karlsson MO. Conditional weighted residuals (CWRES): a model diagnostic for the FOCE method. Pharm Res. 2007;24(12):2187–97.
Wiersinga WJ, Leopold SJ, Cranendonk DR, van der Poll T. Host innate immune responses to sepsis. Virulence. 2014;5(1):36–44.
Barzilay E, Kessler D, Berlot G, Gullo A, Geber D, Ben ZI. Use of extracorporeal supportive techniques as additional treatment for septic-induced multiple organ failure patients. Crit Care Med. 1989;17(7):634–7.
Rimmelé T, Kellum JA. Clinical review: blood purification for sepsis. Crit Care. 2011;15(1):205.
Huang Z, Wang SR, Su W, Liu JY. Removal of humoral mediators and the effect on the survival of septic patients by hemoperfusion with neutral microporous resin column. Ther Apher Dial. 2010;14(6):596–602.
Singhan W, Vadcharavivad S, Areepium N, et al. The effect of direct hemoperfusion with polymyxin B immobilized cartridge on meropenem in critically ill patients requiring renal support. J Crit Care. 2019;51:71–6.
Li Z, Bai J, Wen A, et al. Pharmacokinetic and pharmacodynamic analysis of critically ill patients undergoing continuous renal replacement therapy with imipenem. Clin Ther. 2020;42(8):1564–77.
Acknowledgements
We sincerely thank the patient for willing to share his therapy information, thank doctor Mingxia Zhu for her guidance of cytokines detection methods, and thank the multidisciplinary therapy team for their assistance in this research.
Funding
This work was supported by Peking University Medicine Fund of Fostering Young Scholars’ Scientific & Technological Innovation, which was established by Fundamental Research Funds for the Central Universities [Grant number BMU2022PYB011, receiver: Xiao-xiao, Li].
Author information
Authors and Affiliations
Contributions
Conception: XXL, CL, SDZ, and CHW; Data curation: CHW, CL, PY, YGL and XX; Formal analysis: CHW, XXL, and CL; Funding acquisition: XXL; Investigation: CHW, CL, PY, YGL and XX; Methodology: CHW, XXL, PY, and XX; Project administration: XXL and SDZ; Resources: CHW, CL and YGL; Software: CHW, PY and XX; Supervision: XXL and SDZ; Validation: XXL and SDZ; Visualization: KXL; Writing - original draft: CHW and CL; Writing - review & editing: XXL, PY, SDZ, XX, KXL and YGL.
Corresponding authors
Ethics declarations
Ethical approval
Not required.
Patient consent statement
Written informed consent was obtained from the individual for the publication of any potentially identifiable images or data included in this article.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, C., Li, C., Yang, P. et al. High adsorption capacity of hemoperfusion on imipenem in critically ill patients with septic shock: a case report. BMC Infect Dis 24, 894 (2024). https://doi.org/10.1186/s12879-024-09774-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09774-3