Abstract
Background
Prior antibiotic exposure has been identified as a risk factor for VAP occurrence, making it a growing concern among clinical practitioners. But there is a lack of systematic research on the types of antibiotics and the duration of exposure that influence VAP occurrence in children at current.
Methods
We retrospectively reviewed 278 children admitted to the Pediatric Intensive Care Unit (PICU) and underwent invasive mechanical ventilation (MV) between January 2020 and December 2022. Of these, 171 patients with MV duration ≥ 48 h were included in the study, with 61 of them developing VAP (VAP group) and the remaining 110 as the non-VAP group. We analyzed the relationship between early antibiotic exposure and VAP occurrence.
Results
The incidence of VAP was 21.94% (61/278). The VAP group had significantly longer length of hospital stay (32.00 vs. 20.00 days, p<0.001), PICU stay(25.00 vs. 10.00 days, p<0.001), and duration of mechanical ventilation(16.00 vs. 6.00 days, p<0.001) compared to the non-VAP group. The mortality in the VAP group was significantly higher than that in the non-VAP group (36.07% vs. 21.82%, p = 0.044). The VAP group had a significantly higher rate of carbapenem exposure (65.57% vs. 41.82%, p = 0.003) and duration of usage (9.00 vs. 5.00 days, p = 0.004) than the non-VAP group. Vancomycin and/or linezolid exposure rates (57.38% vs. 40.00%, p = 0.029) and duration (8 vs. 4.5 days, p = 0.010) in the VAP group were significantly higher than that in the non-VAP group, either. Multivariate logistic regression analysis identified the use of carbapenem (≥ 7 days) (OR = 5.156, 95% CI: 1.881–14.137, p = 0.001), repeated intubation (OR = 3.575, 95% CI: 1.449–8.823, p = 0.006), and tracheostomy (OR = 5.767, 95% CI:1.686–19.729, p = 0.005) as the independent risk factors for the occurrence of VAP, while early intravenous immunoglobulin (IVIG) was a protective factor against VAP (OR = 0.426, 95% CI: 0.185–0.98, p = 0.045).
Conclusion
Prior carbapenem exposure (more than 7 days) was an independent risk factor for the occurrence of VAP. For critically ill children, reducing carbapenem use and duration as much as possible should be considered.
Similar content being viewed by others
Background
Ventilation-Associated Pneumonia (VAP) occurs in patients who have been mechanically ventilated via endotracheal intubation or tracheostomy for 48 h or more. Pneumonia occurring within 48 h after extubating also belonged to VAP [1, 2]. VAP is one of the most common hospital-associated infections (HAIs) in the pediatric intensive care unit (PICU) [3, 4], second only to bloodstream infections, accounting for approximately 20% of HAIs in the PICU [5]. The occurrence of VAP lead to a prolonged hospital stay, an increase in medical costs and clinical mortality, and an impact on children’s prognosis [6]. In recent years, as healthcare professionals have gained a deeper understanding of VAP, more intensive care units have adopted standardized operating procedures (SOPs) for VAP prevention. The SOPs encompassed key practices such as oral hygiene, elevation of the head of the bed, sterile endotracheal suctioning, minimal ventilator circuit adjustments, daily sedation interruption, assessment for extubation readiness, intubation and equipment management, and the use of H2-receptor antagonists [7, 8], which was considered to be VAP bundle. In Spain, VAP bundle proved effective in reducing VAP rates, with Peña-López [9] reporting a decrease from 8.16 to 0.65 per 1,000 tracheostomy ventilation-days, and Esteban [10] noting a reduction from 28.3 to 10.6 per 1,000 ventilation days. A multinational study by Rosenthal [11] covering Colombia, Turkey, El Salvador, India, and the Philippines showed a 31% reduction in VAP rates from 11.7 to 8.1 per 1,000 ventilator days following bundle implementation. These findings indicate that bundles are highly effective in reducing VAP incidence across diverse regions and healthcare settings. Although a decrease in the incidence has been observed, it is still high, and once it occurs, the mortality and economic burden of the patient have increased significantly. Antibiotic exposure has been reported as a risk factor for the development of VAP, but it is unclear which antibiotic causes it.
The use of broad-spectrum antibiotics remains a crucial treatment for critically ill pediatric patients. Antibiotic treatment regimens and durations were influenced by various clinical factors, including the infectious pathogen, site of infection, and the host’s immune status. Timely and appropriate antimicrobial therapy can improve the prognosis of critically ill pediatric patients [12, 13]. However, prolonged exposure to antibiotics can lead to the growing of drug-resistant bacterial strains, alterations in the host’s microbial ecology, and even disruption of the immunity. Prior antibiotic exposure has been identified as a risk factor for VAP development [14], making it a growing concern among clinical practitioners. Moreover, although SOPs were applied to prevent the occurrence of VAP in clinical practice, some children still developed VAP, and many pathogens have been shown to originate from microorganisms colonizing the intestines. Therefore, we speculated that the use of broad-spectrum antibiotics in critically ill children may be a key factor in the development of VAP, but there is a lack of systematic research on the types of antibiotics and the duration of exposure before VAP occurrence in children. A systematic analysis of VAP patients was conducted in this study, aim to find factors that may affect the occurrence of VAP.
Methods
Subjects
This study was a three-year, multi-center retrospective study conducted in accordance with the principles of the Helsinki Declaration and approved by the Clinical Research Ethics Committee of the First People’s Hospital of Lianyungang (Approval No. LW-20231024003-01) and the Children’s Hospital of Soochow University (Approval No. 2023CS034). Written informed consent was obtained from patients or their guardians.
A total of 278 children admitted to the Pediatric Intensive Care Units (PICU) at the Children’s Hospital of Soochow University and the First People’s Hospital of Lianyungang and received invasive mechanical ventilation (MV) between January 2020 and December 2022 were included in this study. Among these patients, 171 met the inclusion criteria, which required a minimum MV duration of ≥ 48 hours and excluded patients who had undergone MV before admission to the PICU, and patients who developed pneumonia within 48 hours after MV initiation (Fig. 1). VAP was diagnosed according to the diagnostic criteria outlined in the " Pneumonia (Ventilator-associated [VAP] and non-ventilator- associated Pneumonia [PNEU]) Event [2]. During the observation period, 61 cases developed VAP and were classified as VAP group, while the remaining 110 cases did not develop VAP and were classified as non-VAP group.
Definitions
The prior antibiotic exposure refers to the period of one month before the occurrence of VAP. The observation endpoint was 48 h after of mechanical ventilation (MV) withdrawal. Disease severity was assessed on admission using the Pediatric Critical Illness Score (PCIS) and the Pediatric Risk of Mortality Score III (PRISM III) [15].
Antibiotic information
The daily dosage and duration of all antibiotics used by the enrolled patients during the observation period of antibiotic exposure (if the duration was less than 1 day, it was not included in the statistics) were collected and analyzed. Prior exposure to antibiotics includes carbapenems (including meropenem and imipenem), cephalosporins (such as cefotetan, ceftazidime, ceftriaxone, and cefuroxime), beta-lactam/beta-lactamase inhibitor combinations (referred to as beta-lactam/lactamase inhibitor combinations, such as piperacillin-tazobactam and ampicillin-sulbactam), vancomycin, linezolid, azithromycin, trimethoprim-sulfamethoxazole, tigecycline, polymyxin B, amikacin, and metronidazole. In 2016, the Infectious Diseases Society of America recognized the duration of treatment for pneumonia associated with ventilators and medical institutions as seven days [16], and the same recommendation was made for the diagnosis and treatment of sepsis and septic shock in children [17].Therefore, we set a 7-day cutoff for carbapenem exposure.
Collection of clinical and laboratory data
According to the aim of the research, the case report form was designed to track the electronic medical records of all the selected subjects. Data entry was carried out after the training of data entry clerks, and the double entry method was adopted, which was completed by two people independently. General information, outcomes, the choice of endotracheal intubation, mental status and underlying disease were collected. Factors potentially related to the occurrence of VAP during the antibiotic exposure were also collected. These factors included the use of intravenous immunoglobulin (IVIG), enteral/parenteral nutrition, proton pump inhibitors, corticosteroids, nasogastric tube placement, central venous catheterization, hemodialysis, tracheostomy status, repeated intubation, and prior use of non-invasive ventilation.
Statistical analysis
Data analysis was conducted using SPSS 27.0 statistical software. Continuous data was represented by the median and quartile interval [M (P25, P75)], and the Mann-Whitney U test was used for comparison between the two groups. Categorical data were presented as frequencies and percentages (%), and the chi-squared test or Fisher’s exact test was used to compare these two groups. Initially, a univariate analysis was conducted, then variables with clinically determined risk factors for incidence of VAP and a p-value < 0.2 [18, 19] were included in the multivariate regression. Multivariate Cox regression model was used to determine the independent risk factors for the occurrence of VAP, which was the primary outcome in this study. P < 0.05 was determined as statistically significant.
Results
Clinical characteristics
There were no significant differences of gender (p = 0.613), age (p = 0.276), PCIS score on admission (p = 0.219) and PRISM III score (p = 0.206) between the VAP group and the non-VAP group. The clinical characteristics of the VAP group and the non-VAP group were shown in Table 1. Patients in the VAP group had significantly higher mortality (36.07% vs. 21.82, p = 0.044), length of hospital stay (32.00 vs. 20.00 days, p<0.001), length of PICU stay (25.00 vs. 10.00 days, p<0.001), duration of mechanical ventilation (16.00 vs. 6.00 days, p<0.001), and hospitalization costs (16,6100 vs. 6,3400 yuan, p<0.001) compared to the non-VAP group. After intubation, the median time of VAP was 7 days (4.4,13) for the VAP group.
Analysis of antibiotics exposure
The antibiotic exposure rate for the 171 mechanically ventilated (MV) patients was 98.83% (169/171). The comparison of antibiotic exposure in pediatric patients between the VAP group and the non-VAP group was shown in Table 2. The VAP group had a significantly higher rate of exposure to ≥ 3 types of antibiotics, the duration of exposure ≥ 7 days, and a longer duration of antibiotic exposure compared to the non-VAP group (Table 2).
In order to analyze the relationship between the type of antibiotic and the duration of exposure and VAP, we did further analysis and the results showed that there were no differences of cephalosporin, β-lactamase inhibitor combination, vancomycin and/or linezolid, azithromycin and trimethoprim-sulfamethoxazole between these two groups, but the VAP group had significantly higher rates of exposure to carbapenem antibiotics, vancomycin and/or linezolid, and longer exposure durations for these classes of antibiotics, as well as a higher rate of exposure ≥ 7 days, compared to the non-VAP group (Table 3).
Carbapenem exposure was an independent risk factor for the occurrence of VAP
To identify risk factors that may be associated with occurrence of VAP, we first performed univariate analysis. The results revealed that underlying diseases (such as hematological malignancies, genetic metabolic diseases, neurological diseases, congenital heart defects, congenital respiratory system developmental abnormalities, immunodeficiency, malnutrition, rheumatic autoimmune diseases, etc.), a history of repeated intubations, tracheostomy status, total antibiotic exposure ≥ 7 days, exposure to ≥ 3 types of antibiotics, exposure to carbapenem antibiotics for ≥ 7 days and exposure to vancomycin and/or linezolid for ≥ 7 days were significantly associated with the occurrence of VAP.
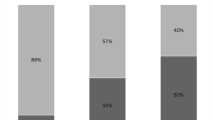
To find risk factors that could independently predict the occurrence of VAP, multivariate regression analysis was performed with p value less than 0.2 and clinically determined possible risk factors. The results showed that exposure to carbapenem antibiotics for ≥ 7 days (OR = 5.156; 95% CI, 1.881–14.137; P = 0.001), a history of repeated endotracheal intubations (OR = 3.575; 95% CI, 1.449–8.823; P = 0.006), tracheostomy status (OR = 5.767; 95% CI, 1.686–19.729, P = 0.005), and prior use of IVIG (OR = 0.426; 95% CI, 0.185–0.981; P = 0.045) were significantly associated with the occurrence of VAP. Therefore, exposure to carbapenem antibiotics for ≥ 7 days, a history of multiple endotracheal intubations (≥ 2 times), and tracheostomy status were independent risk factors for VAP, while the use of IVIG was an independent protective factor against VAP (Table 4).
Distribution of pathogens detected in the VAP patients
According to the diagnostic criteria for VAP, there were 61 cases with VAP, of which 63.93% (39/61) of the children were detected with pathogenic bacteria in respiratory specimens. There were 11 cases isolated with mixed pathogens. A total of 55 strains were isolated, mainly Gram-negative bacteria (72.73%,40/55), Gram-positive bacteria (18.18%,18/55) and fungi (9.09%, 5/55). Moreover, the detail pathogens for the VAP patients were also listed (Table 5). From the results, we found 67.5% (27/40) Gram-negative bacteria, 40% (4/10) Gram-positive bacteria and 100% (5/5) were presented in patients with prior carbapenem. For Gram-negative bacteria, Acinetobacter baumannii was the most common isolated pathogen, next was Pseudomonas aeruginosa. Few fungi have been isolated, but 100% of patients were indicated with prior carbapenem (Table 5), indicating dysbiosis caused by prior carbapenem exposure made fungi opportunistic pathogens.
Discussion
The incidence of VAP in pediatric patients varied significantly worldwide, ranging from 2.00 to 38.4% [20,21,22,23]. This variability can be attributed to multiple factors, including underlying disease, the etiology of MV, and the quality of infection control implementation. In this study, the VAP incidence was 21.94%, which may be related to the high proportion of immunocompromised patients with hematologic malignancies admitted to our center. For these patients, there were high-risk factors for infection, and once fever with neutropenia occurs, antibiotic was initiated. In addition, due to the difficulties in the duration of antibiotic because of the complicated conditions, long-term use of antibiotics may occur, and whether these measures are risk factors for VAP is worth consideration.
This research identified prolonged exposure (more than 7 days) to carbapenem as an independent risk factor for VAP occurrence among various antibiotic classes. Carbapenem have been associated with an increased risk of nosocomial infections, including Clostridioides difficile infections and VAP [24,25,26]. As a class of broad-spectrum antimicrobial agents, carbapenems exhibit excellent antibacterial activity against most aerobic and anaerobic bacteria. Under the pressure of carbapenem exposure, colonizing bacteria in the respiratory tract may develop resistance due to metallo-β-lactamase production, high-level cephalosporinase production, extended-spectrum β-lactamase production, and alterations in binding sites. This can lead to multidrug-resistant strains capable of cross-resistance to carbapenems, β-lactams, and aminoglycosides [27]. These antibiotic-resistant strains can expand and become dominant in the respiratory tract, serving as potential pathogens for VAP. In our study, the main pathogenic pathogens of ventilator-associated pneumonia was Gram-negative bacteria, accounting for 72.73%, and the cases with prior carbapenem exposure were about twice as high as those without prior carbapenem exposure. The most prevalent Gram-negative bacteria were Acinetobacter baumannii, Pseudomonas aeruginosa, and Klebsiella pneumoniae, all of which exhibited carbapenem resistance, consistent with previous studies. Additionally, the use of carbapenem can alter the gut microbiota, disrupting the normal host-microbiota interactions in both the gut and the lungs, which is known as the gut-lung axis. This disruption can contribute to lung injury and pulmonary infections [28]. These factors collectively increase the risk of VAP in MV patients following exposure to carbapenem antibiotics.
The study also found a higher proportion of exposure to vancomycin and/or linezolid in the VAP group. However, the multivariate regression analysis did not identify it as an independent risk factor for VAP occurrence. Vancomycin and linezolid belong to the glycopeptide and oxazolidinone classes of antibiotics, respectively, and are used to treat severe Gram-positive bacterial infections, especially methicillin-resistant Staphylococcus aureus infections. Previous experiments in mice have shown that vancomycin and linezolid administration, either subcutaneously or orally, can suppress anaerobic bacteria and Enterococci in the gut microbiota and promote the colonization of extended-spectrum β-lactamase-producing Klebsiella pneumoniae [29]. Vancomycin has also been shown to reduce gut microbiota diversity in mice, leading to a decrease in Gram-positive bacteria (e.g., Firmicutes) and an increase in Gram-negative bacteria (e.g., Proteobacteria) [30]. These changes may explain why MV patients are more prone to developing VAP after exposure to vancomycin and/or linezolid. Furthermore, a significant correlation between prior antibiotic exposure (≥ 3 types or ≥ 7 days) and VAP occurrence was revealed in this study. Several studies pointed out that the use of multiple antibiotics has a greater impact on the microbiota [31]. Additionally, Pérez-Cobas et al. found that antibiotics can influence the composition of the gut microbiota early in treatment, with microbiota diversity reaching its lowest point after 11 days of treatment [32]. The use of multiple antibiotics or prolonged antibiotic treatment may have a more significant impact on the microbiota and could be a contributing factor to the development of VAP.
This study has some limitations. Firstly, there is an inevitable selection bias in the design of the retrospective study, and the influence of unmeasured variables and unknown confounding factors cannot be ruled out in this study. Secondly, although this study is a multi-center study, the sample size was small, which may lead to lack certain generalization. In the future, we will continue to work on the potential threats of antibiotic exposure, especially for carbapenem antibiotics. In the next step, we will plan a multicenter and prospective study in this area, thus further testing our conclusions. Additionally, molecular biology and genomics methods can be used to study the association between antibiotic exposure and bacterial resistance, to reveal the specific mechanism of antibiotic resistance in the development of VAP in children, and to use microbiome technology to compare the intestinal and respiratory microbial composition of children with VAP and healthy controls to understand the effect of antibiotic exposure on the structure and function of microbial communities, and then explore how the gut-lung axis promotes the occurrence of VAP.
In summary, carbapenem exposure was an independent risk factor for the occurrence of VAP, especially when the duration was more than 7 days. For critically ill children, reducing carbapenem use and duration as much as possible should be considered.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- MV:
-
Mechanical ventilation
- VAP:
-
Ventilation-Associated Pneumonia
- PICU:
-
Pediatric Intensive Care Unit
- IVIG:
-
Intravenous immunoglobulin
- PCIS:
-
Pediatric Critical Illness Score
- PRISM III:
-
Pediatric Risk of Mortality Score III
References
Society AT, America IDSO. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. AM J RESP CRIT CARE 2005, 171(4).
Prevention CFDC. Pneumonia (ventilator-associated [VAP] and non-ventilator- associated pneumonia [PNEU]) event. In.; 2018.
Iosifidis E, Pitsava G, Roilides E. Ventilator-associated pneumonia in neonates and children: a systematic analysis of diagnostic methods and prevention. FUTURE MICROBIOL. 2018;13(12):1431–46.
Antalová N, Klučka J, Říhová M, Poláčková S, Pokorná A, Štourač P. Ventilator-Associated Pneumonia Prevention in Pediatric patients: Narrative Review. Children. 2022;9(10):1540.
Jaimes F, De La Rosa G, Gómez E, Múnera P, Ramírez J, Castrillón S. Incidence and risk factors for ventilator-associated pneumonia in a developing country: where is the difference? RESP MED 2007, 101(4).
Bassi GL, Xiol EA, Pagliara F, Hua Y, Torres A. Body position and Ventilator-Associated Pneumonia Prevention. SEMIN RESP CRIT CARE. 2017;38(3):371–80.
Niedzwiecka T, Patton D, Walsh S, Moore Z, O’Connor T, Nugent L. What are the effects of care bundles on the incidence of ventilator-associated pneumonia in paediatric and neonatal intensive care units? A systematic review. J SPEC PEDIATR NURS. 2019;24(4):e12264.
De Neef M, Bakker L, Dijkstra S, Raymakers-Janssen P, Vileito A, Ista E. Effectiveness of a Ventilator Care Bundle to Prevent Ventilator-Associated Pneumonia at the PICU: a systematic review and Meta-analysis. Pediatr Crit care Medicine: J Soc Crit Care Med World Federation Pediatr Intensive Crit Care Soc 2019, 20(5).
Pena-Lopez Y, Pujol M, Campins M, Gonzalez-Antelo A, Rodrigo JA, Balcells J, Rello J. Implementing a care bundle approach reduces ventilator-associated pneumonia and delays ventilator-associated tracheobronchitis in children: differences according to endotracheal or tracheostomy devices. INT J INFECT DIS. 2016;52:43–8.
Esteban E, Ferrer R, Urrea M, Suarez D, Rozas L, Balaguer M, Palomeque A, Jordan I. The impact of a quality improvement intervention to reduce nosocomial infections in a PICU. PEDIATR CRIT CARE ME. 2013;14(5):525–32.
Rosenthal VD, Alvarez-Moreno C, Villamil-Gomez W, Singh S, Ramachandran B, Navoa-Ng JA, Duenas L, Yalcin AN, Ersoz G, Menco A, et al. Effectiveness of a multidimensional approach to reduce ventilator-associated pneumonia in pediatric intensive care units of 5 developing countries: international nosocomial infection Control Consortium findings. AM J INFECT CONTROL. 2012;40(6):497–501.
Evans I, Phillips GS, Alpern ER, Angus DC, Friedrich ME, Kissoon N, Lemeshow S, Levy MM, Parker MM, Terry KM, et al. Association between the New York Sepsis Care Mandate and In-Hospital mortality for Pediatric Sepsis. JAMA-J AM MED ASSOC. 2018;320(4):358–67.
Sterling SA, Miller WR, Pryor J, Puskarich MA, Jones AE. The impact of timing of antibiotics on outcomes in severe Sepsis and septic shock: a systematic review and Meta-analysis. CRIT CARE MED 2015, 43(9).
Galal YS, Youssef MR, Ibrahiem SK. Ventilator-Associated Pneumonia: incidence, risk factors and outcome in paediatric intensive care units at Cairo University Hospital. J CLIN DIAGN RES. 2016;10(6):C6–11.
Matics TJ, Sanchez-Pinto LN. Adaptation and validation of a Pediatric Sequential Organ failure Assessment score and evaluation of the Sepsis-3 definitions in critically Ill Children. JAMA PEDIATR. 2017;171(10):e172352.
Kalil AC, Metersky ML, Klompas M, Muscedere J, Sweeney DA, Palmer LB, Napolitano LM, O’Grady NP, Bartlett JG, Carratala J, et al. Management of adults with hospital-acquired and ventilator-associated Pneumonia: 2016 clinical practice guidelines by the Infectious Diseases Society of America and the American Thoracic Society. CLIN INFECT DIS. 2016;63(5):e61–111.
Weiss SL, Peters MJ, Alhazzani W, Agus M, Flori HR, Inwald DP, Nadel S, Schlapbach LJ, Tasker RC, Argent AC, et al. Surviving sepsis campaign international guidelines for the management of septic shock and sepsis-associated organ dysfunction in children. INTENS CARE MED. 2020;46(Suppl 1):10–67.
Peng M, Hu M, Peng X, Gong Y, Qian K, Li J, Zhao J, Li X, Huang J, Zhang M, et al. What contributes to the re-positive nucleic acid test results for the omicron variant of SARS-CoV-2 in the shelter cabin hospital in Shanghai. China? HELIYON. 2023;9(5):e15679.
Seifu A, Eshetu O, Tafesse D, Hailu S. Admission pattern, treatment outcomes, and associated factors for children admitted to pediatric intensive care unit of Tikur Anbessa specialized hospital, 2021: a retrospective cross-sectional study. BMC ANESTHESIOL 2022, 22(1).
Safdar N, Crnich CJ, Maki DG. The pathogenesis of ventilator-associated pneumonia: its relevance to developing effective strategies for prevention. RESP CARE. 2005;50(6):725–39.
Maha A, Ziad AM, Hanan HB, Hala A, Abdulrahman A. Ventilator-Associated Pneumonia in a Pediatric Intensive Care Unit in Saudi Arabia: a 30-Month prospective surveillance. Infect Control Hosp Epidemiol 2004, 25(9).
Elward AM, Warren DK, Fraser VJ. Ventilator-associated pneumonia in pediatric intensive care unit patients: risk factors and outcomes. Pediatrics 2002, 109(5).
Vijay G, Mandal A, Sankar J, Kapil A, Lodha R, Kabra SK. Ventilator Associated Pneumonia in Pediatric Intensive Care Unit: incidence, risk factors and Etiological agents. Indian J Pediatr. 2018;85(10):861–6.
Vincent F, Jonathan M, David H, Véronique T, Stéphane G, Fatma M, Guilène B, Typhaine B, Catherine B, Didier D et al. Five-year trends for ventilator-associated pneumonia: correlation between microbiological findings and antimicrobial drug consumption. INT J ANTIMICROB AG 2015, 46(5).
Hu JN, Hu SQ, Li ZL, Bao C, Liu Q, Liu C, Xu SY. Risk factors of multidrug-resistant bacteria infection in patients with ventilator-associated pneumonia: a systematic review and meta-analysis. J INFECT CHEMOTHER. 2023;29(10):942–7.
Hensgens MP, Goorhuis A, Dekkers OM, Kuijper EJ. Time interval of increased risk for Clostridium difficile infection after exposure to antibiotics. J ANTIMICROB CHEMOTH. 2012;67(3):742–8.
Djordjevic ZM, Folic MM, Jankovic SM. Previous antibiotic exposure and antimicrobial resistance patterns of Acinetobacter spp. and Pseudomonas aeruginosa isolated from patients with nosocomial infections. BALK MED J. 2017;34(6):527–33.
Ignacio M, Robert D, Antoni T, Håkan H, Jeffrey L, Massimo A, Gennaro DP, Fernando B, Jean LV, Srinivas M et al. The importance of airway and lung microbiome in the critically ill. Crit Care (London England) 2020, 24(1).
Pultz NJ, Stiefel U, Donskey CJ. Effects of daptomycin, linezolid, and Vancomycin on establishment of intestinal colonization with Vancomycin-resistant enterococci and extended-spectrum-beta-lactamase-producing Klebsiella pneumoniae in mice. ANTIMICROB AGENTS CH. 2005;49(8):3513–6.
Anne V, Carolien O, Susana F, Lisanne J, Isaie R, Ruud SK, Els VN, Frits H, Max K, Johannes AR et al. Impact of oral Vancomycin on gut microbiota, bile acid metabolism, and insulin sensitivity. J HEPATOL 2014, 60(4).
Manuel F, Celia M, David R, Coral B, Andrés M. Antibiotic use and microbiome function. BIOCHEM PHARMACOL 2016, 134.
Perez-Cobas AE, Gosalbes MJ, Friedrichs A, Knecht H, Artacho A, Eismann K, Otto W, Rojo D, Bargiela R, von Bergen M, et al. Gut microbiota disturbance during antibiotic therapy: a multi-omic approach. Gut. 2013;62(11):1591–601.
Funding
Design of the study and collection, analysis and interpretation of data by fund from Suzhou Science and Technology Development Project (SKY2022178), GuSu Health Talent Training Project (GSWS2019050, GSWS2020044) and Special research project on infection management of Suzhou Hospital Association (SZSYYXH-2023-YB2). Writing the manuscript was supported by the Natural Science Foundation of Jiangsu Province (BK20210097, BK20211077) and Key Disciplines Support Project in Suzhou City (SZFCXK202134).
Author information
Authors and Affiliations
Contributions
XW, MZ: acquisition of data, or analysis and interpretation of data. SW, ZB: designed and drafted the work and substantively revised it for content. YZ, YG, LJ: made contributions to the conception. SH, XW, CS and WN: interpretation of data. All authors have approved the submitted version and agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Research Ethics Committee of Children’s Hospital of Soochow University (2023CS034) and First People’s Hospital of Lianyungang (LW-20231024003-01). Informed written consent to participate was obtained from the parents/guardians of the minors included in this study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, X., Zheng, M., Zhang, Y. et al. Prior carbapenem exposure increases the incidence of ventilator-associated pneumonia in critically Ill children. BMC Infect Dis 24, 855 (2024). https://doi.org/10.1186/s12879-024-09735-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09735-w