Abstract
Background
In the hospital environment, carbapenemase-producing Pseudomonas aeruginosa (CPPA) may lead to fatal patient infections. However, the transmission routes of CPPA often remain unknown. Therefore, this case study aimed to trace the origin of CPPA ST357, which caused a hospital-acquired pneumonia in a repatriated critically ill patient suffering from Guillain-Barré Syndrome in 2023.
Methods
Antimicrobial susceptibility of the CPPA isolate for 30 single and combination therapies was determined by disk-diffusion, Etest or broth microdilution. Whole-genome sequencing was performed for three case CPPA isolates (one patient and two sinks) and four distinct CPPA ST357 patient isolates received in the Dutch CPPA surveillance program. Furthermore, 193 international P. aeruginosa ST357 assemblies were collected via three genome repositories and analyzed using whole-genome multi-locus sequence typing in combination with antimicrobial resistance gene (ARG) characterization.
Results
A Dutch patient who carried NDM-1-producing CPPA was transferred from Kenya to the Netherlands, with subsequent dissemination of CPPA isolates to the local sinks within a month after admission. The CPPA case isolates presented an extensively drug-resistant phenotype, with susceptibility only for colistin and cefiderocol-fosfomycin. Phylogenetic analysis showed considerable variation in allelic distances (mean = 150, max = 527 alleles) among the ST357 isolates from Asia (n = 92), Europe (n = 58), Africa (n = 21), America (n = 16), Oceania (n = 2) and unregistered regions (n = 4). However, the case isolates (n = 3) and additional Dutch patient surveillance program isolates (n = 2) were located in a sub-clade of isolates from Kenya (n = 17; varying 15–49 alleles), the United States (n = 7; 21–115 alleles) and other countries (n = 6; 14–121 alleles). This was consistent with previous hospitalization in Kenya of 2/3 Dutch patients. Additionally, over half of the isolates (20/35) in this sub-clade presented an identical resistome with 9/17 Kenyan, 5/5 Dutch, 4/7 United States and 2/6 other countries, which were characterized by the blaNDM-1, aph(3’)-VI, ARR-3 and cmlA1 ARGs.
Conclusion
This study presents an extensively-drug resistant subclone of NDM-producing P. aeruginosa ST357 with a unique resistome which was introduced to the Netherlands via repatriation of critically ill patients from Kenya. Therefore, the monitoring of repatriated patients for CPPA in conjunction with vigilance for the risk of environmental contamination is advisable to detect and prevent further dissemination.
Similar content being viewed by others
Background
In the hospital, introductions of carbapenemase-producing Pseudomonas aeruginosa (CPPA) may lead to patient infection and mortality [1]; however, the exact origin of CPPA can often not be traced. Multiple case reports have suggested an association between CPPA introduction and medical treatment abroad [2,3,4,5,6,7]. The treatment of CPPA infections is a challenge, since it often presents a multidrug-resistant (MDR) or extensively drug-resistant (XDR) phenotype [8, 9]. Therefore, the World Health Organization has highlighted the critical need for the development of new antibiotics to combat CPPA infections [10]. Given the clinical risk CPPA poses, tracing the dissemination is pivotal to restrict further intra- and interhospital transmissions, in addition to enable evidence-based policy making.
Overall, various acquired carbapenemase-encoding genes have been reported in P. aeruginosa. Of these genes blaVIM appears to be the most ubiquitous, while other recurrent genes (blaIMP blaGES, blaKPC and blaNDM) present differences in geographical prevalence [1, 11]. Per example, blaNDM has been commonly reported in South- and Southeast Asia, and infrequently in Europe and North-America [1, 12, 13]. Furthermore, previous studies have shown that certain high-risk CPPA sequence types (ST) are endemic in different countries. For instance, the VIM-2-producing P. aeruginosa ST111 was predominant in the Netherlands [14], IMP-1-producing P. aeruginosa ST235 was the main lineage in Japan [15], and VIM-2-producing P. aeruginosa ST235 dominated in Russia [16]. Nonetheless, a wide diversity of less frequent sequence types can co-occur. In the Netherlands, a third of the CPPA isolates belonged to 21 sequence types other than ST111 between 2015 and 2017 [14]. The presence of these less frequent sequence types could be explained by dissemination through healthcare-related travel, such as medical evacuation, repatriation, and medical tourism. This is exemplified by a rare nation-wide outbreak of VIM-2-producing P. aeruginosa ST111 in the United States, which was determined to originate from bariatric surgery in Mexico [17]. Another example is the doubling of Ukrainian-related CPPA cases in the Netherlands, due to medical evacuation and migration of Ukrainians in 2022 [7].
The true scale at which intercontinental dissemination of CPPA occurs between health-care institutions is not clear. Surveillance studies have provided a molecular overview of CPPA prevalence in various geographic regions [8, 14, 18,19,20]. However, these studies are limited in the epidemiological scope. The reports on patient repatriation and medical tourism provide a detailed insight into the epidemiology underlying intercontinental CPPA transmission events. Still, these reports seldom touch upon the context of CPPA clone endemicity abroad.
Integration of both phylogenetics and antimicrobial resistance gene (ARG) characterization could potentially trace the origin of CPPA. In addition, repositories such as the NCBI Pathogen Detection Isolate Browser contain an assortment of international CPPA isolates which may provide a reference for CPPA endemicity abroad. Therefore, the aim of this case study was to trace the origin of CPPA ST357, which caused a hospital-acquired pneumonia in a repatriated critically ill patient suffering from Guillain-Barré Syndrome.
Methods
Patient screening
According to Dutch guidelines, patients admitted to the Intensive Care Unit (ICU) are routinely screened by oropharyngeal, nasopharyngeal and rectal culture for carbapenemase-producing Pseudomonas aeruginosa, Enterobacterales and Acinetobacter baumanii twice a week and upon admittance. Patient samples are enriched in tryptose phosphate broth (18 h, 35 °C, O2)(Tritium, Eindhoven, Netherlands) and subsequently cultured on selective MacConkey agar plates with ceftazidime-vancomycin and ceftriaxone-vancomycin (18 h, 35 °C, O2)(Tritium, Eindhoven, Netherlands). Isolates were identified by means of MALDI-TOF (Vitek MS, bioMérieux, Lyon, France).
Environmental screening
Environmental screening is not routinely employed, however, this study encompassed three sampling rounds (August 2022, March 2023, September 2023) of the ICU of a large medical center in the Netherlands. To screen for CPPA, all intensive care unit sink drains, faucet aerators, high-touch sites of medical devices and patient beds were sampled. Sink drains were sampled by inserting a flocked swab (eSwab, COPAN diagnostics, Murrieta, CA, USA) 5–7 cm into the sink drains at three equally spaced sites to reduce sampling bias. The samples were enriched in tryptose phosphate broth (18 h, 35 °C, O2)(Tritium, Eindhoven, Netherlands) and subsequently cultured on selective CHROMID ESBL plates (18 h, 35 °C, O2) (bioMérieux, Lyon, France). Isolates were identified by MALDI-TOF (Vitek MS, bioMérieux, Lyon, France).
Antimicrobial susceptibility testing
Susceptibility of one patient CPPA isolate and two environmental CPPA isolates to cefiderocol, ceftazidime, ciprofloxacin, meropenem, piperacillin-tazobactam and tobramycin was assessed by disk diffusion (Oxoid, Thermo Fisher Scientific, UK). Additional MIC values were determined for amikacin, aztreonam, cefiderocol, ceftazidime, ceftazidime-avibactam, ceftolozane-tazobactam, ciprofloxacin, fosfomycin, imipenem-relebactam, meropenem, meropenem-vaborbactam, piperacillin-tazobactam and tobramycin by gradient Etest (bioMérieux, Lyon, France). For colistin, MIC was determined by broth microdilution (Micronaut, MERLIN Diagnostika GmbH, Germany). The antimicrobials described above were tested and interpreted according to EUCAST guidelines (version 13.1) [21]. Antimicrobial synergy was examined by the MIC-cross method described previously [22, 23].
Whole-genome sequencing and genome assembly
Clinical CPPA isolates were sequenced within the Dutch national CPPA surveillance of the National Institute for Public Health and the Environment (RIVM) using the Illumina NextSeq550 platform with the Nextera DNA Flex Library Prep kit (Illumina, San Diego, USA) and the Oxford Nanopore technologies (ONT) GridION with the DNA V14 – barcoding SQK-RBK114.24 kit (Oxford Nanopore Technology, Oxford, UK). The environmental isolates were sequenced as part of the regional surveillance consortium, and processed at the Maastricht University Medical Center using the Illumina MiSeq with the Nextera XT Library Preparation kit (Illumina, San Diego, USA).
The FASTQ read quality was filtered using BBDuk v38.84 [24] to attain a minimum quality of Q25 and minimum read length of 36 bp for Illumina, while a minimum quality of Q10 and minimum read length of 500-bp were retained for ONT. Trimmed read quality was evaluated using Geneious Prime v2023.1.1 [25], with subsequent de novo assembly using SPAdes v3.15.5 [26] for Illumina reads and Flye v2.9.1 [27] for ONT reads.
Collection of international CPPA genomes
P. aeruginosa SNP clusters containing antimicrobial resistance gene (ARG) profiles that were comparable to the case isolate (RIVM_050529) were investigated in the NCBI Pathogen Detection Isolate Browser [28]. The following query criteria were applied: “Pseudomonas aeruginosa AND aac(6')-Il AND aadA1 AND ant(2'')-Ia AND aph(3')-IIb AND aph(3')-VI AND ARR-3 AND blaNDM-1 AND blaOXA-10 AND blaOXA-846 AND blaVEB-9 AND catB7 AND cmlA1 AND crpP AND fosA AND sul1 AND tet(A) AND blaPDC-11”. All the available FASTA assemblies and metadata within the matching SNP cluster were extracted for comparative analysis. Additional assemblies and metadata of P. aeruginosa ST357 genomes were acquired via the Bacterial and Viral Bioinformatics Resource Center (BV-BRC) [29] and the Pseudomonas Genome Database [30].
Whole-genome analyses
An ad hoc whole-genome multi-locus sequencing typing (wgMLST) scheme for P. aeruginosa ST357 was developed by annotation of all assemblies with Prokka v1.14.5 [31] and pangenome analysis using Roary v3.13.0 [32]. The wgMLST scheme consisted of 15835 loci, of which 5662 loci were present in 90% of the assemblies. The allelic distances between strains were calculated with pyMLST v2.1.5 [33], missing alleles were omitted from this analysis. Allelic distances were applied to construct a phylogenetic tree by means of the UPGMA method in ape v5.7–1 [34], and were visualized by means of ggtree v3.8.1 [35, 36]. The resistance markers and multilocus sequence typing (MLST) were determined in the staramr pipeline v0.9.1 [37], which incorporates the ResFinder database v24-05–2022 [38, 39] and the PubMLST database [40] using the MLST v2.23.0 tool [41]. The presence of the resistance markers was plotted into a heatmap with ggplot2 v3.4.3 [42]. Type III secretion system (T3SS) effector genes were identified in the Virulence Factor Database [43]. The P. aeruginosa O-specific antigen was typed using PAst v1.0 [44]. Additional visualizations of the P. aeruginosa assemblies were created in Geneious Prime with annotation of integrons by Integron Finder v2.0.2 [45] and insertion sequences via the ISFinder database [46].
Results
Case description
In February 2023, a young Dutch individual was hospitalized with paresis development similar to Guillain-Barré Syndrome (GBS) in Zanzibar, Tanzania. Three days prior to admission, the patient had suffered from increasingly deteriorating right-sided hemiparesis. Three days after admission, the patient was transferred due to increasing severity of symptoms to the ICU of a referral hospital in Nairobi, Kenya. The patient developed aspiration pneumonia, which led to mechanical ventilation via a tracheostomy and administration of amoxicillin/clavulanic acid (dosage unknown), 7 days after initial admission. In the following 4 days, the patient received additional piperacillin/tazobactam (dosage unknown) due to increased fever and CRP-values. This was subsequently changed to ciprofloxacin (dosage unknown) after an Enterobacter cloacae complex isolate (antibiogram unknown) was cultured from sputum, 13 days after admission. The patient was eventually repatriated to the Netherlands via a ventilator-assisted transcontinental flight following 18 days of hospitalization abroad.
Upon admission to the Dutch ICU ward (Zuyderland MC, Netherlands), the patient was placed in single patient isolation room A. The tracheostomy tube was replaced and the patient was given piperacillin/tazobactam (4.5 g, 4 d.d.) empirically from day 19 until day 21. In addition, an initial oropharyngeal swab was acquired, from which a CPPA isolate (RIVM_C050529) was cultured. Furthermore, a CPPA was cultured from a bronchial secretion which was acquired on day 23, and the patient was administered a combination of meropenem (2 g, 3 d.d.) and colistin IV (3 MIU, 3 d.d.) from day 26 to day 28. The patient developed symptoms similar to locked-in syndrome and suffered from seclusion-induced anxiety in the isolation room. Therefore, the patient was transferred to the standard ICU room B adjacent to the nurses’ station 25 days after initial hospitalization. Furthermore, the patient’s situation deteriorated since the P. aeruginosa infection which caused the pneumonia was unresponsive to meropenem and colistin. Based on additional antimicrobial resistance testing, the patient was switched to a combination treatment of cefiderocol (1 g, 4 d.d.) and intravenous fosfomycin (4 g, 2 d.d.) from day 34 until day 51. This therapy appeared effective and resulted in clinical improvement. Further treatment with nebulized colistin (2 MIU, 2 d.d.) from day 47 until day 71 prevented reinfection, but not the P. aeruginosa colonization. The patient was transferred to a rehabilitation clinic and given a single patient room and sanitary facilities, 72 days after initial admittance. Follow-up screening by oropharyngeal, nasopharyngeal and rectal swabs remained positive for the CPPA until 190 days after initial admittance, followed by four successive negative screening-cultures spanning 78 days.
An environmental screening of the ICU ward during the patient’s admittance exposed sink drain colonization with a CPPA isolate in isolation room A (TY-ZU-0087) and standard room B (TY-ZU-0088), 34 days after the patient’s initial hospitalization. This CPPA appeared to be an introduction to the ICU since 7 months earlier environmental screening provided no cultures of XDR or MDR P. aeruginosa isolates. After assessment of the ICU procedures, it was hypothesized that removal of subglottic secretions from the patient’s tracheal tube was the most likely source of CPPA colonization in the sink drains. Due to the well-characterized risk of P. aeruginosa to colonize patients from the sink drain environment [47,48,49,50], the decision was made to immediately cap-off all sink drains linked to room A and room B. In addition, a permanent water-free patient care protocol was instituted and all sinks in the ICU patient rooms were removed. In addition, the reusable and washable tracheal tubes have been banned and were replaced by disposable tracheal tubes on an institutional level. Environmental follow-up screening of the ICU’s remaining faciliatory sinks two months after the patient’s transfer, did not reveal any suspected XDR or MDR P. aeruginosa isolates. In addition, no transmission to other patients was detected. After the patients discharge from the rehabilitation center, all the sanitary facilities and the adjacent sewage network were replaced.
Phenotypic and genotypic characterization of case isolates
Disk diffusion and gradient test showed that the isolates RIVM_C050529, TY-ZU-0087 and TY-ZU-0088 were resistant to all first and second line antibiotics. Table 1 presents the antimicrobial susceptibility profiles for each isolate according to EUCAST v14.0. Additionally, isolate RIVM_C050529 was resistant to the novel last-resort antibiotics cefiderocol, ceftazidime-avibactam, ceftolozane-tazobactam, imipenem-relebactam, meropenem-vaborbactam. Synergy testing (Table 1) of this isolate revealed borderline sensitivity to cefiderocol (2 µg/ml) when combined with fosfomycin or amikacin. In contrast, none of the other tested synergies appeared to lower the MIC. Genomic analysis of short-read sequencing data characterized the case isolates as high-risk ST357/O11 clones containing the T3SS effector genes exoT, exoU and exoY. All three isolates carried a vast array of ARG (Table 2), including the carbapenemase gene blaNDM-1, beta-lactamase genes blaOXA-10, blaOXA-50 and blaPAO, extended spectrum beta-lactamase gene blaVEB-1, aminoglycoside resistance genes aac(6')-Il, aadA1, ant(2'')-Ia, aph(3')-IIb and aph(3')-VI, and the ciprofloxacin resistance gene crpP. In addition, point mutations were detected in the gyrA (T83I) and parC (S87L) genes, which confer resistance to ciprofloxacin. Of the genes presented in Table 2, aph(3')-IIb, blaOXA-50 blaPAO, catB7 and fosA are part of the intrinsic resistome of P. aeruginosa.
Phylogenetic analysis with international P. aeruginosa ST357 isolates
To trace the potential geographic origin of case isolate RIVM_C050529, we first examined a set of 4 additional clinical CPPA isolates with ST357 that were detected in the Dutch national CPPA surveillance program. As shown in Table 2, three of these isolates were linked to previous travel and hospitalization abroad in Kenya and Somalia. In addition, three of these isolates harbored the blaNDM-1 gene and one isolate harbored blaIMP-7, while two isolates had identical resistomes to RIVM_C050529. Since these isolates were associated with international travel, the NCBI Pathogen Detection Isolate Browser was queried for P. aeruginosa isolates with similar resistomes. Altogether, 29 isolates with identical resistomes were identified. All these isolates were included in a single cluster (PSD000019917) containing 133 isolates varying 0 to 104 SNPs, with a mean of 41 SNPs (accessed September 2023). All available genome assemblies and corresponding metadata in this cluster were extracted (n = 103). In addition, available non-duplicate P. aeruginosa ST357 genome assembly and metadata were extracted from BV-BRC and the Pseudomonas Genome Database (n = 90). The extracted isolates originated from varying geographic regions including Asia (n = 92), Europe (n = 58), Africa (n = 21), North America (n = 11), South America (n = 5),Oceania (n = 2) and unregistered regions (n = 4) (Additional file 1).
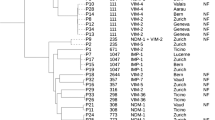
Figure 1 presents the UPGMA tree of CPPA ST357 from the Netherlands in context with internationally obtained ST357 isolates based on wgMLST allelic distances (Additional file 2; Additional file 3). Overall, the genotypic diversity varied considerably, with on average 150 alleles difference between isolates and the largest distance being 527 alleles. Three of five Dutch patient isolates (RIVM_C015245, RIVM_C042465, RIVM_050529) and the two Dutch sink drain isolates (n = 2) clustered in a single clade with 30 international isolates from Kenya (n = 17), United States (n = 7), India (n = 3), Australia (n = 1), Singapore (n = 1) and Tanzania (n = 1) (mean of 29 alleles). All three Dutch patient isolates presented the closest resemblance to the Kenyan isolates (varying 14–31 alleles), followed by the United States isolates (varying 21–38 alleles). This is in accordance with the preceding hospitalization in Kenya related to isolates RIVM_C042465 and RIVM_050529, but not RIVM_C015245. The Dutch sink drain isolates TY-ZU-0086 and TY-ZU-0087 showed the highest degree of similarity to RIVM_C050529 (varying 14–19 alleles). This, in combination with the absence of XDR P. aeruginosa during an earlier environmental screening, supports the hypothesis that these strains were likely introduced to the sink drains via evacuation of the patient’s tracheal tube.
The patient isolate RIVM_C044827 which was linked to previous hospital admission in India, did not appear to directly cluster. However, there were three Indian isolates which showed the highest genotypic similarity (74–77 alleles). Lastly, patient isolate RIVM_C048676 without a link to foreign hospitalization presented a 48–99 allelic difference with six Czech isolates and one German isolate.
Resistome analysis with international P. aeruginosa ST357 isolates
The sub-clade to which the three Dutch patient isolates with identical resistomes belonged, additionally contained international isolates with an identical resistome Fig. 2. This resistome was found in 9 of 17 of the Kenyan, 4 of 7 of the United States isolates, as well as a single Australian and Tanzanian isolate. In contrast, only 3 of the other 165 isolates outside of this subclade contained a resistome that was identical to RIVM_C050529, since the combination of blaNDM-1, APH-3’(VI), ARR-3 and cmlA1 was absent (Additional file 4). Although these three isolates were similar based on the resistome, they were very distantly genotypically related to RIVM_050529 with 220 to 343 allelic differences. To further explore the resistome of the isolates in de Dutch-Kenyan-United States clade, the genomic structure of isolate RIVM_C042465 was analyzed using the long-read ONT data. This resulted in a single chromosome which contained multiple clinically relevant ARG on a resistance island spanning about 37.4 kb (Fig. 3). This resistance island consisted of two distinct intI integrase-associated gene cassettes, which carried among others the beta-lactamase gene blaoxa-10 and tobramycin resistance gene ant(2’’)-Ia. Furthermore, the typical ISAba125–blaNDM-1–ble element which causes carbapenem-resistance was identified. Of the two remaining Dutch isolates, one (RIVM_C048676) also presented an identical resistome to 5/6 Czech isolate with less than 100 alleles difference (Additional file 4). While for isolate RIVM_C044827 no identical resistomes were detected in the international dataset.
Discussion
The aim of this case study was to trace the origin of CPPA ST357, which caused a hospital-acquired pneumonia in a repatriated critically ill patient suffering from Guillain-Barré Syndrome. Therefore, assemblies of Dutch and global isolates were analyzed to attain a high-resolution overview of CPPA ST357 sub-clades by means of whole-genome phylogenetics and ARG characterization. This approach demonstrated the potential to trace the origin of CPPA isolates related to repatriated patients using genomic epidemiology.
A significant finding for this study was that three unique Dutch CPPA ST357 patient isolates belonged to a sub-clade which was largely composed of isolates from Kenya and the United States. This indicated international transmission, which was in accordance with previous repatriation of two Dutch patients from Kenya. Furthermore, this sub-clade could be further characterized by a blaNDM-1-carrying resistance island which induced the XDR phenotype.
These findings are in line with a series of case reports which presented novel CPPA in regions where the endemicity was relatively low and associations of these introductions with preceding medical treatment abroad. While transmission of MDR bacteria is a global and common occurrence, cross-national transmission is rarely traced and confirmed via genomic epidemiology. Such as the study on the CPPA ST111 outbreak in the United States which was derived from medical tourism in Mexico [17], and the outbreak of methicillin-resistant Staphylococcus aureus ST239 in Portugal, which likely originated from South America [51]. Similar to these studies, the current findings have shown that international transmissions of CPPA ST357 belonging to a single sub-clade may occur independently from each other, can be linked to the same geographic region and is ultimately a potential risk for further domestic dissemination. Interestingly, the distinction of the CPPA ST357 blaNDM-1 sub-clade with the co-occurrence of a unique resistome is consistent with other independent observations, which similarly associated the presence of specific ARGs to variation in P. aeruginosa lineages [18, 52].
The Kenyan isolates which were included in the sub-clade were derived from two studies which collected these isolates from six Kenyan medical centers in the period 2015–2020 [19, 20]. Even though 16 of these CPPA ST357 isolates were derived from Nairobi in 2018 and 2019, the endemic dissemination of this sub-clone is not directly evident due to the limited number of participating centers in Nairobi. However, a similar isolate was found in the adjacent Tanzania as early as 2014. This, in addition to the two Dutch isolates of patients admitted in Kenya (Nairobi), support that the clone in this sub-clade is likely endemic to the region.
The ad hoc wgMLST-based allelic distances were unexpectedly high between the patient case isolate RIVM_050529 and the two epidemiologically linked sink isolates (14 and 19 alleles). In contrast, the 16 related Kenyan (Nairobi) isolates included in this study presented only 0 to 18 allelic differences. Previous studies based on a BioNumerics P. aeruginosa wgMLST scheme have shown a range of 0 to 17 allelic differences for epidemiologically linked (outbreak) isolates [49, 53]. While another study presented a range of 0–59 alleles for ST357 isolates from two Indonesian ICUs over the course of 33 months [54]. The allelic distance between the patient case isolate and the two sink isolate might have been caused by differences in the wet-lab protocol rather than the genomic analysis. A benchmarking study for whole-genome short-read sequencing of foodborne microbial pathogens has shown that the use of the Nextera XT DNA library prep kit compared to other Illumina library preparation kits introduced additional allelic differences in a core-genome MLST [55].
Another unanticipated finding was that the Dutch patient RIVM_015245, which was linked to preceding hospitalization in Belgium, was included in the Kenyan sub-clade. To our knowledge, no other P. aeruginosa ST357 from Belgium has previously been reported. Due to the high similarity with the other Kenyan isolates, a possible explanation may be that the preceding travel history of the patient was not complete. Another unexpected finding were four isolates from Minnesota, United States, which presented a close genotypic resemblance to the Dutch and Kenyan isolates of the sub-clade. It is unlikely that these strains have been domestically acquired, since the CPPA prevalence in the United States only contributes to approximately 2 to 4% of all carbapenem-resistant P. aeruginosa [1, 56, 57]. In addition, these studies only reported a 0% to 6% blaNDM-1 prevalence in these CPPA isolates.
For infection prevention and control, the practice of tracing the origin of a novel CPPA or other nosocomial pathogens is one reliant on a combination of available epidemiological and laboratory data [58]. This procedure is often limited by incomplete epidemiological data or the discriminatory power of typing methods such as MLST. For instance, even if a CPPA introduction is linked to foreign hospitalization, this link does not completely exclude the possibility that transmission may have occurred through the local hospital environment. Although, the understanding of intra- and inter-hospital transmissions has increased with the rise of WGS-based approach for CPPA [47,48,49,50, 59], international dissemination still constitutes a challenge. Through a thorough investigation of the domestic and international isolates, we have shown that the patient-to-sink CPPA transmission which occurred in the previously uncolonized sinks were indeed of a non-domestic origin. Therefore, the current study may provide an example for the investigations of additional international transmission events and thus may contribute to optimal infection control measures.
There are some potential drawbacks which apply to the current study. The genomes compared in this study have been assembled using different assembly methods which introduces a degree of bias between the genomes. Additionally, the current study analyzed a few CPPA isolates of a single sequence type which were related to foreign hospitalization. It is unknown if the approach used in this study can be applied to a broader spectrum of CPPA sequence types.
The current approach is dependent on a worldwide coverage of well-characterized CPPA strains analyzed by means of WGS, so that these strains can be used as a reference. Therefore, it is beneficial that endemic CPPA strains are characterized in countries with a limited coverage, such as the studies performed in Kenya by Musila et al. (2021) and Kiyaga et al. (2022) [19, 20].
This study presents an XDR subclone of CPPA ST357 with a unique resistance island which has been introduced to the Netherlands via repatriation of critically ill patients from Kenya. Travel of persons and repatriation of patients from countries with a high CPPA endemicity to countries with a low CPPA endemicity will remain an irrevocable challenge for patient safety. Therefore, the monitoring of repatriated patients for CPPA in conjunction with vigilance for the risk of environmental contamination is advisable to detect and prevent further dissemination.
Availability of data and materials
The datasets supporting the conclusions of this article are available in the SRA repository, under BioProject accession PRJNA1095851 (https://www.ncbi.nlm.nih.gov/bioproject/PRJNA1095851). The corresponding metadata of each isolate used in this study are available in Additional file 1.
References
Reyes J, Komarow L, Chen L, Ge L, Hanson BM, Cober E, et al. Global epidemiology and clinical outcomes of carbapenem-resistant Pseudomonas aeruginosa and associated carbapenemases (POP): a prospective cohort study. Lancet Microbe. 2023;4(3):e159–70.
Baba H, Kanamori H, Katsumi M, Sato T, Chida T, Ikeda S, et al. A case of meningitis due to extensively drug-resistant Pseudomonas aeruginosa imported through medical evacuation: genomic and environmental investigation. J Travel Med. 2021;28(6):taab047. https://doi.org/10.1093/jtm/taab047.
Samuelsen O, Toleman MA, Sundsfjord A, Rydberg J, Leegaard TM, Walder M, et al. Molecular epidemiology of metallo-beta-lactamase-producing Pseudomonas aeruginosa isolates from Norway and Sweden shows import of international clones and local clonal expansion. Antimicrob Agents Chemother. 2010;54(1):346–52.
Compain F, Decré D, Frazier I, Ramahefasolo A, Lavollay M, Carbonnelle E, et al. Carbapenemase-producing bacteria in patients hospitalized abroad. France Emerg Infect Dis. 2014;20(7):1246–8.
Khan A, Shropshire WC, Hanson B, Dinh AQ, Wanger A, Ostrosky-Zeichner L, et al. Simultaneous Infection with Enterobacteriaceae and Pseudomonas aeruginosa Harboring Multiple Carbapenemases in a Returning Traveler Colonized with Candida auris. Antimicrob Agents Chemother. 2020;64(2):1466.
Berger O, Lurie-Weinberger MN, Tsyba E, Talisman R. ST773 Pseudomonas aeruginosa wound infection as a result of medical tourism to Turkey. J Travel Med. 2023;31(1):taad097.
Zwittink RD, Wielders CC, Notermans DW, Verkaik NJ, Schoffelen AF, Witteveen S, et al. Multidrug-resistant organisms in patients from Ukraine in the Netherlands, March to August 2022. Euro Surveill. 2022;27(50):2200896. https://doi.org/10.2807/1560.
Del Barrio-Tofiño E, López-Causapé C, Cabot G, Rivera A, Benito N, Segura C, et al. Genomics and susceptibility profiles of extensively drug-resistant pseudomonas aeruginosa Isolates from Spain. Antimicrob Agents Chemother. 2017;61(11):1589.
Kos VN, Déraspe M, McLaughlin RE, Whiteaker JD, Roy PH, Alm RA, et al. The resistome of Pseudomonas aeruginosa in relationship to phenotypic susceptibility. Antimicrob Agents Chemother. 2015;59(1):427–36.
Tacconelli E, Carrara E, Savoldi A, Harbarth S, Mendelson M, Monnet DL, et al. Discovery, research, and development of new antibiotics: the WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infect Dis. 2018;18(3):318–27.
Wang M, Liu Z, Liao X, Sun R, Li R, Liu Y, et al. Retrospective Data Insight into the Global Distribution of Carbapenemase-Producing Pseudomonas aeruginosa. Antibiotics (Basel). 2021;10(5):548. https://doi.org/10.3390/antibiotics10050548.
Kazmierczak KM, de Jonge BLM, Stone GG, Sahm DF. Longitudinal analysis of ESBL and carbapenemase carriage among Enterobacterales and Pseudomonas aeruginosa isolates collected in Europe as part of the International Network for Optimal Resistance Monitoring (INFORM) global surveillance programme, 2013–17. J Antimicrob Chemother. 2020;75(5):1165–73.
Lee Y, Ko W, Hsueh P. Geographic Patterns of Carbapenem-Resistant Pseudomonas aeruginosa in the Asia-Pacific Region: Results from the Antimicrobial Testing Leadership and Surveillance (ATLAS) Program, 2015–2019. Antimicrob Agents Chemother. 2022;66(2):e0200021.
Pirzadian J, Persoon MC, Severin JA, Klaassen CHW, de Greeff SC, Mennen MG, et al. National surveillance pilot study unveils a multicenter, clonal outbreak of VIM-2-producing Pseudomonas aeruginosa ST111 in the Netherlands between 2015 and 2017. Sci Rep. 2021;11(1):21015.
Miyoshi-Akiyama T, Tada T, Ohmagari N, Viet Hung N, Tharavichitkul P, Pokhrel BM, et al. Emergence and Spread of Epidemic Multidrug-Resistant Pseudomonas aeruginosa. Genome Biol Evol. 2017;9(12):3238–45.
Edelstein MV, Skleenova EN, Shevchenko OV, D’souza JW, Tapalski DV, Azizov IS, et al. Spread of extensively resistant VIM-2-positive ST235 Pseudomonas aeruginosa in Belarus, Kazakhstan, and Russia: a longitudinal epidemiological and clinical study. Lancet Infect Dis. 2013;13(10):867–76.
Kracalik I, Ham DC, McAllister G, Smith AR, Vowles M, Kauber K, et al. Extensively drug-resistant carbapenemase-producing pseudomonas aeruginosa and medical tourism from the United States to Mexico, 2018–2019. Emerg Infect Dis. 2022;28(1):51–61.
Diorio-Toth L, Irum S, Potter RF, Wallace MA, Arslan M, Munir T, et al. Genomic surveillance of clinical pseudomonas aeruginosa isolates reveals an additive effect of Carbapenemase production on carbapenem resistance. Microbiol Spectr. 2022;10(3):e0076622-e76722. Epub 2022 May 31.
Kiyaga S, Kyany’a C, Muraya AW, Smith HJ, Mills EG, Kibet C, et al. Genetic Diversity, Distribution, and Genomic Characterization of Antibiotic Resistance and Virulence of Clinical Pseudomonas aeruginosa Strains in Kenya. Front Microbiol. 2022;13:835403.
Musila L, Kyany’a C, Maybank R, Stam J, Oundo V, Sang W. Detection of diverse carbapenem and multidrug resistance genes and high-risk strain types among carbapenem non-susceptible clinical isolates of target gram-negative bacteria in Kenya. PLoS ONE. 2021;16(2):e0246937.
The European Committee on Antimicrobial Susceptibility Testing. Breakpoint tables for interpretation of MICs and zone diameters, version 14.0. 2024. https://www.eucast.org/clinical_breakpoints. Accessed 8 Feb 2024.
Okoliegbe IN, Hijazi K, Cooper K, Ironside C, Gould IM. Antimicrobial synergy testing: comparing the tobramycin and ceftazidime gradient diffusion methodology used in assessing synergy in cystic fibrosis-derived multidrug-resistant pseudomonas aeruginosa. Antibiotics (Basel). 2021;10(8):967. https://doi.org/10.3390/antibiotics10080967.
Pankey GA, Ashcraft DS, Dornelles A. Comparison of 3 Etest(®) methods and time-kill assay for determination of antimicrobial synergy against carbapenemase-producing Klebsiella species. Diagn Microbiol Infect Dis. 2013;77(3):220–6.
Bushnell B. BBTools software package. 2014. https://sourceforge.net/projects/bbmap/. Accessed 1 Feb 2024.
Geneious Prime 2023.1.1. https://www.geneious.com/. Accessed 1 Feb 2024.
Bankevich A, Nurk S, Antipov D, Gurevich AA, Dvorkin M, Kulikov AS, et al. SPAdes: a new genome assembly algorithm and its applications to single-cell sequencing. J Comput Biol. 2012;19(5):455–77.
Kolmogorov M, Yuan J, Lin Y, Pevzner PA. Assembly of long, error-prone reads using repeat graphs. Nat Biotechnol. 2019;37(5):540–6.
The NCBI Pathogen Detection Project. Bethesda (MD): National Library of Medicine (US), National Center for Biotechnology Information. The NCBI Pathogen Detection Project. 2016. Available at: https://www.ncbi.nlm.nih.gov/pathogens/. Accessed 17 Aug. 2023.
Olson RD, Assaf R, Brettin T, Conrad N, Cucinell C, Davis JJ, et al. Introducing the Bacterial and Viral Bioinformatics Resource Center (BV-BRC): a resource combining PATRIC. IRD and ViPR Nucleic Acids Res. 2023;51(D1):D678–89.
Winsor GL, Lam DKW, Fleming L, Lo R, Whiteside MD, Yu NY, et al. Pseudomonas Genome Database: improved comparative analysis and population genomics capability for Pseudomonas genomes. Nucleic Acids Res. 2011;39(Database issue):596.
Seemann T. Prokka: rapid prokaryotic genome annotation. Bioinformatics. 2014;30(14):2068–9.
Page AJ, Cummins CA, Hunt M, Wong VK, Reuter S, Holden MTG, et al. Roary: rapid large-scale prokaryote pan genome analysis. Bioinformatics. 2015;31(22):3691–3.
Biguenet A, Bordy A, Atchon A, Hocquet D, Valot B. Introduction and benchmarking of pyMLST: open-source software for assessing bacterial clonality using core genome MLST. Microb Genom. 2023;9(11):001126. https://doi.org/10.1099/mgen.0.001126.
Paradis E, Schliep K. ape 5.0: an environment for modern phylogenetics and evolutionary analyses in R. Bioinformatics. 2019;35(3):526–8.
Yu G, Smith DK, Zhu H, Guan Y, Lam TT. ggtree: an r package for visualization and annotation of phylogenetic trees with their covariates and other associated data. Methods Ecol Evol. 2017;8(1):28–36.
Xu S, Dai Z, Guo P, Fu X, Liu S, Zhou L, et al. ggtreeExtra: Compact visualization of richly annotated phylogenetic data. Mol Biol Evol. 2021;38(9):4039–42.
Bharat A, Petkau A, Avery BP, Chen JC, Folster JP, Carson CA, et al. Correlation between Phenotypic and in silico detection of antimicrobial resistance in Salmonella enterica in Canada Using Staramr. Microorganisms. 2022;10(2):292. https://doi.org/10.3390/microorganisms10020292.
Camacho C, Coulouris G, Avagyan V, Ma N, Papadopoulos J, Bealer K, et al. BLAST+: architecture and applications. BMC Bioinformatics. 2009;10:421–421.
Bortolaia V, Kaas RS, Ruppe E, Roberts MC, Schwarz S, Cattoir V, et al. ResFinder 4.0 for predictions of phenotypes from genotypes. J Antimicrob Chemother. 2020;75(12):3491–500.
Jolley KA, Bray JE, Maiden MCJ. Open-access bacterial population genomics: BIGSdb software, the PubMLST .org website and their applications. Wellcome Open Res. 2018;3:124.
Seeman T, Stroehlein A, Goncalves da Silva A. mlst. 2023. https://github.com/tseemann/mlst. Accessed 23 Feb 2024.
Wickham H. ggplot2: Elegant Graphics for Data Analysis. New York: Springer-Verlag; 2009.
Chen L, Yang J, Yu J, Yao Z, Sun L, Shen Y, et al. VFDB: a reference database for bacterial virulence factors. Nucleic Acids Res. 2005;33(Database issue):325.
Thrane SW, Taylor VL, Lund O, Lam JS, Jelsbak L. Application of whole-genome sequencing data for o-specific antigen analysis and in silico serotyping of Pseudomonas aeruginosa Isolates. J Clin Microbiol. 2016;54(7):1782–8.
Néron B, Littner E, Haudiquet M, Perrin A, Cury J, Rocha EPC. IntegronFinder 2.0: identification and analysis of integrons across bacteria, with a focus on antibiotic resistance in Klebsiella. microorganisms. 2022;10(4):700. https://doi.org/10.3390/microorganisms10040700.
Siguier P, Perochon J, Lestrade L, Mahillon J, Chandler M. ISfinder: the reference centre for bacterial insertion sequences. Nucleic Acids Res. 2006;34(Database issue):32.
Catho G, Martischang R, Boroli F, Chraïti MN, Martin Y, Koyluk Tomsuk Z, et al. Outbreak of Pseudomonas aeruginosa producing VIM carbapenemase in an intensive care unit and its termination by implementation of waterless patient care. Crit Care. 2021;25(1):301-y.
de Jonge E, de Boer MGJ, van Essen EHR, Dogterom-Ballering HCM, Veldkamp KE. Effects of a disinfection device on colonization of sink drains and patients during a prolonged outbreak of multidrug-resistant Pseudomonas aeruginosa in an intensive care unit. J Hosp Infect. 2019;102(1):70–4.
De Geyter D, Vanstokstraeten R, Crombé F, Tommassen J, Wybo I, Piérard D. Sink drains as reservoirs of VIM-2 metallo-β-lactamase-producing Pseudomonas aeruginosa in a Belgian intensive care unit: relation to patients investigated by whole-genome sequencing. J Hosp Infect. 2021;115:75–82.
Schärer V, Meier M, Schuepbach RA, Zinkernagel AS, Boumasmoud M, Chakrakodi B, et al. An intensive care unit outbreak with multi-drug-resistant Pseudomonas aeruginosa - spotlight on sinks. J Hosp Infect. 2023;139:161–7.
Harris SR, Feil EJ, Holden MTG, Quail MA, Nickerson EK, Chantratita N, et al. Evolution of MRSA during hospital transmission and intercontinental spread. Science. 2010;327(5964):469–74.
Freschi L, Vincent AT, Jeukens J, Emond-Rheault J, Kukavica-Ibrulj I, Dupont M, et al. The pseudomonas aeruginosa Pan-genome provides new insights on its population structure, horizontal gene transfer, and pathogenicity. Genome Biol Evol. 2019;11(1):109–20.
Blanc DS, Magalhães B, Koenig I, Senn L, Grandbastien B. Comparison of Whole Genome (wg-) and Core Genome (cg-) MLST (BioNumerics(TM)) Versus SNP Variant Calling for Epidemiological Investigation of Pseudomonas aeruginosa. Front Microbiol. 2020;11:1729.
Goyal M, Pelegrin AC, Jaillard M, Saharman YR, Klaassen CHW, Verbrugh HA, et al. Whole genome multi-locus sequence typing and genomic single nucleotide polymorphism analysis for epidemiological typing of Pseudomonas aeruginosa from Indonesian intensive care units. Front Microbiol. 2022;13:861222.
Forth LF, Brinks E, Denay G, Fawzy A, Fiedler S, Fuchs J, et al. Impact of wet-lab protocols on quality of whole-genome short-read sequences from foodborne microbial pathogens. Front Microbiol. 2023;14:1253362.
Vallabhaneni S, Huang JY, Grass JE, Bhatnagar A, Sabour S, Lutgring JD, et al. Antimicrobial susceptibility profiles to predict the presence of Carbapenemase genes among carbapenem-resistant Pseudomonas aeruginosa Isolates. J Clin Microbiol. 2021;59(6):2874.
Walters MS, Grass JE, Bulens SN, Hancock EB, Phipps EC, Muleta D, et al. Carbapenem-resistant pseudomonas aeruginosa at US emerging infections program sites, 2015. Emerg Infect Dis. 2019;25(7):1281–8.
Peacock SJ, Parkhill J, Brown NM. Changing the paradigm for hospital outbreak detection by leading with genomic surveillance of nosocomial pathogens. Microbiology (Reading). 2018;164(10):1213–9.
Pirzadian J, Voor In ‘t Holt AF, Hossain M, Klaassen CHW, de Goeij I, Koene HHHT, et al. Limiting spread of VIM-positive Pseudomonas aeruginosa from colonized sink drains in a tertiary care hospital: A before-and-after study. PLoS One 2023;18(3):0282090.
Acknowledgements
We acknowledge and thank all the members of the study groups and surveillance programs for submitting CPPA isolates to NCBI. A detailed listing for each isolate can be found in Additional file 1.
We thank all the members of the Dutch CPE/CPPA surveillance study group and the Dutch medical microbiology laboratories for submitting Pseudomonas aeruginosa isolates to the RIVM for the national CPPA surveillance program.
Members of the Dutch CPE Surveillance Study Group
• A.L.E. van Arkel, ADRZ medisch centrum, Department of Medical Microbiology, Goes.
• M.A. Leversteijn-van Hall, Alrijne Hospital, Department of Medical Microbiology, Leiden.
• W. van den Bijllaardt, Amphia Hospital, Microvida Laboratory for Microbiology, Breda.
• R. van Mansfeld, Amsterdam UMC—location AMC, Department of Medical Microbiology and Infection Prevention, Amsterdam.
• K. van Dijk, Amsterdam UMC—location Vumc, Department of Medical Microbiology and Infection Control, Amsterdam.
• B. Zwart, Atalmedial, Department of Medical Microbiology, Amsterdam.
• B.M.W. Diederen, Bravis Hospital/ZorgSaam Hospital Zeeuws-Vlaanderen, Department of Medical Microbiology, Roosendaal/Terneuzen.
• H. Berkhout, Canisius Wilhelmina Hospital, Department of Medical Microbiology and Infectious Diseases, Nijmegen.
• D.W. Notermans, Centre for Infectious Disease Control, National Institute for Public Health and the Environment, Bilthoven.
• A. Ott, Certe, Department of Medical Microbiology Groningen & Drenthe, Groningen.
• K. Waar, Certe, Department of Medical Microbiology Friesland & Noordoostpolder, Leeuwarden.
• W. Ang, Comicro, Department of Medical Microbiology, Hoorn.
• J. da Silva, Deventer Hospital, Department of Medical Microbiology, Deventer.
• A.L.M. Vlek, Diakonessenhuis Utrecht, Department of Medical Microbiology and Immunology, Utrecht.
• A.G.M. Buiting, Elisabeth-TweeSteden (ETZ) Hospital, Department of Medical Microbiology and Immunology, Tilburg.
• L.G.M. Bode, Erasmus University Medical Center, Department of Medical Microbiology and Infectious Diseases, Rotterdam.
• Jansz, Eurofins PAMM, Department of Medical Microbiology, Veldhoven.
• S. Paltansing, Franciscus Gasthuis & Vlietland, Department of Medical Microbiology and Infection Control, Rotterdam.
• A.J. van Griethuysen, Gelderse Vallei Hospital, Department of Medical Microbiology, Ede.
• J.R. Lo Ten Foe, Gelre Hospital, Department of Medical Microbiology and Infection Control, Apeldoorn.
• M.J.C.A. van Trijp, Groene Hart Ziekenhuis, Department of Medical Microbiology and Infection Prevention, Gouda.
• M. Wong, Haga Hospital, Department of Medical Microbiology, ‘s-Gravenhage.
• A.E. Muller, HMC Westeinde Hospital, Department of Medical Microbiology, ‘s-Gravenhage.
• M.P.M. van der Linden, IJsselland hospital, Department of Medical Microbiology, Capelle a/d Ijssel.
• M. van Rijn, Ikazia Hospital, Department of Medical Microbiology, Rotterdam.
• S.B. Debast, Isala Hospital, Laboratory of Medical Microbiology and Infectious Diseases, Zwolle.
• E. Kolwijck, Jeroen Bosch Hospital, Department of Medical Microbiology and Infection Control, ‘s-Hertogenbosch.
• N. Al Naiemi, LabMicTA, Regional Laboratory of Microbiology Twente Achterhoek, Hengelo.
• T. Schulin, Laurentius Hospital, Department of Medical Microbiology, Roermond.
• S. Dinant, Maasstad Hospital, Department of Medical Microbiology, Rotterdam.
• S.P. van Mens, Maastricht University Medical Centre, Department of Medical Microbiology, Infectious Diseases & Infection Prevention, Maastricht.
• D.C. Melles, Meander Medical Center, Department of Medical Microbiology, Amersfoort.
• J.W.T. Cohen Stuart, Noordwest Ziekenhuisgroep, Department of Medical Microbiology, Alkmaar.
• P. Gruteke, OLVG Lab BV, Department of Medical Microbiology, Amsterdam.
• A. van Dam, Public Health Service, Public Health Laboratory, Amsterdam.
• Maat, Radboud University Medical Center, Department of Medical Microbiology, Nijmegen.
• Maraha, Regional Laboratory for Microbiology, Department of Medical Microbiology, Dordrecht.
• J.C. Sinnige, Regional Laboratory of Public Health, Department of Medical Microbiology, Haarlem.
• E. van der Vorm, Reinier de Graaf Groep, Department of Medical Microbiology, Delft.
• M.P.A. van Meer, Rijnstate Hospital, Laboratory for Medical Microbiology and Immunology, Velp.
• M. de Graaf , Saltro Diagnostic Centre, Department of Medical Microbiology, Utrecht.
• E. de Jong, Slingeland Hospital, Department of Medical Microbiology, Doetinchem.
• S.J. Vainio , St Antonius Hospital, Department of Medical Microbiology and Immunology, Nieuwegein.
• E. Heikens, St Jansdal Hospital, Department of Medical Microbiology, Harderwijk.
• M. den Reijer, Star-shl diagnostic centre, Department of Medical Microbiology , Rotterdam.
• J.W. Dorigo-Zetsma, TergooiMC, Central Bacteriology and Serology Laboratory, Hilversum.
• A. Troelstra, University Medical Center Utrecht, Department of Medical Microbiology, Utrecht.
• E. Bathoorn, University of Groningen, Department of Medical Microbiology, Groningen.
• J. de Vries, VieCuri Medical Center, Department of Medical Microbiology, Venlo.
• D.W. van Dam, Zuyderland Medical Centre, Department of Medical Microbiology and Infection Control, Sittard-Geleen.
• E.I.G.B. de Brauwer, Zuyderland Medical Centre, Department of Medical Microbiology and Infection Control, Heerlen.
• R. Steingrover, St. Maarten Laboratory Services, Department of Medical Microbiology, Cay Hill (St. Maarten).
Funding
The patient isolates were collected and sequenced as part of the Dutch National CPE surveillance and represent regular activities of the RIVM, financed by the Dutch Ministry of Health, Welfare and Sport. The environmental isolates were sequenced as part of the Regional typing initiative in the province of Limburg, the Netherlands, financed by the Infection Prevention and Antimicrobial Resistance Healthcare Network Limburg (IP & AMR Zorgnetwerk Limburg, previously LINK).
Author information
Authors and Affiliations
Contributions
Conceptualization: CAJR, ERH. Acquisition clinical data: RPJH, AHJWJ, CCK, ERH. Acquisition microbiological data: CAJR, APAH, LBA. Methodology: CAJR, APAH, LBA. Formal analysis: CAJR. Writing – original draft manuscript: CAJR. Writing – review and editing: All authors. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
In line with local hospital regulations regarding descriptive case studies, written patient consent to participate in this study was acquired for the patient referred to in the case description. For the patient isolates received in the Dutch CPPA surveillance program (Type-Ned), patient identifiers provided by medical microbiological laboratories were encrypted and then stored in the Type-Ned database, ensuring patient privacy in accordance with General Data Protection Regulation. Ethical approval was not required, since it is based on genomic and phenotypic surveillance data only. Samples from which the isolates were cultured, were all taken as part of routine healthcare.
Consent for publication
Written informed consent for publication was acquired from the patient for the publication of the identity revealing information.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Rossel, C.A.J., Hendrickx, A.P.A., van Alphen, L.B. et al. Tracing the origin of NDM-1-producing and extensively drug-resistant Pseudomonas aeruginosa ST357 in the Netherlands. BMC Infect Dis 24, 817 (2024). https://doi.org/10.1186/s12879-024-09722-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09722-1