Abstract
Background and aims
Numerous HBeAg-positive chronic hepatitis B (CHB) patients with persistently normal ALT have significant liver histopathology. It is imperative to identify true “immune tolerant” patients. We aimed to evaluate the liver histopathology features of HBeAg-positive CHB patients with normal ALT and the incidence of liver cirrhosis and HCC in CHB patients during follow-up.
Methods
179 HBeAg-positive CHB patients with normal ALT who performed liver biopsy from 2009 to 2018 were retrospectively analyzed. Liver necroinflammation ≥ G2 and/or liver fibrosis ≥ S2 was defined as significant liver histopathological change.
Results
57.5% patients were in the indeterminate phase with significant liver histological changes. The proportion of the patients with evident liver necroinflammation was higher in the high-normal ALT group (21-40U/L) when compared with the low-normal ALT group (≤ 20 U/L) (51.3% vs. 30.0%, p < 0.05), and patients aged ≥ 40 years had a higher proportion of significant fibrosis than those aged < 40 years (64.5% vs. 39.9%, p < 0.05). The percentages of patients with ≥ S2 and ≥ G2/S2 in the HBV DNA < 107 IU/mL group were higher than those in the HBV DNA ≥ 107 IU/mL group (72.7% vs. 40.1%, p < 0.01; 81.8% vs. 54.1%, p < 0.05). During follow-up, two of immune tolerant patients and four of indeterminate patients developed into cirrhosis, and one of immune tolerant patients and one of indeterminate patients developed into HCC, respectively.
Conclusions
HBeAg-positive CHB patients with high-normal ALT or HBV DNA < 107 IU/mL were tend to be indeterminate. Liver biopsy or noninvasive approaches are recommended to evaluate liver histopathology, and antiviral therapy is recommended for patients with significant liver histopathology.
Similar content being viewed by others
Introduction
According to the study on the global prevalence for chronic hepatitis B virus (HBV) infection, approximately 292 million people worldwide are affected, with nearly 59.4 million patients being immune-tolerant. Morever, about 86 million people are affected in China, including 15.84 million patients in the immune tolerant phase [1]. Chronic HBV infection is still a major public health concern.
Chronic HBV infection is usually classified as immune tolerant, immune clearance, inactive carrier, and reactive phase [2]. HBeAg-positive CHB patients with high levels of HBV DNA and persistent normal ALT are usually clinically diagnosed as “immune tolerant” patients, and the risk of disease progression is minimal. The main international guidelines have diverse definitions of the immune tolerant phase. According to the American Association for the Study of the Liver Disease (AASLD) guidelines, the upper limit of normal ALT (ULN) is 35 U/L for men and 25 U/L for women, [3] while the European Association for the Study of the Liver (EASL) and the Asian Pacific Association for the Study of the Liver (APASL) guidelines suggest 40 U/L for both men and women [4, 5]. Additionally, some guidelines propose adopting a more stringent ALT cutoff value: 30 U/L for men and 19 U/L for women [6,7,8]. Besides persistently normal ALT, the cutoff value of HBV DNA defined by various international guidelines differs in this phase; APASL defines HBV DNA > 2 × 105 IU/mL (ALT is 1 ~ 2×ULN)5, EASL defined it as HBV DNA > 107 IU/mL4, and AASLD set it as HBV DNA > 106 IU/mL3. This shows that there is no consensus on clinical criteria for defining the immune-tolerant phase. However, this concept has been challenged in recent years. Some recent studies have found that a sizable number of HBeAg-positive CHB patients with persistently normal ALT have significant liver injury [9], suggesting a high risk of liver cirrhosis and HCC, and some studies have demonstrated that HBV-specific T cells, HBV DNA integration and clonal hepatocyte proliferation were the immune tolerance patients’ specific charateristics [10,11,12]. Therefore, identifying genuine “immune tolerant” patients among HBeAg-positive CHB patients with normal ALT is indispensable, further studies are needed to investigate the definition of true immune tolerant phase.
Thus, we retrospectively analyzed 179 HBeAg-positive CHB patients with normal ALT, aiming to study rates and determinants of clinically significant liver injuries.
Methods
Study population
The study enrolled 179 chronic hepatitis B patients who performed liver biopsy in Guangdong Provincial Hosipital of Chinese Medicine from April 2009 to December 2018. The procedure of this study conformed to the ethical standards of the committee responsible for human trials and the ethical standards of the latest edition of the Declaration of Helsinki, which was approved by the Ethics Committee of Guangdong Provincial Hospital of Chinese Medicine (No. BF2018-175-01).
Also, the patient’s informed consents were obtained. The research proposal was registered on http://www.chictr.org.cn ChiCTR1900025897,9/13/2019). Eligible participants were in chronic HBV infection, HBsAg positive for more than 6 months with at least 6 months of normal ALT (≤ ULN, 40 U/L), and had liver biopsy results. Study exclusion criteria were as follows: (1) evidence of co-infection of HIV (human immunodeficiency virus), HCV(hepatitis C virus) or HDV (hepatitis D virus); (2)EBV, CMV, Wilson’s disease or schistosomiasis liver disease; (3) underwent antiviral treatment; (4) significant alcohol consumption (≥ 40 g/d for males and ≥ 20 g/d for females); (5)and cirrhosis and HCC etc.
Liver biopsy
Liver biopsy and pathological diagnosis were also conducted in Guangdong Provincial Hospital of Chinese Medicine. The patient voluntarily signed the informed consent form and adhered to the protocol requirements. The liver tissue was obtained by percutaneous puncture with a 16G puncture needle, and promptly fixed with 10% formalin, paraffin embedded, serial sectioned, and hematoxylin-eosin (HE) staining and Mason staining followed by pathological analysis. The pathological diagnosis of liver tissue was carried out by experienced pathologists, who were blinded to the clinical and biochemical data of the individual patient.
Definition
Liver necroinflammation histological grading and liver fibrosis staging were guided by Chinese guidelines for the prevention and treatment of CHB (2022 version). Necroinflammation was divided into G0 ~ G4, while liver fibrosis was S0 ~ S4. Necroinflammatory grade ≥ 2 (≥ G2) and/or fibrosis stage ≥ 2 (≥ S2) were recognized as significant liver histopathological change. Indeterminate patients in this study were defined as ALT normal but significant liver histological changes.
The definitions of the Chinese staging of liver histological inflammation and fibrosis in comparisons with Metavir or Ishak have been presented in Chinese guidelines for the prevention and treatment of CHB (2022 version). For example, the Chinese liver fibrosis staging of S0, S1, S2, S3, and S4 approximately corresponds to the Metavir fibrosis staging of F0 (0 score), F1(1 score), F2 (2 score), F3 (3 score), and F4 (4 score).
Data collection of laboratory tests
Patients’ clinical data have been extracted from the electronic medical record, including ALT, aspartate aminotransferase (AST) and HBV DNA levels (the ULN of ALT and AST for both males and females was 40 U/L). HBV immune markers, such as HBsAg, anti-HBs, HBeAg, anti-HBe and anti-HBc were also collected.
Statistical analysis
All statistical analyses were carried out using SPSS ver.26.0. The Mann–Whitney U test was used to analyze the quantitative variables which were non-normally distributed and represented as medians and ranges, while the analysis of categorical variables expressed as frequencies and percentages was performed by chi-square test. Correlations between liver histological changes and clinical factors were tested by using Spearman rank correlation. Multivariate logistic regression was adopted to explore the independent risk factors related to significant liver histological changes. A two-sided p value of < 0.05 indicates a statistically significant difference.
Results
Patients characteristics
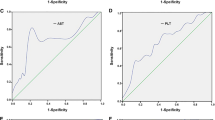
The patients’ baseline characteristics are described in Table 1. Of the 179 HBeAg-positive patients, the case of patients with low-normal ALT (ALT ≤ 20 U/L) was 60, and that with high-normal ALT (ALT > 20 U/L) was 119. The age of the two groups showed no significant difference. The proportion of males in the group with high normal ALT was significantly higher than that in the group with low normal ALT, and the ALT, AST, and GGT levels were also higher. In addition, the group with high normal ALT had a higher proportion of patients with ≥ G2 (51.3% vs. 30.0%, p < 0.05). As shown in Fig. 1 and 103 (57.5%) of patients had significant liver histological changes.
Subgroup comparison of different age
As shown in Supplementary Fig. 1, the proportion of patients with ≥ S2 in the groups of age ≥ 40 years was higher than that in the group of age < 40 years (64.5% vs. 39.9%, p < 0.05). Further stratified by ALT levels, in the group of patients age < 40 years, the proportion of ≥ G2 and ≥ S2 in the group with high normal ALT was higher than that in the group with low normal ALT (48.4% vs. 32.1%, 45.3% vs. 30.2%, p values were 0.054, 0.073, respectively), but there was no statistical difference. When the patients’ age was ≥ 40 years, it was observed that the proportion of patients with ≥ G2 in the group with high normal ALT was significantly higher than that in the group with low normal ALT (62.5% vs. 14.3%, p < 0.05) (Fig. 2). According to different ages and HBV DNA levels, the patients were further analyzed. In the age < 40 years group, patients with HBV DNA ≥ 107 IU/mL had a lower proportion of ≥ S2 and ≥ G2/S2 than those with HBV DNA < 107 IU/mL (36.1% vs. 73.3%, 51.1% vs. 86.7%, p < 0.01) (Fig. 2 and Supplementary Table 2).
Subgroup comparison of different HBV DNA levels
As shown in Supplementary Fig. 2, patients with HBV DNA < 107 IU/mL had a higher proportion of ≥ S2 and ≥ G2/S2 than that in the group with HBV DNA ≥ 107 IU/mL(72.7% vs. 40.1%, p < 0.01; 81.8% vs. 54.1%, p < 0.05). In addition, 42.7% and 40.1% of patients with HBV DNA ≥ 107 IU/mL had ≥ G2 and ≥ S2, respectively. When comparing different ALT levels, as shown in Fig. 3 and Supplementary Table 2, regardless of HBV DNA < 107 IU/mL or ≥ 107 IU/mL, the high-normal ALT group had a higher proportion of ≥ G2 than the low-normal ALT group, and a significant difference was found in patients with HBV DNA ≥ 107 IU/mL (49.0% vs. 30.2%, p = 0.024).
Predictor forsignificant liver histology
As depicted in Supplementary Table 3, Spearman correlation confirmed a positive correlation between age and liver fibrosis (r = 0.262, p < 0.01), and HBV DNA levels in HBeAg-positive CHB patients correlated with liver necroinflammation and fibrosis negatively (r=-0.181, p < 0.05; r=-0.217, p < 0.01). As shown in Table 2, multivariate logistic regressions were performed to analyze and predict independent risk factors for significant liver histology, showing that ALT > 20 U/L was an independent risk factor for predicting significant liver necroinflammation (OR = 2.855, 95% CI 1.421–5.734, p = 0.003), while HBV DNA < 107 IU/mL was an independent risk factor for predicting significant liver fibrosis (OR = 4.173, 95% CI 1.483–11.741, p = 0.007).
Incidence of liver cirrhosis and HCC in CHB patients during follow-up
Liver cirrhosis and HCC events occurred during the follow-up period, as shown in Table 3. Follow-up data were available in 36 immune tolerant patients (mean 5.9 years) and 55 indeterminate patients (mean 4.5 years). In this study, during 212 person-years of follow-up, 2 immune tolerant patients developed cirrhosis, with an annual incidence of 0.94%.One immune tolerant patients developed HCC, with an annual incidence of 0.47%. Besides, during 248 person-years of follow-up, 4 indeterminate patients developed cirrhosis, with an annual incidence of 1.6%, and 1 indeterminate patient developed HCC, with an annual incidence of 0.4%, respectively. Meanwhile, all of the immune tolerant patients experienced a phase change during follow up; none of them remained in the immune tolerant phase, 21 indeterminate patients changed to other phase.
Discussion
It is generally considered that liver biopsy of immune tolerance patients shows no liver fibrosis and mild liver necroinflammation [13], a study showed that the progression of liver injury in immune tolerance patients with a course of more than 5 years was very slow, with only 3 cases (6.3%, 3/48) progressing to fibrosis [14]. Therefore, the main international guidelines recommend that true immune tolerance patients should be closely observed rather than be given antiviral therapy. However, a number of recent studies have found that approximately 1/3 − 1/2 of HBeAg-positive patients with normal ALT have obvious liver histological changes [9, 15,16,17], indicating that these patients have a high risk of progressing to cirrhosis and HCC. Similarly, in our study, 42.7% and 40.1% of HBeAg-positive patients with normal ALT and HBV DNA ≥ 107 IU/mL had ≥ G2 and ≥ S2, respectively. Our study confirmed that among a noticeable number of HBeAg-positive patients with normal ALT and high HBV DNA levels, significant liver histological changes still exist, suggesting that these patients have disease progression and should be given antiviral therapy. Therefore, it is necessary to look for true immune tolerance patients and to reconsider the patients who meet the antiviral indications and the timing of antiviral treatment among HBeAg-positive CHB patients with normal ALT.
Our study reveals that in HBeAg-positive patients, the proportion of ≥ G2 in the group with high normal ALT was higher than that in the low- normal ALT group (51.3% vs. 30.0%, p < 0.01), which was also found in patients aged > 40-year-old and the HBV DNA ≥ 107 IU/mL group. Several studies have presented similar results [18]. Lai et al. cconducted liver biopsy on CHB patients with persistently normal ALT (56% HBeAg positive) and discovered that 46% of patients with high-normal ALT had significant liver necroinflammation or liver fibrosis, which was quite higher than the 20% in the low-normal ALT group [19]. Wong et al. employed transient elastography to examine 254 “immune tolerant” patients, and the proportions of patients over 35 years old with ≥ F2 in the high and low normal ALT groups were 37% and 2%, respectively [20]. These studies demonstrated that patients with high normal ALT had a higher proportion of liver histopathological changes, suggesting that patients with high-normal ALT have an increased risk of disease progression. ALT > 20 U/L was found as a risk factor for predicting significant liver necroinflammation independently through logistic regression analysis. Therefore, we recommend performing liver biopsy and/or implementing noninvasive approaches for patients with high normal ALT to determine whether antiviral therapy is necessary. On the other hand, previous study have shown that male patients were associated with adverse progression of CHB, but our study demonstrated that it did not emerge as significant factor in the multivariate analyses. To identify the reason of inconsistency, we compared the proportion of male and female patients who had significant liver histopathology with ALT > 20 IU/L (supplementary Table 5), and it showed that a higher proportion of female patients have significant liver histology than male patients (72.3% vs. 55.6%, p = 0.065), although these results were not statistically significant. The explanation of this result was that ALT > 20 IU/L may be a normal level for male but abnormal for female. Consequently, the relationship between gender and liver histopathology needs to be further investigation, and gender factors should also be taken into account when evaluating the ULN level of ALT.
Patient age is also a key factor in deciding the initiation of antiviral therapy. Currently, the age cutoff value for immune tolerance has not been clearly delineated. The AASLD guidelines point out that patients aged > 40 years are more prone to have significant liver histological disease, and antiviral therapy is recommended for immune tolerance patients aged > 40 years [3]. The EASL guidelines recommend that patients with an ALT of 41–80 U/L should be evaluated for liver histology via transient elastography and/or liver biopsy and antiviral therapy should be contemplated for patients over 30 years old, even if liver fibrosis is not assessed [4]. A study involving 253 CHB patients demonstrated that when ALT was normal (ULN:30 U/L for males; 19 U/L for females), the proportions of ≥ F2 in patients aged over 40 and under 40 years were 42% and 30%, respectively [21]. In our study, it was noted that the ≥ 40-year-old group exhibited a higher proportion of ≥ S2 than the < 40-year-old group (64.5% vs. 39.9%, p < 0.05). Furthermore, this study revealed that 39.9% of patients with normal ALT and an age < 40 years have significant liver fibrosis, which indicates that more rigorous monitoring of liver fibrosis is also necessary for patients aged < 40 years, and more data are needed in the future to investigate the relationship between age and the immune tolerance phase.
The interaction between HBV DNA and liver histological changeshas still not been completely clarified. Previous studies have found that HBV DNA levels of HBeAg-negative patient are positively correlated with liver injuries [22, 23], while Bai et al. found that in HBeAg-positive patients, there was no significant relation between them [24]. In this study, among HBeAg-positive patients with normal ALT, HBV DNA levels are negatively correlated with liver fibrosis (r=-0.217, p = 0.004), (Supplementary Figs. 3 and 4), which is in conformity with the results of a previous study of HBeAg-positive patients(r=-0.491, p < 0.001) [25]. We also found that the proportion of ≥ G2/S2 in the HBV DNA < 107 IU/mL group was higher than that in the group with HBV DNA ≥ 107 IU/mL (81.8% vs. 54.1%, p < 0.05). Similar results were observed in patients aged < 40 years or ≥ 30 years (Supplementary Table 4). However, when the age was ≥ 40 years, there was no difference in the proportion of significant liver histopathology between them, which further indicates that when the age is higher than 40 years, most patients are no longer in the true immune tolerance phase, and antiviral therapy is needed. In addition, research on the relationship between HBV DNA levels and HCC had shown that patients with persistently high HBV DNA levels (> 107 IU/mL) had a significantly lower risk of HCC than patients with HBV DNA levels between 106~107 IU/mL [26]. Moreover, Lee et al. discovered that the cutoff of HBV DNA > 107 IU/mL can be used to determine the immune tolerance phase [27]. In our study, it can be seen that HBV DNA < 107 IU/mL is a risk factor for independently predicting liver fibrosis ≥ S2, which indicats that patients with HBV DNA > 107 IU/mL are more likely to be truly immune tolerant. In the future, more research is demanded to figure out the cutoff value of HBV DNA during immune tolerance. Thus, it is important to monitor “immune tolerant” patients with older age, higher normal ALT and lower HBV DNA levels closely who might have a high risk of advanced disease.
Recently, a fiery discussion is focused on whether to expand antiviral treatment indicators in CHB patients, especially in immune-tolerant patients [28, 29]. In our study, a higher proportion of indeterminate patients were reported, therefore, it is necessary to further explore how to determine the true immune tolerant patients. In fact, there have been studies consistent with our research. A Korean study conducted by Yoo et al. reported that nearly 70% of patients were not in the true immune-tolerant phase [30]. Another Chinese research also showed that over 30% of immune tolerant CHB patients had significant liver fibrosis [31]. Both of them have demonstrated that lower HBV DNA levels was associated with significant liver injuries. In a European setting, Göbel T et al. demonstrated that patients with CHB infection and normal ALT levels had significant liver fibrosis(36%) or necroinflammation(27%) [21]. At the same time, the indeterminate patients have a phase change tendency and may develop into liver cirrhosis and HCC during follow up. Chinese guidelines (2022 versions) suggest deciding whether antiviral therapy needs to be initiated based on a comprehensively disease progression by assessing serum HBV DNA, ALT level, and liver disease severity, combined with factors such as age, family history, and concomitant diseases [32]. It is expected that more research will be carried out on the effectiveness of antiviral therapy for patients in the immune tolerance phase, so as to better manage the patients in this phase individually.
Our study focused on the hot issues regarding the management of ALT-normal CHB patients; however, there were several limitations. First, the sample size was not large enough. The patients in this study were collected from one provincial hospital. Second, we lack the data on obesity and diabetes, which are potential cofounders of liver histopathology. Third, it was also limited by the inadequate data of follow-up and we didn’t have data on HBV genotypes of the study population, which might better illustrate the dynamic changes of the long-term prognosis. Therefore, we could enroll more cases from different region in the future to better explore the prognosis of ALT-normal CHB patients.
In summary, our research showed that (57.5%) significant liver histological changes were revealed in HBeAg-positive CHB patients with normal ALT, and 81.8% of patients with HBV DNA < 107 IU/mL had significant liver histopathology. Based on our finding, liver biopsy or noninvasive approaches are strongly recommended for patients with high-normal ALT or with HBV DNA < 107 IU/mL to evaluate the degree of liver histological changes and to recommend antiviral therapy for patients with significant liver histopathology. Future studies should be carried out to explore the need for antiviral therapy and to individualize the management of those indeterminate patients.
Data availability
The data that support the findings of this study are available on request from the corresponding author.
References
Global prevalence. Treatment, and prevention of hepatitis B virus infection in 2016: a modelling study. Lancet Gastroenterol Hepatol. 2018;3(6):383–403.
Liaw YF. Natural history of chronic hepatitis B virus infection and long-term outcome under treatment. Liver Int. 2009;29(Suppl 1):100–7.
Terrault NA, Lok ASF, McMahon BJ, Chang KM, Hwang JP, Jonas MM, et al. Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance. Hepatology. 2018;67(4):1560–99.
EASL. 2017 Clinical Practice Guidelines on the management of hepatitis B virus infection. J Hepatol 2017; 67(2): 370 – 98.
Sarin SK, Kumar M, Lau GK, Abbas Z, Chan HL, Chen CJ, et al. Asian-pacific clinical practice guidelines on the management of hepatitis B: a 2015 update. Hepatol Int. 2016;10(1):1–98.
Kao JH, Hu TH, Jia J, Kurosaki M, Lim YS, Lin HC, et al. East Asia expert opinion on treatment initiation for chronic hepatitis B. Aliment Pharmacol Ther. 2020;52(10):1540–50.
Sarri G, Westby M, Bermingham S, Hill-Cawthorne G, Thomas H, et al. Diagnosis and management of chronic hepatitis B in children, young people, and adults: summary of NICE guidance. BMJ. 2013;26(346):f3893.
Keeffe EB, Dieterich DT, Han SH, et al. A treatment algorithm for the management of chronic hepatitis B virus infection in the United States: 2008 update. Clin Gastroenterol Hepatol. 2008;6(12):1315–41.
Kumar M, Sarin SK, Hissar S, Jacobson IM, Martin P, Schiff ER, et al. Virologic and histologic features of chronic hepatitis B virus-infected asymptomatic patients with persistently normal ALT. Gastroenterology. 2008;134(5):1376–84.
Mason WS, Gill US, Litwin S, Zhou Y, Peri S, Pop O et al. HBV DNA integration and clonal hepatocyte expansion in Chronic Hepatitis B patients considered Immune Tolerant. Gastroenterology 2016; 151(5): 986 – 98. e4.
Bertoletti A, Ferrari C. Adaptive immunity in HBV infection. J Hepatol. 2016;64(1 Suppl):S71–83.
Kennedy PTF, Sandalova E, Jo J, Gill U, Ushiro-Lumb I, Tan AT, et al. Preserved T-cell function in children and young adults with immune-tolerant chronic hepatitis B. Gastroenterology. 2012;143(3):637–45.
Andreani T, Serfaty L, Mohand D, Dernaika S, Wendum D, Chazouillères O, et al. Chronic hepatitis B virus carriers in the immunotolerant phase of infection: histologic findings and outcome. Clin Gastroenterol Hepatol. 2007;5(5):636–41.
Hui CK, Leung N, Yuen ST, Zhang HY, Leung KW, Lu L, et al. Natural history and disease progression in Chinese chronic hepatitis B patients in immune-tolerant phase. Hepatology. 2007;46(2):395–401.
Nguyen MH, Garcia RT, Trinh HN, Lam KD, Weiss G, Nguyen HA, et al. Histological disease in asian-americans with chronic hepatitis B, high hepatitis B virus DNA, and normal alanine aminotransferase levels. Am J Gastroenterol. 2009;104(9):2206–13.
Park JY, Park YN, Kim DY, Paik YH, Lee KS, Moon BS, et al. High prevalence of significant histology in asymptomatic chronic hepatitis B patients with genotype C and high serum HBV DNA levels. J Viral Hepat. 2008;15(8):615–21.
Liao B, Wang Z, Lin S, Xu Y, Yi J, Xu M, et al. Significant fibrosis is not rare in Chinese chronic hepatitis B patients with persistent normal ALT. PLoS ONE. 2013;8(10):e78672.
Gui HL, Wang H, Yang YH, Wu YW, Zhou HJ, Guo SM, et al. Significant histopathology in Chinese chronic hepatitis B patients with persistently high-normal alanine aminotransferase. J Viral Hepat. 2010;17(Suppl 1):44–50.
Lai M, Hyatt BJ, Nasser I, Curry M, Afdhal NH. The clinical significance of persistently normal ALT in chronic hepatitis B infection. J Hepatol. 2007;47(6):760–7.
Wong GL, Wong VW, Choi PC, Chan AW, Chim AM, Yiu KK, et al. Clinical factors associated with liver stiffness in hepatitis B e antigen-positive chronic hepatitis B patients. Clin Gastroenterol Hepatol. 2009;7(2):227–33.
Göbel T, Erhardt A, Herwig M, Poremba C, Baldus SE, Sagir A, et al. High prevalence of significant liver fibrosis and cirrhosis in chronic hepatitis B patients with normal ALT in central Europe. J Med Virol. 2011;83(6):968–73.
Wang Y, Xu MY, Zheng RD, Xian JC, Xu HT, Shi JP, et al. Prediction of significant fibrosis and cirrhosis in hepatitis B e-antigen negative patients with chronic hepatitis B using routine parameters. Hepatol Res. 2013;43(5):441–51.
Duan M, Chi X, Xiao H, Liu X, Zhuang H, et al. High-normal alanine aminotransferase is an indicator for liver histopathology in HBeAg-negative chronic hepatitis B. Hepatol Int. 2021;15(2):318–27.
Bai H, Liu H, Chen X, Xu C, Dou X. Influence of age and HBeAg status on the correlation between HBV DNA and hepatic inflammation and fibrosis in chronic hepatitis B patients. Dig Dis Sci. 2013;58(5):1355–62.
Xie Q, Hu X, Zhang Y, Jiang X, Li X, Li J. Decreasing hepatitis B viral load is associated with a risk of significant liver fibrosis in hepatitis B e antigen positive chronic hepatitis B. J Med Virol. 2014;86(11):1828–37.
Chen CF, Lee WC, Yang HI, Chang HC, Jen CL, Iloeje UH, et al. Changes in serum levels of HBV DNA and alanine aminotransferase determine risk for hepatocellular carcinoma. Gastroenterology. 2011;141(4):1240–8.
Lee HA, Lee HW, Kim IH, Park SY, Sinn DH, Yu JH, et al. Extremely low risk of hepatocellular carcinoma development in patients with chronic hepatitis B in immune-tolerant phase. Alimenta Pharmacol Ther. 2020;52(1):196–204.
Kim HL, Kim GA, Park JA, Kang HR, Lee EK, Lim YS. Cost-effectiveness of antiviral treatment in adult patients with immune-tolerant phase chronic hepatitis B. Gut. 2021;70(11):2172–82.
Jeng WJ, Lok AS. Should treatment indications for chronic Hepatitis B be expanded? [J]. Clin Gastroenterol Hepatol. 2021;19(10):2006–14.
Yoo JJ, Park SY, Moon JE, Lee YR, Lee HA, Lee J, et al. Long-term prognosis and the need for histologic assessment of chronic hepatitis B in the serological immune-tolerant phase. Clin Mol Hepatol. 2023;29(2):482–95.
Wang J, Yan X, Zhu L, Liu J, Qiu Y, Li Y, et al. Significant histological disease of patients with chronic hepatitis B virus infection in the grey zone. Aliment Pharmacol Ther. 2023;57(5):464–74.
Chinese Society of Hepatology, Chinese Medical Association; Chinese Society of Infectious Diseases, Chinese Medical Association. [Guidelines for the prevention and treatment of chronic hepatitis B (version 2022)]. Zhonghua Gan Zang Bing Za Zhi. 2022;30(12):1309–31.
Acknowledgements
We would like to acknowledge all members performing biochemical test and biopsy.
Funding
This study was supported by the Major Science and Technology Special Project of ChinaThirteenth Five-Year Plan, No. 2018ZX10732401-003-015 and No.2018ZX10725506-003.
Author information
Authors and Affiliations
Contributions
Study concept and design (XEL, XLC), acquisition of data (HMX, MJS, YBX, PTZ, SL), analysis and interpretation of data (MHD, HMX), drafting of the manuscript (MHD, HMX), critical revision of the manuscript for important intellectual content (XEL, HZ).
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This stuyd was approved by the Ethics Committee of Guangdong Provincial Hospital of Chinese Medicine (No. BF2018-175-01). Written informed consents were obtained from all patients through following up in outpatient department or by telephone and letter follow-up before this study.
Consent for publication
We have the consent to publish this study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Duan, M., Xiao, H., Shi, M. et al. Significant liver histological change is common in HBeAg-positive chronic hepatitis B with normal ALT. BMC Infect Dis 24, 723 (2024). https://doi.org/10.1186/s12879-024-09617-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09617-1