Abstract
Background
Dengue infection is a mosquito-borne, endemic viral disease, particularly in developing countries. Here, we report the results of the clinicodemographic, serologic profile and the monthly occurrence of a recent dengue fever outbreak in Puntland State (Somalia).
Methodology
We analyzed the data of 956 dengue-suspected patients who were investigated using the rapid diagnostic testing (RDT) method for detecting NS1 (dengue virus non-structural protein) and IgM antibodies employing the SD Biosensor Dengue Dou NS Ag and IgM test kit (Germany) at the Puntland Public Health Referral Laboratory from November 21, 2022, to May 27, 2023.
Results
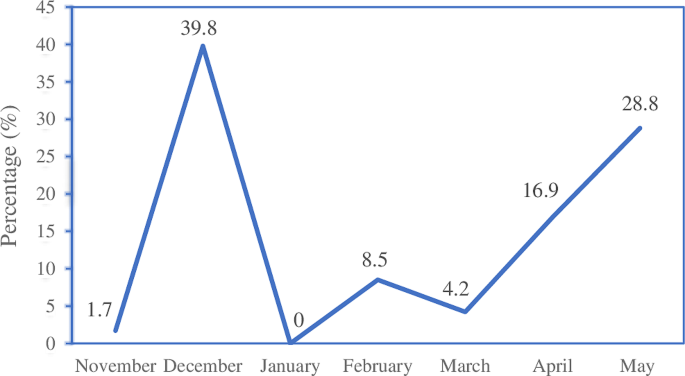
We found that 118 cases were positive for dengue among the suspected patients enrolled in the present study. Of these cases, 76.2% were dengue NSI positive, 13.6% were dengue IgM positive, and 10.2% were both NSI and IgM positive. The number of females and males in the confirmed cases was equal, and most (48.3%) were aged 20 years or less. 43.1% of them lived in the Nugal region, particularly in Garowe. Clinically, fever was the most frequent symptom (88.9%). The cases peaked in December 2022 but dropped from January to March, with a slight rise in February, and then increased in April and May 2023.
Conclusion
This study highlights the clinicodemographic characteristics, seroprevalence, and monthly occurrence of dengue in Puntland. We recommend improving vector control measures, enhancing case management, strengthening dengue surveillance, developing an early warning system, and conducting future studies to characterize the circulating strains.
Background
Dengue, one of the relevant public health issues, especially in tropical and subtropical countries, is a systemic febrile illness caused by the dengue virus (DENV), a single-stranded RNA virus that belongs to the genus Flavivirus and consists of four serotypes (DEN 1–4), transmitted to humans by the bite of the Aedes aegypti mosquito [1, 2]. The spread of the mosquito has been significantly aided by major demographic shifts, including population expansion, unplanned urbanization leading to poor housing, and the need for water storage [3].
Clinically, the illness can be asymptomatic or have manifestations such as fever, headache, retro-orbital pain, muscle and joint pain, rash, lymphadenopathy, hepatomegaly, nausea, and vomiting. In addition, some patients experience severe abdominal pain, persistent vomiting, tachypnea, hemorrhagic presentations, and neurological and mildly altered mental status features, which are considered to be warning signs [4,5,6].
Currently, serological tests used for diagnosing dengue infection rely on detecting either dengue non-structural protein 1 (NS1) antigen or dengue immunoglobulin M (IgM) through the enzyme-linked immunosorbent assay (ELISA) method [7]. Unfortunately, these tests might not be available in resource-limited settings. Therefore, less-sensitive, rapid diagnostic tests (RDTs) detecting dengue NS1 antigen or IgM are frequently used in these areas. Combining the two RDT tests raises their sensitivity for detecting dengue to 88.7% [8].
About 2.5 billion (> 40% of the world’s population) are at risk of dengue. According to World Health Organization (WHO) estimates, there may be 50–100 million dengue infections annually worldwide [9]. Epidemics of dengue have been reported in several African nations [10]. In Somalia, an outbreak of the dengue disease has been documented as early as 1985 in Hargeisa [11]. Also, infections of DENV-1, DENV-2, and DENV-3 and co-infections of DENV-1/2 and DENV-2/3 serotypes were identified in the Mogadishu outbreak in 2011 [12]. Recently, dengue was reported in the country in October 2022 [13]. In Puntland State (Somalia), the first case of dengue fever from the Sol region (Las Anod district) was confirmed on 21 November 2022. To our knowledge, no onset of dengue has been previously reported in the Puntland State. The present study, therefore, aims to describe the clinicodemographic, serologic profile, and monthly occurrence of a recent dengue fever outbreak in Puntland State (Somalia).
Methods
Study design
A descriptive observational, retrospective study was conducted using secondary data from the Puntland Public Health Referral Laboratory in the period from November 21, 2022, to May 27, 2023.
Study area
This study was carried out in the Puntland State of Somalia, which is located in the northeastern part of the country and bordered by the Indian Ocean to its east and the Gulf of Aden to the north. The Puntland State consists of nine regions, namely, Bari, Karkar, Sanag, Nugal, Mudug, Sool, Ayn, Haylan, and Gardafue.
Study population and sample size
All dengue-suspected cases tested and registered in the computerized record of the Puntland Public Health referral laboratory during the study period were included in the study. Patients with incomplete data on demographic, clinical, and serological profiles were excluded. A total of 956 dengue-suspected patients were included in this study.
Diagnostic tool
All patients were tested for dengue rapid diagnostics of both NS1 and IgM using the SD Biosensor Dengue Dou NS Ag and IgM test kit (Germany) at the Puntland Public Health Lab. The SD Biosensor DENV NS1 has a sensitivity and specificity of 90.0%/90.2%, whereas the anti-DENV IgM has a sensitivity and specificity of 71.8%/83.5%.
Data collection tool
Data were obtained from the laboratory in an Excel sheet. The data regarding demographic characteristics (sex, age, region, and district), clinical symptoms, testing dates, and results of dengue IgM and NS1 RDTs were collected.
Statistical analysis
The data, obtained in a Microsoft Excel sheet, was checked for repetition. The data were complete regarding demographic characteristics, testing dates, and serologic results. Data were then imported into Statistical Package for the Social Sciences (SPSS) 20, and descriptive analysis was carried out by frequencies, and percentages and presented in tables and figures.
Results
Demographic characteristics of the dengue cases
Of the 956 dengue-suspected patients examined, we found that 118 were dengue-positive. The number of dengue-positive females and males was equal. Most of the dengue cases (48.3%) were aged 20 years or younger, and the age group (21–40 years) represented 42.4%, while the remaining 9.3% were 41 years of age or older (Table 1).
Regarding the geographic distribution of the dengue-positive cases, inhabitants of the Nugal region represented 43.1%, of which 38.1% were living in the Garowe district and 5% were in the Burtinle district. Residents of Mudug region (Galkayo district), Sool region (Las Anod district), and Karkar region (Gardo district) infected with dengue were 16.1%, 15.3%, and 13.6%, respectively, whereas 9.3% of the cases were from Bari region (Bossaso district). Finally, 2.5% of the cases were residents of the Sanag region (Dhahar district), as shown in Table 1.
Clinical profile of dengue cases
Furthermore, the clinical symptoms observed in the dengue-infected patients and their frequencies after we excluded 10 cases with missing clinical symptoms are summarized in Table 2.
Severity of the dengue patients
In this study, only 7 patients aged 18 years or less were hospitalized; of them, 4 were females and 3 were males (Table 3).
Serology profile of the dengue-positive cases
Finally, as reported in Table 4, out of the 956 dengue-suspected patients examined in the present study, 118 cases were confirmed dengue-positive. The current study showed that 90 (76.2%) of the dengue cases were dengue NSI positive, 16 (13.6%) of them were dengue IgM positive, and the remaining 12 (10.2%) were both dengue IgM and NSI positive (Table 4).
Monthly distribution of dengue cases
The frequency of occurrence of the dengue cases varied during the study period. The monthly distribution of the dengue cases in Puntland is reported in Fig. 1.
Discussion
Currently, dengue infection is endemic in many parts of the world [14]. Patients with this infection may present with various clinical features that resemble other acute febrile illnesses, making its diagnosis difficult [15]. Therefore, efficient clinical and laboratory evaluations are cornerstones of care for dengue-suspected patients.
Of the 956 dengue-suspected patients examined in this study, we found 118 dengue positive cases. The number of males and females infected was equal, contrasting the results of earlier reports, where female preponderance was observed [16,17,18,19]. This observation also contrasts with other studies that found a higher rate of dengue infection among males [20,21,22]. Further, we found that most (48.3%) of the infected cases were 20 years of age or less. This result is comparable to that (52%) reported in Darfur, Sudan [23]. The higher vulnerability of this age group to the disease might be due to their exposure to mosquito bites in schools, during outdoor activities, and indoor biting since many of them stay home longer. Also, the clinical features are known to be more apparent in children [24]. In the present study, we investigated the distribution of the disease in all regions of Puntland State (Somalia) (see Table 1). Most of the dengue-positive cases were in the Nugal region, particularly in Garowe, the capital city of Puntland. This city has experienced rapid population growth, fast urbanization, an increase in internally displaced persons (IDPs) camps, and the influx of large returnees and migrants [25]. The higher prevalence of dengue in Garowe could be related to these demographic factors and climate changes.
Clinically, dengue patients frequently present with a triad of fever, pain, and rash. Nevertheless, gastrointestinal and bleeding symptoms might occur in variable proportions [26]. Our study showed that fever was the most common clinical symptom (88.9%), which is consistent with earlier studies [27, 28]. The second most frequent symptom (35.2%) was myalgia (Table 1). A higher frequency of myalgia among dengue patients was described before [5, 29, 30]. This was followed by skin rash and gastrointestinal symptoms, consistent with a study conducted in Saudi Arabia [31].
In our study, most of the dengue-positive cases were mild and treated as outpatients. Only seven pediatric cases required hospital admission. The increased risk of severe forms of dengue resulting in hospitalization and mortality among children in tropical areas has been documented [32]. Moreover, in pediatric patients, dengue frequently causes profound vascular leakage and abrupt shock [33].
In this study, the overall seroprevalence of dengue was found to be 118 (12.3%), which is lower than the results of other studies carried out in Kenya (61.2%) and Sudan (42%) [34, 35]. The study also showed that 13.6% of dengue cases were dengue IgM antibody positive, which is in line with the 14.7% reported from Eastern Italy [36]. This result was lower than the 21% reported in northwest Ethiopia [37]. Furthermore, the present study revealed a higher positive rate (76.2%) of dengue NS1 among the study participants (Table 3). It is known that NS1 antibody is useful in the early stages of the disease, especially in the days 3–5 after the onset of the illness, when viremia levels might be undetectable and anti-IgM antibody levels have yet to rise [38]. Thus, the higher positive rates of NS1 in this study could be attributed to patients presenting in the acute phase of the illness. The discrepancies in the seroprevalence of dengue might be explained by the differences in environmental conditions, the sample sizes, and the diagnostic methods employed.
Rainfall and temperature play an important role in mosquito proliferation and the incidence of dengue illness [39]. The temperature in Puntland varies from 27 °C to 37 °C, and the spring season (April–June) is regarded as the principal rainy season, while the autumn season (October–December) is a short rainy season [40]. The seasonal distribution of dengue throughout the study period is reported in Fig. 1. Dengue cases peaked in December 2022, fell from January to March with a slight rise in February, and then increased in April and May 2023. The monthly variation in dengue cases could be due to weather changes and rainfall. A previous study revealed the impact of climate variability on the occurrence of dengue [29].
Although this study presents evidence of the dengue fever outbreak in Puntland State, Somalia, some limitations should be considered. Firstly, the study used secondary data subjected to incomplete or missing information. As discussed earlier, there were cases with missing clinical features. Secondly, we were unable to characterize the virus since we used serologic tests for the diagnosis. Thirdly, we were unable to identify the source of dengue infection or provide detailed information related to the disease transmission. Lastly, data on dengue case outcomes was not recorded, so assessing the patients’ outcomes was impossible.
Conclusion
In conclusion, we found that of the 956 dengue-suspected patients investigated, 118 cases were dengue-positive. Patients aged 20 years or younger were the most infected. Fever was the most frequent clinical symptom in the patients. Cases were highest in December 2022, followed by May 2023. We recommend improving vector control measures, enhancing case management, strengthening dengue surveillance, developing an early warning system, and conducting future studies to characterize the circulating strains.
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Abbreviations
- RDTs:
-
Rapid diagnostic tests
- DENV:
-
Dengue virus
- RNA:
-
Ribonucleic acid
- NS1:
-
Non-structural protein 1 antigen
- IgM:
-
Immunoglobulin M
- ELISA:
-
Enzyme-linked immunosorbent assay
- WHO:
-
World Health Organization
- IDPs:
-
Internally displaced persons
References
Unnikrishnan R, Faizal BP, Vijayakumar P, et al. A retrospective study on the socio-demographic factors and clinical parameters of dengue disease and their effects on the clinical course and recovery of the patients in a tertiary care hospital of Bangladesh. Ngondi JM, editor. J Fam Med Prim Care. 2015;4:369–72. https://doi.org/10.1371/journal.pntd.0010297.
Unnikrishnan R, Faizal BP, Vijayakumar P, et al. Clinical and laboratory profile of dengue in the elderly. J Fam Med Prim Care. 2015;4:369–72.
Maheshwari V, Gupta D, Parmar D. Clinico–epidemiological profile of confirmed cases of dengue infection: a tertiary care teaching hospital based study of central India. Indian J Pathol Oncol. 2020;5:531–5.
Castilho BM, Silva MT, Freitas ARR, et al. Factors associated with thrombocytopenia in patients with dengue fever: a retrospective cohort study. BMJ Open. 2020;10:e035120. https://doi.org/10.1136/bmjopen-2019-035120. https://bmjopen.bmj.com/lookup/doi/.
Mohan K, Malaiyan J, Nasimuddin S, et al. Clinical profile and atypical manifestation of dengue fever cases between 2011 and 2018 in Chennai, India. J Fam Med Prim Care. 202AD;9:1119–23.
Alvarado-Castro VM, Ramírez-Hernández E, Paredes-Solís S, et al. Clinical profile of dengue and predictive severity variables among children at a secondary care hospital of Chilpancingo, Guerrero, Mexico: case series. Boletín Médico Del Hosp Infant México (English Ed. 2016;73:237–42.
Chaloemwong J, Tantiworawit A, Rattanathammethee T, et al. Useful clinical features and hematological parameters for the diagnosis of dengue infection in patients with acute febrile illness: a retrospective study. BMC Hematol. 2018;18:1–10.
Luvira V, Thawornkuno C, Lawpoolsri S, et al. Diagnostic performance of Dengue NS1 and antibodies by serum concentration technique. Trop Med Infect Dis. 2023;8:1–12.
Mehta SR, Bafna TA, Aarati B. Pokale. Demographic and clinical spectrum of dengue patients admitted in a tertiary care hospital. Med J Dr DY Patil Vidyapeeth. 2018;11:128–31.
Were F. The dengue situation in Africa. Paediatr Int Child Health. 2012;32:18–21.
Botros BA, Watts DM, Soliman AK, et al. Serological evidence of dengue fever among refugees, Hargeysa, Somalia. J Med Virol. 1989;29:79–81.
Bosa HK, Montgomery JM, Kimuli I, et al. Dengue fever outbreak in Mogadishu, Somalia 2011: co-circulation of three dengue virus serotypes. Int J Infect Dis. 2014;21:3. https://doi.org/10.1016/j.ijid.2014.03.412.
Somalia World Health Emergency Programme Update – Somalia. 2023;(Jan):1–5. https://reliefweb.int/attachments/bc3d1897-6915-4165-88c8-ca4549e5b584/Health-Emergency-Programme-January-2023.pdf.
World Health Organization (WHO). Dengue and severe dengue. 2023; https://www.who.int/news-room/fact-sheets/detail/dengue-and-severe-dengue.
Prashanth E, Adnan I. Clinical profile of dengue infection at a center in north Karnataka, India. Glob J Infect Dis Clin Res. 2019;5:006–9.
Hussien HH. Epidemiological Descriptive Analysis of Disease Outbreaks in 2019 in Sudan. Open J Epidemiol. 2020;10:419–31.
Bello OA, Aminu M, Jatau ED. Seroprevalence of IgM Antibodies to Dengue Fever Virus among patients presenting with symptoms of Fever in some hospitals in Kaduna State, Nigeria. Int J Sci Res. 2016;5(3):1255–9.
Aniakwaa-Bonsu E, Amoako-Sakyi D, Dankwa K, et al. Seroprevalence of Dengue viral infection among adults attending the University of Cape Coast Hospital. Adv Infect Dis. 2021;11:60–72.
Fujimoto DE, Koifman S. Clinical and laboratory characteristics of patients with dengue hemorrhagic fever manifestations and their transfusion profile. Rev Bras Hematol Hemoter. 2014;36:115–20.
Woyessa AB, Mengesha M, Kassa W, et al. The first acute febrile illness investigation associated with dengue fever in Ethiopia, 2013: a descriptive analysis. Ethiop J Heal Dev. 2014;28:155–61.
Kumar A, Sarwari S, Ahmed Arain W, et al. A retrospective study on Laboratory Profile and Clinical parameters of Dengue Fever patients. Pakistan J Med Heal Sci. 2021;15:3357–9.
Riccò M, Peruzzi S, Balzarini F et al. Dengue fever in Italy: the eternal return of an emerging Arboviral Disease. Trop Med Infect Dis. 2022;7.
Ahmed A, Ali Y, Elmagboul B, et al. Dengue fever in the Darfur area, Western Sudan. Emerg Infect Dis. 2019;25:2125–6.
Alera MT, Srikiatkhachorn A, Velasco JM, et al. Incidence of Dengue Virus infection in adults and children in a prospective longitudinal cohort in the Philippines. PLoS Negl Trop Dis. 2016;10:1–14.
UN-HABITAT. Puntland’s Ministry of Public Transport and Work. Garowe Urban Profile. www.unhabitat.org/somalia.
Hasan MJ, Tabassum T, Sharif M, et al. Comparison of clinical manifestation of dengue fever in Bangladesh: an observation over a decade. BMC Infect Dis. 2021;21:1–10. https://doi.org/10.1186/s12879-021-06788-z.
Obonyo M, Fidhow A, Ofula V. Investigation of laboratory confirmed dengue outbreak in north-eastern Kenya, 2011. PLoS ONE. 2018;13:1–11.
Islam QT, Sagor HB, Tuli TC. Et. Changing clinical pattern of Dengue Fever and its unusual Manifestations- 9 2019 outbreak in Dhaka, Bangladesh. J Bangladesh Coll Physicians Surg. 2020;39:9–18.
Al Awaidy ST, Khamis F, Al-Zakwani I et al. Epidemiological and clinical characteristics of patients with Dengue Fever in a recent outbreak in Oman: a single center retrospective-cohort study. Oman Med J. 2022;37.
Aziz BAA, Hassanien SEA, Abdou AM. Clinical and Hematological Effects of Dengue Viruses Infection. Am J Infect Dis Microbiol Vol 4, 2016, Pages 74–78. 2016;4:74–8. http://pubs.sciepub.com/ajidm/4/4/2/index.html, http://pubs.sciepub.com/ajidm/4/4/2/abstract.html.
Shahin W, Nassar A, Kalkattawi M, et al. Dengue fever in a tertiary hospital in Makkah, Saudi Arabia. Dengue Bull. 2009;33:34–44.
Tsheten T, Clements ACA, Gray DJ, Adhikary RK, Furuya-Kanamori L, Wangdi K. Clinical predictors of severe dengue: a systematic review and meta-analysis. Infect Dis Poverty. 2021;10(1):1–10. https://doi.org/10.1186/s40249-021-00908-2.
Idrus NL, Jamalid SM, Bakar AA, Embong H, Ahmad NS. Comparison of clinical and laboratory characteristics between severe and non-severe dengue in paediatrics. PLoS Negl Trop Dis. 2023;2023–December:1–10. https://doi.org/10.1371/journal.pntd.0011839.
Lim JK, Matendechero SH, Alexander N, Lee JS, Lee KS, Namkung S, et al. Clinical and epidemiologic characteristics associated with dengue fever in Mombasa, Kenya. Int J Infect Dis. 2020;100:207–15. https://doi.org/10.1016/j.ijid.2020.08.074.
Elaagip A, Alsedig K, Altahir O, et al. Seroprevalence and associated risk factors of dengue fever in Kassala state, eastern Sudan. PLoS Negl Trop Dis. 2020;14:e0008918. https://doi.org/10.1371/journal.pntd.0008918.
Loconsole D, Metallo A, De Robertis AL, et al. Seroprevalence of Dengue Virus, West Nile Virus, Chikungunya Virus, and Zika Virus in International Travelers attending a travel and Migration Center in 2015–2017, Southern Italy. Vector-Borne Zoonotic Dis. 2018;18:331–4.
Ferede G, Tiruneh M, Abate E, et al. A serologic study of dengue in northwest Ethiopia: suggesting preventive and control measures. PLoS Negl Trop Dis. 2018;12:1–17.
Moi ML, Omatsu T, Tajima S, et al. Detection of dengue virus nonstructural protein 1 (NS1) by using ELISA as a useful laboratory diagnostic method for dengue virus infection of international travelers. J Travel Med. 2013;20:185–93.
Morales I, Salje H, Saha S, et al. Seasonal distribution and climatic correlates of dengue disease in Dhaka, Bangladesh. Am J Trop Med Hyg. 2016;94:1359–61.
Puntland W. 2023. http://de.wikipedia.org/wiki/Puntland.
Acknowledgements
The authors would like to thank the Ministry of Health, (Puntland), and the Puntland Public Health Lab.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
SSJ designed the study, performed data analysis and interpretation, and drafted the manuscript. SNA and JSJ contributed to the collection, analysis, and interpretation of the data and the writing of the manuscript. MMA was involved in laboratory tests, the collection, analysis, and interpretation of data, and writing the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Ethical declaration
This study was approved by the ethical review committee (ERC) for the Ministry of Health of Puntland State (Somalia), and the need for consent to participate was waived by the ERC under approval number MOH-PL/ERC/2206. Permission was obtained from the General Directorate office of the Ministry. The study was performed according to the relevant guidelines and regulations.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jama, S.S., Abshir, S.N., Jama, J.S. et al. Retrospective study on the dengue fever outbreak in Puntland State, Somalia. BMC Infect Dis 24, 735 (2024). https://doi.org/10.1186/s12879-024-09552-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09552-1