Abstract
Background
Both disseminated intravascular coagulation and thrombotic microangiopathy are complications of sepsis as Salmonella septicemia, respectively. They are related and have similar clinical characteristics as thrombopenia and organ dysfunctions. They rarely co-occur in some specific cases, which requires a clear distinction.
Case presentation
A 22-year-old woman had just undergone intracranial surgery and suffered from Salmonella derby septicemia with multiorgan involvement in the hospital. Laboratory workup demonstrated coagulation disorder, hemolytic anemia, thrombocytopenia, and acute kidney injury, leading to the co-occurrence of disseminated intravascular coagulation and secondary thrombotic microangiopathy. She received antibiotics, plasma exchange therapy, dialysis, mechanical ventilation, fluids, and vasopressors and gained full recovery without complications.
Conclusion
Disseminated intravascular coagulation and secondary thrombotic microangiopathy can co-occur in Salmonella derby septicemia. They should be treated cautiously in diagnosis and differential diagnosis. Thrombotic microangiopathy should not be missed just because of the diagnosis of disseminated intravascular coagulation. Proper and timely identification of thrombotic microangiopathy with a diagnostic algorithm is essential for appropriate treatment and better outcomes.
Similar content being viewed by others
Background
Both thrombotic microangiopathy (TMA) and disseminated intravascular coagulation (DIC) are acute life-threatening conditions. They share similar clinical presentations as a bleeding tendency, thrombocytopenia, and organ failure, which makes it challenging to distinguish one from the other [1].
DIC is typically featured by the simultaneous occurrence of widespread vascular clot deposition, compromising blood supply to various organs and contributing to organ failure [2,3,4,5,6]. The characteristic of DIC is systemic activation of the coagulation system, followed by consumption of platelets and clotting factors and secondary fibrinolysis arising from both inflammatory and non-inflammatory causes [7]. The generation of fibrin-related markers (FRMs) in DIC reflects microvascular changes [1]. Though there is no gold standard and no specific biomarker for diagnosing DIC, a reliable diagnosis of DIC can be made through simple scoring algorithms based on readily available routine hemostatic parameters [6]. About 35% of cases of severe sepsis with Gram-negative and Gram-positive microorganisms may be complicated by DIC [6, 8,9,10].
TMA is not as common as DIC. According to the experts’ experience, physicians encounter an average of three cases of TMA per year in the intensive care unit (ICU) [11]. TMA is a pathological term describing small vessel (arterioles and capillaries) injury and microvascular thrombosis. It is defined by microangiopathic hemolytic anemia (MAHA), thrombocytopenia, and organ failure of the kidney, central nervous system, and other organs [1, 12, 13]. It includes Shiga toxin-associated hemolytic uremic syndrome (STEC-HUS), atypical hemolytic uremic syndrome (aHUS), and thrombotic thrombocytopenic purpura (TTP), as well as secondary TMA with a coexisting diseases/condition (e.g., infection, malignancy, autoimmune disease, pregnancy, transplantation, or drug) [11, 14, 15]. Core processes of TMA is the remarkable activation, aggregation, and consumption of platelet originating from widespread inflammation and vascular endothelial cell injuries [11, 14, 15].
Prompt identification and accurate etiological diagnosis are crucial for early therapeutic approaches to minimize organ damage and improve patient survival. For differential diagnosis, the elevation of FRMs is required in DIC [15], deficiency of A disintegrin-like and metalloprotease with thrombospondin type 1 motifs 13(ADAMTS13) activity (< 10%) is required in TTP, Shiga toxin is required in STEC-HUS, abnormalities of the complement system are necessary for aHUS [10, 13, 14]. Several diagnostic algorithms that aid rapid differential diagnosis have been published [16,17,18,19]. Only a few have been tailored to intensivists [11, 20], and none have mentioned the co-occurrence of DIC and TMA.
The co-occurrence of DIC and TMA in the sepsis population is extremely rare and should raise our attention. Herein we first report a Salmonella derby septicemia complicated with DIC and secondary TMA in a 22-year-old woman. Comprehensive management with antibiotics, plasma exchange, and supportive therapies resulted in good outcomes without chronic sequelae.
Case presentation
A 22-year-old female patient underwent craniopharyngioma surgery in our hospital. She developed panhypopituitarism postoperatively, supplemented with desmopressin, hydrocortisone, and L-thyroxine. She was otherwise healthy, and her familial medical histories were negative for renal and thrombotic diseases.
On the 20th postoperative day, she developed a fever(38.2℃), vomiting, and non-bloody diarrhea with exposure to undercook seafood in the neurosurgical ward. She was transferred to ICU for respiratory distress the next day.
On the 21st postoperative day, her condition deteriorated. She presented tachycardia (145/min), hypotension (80/65 mmHg), tachypnea (40/min) on a high-flow nasal cannula, and anuric acute kidney injury (AKI). Physical examination revealed non-palpable skin petechiae, subcutaneous hematoma in the right inguinal area, and diffuse bilateral lung crackles.
Laboratory test results in ICU were as follows (Table 1). Her hematology revealed anemia (68 g/L) and thrombocytopenia (6 × 109/L). Coagulation suggested prolonged activated partial thromboplastin time (50.2 s, reference 28.0–43.0 s) and prothrombin time (21.0 s, reference 11.0–15.0 s), elevated fibrinogen and fibrin degradation products (FDPs) (70.84 mg/L, reference 0–5.00 mg/L). Urinalysis showed proteinuria. Urinary sediment contained 3–5 white blood cells and > 60 red blood cells per high-power field. Procalcitonin was 96.33 ng/mL. The renal function test showed increased urea nitrogen (10.9 mmol/L) and serum creatinine (161 umol/L). Chest computed tomography revealed bilateral pulmonary filtrations and pleural effusions. Cardiac echography revealed moderate tricuspid regurgitation with estimated pulmonary systolic pressure of 43 mmHg.
Her blood pressure coagulation disorder returned to normal on the 23rd postoperative day. She was still anuric. She was anemic despite transfusions of 10.5 U packed red blood cells in 3 days. Her hemoglobin was 60 g/L. Her platelet count was 21 × 109/L. Lactate dehydrogenase (LDH) was 2794 IU/L. The reticulocyte count was 2.42%; The percentage of schistocytes was 5%. All the above revealed Coombs’ negative microangiopathic hemolytic anemia with thrombocytopenia, indicating TMA.
The results of the etiological workup were as follows (Table 2; Additional file 1: Table S1). Complement factors (C3, C4, CH50), immunoglobulins, autoimmune, anti-phospholipid, and vasculitis antibodies all tested normal, except for a mild decrease of immunoglobulin G (6.68 g/L, reference 8.60–17.40 g/L). Further hematological tests returned negative, including CD59 of red blood cells and white blood cells, anti-platelet antibodies, and levels of ferritin, folic acid, and vitamin B12. Salmonella derby was isolated from blood cultures, while Escherichia coli and Enterococcus faecalis were isolated from urine cultures. Neither O-157 Escherichia coli nor Salmonella was isolated from stool and urine cultures. Mildly reduced ADAMTS13 activity was reported (46%; reference 70–120%). Complement Factor H was 517.4 ug/ml (reference 247.0–1010.8 ug/ml). Factor H autoantibody and inhibitor of ADAMTS13 were both negative.
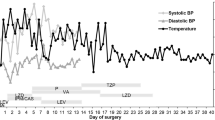
Her overt DIC score was 6, and her sepsis-induced coagulopathy score was 6. A diagnosis of septic shock due to Salmonella derby, with complications of DIC and TMA, was established. The Antibiotic was adjusted from ceftriaxone to meropenem on the arrival day to ICU. She received fluid resuscitation, vasopressor, mechanical ventilation, dialysis, and hydrocortisone for septic shock (200–300 mg/d increase from 100 mg/d). She received transfusions of 10.5U packed red blood cells, 800 ml fresh frozen plasma, and four packs of platelets from the 21st to the 23rd postoperative day. On the 24th postoperative day, plasma exchange therapy (fresh frozen plasma 2–2.4 L/d) started immediately. She underwent seven consecutive plasma exchange therapies in total (Fig. 1).
She made a rather good recovery, fortunately. She was extubated on the 31st postoperative day. As she regained her platelet count of 63 × 109/L on the 32nd postoperative day, plasma exchange therapy ceased. Continuous veno-venous hemodialysis stopped the next day as she was able to urinate 868 ml/day. Her plasma ADAMTS13 activity raised to 86% (Table 2). During the whole course of the illness, her neurological status stayed alert. She was discharged from ICU on the 38th postoperative day with renal dysfunction (urea nitrogen, 24.07 mmol/L; creatinine, 344 umol/L).
She was discharged from the hospital with normal renal function (urea nitrogen, 7.17 mmol/L; creatinine, 73 umol/L) on the 68th postoperative day.
Discussion and conclusions
Salmonella derby was one serovar out of over 2500 recognized serovars of Salmonella causing invasive non-typhoidal salmonella infections(iNTS), presenting as septicemia with and without a secondary extra-intestinal focus of infection. iNTS has a lower prevalence yet a greater severity and case fatality than Salmonella enteritidis or typhoid fever [21]. Salmonella derby was one of the top five causes of iNTS in China [22, 23]. At the same time, it rated behind 30 in the United States [24]. Corticosteroid use increases the risk of non-typhoidal salmonella septicemia [25, 26].
Our case highlights one significant finding: an uncommon secondary TMA in the context of Salmonella septicemia-induced DIC. It is the first report of the co-occurrence of DIC and TMA in Salmonella septicemia.
Most cases of Salmonella septicemia have been diagnosed with DIC based on the overt DIC criteria [27]. Our patient fulfilled both overt DIC (score 6) and sepsis-induced coagulopathy criteria (score 6) for diagnosis of DIC [27, 28]. She manifested with cutaneous and mucosal bleeding and subcutaneous hematoma, abnormal coagulation, thrombocytopenia, elevated FRMs, and multiorgan dysfunction. However, later during her resolution of sepsis, the elevation of indirect bilirubin, and persistent severe anemia, which was not consistent with the severity of bleeding, indicated hemolytic anemia. The increased LDH and reticulocyte percentage, with peripheral schistocytes, demonstrated MAHA. Measurement of haptoglobin is not available in our hospital. MAHA also presents in DIC, but TMA is a more appropriate diagnosis when atypical MAHA appears. ADAMTS13 activity (before initiation of plasma exchange therapy), microbiological testing, and complement factor testing helped us rule out TTP, STEC-HUS, and aHUS. Our patient was diagnosed with an infection-associated TMA. Thereby co-occurrence of DIC and TMA complicated septicemia had been finally established. Salmonella septicemia triggered overt DIC and TMA simultaneously and incidentally from clues in the timeline of coagulation and hemolysis.
DIC and TMA occasionally co-occurred in previous literature [1, 29]. Most cases were patients with sepsis as Entero-hemorrhagic Escherichia coli, Proteus mirabilis, Group A Streptococcus, and Capnocytophaga canimorsus [1, 30,31,32,33,34,35,36,37]. Other cases were patients with bone marrow metastasis from gastric cancer and liver failure [1, 38]. From the Oklahoma Thrombotic Thrombocytopenic Purpura-Hemolytic Uremic Syndrome registry, 32.3% (10/31) of patients with TTP manifested coagulation disorders, indicating DIC development [39]. Up to 14% of patients in one STEC-HUS cohort experienced DIC during the disease [40]. Multicentric studies are needed to determine the actual risk of co-occurrence of DIC and TMA.
It remains unclear whether these were the co-morbid state of DIC and TMA or TMA progression mediated by coagulopathy due to DIC [15] or, in fact, misdiagnosed cases. These findings propose that TMA should not be overlooked in patients with DIC. Signs of MAHA and thrombocytopenia would be a critical clue for TMA diagnosis. In suspicious TMA cases in the context of DIC, further investigations of Shiga-toxins, complements, ADAMTS13 activity, and inhibitors are recommended [11]. Renal biopsy, if feasible, also played a vital part in TMA diagnosis. Detection of microvascular thrombosis, especially platelet thrombosis on biopsy, usually indicates TMA. Fibrinolysis may dissolve micro-thrombosis in patients with DIC [1]. As classic pathological entities in TMA and DIC have been identified, renal biopsy contributes to better differentiation [15]. Nevertheless, our patient had rejected renal biopsy.
Regarding treatment, the keystone in managing DIC and TMA is the adequate treatment of the etiology. In the present case, it would be the antibiotics targeting Salmonella septicemia.
In DIC, platelet transfusion is advised in patients with bleeding tendencies due to thrombocytopenia [41, 42]. Anti-coagulation or anti-fibrinolytic therapy is indicated according to DIC’s hypercoagulative or hyperfibrinolytic state [41, 42]. Antithrombin concentrate and recombinant thrombomodulin for DIC are frequently used in Japan [43, 44].On the contrary, platelet transfusion is contraindicated in TMA [1]. In our case, recognition of TMA prevented the patient from deterioration as we stopped further transfusion of platelet, which might be the reason for persistent MAHA and thrombocytopenia.
Different therapeutic intervention according to specific etiology is advised. Plasma exchange therapy is recommended in TTP, eculizumab is useful for aHUS, and rituximab is effective for acquired TTP [45,46,47]. Plasma exchange therapy is necessary to start empirically in adult patients with TMA of unclear etiology to avoid delaying TTP treatment [11, 13, 48, 49]. Plasma exchange therapy in TMA is considered helpful in replenishing ADAMTS13, eliminating antibodies to ADAMTS13, replacing normal-sized von Willebrand factor (vWF), and eliminating ultra vWF multimers and excess cytokines. Plasma exchange therapy also had a role in sepsis or septic shock with DIC, TMA, and multiple organ dysfunction [50,51,52,53]. Plasma exchange therapy also benefited septic patients with decreased ADAMTS13 activity [54]. The possible underlying mechanism of plasma exchange therapy was via repairing endothelial function in sepsis and DIC. Evidence for therapeutic interventions beneficial in sepsis complicated with DIC and TMA is lacking. Therapeutic interventions were adopted empirically and varied from case to case in previous reports. A specific treatment according to the etiology of TMA could be a reasonable strategy for a better outcome.
However, the relationship between ADAMTS13 activity and severity, organ failure and outcome in sepsis, and sepsis-associated DIC remained controversial [37, 55,56,57,58]. One hypothesis is that severe endothelial injury in sepsis-associated TMA leads to the release of a massive number of vWF multimers and the consumption of ADAMTS13, contributing to a mild decrease in ADAMTS13 activity [59]. Another hypothesis is that damage to endothelium and activation of the complement system in systemic inflammation in sepsis and DIC followed by the formation of neutrophil extracellular traps, which affects the change of ADAMTS13 structure and reduces the activity of ADAMTS13 [59,60,61]. Both endothelial injuries and neutrophil extracellular traps might contribute to the pathogenesis of the co-occurrence of TMA and DIC.
In conclusion, constant vigilance is necessary to avoid missing TMA in patients with sepsis-associated DIC. DIC itself should not be an exclusion for TMA diagnosis. An atypical clinical course for sepsis-associated DIC with atypical MAHA and thrombocytopenia often implies the clue for TMA. A throughout workup, including microbiological testing, ADAMTS13 activity, and complement factor testing, is necessary for the diagnosis of TMA etiologies. Proper and timely recognition of TMA is vital for appropriate decisions regarding the use of plasma exchange therapy and restriction of platelet transfusion in patients with co-occurrence of DIC and TMA.
Data availability
All data included in this case are included in this published article. All data are available from the corresponding author upon reasonable request.
Abbreviations
- DIC:
-
Disseminated intravascular coagulation
- TMA:
-
Thrombotic microangiopathy
- FRMs:
-
Fibrin-related markers
- ICU:
-
Intensive care unit
- MAHA:
-
Microangiopathic hemolytic anemia
- STEC-HUS:
-
Shiga toxin-associated hemolytic uremic syndrome
- aHUS:
-
Atypical hemolytic uremic syndrome
- TTP:
-
Thrombotic thrombocytopenic purpura
- ADAMTS13:
-
A disintegrin-like and metalloprotease with thrombospondin type 1 motifs 13
- AKI:
-
Acute kidney injury
- FDPs:
-
Fibrinogen and fibrin degradation products
- LDH:
-
Lactate dehydrogenase
- iNTS:
-
Invasive non-typhoidal salmonella infections
- vWF:
-
von Willebrand factor
References
Wada H, Matsumoto T, Suzuki K, Imai H, Katayama N, Iba T, et al. Differences and similarities between disseminated intravascular coagulation and thrombotic microangiopathy. Thromb J. 2018;16:14.
Gando S, Levi M, Toh CH. Disseminated intravascular coagulation. Nat Rev Dis Primers. 2016;2:16037.
Levi M. Disseminated intravascular coagulation. Crit Care Med. 2007;35(9):2191–5.
Schmaier AH. Disseminated intravascular coagulation. N Engl J Med. 1999;341(25):1937–8.
Boral BM, Williams DJ, Boral LI. Disseminated intravascular coagulation. Am J Clin Pathol. 2016;146(6):670–80.
Levi M, Scully M. How I treat disseminated intravascular coagulation. Blood. 2018;131(8):845–54.
Popescu NI, Lupu C, Lupu F. Disseminated intravascular coagulation and its immune mechanisms. Blood. 2022;139(13):1973–86.
Levi M, van der Poll T. Coagulation and sepsis. Thromb Res. 2017;149:38–44.
Kinasewitz GT, Yan SB, Basson B, Comp P, Russell JA, Cariou A, et al. Universal changes in biomarkers of coagulation and inflammation occur in patients with severe sepsis, regardless of causative micro-organism [ISRCTN74215569]. Crit Care. 2004;8(2):R82–90.
Angus DC, van der Poll T. Severe sepsis and septic shock. N Engl J Med. 2013;369(9):840–51.
Azoulay E, Knoebl P, Garnacho-Montero J, Rusinova K, Galstian G, Eggimann P, et al. Expert statements on the Standard of Care in critically ill adult patients with atypical hemolytic uremic syndrome. Chest. 2017;152(2):424–34.
Wada H, Matsumoto T, Yamashita Y. Natural history of thrombotic thrombocytopenic purpura and hemolytic uremic syndrome. Semin Thromb Hemost. 2014;40(8):866–73.
Matsumoto M, Fujimura Y, Wada H, Kokame K, Miyakawa Y, Ueda Y, et al. Diagnostic and treatment guidelines for thrombotic thrombocytopenic purpura (TTP) 2017 in Japan. Int J Hematol. 2017;106(1):3–15.
Jokiranta TS. HUS and atypical HUS. Blood. 2017;129(21):2847–56.
Scully M, Cataland S, Coppo P, de la Rubia J, Friedman KD, Kremer Hovinga J, et al. Consensus on the standardization of terminology in thrombotic thrombocytopenic purpura and related thrombotic microangiopathies. J Thromb Haemost. 2017;15(2):312–22.
Campistol JM, Arias M, Ariceta G, Blasco M, Espinosa L, Espinosa M, et al. An update for atypical haemolytic uraemic syndrome: diagnosis and treatment. A consensus document. Nefrologia. 2015;35(5):421–47.
Coppo P, Schwarzinger M, Buffet M, Wynckel A, Clabault K, Presne C, et al. Predictive features of severe acquired ADAMTS13 deficiency in idiopathic thrombotic microangiopathies: the french TMA reference center experience. PLoS ONE. 2010;5(4):e10208.
Laurence J, Haller H, Mannucci PM, Nangaku M, Praga M, Rodriguez de Cordoba S. Atypical hemolytic uremic syndrome (aHUS): essential aspects of an accurate diagnosis. Clin Adv Hematol Oncol. 2016;14(Suppl 11(11):2–15.
Bendapudi PK, Hurwitz S, Fry A, Marques MB, Waldo SW, Li A, et al. Derivation and external validation of the PLASMIC score for rapid assessment of adults with thrombotic microangiopathies: a cohort study. Lancet Haematol. 2017;4(4):e157-e64.
Vincent JL, Castro P, Hunt BJ, Jorres A, Praga M, Rojas-Suarez J, et al. Thrombocytopenia in the ICU: disseminated intravascular coagulation and thrombotic microangiopathies-what intensivists need to know. Crit Care. 2018;22(1):158.
Marchello CS, Birkhold M, Crump JA. Vacc-i NTScc. Complications and mortality of non-typhoidal salmonella invasive disease: a global systematic review and meta-analysis. Lancet Infect Dis. 2022;22(5):692–705.
Liu J, Bai L, Li W, Han H, Fu P, Ma X, et al. Trends of foodborne diseases in China: lessons from laboratory-based surveillance since 2011. Front Med. 2018;12(1):48–57.
Zhan Z, Xu X, Gu Z, Meng J, Wufuer X, Wang M, et al. Molecular epidemiology and antimicrobial resistance of invasive non-typhoidal Salmonella in China, 2007–2016. Infect Drug Resist. 2019;12:2885–97.
(CDC) CfDCaP. National Salmonella Surveillance Annual Report. 2016. Atlanta: US Department of Health and Human Services, CDC, 2018.
Katz D, Ben-Chetrit E, Sherer SS, Cohen D, Muhsen K. Correlates of non-typhoidal Salmonella bacteraemia: a case-control study. Int J Infect Dis. 2019;81:170–5.
Fierer J. Invasive non-typhoidal Salmonella (iNTS) infections. Clin Infect Dis. 2022;75(4):732–8.
Taylor FB Jr, Toh CH, Hoots WK, Wada H, Levi M, Scientific Subcommittee on Disseminated Intravascular Coagulation of the International Society on T, et al. Towards definition, clinical and laboratory criteria, and a scoring system for disseminated intravascular coagulation. Thromb Haemost. 2001;86(5):1327–30.
Iba T, Levy JH, Warkentin TE, Thachil J, van der Poll T, Levi M, et al. Diagnosis and management of sepsis-induced coagulopathy and disseminated intravascular coagulation. J Thromb Haemost. 2019;17(11):1989–94.
Schwameis M, Schorgenhofer C, Assinger A, Steiner MM, Jilma B. VWF excess and ADAMTS13 deficiency: a unifying pathomechanism linking inflammation to thrombosis in DIC, malaria, and TTP. Thromb Haemost. 2015;113(4):708–18.
Sakamaki Y, Konishi K, Hayashi K, Hashiguchi A, Hayashi M, Kubota E, et al. Renal thrombotic microangiopathy in a patient with septic disseminated intravascular coagulation. BMC Nephrol. 2013;14:260.
Tani N, Nakamura K, Sumida K, Suzuki M, Imaoka K, Shimono N. An Immunocompetent Case of Capnocytophaga canimorsus infection complicated by secondary thrombotic microangiopathy and disseminated intravascular coagulation. Intern Med. 2019;58(23):3479–82.
Wang Z, Yu Z, Su J, Cao L, Zhao X, Ruan C. Sepsis-induced disseminated intravascular coagulation with features of thrombotic thrombocytopenic purpura: a fatal fulminant syndrome. Clin Appl Thromb Hemost. 2011;17(3):251–3.
Abe T, Sasaki A, Ueda T, Miyakawa Y, Ochiai H. Complement-mediated thrombotic microangiopathy secondary to sepsis-induced disseminated intravascular coagulation successfully treated with eculizumab: a case report. Med (Baltim). 2017;96(6):e6056.
Badami KG, Srivastava RN, Kumar R, Saraya AK. Disseminated intravascular coagulation in post-dysenteric haemolytic uraemic syndrome. Acta Paediatr Scand. 1987;76(6):919–22.
Kawasaki Y, Suyama K, Ono A, Oikawa T, Ohara S, Suzuki Y, et al. Efficacy of recombinant human soluble thrombomodulin for childhood hemolytic uremic syndrome. Pediatr Int. 2013;55(5):e139-42.
Matano S, Inamura K, Konishi M, Okumura T, Kawai H, Okamura T, et al. Encephalopathy, disseminated intravascular coagulation, and hemolytic-uremic syndrome after infection with enterohemorrhagic Escherichia coli O111. J Infect Chemother. 2012;18(4):558–64.
Ono T, Mimuro J, Madoiwa S, Soejima K, Kashiwakura Y, Ishiwata A, et al. Severe secondary deficiency of von Willebrand factor-cleaving protease (ADAMTS13) in patients with sepsis-induced disseminated intravascular coagulation: its correlation with development of renal failure. Blood. 2006;107(2):528–34.
Seki Y, Wakaki K. Pathological findings in a case of bone marrow carcinosis due to gastric cancer complicated by disseminated intravascular coagulation and thrombotic microangiopathy. Int J Hematol. 2016;104(4):506–11.
Booth KK, Terrell DR, Vesely SK, George JN. Systemic infections mimicking thrombotic thrombocytopenic purpura. Am J Hematol. 2011;86(9):743–51.
Vashakidze E, Megrelishvili T, Pachkoria E, Tevzadze L, Lashkarashvili M. Enterohemorrhagic E. coli and hemolytic uremic syndrome in Georgia. Georgian Med News. 2010;186:38–41.
Wada H, Asakura H, Okamoto K, Iba T, Uchiyama T, Kawasugi K, et al. Expert consensus for the treatment of disseminated intravascular coagulation in Japan. Thromb Res. 2010;125(1):6–11.
Wada H, Thachil J, Di Nisio M, Mathew P, Kurosawa S, Gando S, et al. Guidance for diagnosis and treatment of DIC from harmonization of the recommendations from three guidelines. J Thromb Haemost. 2013. https://doi.org/10.1111/jth.12155.
Hayakawa M, Yamakawa K, Saito S, Uchino S, Kudo D, Iizuka Y, et al. Recombinant human soluble thrombomodulin and mortality in sepsis-induced disseminated intravascular coagulation. A multicentre retrospective study. Thromb Haemost. 2016;115(6):1157–66.
Iba T, Gando S, Saitoh D, Wada H, Di Nisio M, Thachil J. Antithrombin supplementation and risk of bleeding in patients with sepsis-associated disseminated intravascular coagulation. Thromb Res. 2016;145:46–50.
Rock GA, Shumak KH, Buskard NA, Blanchette VS, Kelton JG, Nair RC, et al. Comparison of plasma exchange with plasma infusion in the treatment of thrombotic thrombocytopenic purpura. Canadian apheresis Study Group. N Engl J Med. 1991;325(6):393–7.
Legendre CM, Licht C, Muus P, Greenbaum LA, Babu S, Bedrosian C, et al. Terminal complement inhibitor eculizumab in atypical hemolytic-uremic syndrome. N Engl J Med. 2013;368(23):2169–81.
George JN, Woodson RD, Kiss JE, Kojouri K, Vesely SK. Rituximab therapy for thrombotic thrombocytopenic purpura: a proposed study of the Transfusion Medicine/Hemostasis clinical trials network with a systematic review of rituximab therapy for immune-mediated disorders. J Clin Apher. 2006;21(1):49–56.
Zheng XL, Vesely SK, Cataland SR, Coppo P, Geldziler B, Iorio A, et al. ISTH guidelines for the diagnosis of thrombotic thrombocytopenic purpura. J Thromb Haemost. 2020;18(10):2486–95.
Scully M, Hunt BJ, Benjamin S, Liesner R, Rose P, Peyvandi F, et al. Guidelines on the diagnosis and management of thrombotic thrombocytopenic purpura and other thrombotic microangiopathies. Br J Haematol. 2012;158(3):323–35.
Upadhya SR, Mahabala C, Kamat JG, Jeganathan J, Kumar S, Prabhu MV. Plasmapheresis in Sepsis-induced thrombotic microangiopathy: a Case Series. Indian J Crit Care Med. 2020;24(3):195–9.
Stegmayr BG. Apheresis as therapy for patients with severe sepsis and multiorgan dysfunction syndrome. Ther Apher. 2001;5(2):123–7.
Qu L, Kiss JE, Dargo G, Carcillo JA. Outcomes of previously healthy pediatric patients with fulminant sepsis-induced multisystem organ failure receiving therapeutic plasma exchange. J Clin Apher. 2011;26(4):208–13.
Weng J, Chen M, Fang D, Liu D, Guo R, Yang S. Therapeutic plasma Exchange protects patients with Sepsis-Associated disseminated intravascular coagulation by improving endothelial function. Clin Appl Thromb Hemost. 2021;27:10760296211053313.
Nguyen TC, Han YY, Kiss JE, Hall MW, Hassett AC, Jaffe R, et al. Intensive plasma exchange increases a disintegrin and metalloprotease with thrombospondin motifs-13 activity and reverses organ dysfunction in children with thrombocytopenia-associated multiple organ failure. Crit Care Med. 2008;36(10):2878–87.
Martin K, Borgel D, Lerolle N, Feys HB, Trinquart L, Vanhoorelbeke K, et al. Decreased ADAMTS-13 (a disintegrin-like and metalloprotease with thrombospondin type 1 repeats) is associated with a poor prognosis in sepsis-induced organ failure. Crit Care Med. 2007;35(10):2375–82.
Peigne V, Azoulay E, Coquet I, Mariotte E, Darmon M, Legendre P, et al. The prognostic value of ADAMTS13 (a disintegrin and metalloprotease with thrombospondin type 1 repeats, member 13) deficiency in septic shock patients involves interleukin-6 and is not dependent on disseminated intravascular coagulation. Crit Care. 2013;17(6):R273.
Kremer Hovinga JA, Zeerleder S, Kessler P, Romani de Wit T, van Mourik JA, Hack CE, et al. ADAMTS-13, von Willebrand factor and related parameters in severe sepsis and septic shock. J Thromb Haemost. 2007;5(11):2284–90.
Semeraro N, Ammollo CT, Semeraro F, Colucci M. Coagulopathy of acute sepsis. Semin Thromb Hemost. 2015;41(6):650–8.
Makatsariya AD, Slukhanchuk EV, Bitsadze VO, Khizroeva JKH, Tretyakova MV, Tsibizova VI, et al. Thrombotic microangiopathy, DIC-syndrome and COVID-19: link with pregnancy prothrombotic state. J Matern Fetal Neonatal Med. 2022;35(13):2536–44.
Chang JC. Sepsis and septic shock: endothelial molecular pathogenesis associated with vascular microthrombotic disease. Thromb J. 2019;17:10.
Morrell CN, Hilt ZT, Pariser DN, Maurya P. PAD4 and von willebrand factor link inflammation and thrombosis. Circ Res. 2019;125(5):520–2.
Acknowledgements
The authors would like to acknowledge the patient for her kind participation and permission to use the data. The authors would like to acknowledge all the Department of Intensive Care staff for their collaboration. The authors would like to thank Huilin Yang for his microbiological identification and Zibo Xiong for his participation.
Funding
Peking University Shenzhen Hospital supports this work. The funding supported the cost of publication. The funding was not used in any other aspect of the study, including its design, data collection, writing of the report, or decision to submit for publication.
Author information
Authors and Affiliations
Contributions
YL wrote the first draft of the manuscript. YL, LH and SZ were involved in draft revision and editing. BH, YT, YC and WL were involved in the clinical management of patients and data collection. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patients involved to publish this case report. On request, a copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Laboratory workup for thrombotic microangiopathy.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lin, Y., Huang, L., Tu, Y. et al. Case report of Salmonella derby septicemia complicated with co-occurrence of disseminated intravascular coagulation and thrombotic microangiopathy. BMC Infect Dis 22, 914 (2022). https://doi.org/10.1186/s12879-022-07913-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-022-07913-2