Abstract
Background
Low mixed or central venous saturation (S(c)vO2) can reveal global tissue hypoxia and therefore can predict poor prognosis in critically ill patients. Early goal directed therapy (EGDT), aiming at an ScvO2 ≥ 70%, has been shown to be a valuable strategy in patients with sepsis or septic shock and is incorporated in the Surviving Sepsis Campaign guidelines.
Methods
In this prospective observational multi-center study, we determined central venous pressure (CVP), hematocrit, pH, lactate and ScvO2 or SvO2 in a heterogeneous group of critically ill patients early after admission to the intensive care units (ICUs) in three Dutch hospitals.
Results
Data of 340 acutely admitted critically ill patients were collected. The mean SvO2 value was > 65% and the mean ScvO2 value was > 70%. With mean CVP of 10.3 ± 5.5 mmHg, lactate plasma levels of 3.6 ± 3.6 and acute physiology, age and chronic health evaluation (APACHE II) scores of 21.5 ± 8.3, the in-hospital mortality of the total heterogeneous population was 32.0%. A subgroup of septic patients (n = 125) showed a CVP of 9.8 ± 5.4 mmHg, mean ScvO2 values of 74.0 ± 10.2%, where only 1% in this subgroup revealed a ScvO2 value < 50%, and lactate plasma levels of 2.7 ± 2.2 mmol/l with APACHE II scores 20.9 ± 7.3. Hospital mortality of this subgroup was 26%.
Conclusion
The incidence of low ScvO2 values for acutely admitted critically ill patients is low in Dutch ICUs. This is especially true for patients with sepsis/septic shock.
Similar content being viewed by others
Background
Global tissue hypoxia as a result from systemic inflammatory response or circulatory failure is an important indicator of shock preceding multiple organ dysfunction syndrome (MODS). The development of MODS predicts outcome of the septic patient [1]. Unrecognized and untreated global tissue hypoxia increases morbidity and mortality. Accurate detection of global tissue hypoxia is therefore of vital importance. Physical findings, vital signs, measuring central venous pressure (CVP) and urinary output are of the utmost importance, but not always sufficient for accurate detection of global tissue hypoxia [2, 3].
It is now generally accepted that a decreased central venous oxygen saturation (ScvO2) obtained from a central venous catheter, can reveal a mismatch between oxygen supply and oxygen demand, hence global tissue hypoxia [1]. Decreased values predict poor prognosis after cardiovascular surgery [4], in severe cardiopulmonary disease [5], and in septic or cardiogenic shock [6, 7]. ScvO2 and SvO2 (mixed venous oxygen saturation) can therefore be used as hemodynamic goals during resuscitation. According to Rivers et al. [8], hemodynamic optimization demands 'early goal-directed therapy' (EGDT), including ScvO2-guided treatment. It was concluded that goal-oriented manipulation of cardiac preload, afterload and contractility, to achieve a balance between systemic oxygen delivery and oxygen demand, is a valuable strategy in patients with sepsis or septic shock during the resuscitation period in the emergency department (ED) [8]. More recently, as a result of this study, an EGDT treatment protocol was included in the 'Surviving Sepsis Campaign' guidelines [1]. Also, several studies on implementation of such a protocol, partially in combination with other recommendations, have been published over the last years [9–11].
Based on clinical experience it seemed that the syndrome targeted in the EGDT study [8] was not very common in intensive care units (ICUs) in The Netherlands, and thus EGDT was not commonly indicated. The main purpose of this study was to determine the incidence of low ScvO2 values in our geographical setting. We monitored a heterogeneous group of critically ill patients during unplanned admission in three Dutch multidisciplinary ICUs. Also, illustratively, we compared the subgroup of septic patients with the population of septic patients as described by Rivers et al. [8], with respect to ScvO2 and other baseline characteristics.
Methods
Study centers
We studied ICU populations in one academic ICU (the Academic Medical Center (AMC) in Amsterdam, The Netherlands) and two non-academic ICUs (Gelre Hospital (GH) location Lukas, in Apeldoorn, The Netherlands; Medical Center Leeuwarden (MCL) in Leeuwarden, The Netherlands). The AMC is a large teaching hospital where the ICU is a 28-bed 'closed format' department in which medical/surgical patients, including cardiothoracic and neurosurgical patients, are being treated. GH is an affiliated teaching hospital where the ICU is a 10-bed 'closed format' department. MCL is a large general teaching hospital in the north of The Netherlands, with a 14-bed 'closed format' mixed medical/surgical ICU, including cardiothoracic patients.
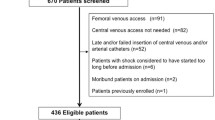
Patients and data collection
Between January 2006 and March 2007 a total of 340 patients, all 18 years or older, with a clinical indication for a central venous catheter (CVC) (BD Medical Systems, Singapore), pulmonary artery catheter (PAC) (Edwards Lifesciences LLC, Irvine, CA, USA) or Continuous Cardiac Output (CCO) catheter that measures SvO2 continuously (Arrow Deutschland GmbH, Erding, Germany) were recruited. Indication for a central venous, PAC or CCO catheter was left to the discretion of the attending physician. The patients arrived into the ICU either directly from the ED, from the general ward, or after acute surgery with severe sepsis, septic shock or cardiogenic shock, respiratory failure, central nervous problems, and other acute conditions. In the EDs, there was no standardized protocol for hemodynamic treatment of septic patients. Fluid resuscitation was mostly guided by blood pressure monitoring. Inotropes were given scarcely at the study EDs. Intubation in the ED was also uncommon. In the operating theatres no ScvO2/SvO2 measurements took place, nor any kind of goal-directed therapy implemented. All patients were treated according to standard practice for the ICU. Exclusion criteria were elective surgery and aged < 18 years. Collection of data for observational study without informed consent was approved by the Medical Ethics Committees of all three hospitals.
Measurements of systolic arterial pressure (SAP), mean arterial pressure (MAP) and central venous pressure (CVP) were recorded immediately after arrival into the ICU. Hematocrit (Hct), lactate plasma levels and pH were determined from the first obtained arterial blood sample in the ICU.
Acute physiology, age and chronic health evaluation (APACHE) II score [12] and sequential organ failure assessment (SOFA) score [13] at the time of admission into the ICU were also collected.
Statistical analysis
The statistical package SPSS 15.0.1 for Windows (SPSS Inc., Chicago, IL, USA)) was used for statistical analysis. All data were tested for normal distribution with the Kolmogorov-Smirnov test before further statistical analysis. Differences between populations were assessed using the Student's paired t test (normally distributed data). Data were displayed as mean ± SD. Statistical significance was assumed at p < 0.05.
Results
Patients
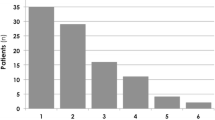
A heterogeneous population with a total of 340 critically ill patients was evaluated in the three participating ICUs (Table 1). The patients arrived into the ICU either directly from the ED (n = 135; 40%), from the general ward (n = 126; 37%) or after acute surgery (n = 79; 23%). To determine ScvO2 or SvO2 values, central venous or mixed venous oxygen saturation was measured as early as possible after insertion of a central venous catheter (n = 263) or pulmonary artery/CCO catheter (n = 77). The vast majority (93%) of the patients were enrolled within 6 h after presentation in the ER. More than 99% of all the data was obtained within 2 h after ICU admission. The numbers of measurements of central or mixed oxygen venous saturation were not normally distributed between the three ICUs. In all three hospitals the mean SvO2 was higher than 65% and mean ScvO2 was higher than 70%. Overall in-hospital mortality of our population was 32.0%.
In 263 patients venous oxygen saturation was measured centrally (Table 2). Mean ScvO2 was 72.0 ± 12.3%. A total of 38 patients (14%) had a ScvO2 < 60%, and only 14 (5%) patients had a ScvO2 < 50%. While only a single patient of the latter group was in septic shock, in-hospital mortality of these 14 patients was 57% (8/14).
Septic patients
In patients with sepsis or septic shock (n = 150) central venous oxygen was measured in 125 patients and mixed venous oxygen saturation was measured in 25 patients. The in-hospital mortality of our septic patients was 27%. A total of 73 patients arrived in the ICU from general wards (49%). The mean ScvO2 value was normal: 74.0 ± 10.2%. Only eight (6%) patients had a ScvO2 < 60%, and one (1%) < 50% (Table 2).
Comparison with the EGDT population
Compared to the Rivers study group our septic patients revealed a significantly higher ScvO2 (74.0 ± 10.2 vs 48.9 ± 12.3%; p < 0.01), lower lactate plasma levels (2.7 ± 2.2 vs 7.3 ± 4.6 mmol/l; p < 0.01), and lower hematocrit (30.3 ± 6.9 vs 34.7 ± 8.5%; p < 0.01). A total of 83% of patients needed endotracheal intubation versus 55% in the EGDT study [8]. APACHE II scores were equal (20.9 ± 7.0 vs 20.9 ± 7.2; p = 1.0). The in-hospital mortality of this subgroup was 26% (Table 2).
Mixed venous oxygen saturation
Measurement of mixed venous oxygen saturation took place in 77 patients. Mean SvO2 was 68.2 ± 11.8%. Mean lactate was 4.3 ± 4.2 mmol/l; arterial pH was 7.30 ± 0.11. With mean APACHE II scores of 21.8 ± 7.3 and mean SOFA scores of 9.3 ± 3.6, the in-hospital mortality was 37% (Table 3).
Of the 25 patients in whom mixed venous oxygen saturation was measured in the subgroup of septic patients, four (16%) patients showed a SvO2 value < 60% on admission. One patient (4%) had a SvO2 < 50%. In this relatively small subgroup, mean Hct was 28.2 ± 5.4%, mean MAP 61.0 ± 13.4 mmHg and mean CVP 13.7 ± 4.6 mmHg, while 80% (20/25 patients) needed mechanical ventilation. Mean APACHE II score was 22.2 ± 5.4 and mean SOFA score10.3 ± 3.7. The in-hospital mortality of this subgroup was 28% (Table 3).
Discussion
The main result of this present multi-center observational study is the low incidence of low ScvO2 values (< 50%) in septic patients being only 1%. Secondary findings were the normal mean ScvO2 values and normal mean SvO2 values in critically ill patients, including patients with severe sepsis or septic shock, on admission in the three ICUs.
Development of severe sepsis and septic shock involves several pathogenic changes, including global tissue hypoxia as a result of circulatory abnormalities [14]. In particular, hemodynamic optimization as a therapeutic target has been studied over the last decade [2, 8, 9, 15, 16]. Based on promising results from earlier studies [2], Rivers et al. randomized patients with severe sepsis or septic shock to standard therapy or EGDT. The latter resulted in an absolute reduction in 28-day mortality of 16% [8]. Improvement of the balance between oxygen delivery (DO2) and oxygen demand (VO2) played an important role. Other studies, however, found no reduction of morbidity or mortality as a result of aggressive hemodynamic optimization, despite higher central venous oxygenation or lower lactate concentrations [15, 16]. Studies that enrolled patients admitted into the ICU were unable to show a decrease in mortality rate after aggressive hemodynamic optimization [16, 17], in contrast to studies that implemented certain treatment protocols, including antibiotic therapy, in the emergency department [8, 9, 11]. In this ICU study we found mean ScvO2 and SvO2 values in the normal range. Similar figures are described previously in the later stage of sepsis and in ICU patients [18, 19]. This is in concordance with the findings by Gattinoni et al. (67, 3–69, 7%) [15] and Bracht et al. (70%) [20].
ScvO2 is a surrogate for SvO2: a significant correlation between the two has been described [21]. Although it might still be debatable whether central venous and mixed venous oxygen saturation are equivalent or not [18, 19, 21], the clinical importance of both measurements seems not to be an issue. The Surviving Sepsis Campaign recognizes such in the resuscitation portion of its severe sepsis and septic shock information [1]. Our study design does not allow for any statistical evaluation of ScvO2 compared to SvO2.
APACHE II scores were similar in comparison to the population described in the EGDT study [8]. This suggests equal mortality rate predictions. However, physiological scores such as APACHE II are dependent on variables that reflect the progression or reversal of organ dysfunction. Treatment in the ED or operating theatre prior to ICU admission influences calculation of the physiological scores. Consequently, the physiological scores at our ICUs could partially be underestimated. The significantly higher lactate plasma levels in the EGDT study suggest a more severe tissue hypoperfusion in that group. However, it is the clearance rate that is associated with less organ failure and improved survival [22].
Unlike significantly lower mean arterial pressures, the higher CVP and the lower hematocrit suggest that the septic patients were less hypovolemic compared to the EGDT population. Relatively high mean blood pressure in the EGDT population suggests an earlier stage of sepsis with predominating vasoconstriction, or pre-existing hypertension. The higher CVP in the subgroup with septic patients (n = 125) is partially the result of high percentage of endotracheal intubation and thus increased intrathoracic pressure before measurement (83%). In the EGDT study, less than 55% needed intubation at admission.
As mentioned earlier, in the present study the patients were treated in the ED, or elsewhere, before admission to the ICU. This treatment was different from the treatment given in the EGDT study. Nevertheless, our patients received some fluid therapy. Transfusion of red blood cells in our EDs was based on clinical suspicion or evidence of severe blood loss and not on low hematocrit only. Also, a main principle of treatment is to improve oxygen delivery and this could contribute to higher ScvO2 values in the ICU population compared to the patients described in the EGDT study and other ED studies. Other interventions such as sedation and analgesia, most often to facilitate endotracheal intubation and ventilation, might have been beneficial for the balance between oxygen delivery and oxygen demand. Also, the trend of changing ScvO2 and other physiological values influencing outcome [23, 24] is not taken into account in our study. Of course, all these factors are important differences between ER populations and ICU populations, but are not predominating. We are aware that comparison between those populations is limited by the above-mentioned differences.
As a result of the study design, statements about cut-off S(c)vO2 values for outcome prediction [20, 24] or impact on therapeutic intervention are not possible. Also, we did not investigate the use of vital signs as indicator of tissue oxygenation in comparison to mixed or central venous saturation. Lack of clear insight of treatment and time spent at the different EDs, operating theatres or wards is a limitation of our study as well. Nevertheless, since we also aimed at the usefulness of measuring ScvO2 or SvO2 on ICU admission, we think these factors are not pertinent to the results. For example, Bracht et al. [20] found no correlation between ScvO2 values and length of hospital stay before unplanned ICU admission.
Comparing our sepsis population with the ED population described in the important study by Rivers [8] is meant to be purely illustrative. Obviously, as we described, there are differences between ED and ICU populations in general. But there are also, depending on geographical setting, important differences between populations and health care systems. Therefore, we subscribe to the view of Ho et al. [25] that the syndrome described in the EGDT trial may be relatively uncommon depending on geographical setting and health care system. However, this does not undermine the importance of early identification of patients at high risk for cardiovascular collapse. For example, in our study of the 14 patients with a ScvO2 < 50%, the in-hospital mortality was 57%.
Finally, the in-hospital mortality in our study was 32.0% for the total population and 27.0% for the patients with severe sepsis or septic shock. Again this reflects recent findings by others: Ho et al. (30.2%) [25] and Shapiro et al. (26.9%) [26].
Conclusion
In conclusion, the incidence of low ScvO2 values for acutely admitted critically ill patients is low in Dutch ICUs. This is especially true for patients with sepsis/septic shock.
Key messages
The incidence of low ScvO2 values of acutely admitted critically ill patients is low in Dutch ICUs. This is especially true for patients with sepsis or septic shock.
In our setting, use of ScvO2-guided resuscitation may only be helpful in a small subset of sepsis.
Mean SvO2 values and mean ScvO2 values in acutely admitted critically ill patients, including patients with severe sepsis or septic shock, were normal in our ICUs.
Abbreviations
- AMC:
-
AMC = Amsterdam Medical Center
- APACHE = acute physiology:
-
age and chronic health evaluation
- CCO:
-
CCO = continuous cardiac output
- CI:
-
CI = confidence interval
- CVC:
-
CVC = central venous catheter
- CVP:
-
CVP = central venous pressure
- DO:
-
DO2DO = (systemic) oxygen delivery
- ED:
-
ED = emergency department
- EGDT:
-
EGDT = early goal directed therapy
- GH:
-
GH = Gelre Hospital
- Hct:
-
Hct = hematocrit
- ICU:
-
ICU = intensive care unit
- MAP:
-
MAP = mean arterial pressure
- MCL:
-
MCL = Medical Center Leeuwarden
- MODS:
-
MODS = multiple organ dysfunction syndrome
- PAC:
-
PAC = pulmonary artery catheter
- SAP:
-
SAP = systolic arterial pressure
- SAPS:
-
SAPS = simplified acute physiology score
- ScvO:
-
ScvO2 = central venous oxygen saturation
- SvO:
-
SvO2 = mixed venous oxygen saturation
- S(c)vO:
-
S(c)vO2S(c)vO = mixed/central venous oxygen saturation
- SOFA:
-
SOFA = sequential organ failure assessment
- VO:
-
VO2VO = (systemic) oxygen consumption.
References
Dellinger RP, Carlet JM, Masur H, Gerlach H, Calandra T, Cohen J, Gea-Banacloche J, Keh D, Marshall J, Parker MM, Ramsay G, Zimmerman JL, Vincent JL, Levy MM, for Surviving Sepsis Campaign: Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Crit Care Med 2004, 32: 858-873. 10.1097/01.CCM.0000117317.18092.E4
Rady MY, Rivers EP, Novak RM: Resuscitation of the critically ill in the ED: responses of blood pressure, heart rate, shock index, central venous oxygen saturation, and lactate. Am J Emerg Med 1996, 14: 218-225. 10.1016/S0735-6757(96)90136-9
Brun-Buisson C, Doyon F, Carlet J, Dellamonica P, Gouin F, Lepoutre A, Mercier JC, Offenstadt G, Regnier B: Incidence, risk factors, and outcome of severe sepsis and septic shock in adults: a multicenter prospective study in intensive care units; French ICU Group for Severe Sepsis. JAMA 1995, 274: 968-974. 10.1001/jama.274.12.968
Polonen P, Ruokonen E, Hippelainen M, Poyhonen M, Takala J: A prospective, randomized study of goal-oriented hemodynamic therapy in cardiac surgical patients. Anesth Analg 2000, 90: 1052-1059. 10.1097/00000539-200005000-00010
Kasnitz P, Druger Gl, Yorra F, Simmons DH: Mixed venous oxygen tension and hyperlactatemia. Survival in severe cardiopulmonary disease. JAMA 1976, 236: 570-574. 10.1001/jama.236.6.570
Krafft P, Steltzer H, Hiesmayr M, Klimscha W, Hammerle AF: Mixed venous oxygen saturation in critically ill septic shock patients. The role of defined events. Chest 1993, 103: 900-906. 10.1378/chest.103.3.900
Edwards JD: Oxygen transport in cardiogenic and septic shock. Crit Care Med 1991, 19: 658-663.
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Tomlanovich M, for the Early Goal-Directed Therapy Collaborative Group: Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 2001, 345: 1368-1377. 10.1056/NEJMoa010307
Shapiro NI, Howell MD, Talmor D, Lahey D, Ngo L, Buras J, Wolfe RE, Weiss JW, Lisbon A: Implementation and outcomes of the Multiple Urgent Sepsis Therapies (MUST) protocol. Crit Care Med 2006, 34: 1025-1032. 10.1097/01.CCM.0000206104.18647.A8
Trzeciak S, Dellinger RP, Abate NL, Cowan RM, Strauss M, Kilgannon H, Zanotti S, Parrillo JE: A 1-year experience with implementing early goal-directed therapy for septic shock in the emergency department. Chest 2006, 129: 225-232. 10.1378/chest.129.2.225
Kortgen A, Niederprüm , Bauer M: Implementation of an evidence-based "standard operating procedure" and outcome in septic shock. Crit Care Med 2006, 34: 943-949. 10.1097/01.CCM.0000206112.32673.D4
Knaus WA, Draper EA, Wagner DP, Zimmerman JE: APACHE II: a severity of disease classification system. Crit Care Med 1985, 13: 818-829. 10.1097/00003246-198510000-00009
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonca A, Bruining H, Reinhart CK, Suter PM, Thijs LG: The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 1996, 22: 707-710. 10.1007/BF01709751
Rangel-Frausto MS, Pittet D, Costigan M, Hwang T, Davis CS, Wenzel RP: The natural history of the systemic inflammatory response syndrome (SIRS): a prospective study. JAMA 1995, 273: 117-123. 10.1001/jama.273.2.117
Gattinoni L, Brazzi L, Pelosi P, Latini R, Tognoni G, Pesenti A, Fumagalli R – SvO2 collaborative group: A trial of goal-oriented hemodynamic therapy in critically ill patients. N Engl J Med 1995, 333: 1025-1032. 10.1056/NEJM199510193331601
Hayes MA, Timmins AC, Yau E, Palazzo M, Hinds CJ, Watson D: Elevation of systemic oxygen delivery in the treatment of critically ill patients. N Engl J Med 1994, 330: 1717-1722. 10.1056/NEJM199406163302404
Krafft P, Steltzer H, Hiesmayr , Klimscha , Hammerle AF: Mixed venous oxygen saturation in critically ill septic shock patients: The role of defined events. Chest 1993, 103: 900-906. 10.1378/chest.103.3.900
Reinhart K, Rudolph T, Bredle DL, Hannemann L, Cain SM: Comparison of ventral-venous to mixed-venous oxygen saturation during changes in oxygen supply/demand. Chest 1989, 95: 1216-1221. 10.1378/chest.95.6.1216
Varpula M, Karlsson S, Ruokonen E, Pettila V: Mixed venous oxygen saturation cannot be estimated by cantral venous oxygen saturation in septic shock. Intensive Care Med 2006, 32: 1336-1343. 10.1007/s00134-006-0270-y
Bracht H, Hängi M, Jeker B, Wegmüller N, Porta F, Tüller D, Takala J, Jakob SM: Incidence of low central venous oxygen saturation during unplanned admissions in a multidisciplinary ICU: an observational study. Crit Care 2007, 11: R2-R9. 10.1186/cc5144
Reinhart K, Kuhn H-J, Hartog C, Bredle DL: Continuous central venous and pulmonary artery oxygen saturation monitoring in the critically ill. Intensive Care Med 2004, 30: 1572-1578. 10.1007/s00134-004-2337-y
Nguyen HB, Rivers EP, Knoblich BP, Jacobsen G, Muzzin A, Ressler JA, Tomlanovich MC: Early lactate clearance is associated with improved outcome in severe sepsis and septic shock. Crit Care Med 2004, 32: 1637-1642. 10.1097/01.CCM.0000132904.35713.A7
Collaborative Study Group on Perioperative ScvO2 monitoring: Multicentre study on peri- and postoperative central venous oxygen saturation in high-risk surgical patients. Crit Care 2006, 10: R158-R165. 10.1186/cc5094
Pearse RM, Dawson D, Fawcett J, Rhodes A, Grounds M, Bennett ED: Changes in central venous saturation after major surgery, and association with outcome. Crit Care 2005, 9: R694-R699. 10.1186/cc3888
Ho BCH, Bellomo R, McGain F, Jones D, Naka T, Wan L, Braitsberg G: The incidence and outcome of septic shock patients in the absence of early-goal directed therapy. Crit Care 2006, 10: R80. 10.1186/cc4918
Shapiro NI, Wolfe RE, Moore RB, Smith E, Burdick E, Bates DW: Mortality in Emergency Department Sepsis (MEDS) score: a prospectively derived and validated clinical prediction rule. Crit Care Med 2003, 31: 670-675. 10.1097/01.CCM.0000054867.01688.D1
Acknowledgements
The authors would like to thank research nurse Matty Koopmans and Vivian Leeuwe for their invaluable help in the acquisition of patient data.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
PB drafted the manuscript, participated in coordination, and performed statistical analysis. JH was responsible for acquisition of patient data in AMC. MS participated in the design of the study and helped to draft the manuscript. CB provided general support. PS participated in the design of the study, was responsible for acquisition of patient data. in GH and helped to draft the manuscript. MK conceived of the study and participated in its design and coordination and helped to draft the manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
van Beest, P.A., Hofstra, J.J., Schultz, M.J. et al. The incidence of low venous oxygen saturation on admission to the intensive care unit: a multi-center observational study in The Netherlands. Crit Care 12, R33 (2008). https://doi.org/10.1186/cc6811
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/cc6811