Abstract
In this review, 21 original papers published last year in the respirology and critical care sections of Critical Care are classified and analyzed in the following categories: mechanical ventilation, lung recruitment maneuvers, and weaning; the role of positive end-expiratory pressure in acute lung injury models; animal models of ventilator-induced lung injury; diaphragmatic dysfunction; the role of mechanical ventilation in heart-lung interaction; and miscellanea.
Similar content being viewed by others
Introduction
Treatment of acute respiratory failure is one of the most difficult challenges in intensive care unit (ICU) management. The most important advance in decreasing mortality in patients with acute lung injury/acute respiratory distress syndrome (ALI/ARDS) has been the use of a low-tidal volume, lung protective ventilation strategy [1]. As such, there has been extensive research to explore the mechanisms of ALI in order to develop novel therapeutic approaches. Here, we review the key respiratory failure papers that appeared last year in Critical Care.
Mechanical ventilation, lung recruitment maneuvers, and weaning
Ventilation and perfusion mismatch, as a consequence of lung injury, leads to hypoxemia and can lead to hypercapnia. A previous study demonstrated that elevated values of dead-space fraction (Vd/Vt) are associated with increased risk of death in patients with ARDS [2].
Siddiki and colleagues [3] examined the utility of bedside calculation of pulmonary Vd/Vt in predicting the prognosis of patients with ALI/ARDS. The goal of the authors was to calculate Vd/Vt by using variables, such as minute ventilation (VE) and the arterial tension of carbon dioxide (PaCO2), that are readily available at the bedside. The authors used the rearranged alveolar gas equation: Vd/Vt = 1 - [(0.86 × VCO2est)/VE × PaCO2], where VCO2est represents the estimated carbon dioxide production derived from the modified Harris-Benedict equation. Data from two large databases of approximately 2,000 patients in total were used to calculate the Vd/Vt on days 1 and 3 of admission. A contingency analysis showed that higher Vd/Vt values were associated with higher mortality. For example, Vd/Vt values of less than 0.4 and greater than 0.8 were associated with hospital mortality rates of about 20% and 50%, respectively. This relationship was valid after adjustment for Acute Physiology and Chronic Health Evaluation III (APACHE III) score, presence of shock, hypoxemia, and positive end-expiratory pressure (PEEP).
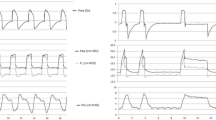
De Robertis and colleagues [4] employed two techniques to decrease dead space: flushing the ventilator circuit and aspiration of dead space (ASPID). In healthy pigs ventilated at a respiratory rate of up to 60 breaths per minute, the authors demonstrated that circuit flushing and ASPID were able to reduce the PaCO2 by 26% and 41%, respectively. These techniques are likely to be much more effective in healthy lungs than lungs with ALI, which have a high alveolar dead space. In addition, the combined effect of these two strategies to minimize dead space in ARDS remains to be determined.
In patients with otherwise-healthy lungs, the use of mechanical ventilation (MV) with large tidal volume, along with higher transpulmonary pressures, has been associated with the development of ALI/ARDS [5–7]. The predisposing factor for the development of ALI/ARDS is the duration of MV or an underlying systemic inflammatory response or both [8, 9]. Two studies published in Critical Care expanded these findings, supporting the concept that low-tidal volume ventilation prevents the development of ALI and attenuates innate immune response activation [6, 10].
Pinheiro de Oliveira and colleagues [10] randomly assigned 20 patients without ALI to low-tidal volume MV (5 to 7 mL of predicted body weight, or PBW) or high-tidal volume MV (10 to 12 mL/PBW). Patients in the lower tidal volume arm of the study had an attenuation of the lung inflammatory response after 12 hours, as demonstrated by reductions in bronchoalveolar lavage (BAL) concentrations of tumor necrosis factor-alpha (TNF-α) and interleukin-8 (IL-8).
In a larger prospective randomized clinical trial, Determann and colleagues [6] demonstrated that patients who initially did not have ALI were less likely to develop ALI if they were ventilated with a low-tidal volume strategy. One hundred fifty patients without ALI were randomly assigned to receive a tidal volume of 6 or 10 mL of PBW. The group of patients treated with lower tidal volumes had lower IL-6 plasma levels compared with the group ventilated with conventional tidal volume. Underlying risk factors for the development of ALI, oxygenation index, number of transfused blood products, and the baseline lung lavage-fluid IL-6 level were all associated with lung injury in the univariate analysis. Moreover, a multivariate analysis showed that tidal volume, together with the level of PEEP, was an independent predictor of ALI/ARDS development. However, the study was not powered to investigate various risk factors for ALI/ARDS separately in a multivariate model; it is possible that the PEEP levels may be simply a marker of disease severity. Unfortunately, this study was stopped early at the second interim analysis, even though the trends for duration of MV and mortality rate in the two groups were similar. This early stopping may have overestimated the treatment effects [11].
Constantin and colleagues [12] showed the beneficial effect of lung recruitment maneuvers (LRMs) in reversing acute hypoxemia immediately after intubation for acute respiratory failure. In this study, 44 patients with acute respiratory failure were randomly assigned to receive 40 cm H2O LRM for 30 seconds, or not, within 2 minutes after intubation. The patients treated with LRM had better oxygenation 5 minutes after intubation and this improvement persisted up to 30 minutes. The LRM strategy was not associated with significant hemodynamic impairment. After intubation, about 30% of the patients in both groups had blood cultures that were positive for the same bacteria that were present in the tracheal aspirate. However, as opposed to MV, LRM does not seem to be a risk factor for bacterial translocation.
Liberation from MV is one of the major challenges in the management of critically ill patients. Time spent in the weaning process represents 40% to 50% of the total duration of MV [13]. Many factors may negatively affect the ability to wean a patient from ventilator support. Neuropsychological problems play a significant role. Among these problems, agitation after withdrawal of sedation may have a great impact. Sztrymf and colleagues [14] showed the beneficial effect of loxapine, a neuroleptic agent, in mitigating agitation and facilitating weaning. Patients who were ventilated for more than 48 hours, who were ready for weaning, and who exhibited agitation after the reduction or withdrawal of sedation (a combination of benzodiazepines and opioid) were eligible for this study. Loxapine was well tolerated and significantly reduced agitation, as assessed by three different agitation scales, and improved breathing patterns until 180 minutes after administration.
Tracheostomy is advised for patients undergoing prolonged ventilation to improve patient comfort, reduce sedation, and facilitate liberation from MV. In a retrospective observational study, Wu and colleagues [15] compared the outcome of patients ventilated via tracheostomy or via the translaryngeal route in a respiratory care center. In this specific population, weaning success was similar in the two groups; however, there was a trend to lower mortality in the tracheostomy group.
The role of positive end-expiratory pressure in acute lung injury models
Increased vascular permeability and lung edema are the key features of ALI and ARDS. PEEP is applied during MV to increase functional residual capacity (FRC), to redistribute edema fluid, and to decrease ventilator-induced lung injury (VILI). Alveolar fluid clearance (AFC) by alveolar epithelial cells is a major mechanism for edema resolution after injury. In healthy pigs, Garcia-Delgado and colleagues [16] showed that PEEP actively participates in AFC. The authors demonstrated that, after intra-tracheal administration of saline (4 or 10 mL/kg), PEEP of 10 cm H2O induced an increase in AFC, which occurred earlier in the presence of less severe edema.
In recent years, the role of PEEP has been extensively investigated to clarify its physiological effects in patients with ARDS and to define its role in protective ventilation strategies. However, after exciting results of the ARMA (Respiratory Management in Acute Lung Injury/Acute Respiratory Distress Syndrome) study limiting tidal volume, three randomized controlled trials failed to demonstrate further improvement in mortality by higher PEEP levels [17]. Higher PEEP levels can increase the end-expiratory lung volume, but degree of recruitability is quite variable in patients with ARDS [18], and not all patients with ARDS may benefit from higher levels of PEEP. An ideal PEEP level in each patient should be set on the basis of individualized and physiologically based measurements.
Krebs and colleagues [19] demonstrated that an 'open lung' ventilation strategy using high-frequency oscillation ventilation (HFOV) or conventional mechanical ventilation (CMV) has the potential to mitigate VILI compared with CMV with low PEEP. After surfactant lavage, rats were randomly assigned to one of three ventilation strategies: CMV with low PEEP, CMV with high PEEP, or HFOV. The open lung approach, whether applied with CMV or HFOV, reduced VILI compared with the low-PEEP group. HFOV was superior to CMV only with respect to oxygenation. A notable strength of this study was the physiological method used to set PEEP in the CMV open lung group; this PEEP value corresponded to the minimum respiratory system elastance. Moreover, to make the two ventilation strategies comparable, the investigators set the HFOV mean airway 2 cm H2O above the mean airway pressure measured during CMV and 'best PEEP'.
Assisted modes of MV have the potential to maintain diaphragm activation, which can be associated with clearance of some atelectatic areas in the dependent lung zones. There are two potential advantages: first, improvement in gas exchange by a reduction of shunt and, second, attenuation of VILI by a reduction of non-aerated and overinflated area. Using a surfactant lavage model, Gama de Abreu and colleagues [20] randomly assigned pigs to one of three different ventilation strategies: pressure support ventilation (PSV), bilevel positive airway pressure (BPAP) + spontaneous breathing (SB), and BIPAP without SB. Compared with the PSV strategy, the BIPAP + SB strategy was able to reduce the amount of opening/closing and hyperinflated area as assessed by dynamic computed tomography (CT) scan analysis of the lung. Moreover, this aeration pattern was associated with a lower tidal volume. Interestingly, the SB activity during BIPAP may mitigate some mechanism of VILI, but further studies are warranted.
Electrical impedance tomography is a relatively new non-invasive, real-time, radiation-free, bedside imaging tool that has the potential to individualize lung protective ventilation. It is based on the principle that electrical currents generated at the surface of the thorax result in different voltages, depending on the underlying tissue impedance. A reconstruction algorithm gives the anatomical distribution of ventilation or perfusion of the area of interest or both. The global inhomogeneity (GI) index was recently introduced to quantify the degree of inhomogeneity of lung aeration and may be useful in minimizing the risk of volutrauma and atelectrauma. Zhao and colleagues [21] demonstrated, in 10 healthy anesthetized patients, that the PEEP value identified at the lowest value of the GI index was in good agreement with the PEEP value derived by the maximum global dynamic compliance and the compliance-volume curve methods. However, future studies to address the feasibility of this approach in patients with ALI/ARDS are needed.
Severe abdominal hypertension may be associated with a critical FRC reduction caused by a collapse of dependent lung areas and by increasing chest wall elastance. Regli and colleagues [22] demonstrated, in a pig model of abdominal hypertension, that predetermined PEEP levels of up to 15 cm H2O were not able to counterbalance the FRC decrease induced by the high abdominal pressure of 26 mm Hg. This study highlighted the critical role of transpulmonary pressure as a key determinant of alveolar recruitment and VILI, especially when chest wall elastance is increased.
MV with higher PEEP levels and LRMs may be part of a lung protective ventilation strategy [23]. Hypotension is one of the most common complications during the application of LRM. To counterbalance the negative effect of LRM on venous return, fluid boluses are used. In a sepsis model of ALI and 1 hour of MV, Silva and colleagues [24] shed light on the potential detrimental effects of hypervolemia by increasing shear stress injury to the lung. The authors demonstrated that hypervolemia (with colloid infusion) and LRM were associated with increased lung injury and higher inflammatory and fibrogenic responses as demonstrated by a more pronounced detachment of the alveolar-capillary membrane, increased levels of vascular cell adhesion molecule-1 (VCAM-1), and procollagen III (PC III) mRNA lung expression.
Animal models of ventilator-induced lung injury
MV with high pressures, in the absence of adequate levels of PEEP, has been shown to cause lung injury, including pulmonary edema, epithelial/endothelial cell damage, and innate immune responses such as neutrophil recruitment and macrophage activation. Statins have been shown to modulate the inflammatory immune response during ischemia-reperfusion [25], peritonitis [26], and aerosolized lipopolysaccharide (LPS) [27], likely by their inhibition of the hydroxy-methylglutaryl coenzyme A reductase. All of these conditions can induce lung injury and may be exacerbated by MV. Müller and colleagues [28] showed, in a mouse model of VILI, that the administration of simvastatin mitigated lung injury caused by large-tidal volume MV. Mice treated with simvastatin had greater oxygenation, better vascular integrity, and less pulmonary inflammation. Moreover, simvastatin treatment mitigated endothelial cell injury as demonstrated by a reduction in cell swelling as assessed by electron microscopy.
Neutrophilic alveolitis is a cardinal feature of the acute phase of ALI/ARDS. Modulation of the neutrophil inflammatory response could be important in improving outcomes in ALI/ARDS. Neutrin 1 is a protein, first described in central nervous system development, which is downregulated in the lung during the acute phase of ALI. Mutz and colleagues [29] showed that, after ALI was induced by LPS challenge, the anti-inflammatory protein neutrin 1, nebulized into the lungs of pigs or administered intravenously, attenuated the lung and systemic inflammatory response. The treated animals had decreased histopathological signs of pulmonary inflammation and a reduction of BAL and serum concentrations of IL-6 and TNF-α. Notably, the efficacy of the intervention was also evident on the degree of pulmonary edema and infiltrates on CT scan.
Mechanical stretch of the lung enhances oxidative stress [30, 31], which can contribute to the pathogenesis of VILI by increasing alveolar and vascular permeability [32, 33]. Recently, molecular hydrogen (H2) was shown to selectively reduce the hydroxyl radical, which is the most cytotoxic of reactive oxygen species (ROS) [34]. In a mouse model of VILI, Huang and colleagues [35] compared the inhalation of two different gases: nitrogen and hydrogen. Compared with inhalation of nitrogen, that of hydrogen mitigated VILI. Inhalation of hydrogen was associated with increased expression of anti-apoptotic genes and with an attenuation of histopathological and inflammatory markers of VILI.
Diaphragmatic dysfunction: the role of mechanical ventilation and endotoxemia
Controlled MV is one of the most important risk factors for diaphragm dysfunction and is associated with rapid atrophy and enhanced muscular proteolysis [36]. Moreover, muscular weakness is an important disability in ARDS survivors [37].
In a small series of 10 ICU patients, Hermans and colleagues [38] measured twitch transdiaphragmatic pressure (TwPdi) by using bilateral anterior magnetic phrenic nerve stimulation (BAMPS). They demonstrated a 70% reduction in diaphragm force compared with healthy individuals; most of the patients were septic and had received corticosteroids. Moreover, there was a logarithmic relationship between TwPdi and the duration of MV and cumulative dose of piritramide and propofol.
ICU-acquired muscular weakness is a common complication of critical illness; moreover, its incidence in the subgroup of patients with sepsis has been reported to be 50% to 100%. Increased proteolysis by activation of the proteasome system, oxidative stress, and acquired channelopathy involving dysregulation of sodium channels have all been shown to participate in sepsis-induced muscular weakness. Labbe and colleagues [39] highlighted the importance of protein monocyte chemoattractant protein-1 (MCP-1) as contributing to diaphragm weakness after endotoxemia. In a mouse model of endotoxemia, there was impairment of diaphragmatic contractility along with upregulation of MCP-1. Treatment with an antibody blocking MCP-1 restored the force frequency of the diaphragm to levels observed in non-septic mice. Of note, the increased expression of MCP-1 after the endotoxic challenge was not associated with increased leukocyte infiltration, suggesting a direct role of the protein in the pathogenesis of endotoxic diaphragm weakness.
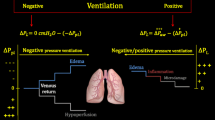
Effects of mechanical ventilation on heart-lung interactions
Non-invasive ventilation - continuous positive airway pressure (CPAP) and non-invasive BIPAP ventilation - are considered safe and effective treatment options in acute cardiogenic pulmonary edema (ACPE) [40]. In a retrospective study, Aliberti and colleagues [41] demonstrated that the majority of patients with ACPE had acidosis on arrival to the emergency department. CPAP corrected the acidosis in many of these patients. Moreover, in patients treated with CPAP, the presence of both respiratory and metabolic acidosis was not a risk factor for clinical deterioration as determined by the need for BIPAP, tracheal intubation, and hospital mortality.
Right ventricle (RV) dysfunction and failure are serious conditions in the ICU, usually occurring in the context of left ventricular failure, pulmonary embolism, pulmonary hypertension, sepsis, or ALI or after cardiothoracic surgery. RV dysfunction is difficult to diagnose and manage at the bedside. In a systematic review of the literature, Price and colleagues [42] provided an excellent overview of the pathogenesis, diagnosis, and treatment options, focusing on the most commonly used vasoactive drugs to improve RV function and to reduce afterload. Of interest, Guyatt and colleagues [43] used the GRADE (Grading of Recommendations Assessment, Development and Evaluation) system to make recommendations that potentially could help clinicians face this challenging heart dysfunction.
Miscellanea
Ischemia reperfusion injury, as occurs in the post-resuscitative phase of hemorrhagic shock, is characterized by organ damage caused by activation of the innate immune response and oxidative stress. Ganster and colleagues [44] used a rat model of ischemia reperfusion injury induced by controlled hemorrhage and demonstrated that sodium hydrosulfide treatment significantly reduced vascular dysfunction in vivo and release of ROS in vitro as demonstrated by paramagnetic resonance in the heart and aorta.
Abbreviations
- ACPE:
-
acute cardiogenic pulmonary edema
- AFC:
-
alveolar fluid clearance
- ALI:
-
acute lung injury
- ARDS:
-
acute respiratory distress syndrome
- ASPID:
-
aspiration of dead space
- BAL:
-
bronchoalveolar lavage
- BIPAP:
-
bilevel positive airway pressure
- CMV:
-
conventional mechanical ventilation
- CPAP:
-
continuous positive airway pressure
- CT:
-
computed tomography
- FRC:
-
functional residual capacity
- GI:
-
global inhomogeneity
- HFOV:
-
high-frequency oscillation ventilation
- ICU:
-
intensive care unit
- IL:
-
interleukin
- LPS:
-
lipopolysaccharide
- LRM:
-
lung recruitment maneuver
- MCP-1:
-
monocyte chemoattractant protein-1
- MV:
-
mechanical ventilation
- PaCO2:
-
arterial tension of carbon dioxide
- PBW:
-
predicted body weight
- PEEP:
-
positive end-expiratory pressure
- PSV:
-
pressure support ventilation
- ROS:
-
reactive oxygen species
- RV:
-
right ventricle
- SB:
-
spontaneous breathing
- TNF-α:
-
tumor necrosis factor-alpha
- TwPdi:
-
twitch transdiaphragmatic pressure
- VCO2est:
-
estimated carbon dioxide production
- Vd/Vt:
-
dead-space fraction
- VE:
-
minute ventilation
- VILI:
-
ventilator-induced lung injury.
References
National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network: Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. N Engl J Med 2000, 342: 1301-1308.
Nuckton TJ, Alonso JA, Kallet RH, Daniel BM, Pittet JF, Eisner MD, Matthay MA: Pulmonary dead-space fraction as a risk factor for death in the acute respiratory distress syndrome. N Engl J Med 2002, 346: 1281-1286. 10.1056/NEJMoa012835
Siddiki H, Kojicic M, Li G, Yilmaz M, Thompson TB, Hubmayr RD, Gajic O: Bedside quantification of dead-space fraction using routine clinical data in patients with acute lung injury: secondary analysis of two prospective trials. Crit Care 2010, 14: R141. 10.1186/cc9206
De Robertis E, Uttman L, Jonson B: Re-inspiration of CO(2) from ventilator circuit: effects of circuit flushing and aspiration of dead space up to high respiratory rate. Crit Care 2010, 14: R73. 10.1186/cc8986
Gajic O, Dara SI, Mendez JL, Adesanya AO, Festic E, Caples SM, Rana R, St Sauver JL, Lymp JF, Afessa B, Hubmayr RD: Ventilator-associated lung injury in patients without acute lung injury at the onset of mechanical ventilation. Crit Care Med 2004, 32: 1817-1824. 10.1097/01.CCM.0000133019.52531.30
Determann RM, Royakkers A, Wolthuis EK, Vlaar AP, Choi G, Paulus F, Hofstra JJ, de Graaff MJ, Korevaar JC, Schultz MJ: Ventilation with lower tidal volumes as compared with conventional tidal volumes for patients without acute lung injury: a preventive randomized controlled trial. Crit Care 2010, 14: R1. 10.1186/cc8230
Yilmaz M, Keegan MT, Iscimen R, Afessa B, Buck CF, Hubmayr RD, Gajic O: Toward the prevention of acute lung injury: protocol-guided limitation of large tidal volume ventilation and inappropriate transfusion. Crit Care Med 2007, 35: 1660-1666. quiz 1667 10.1097/01.CCM.0000269037.66955.F0
Schultz MJ, Haitsma JJ, Slutsky AS, Gajic O: What tidal volumes should be used in patients without acute lung injury? Anesthesiology 2007, 106: 1226-1231. 10.1097/01.anes.0000267607.25011.e8
Mascia L, Zavala E, Bosma K, Pasero D, Decaroli D, Andrews P, Isnardi D, Davi A, Arguis MJ, Berardino M, Ducati A, Brain IT group: High tidal volume is associated with the development of acute lung injury after severe brain injury: an international observational study. Crit Care Med 2007, 35: 1815-1820. 10.1097/01.CCM.0000275269.77467.DF
Pinheiro de Oliveira R, Hetzel MP, dos Anjos Silva M, Dallegrave D, Friedman G: Mechanical ventilation with high tidal volume induces inflammation in patients without lung disease. Crit Care 2010, 14: R39. 10.1186/cc8919
Villar J, Slutsky AS: Is acute respiratory distress syndrome an iatrogenic disease? Crit Care 2010, 14: 120. 10.1186/cc8842
Constantin JM, Futier E, Cherprenet AL, Chanques G, Guerin R, Cayot-Constantin S, Jabaudon M, Perbet S, Chartier C, Jung B, Guelon D, Jaber S, Bazin JE: A recruitment maneuver increases oxygenation after intubation of hypoxemic intensive care unit patients: a randomized controlled study. Crit Care 2010, 14: R76. 10.1186/cc8989
Boles JM, Bion J, Connors A, Herridge M, Marsh B, Melot C, Pearl R, Silverman H, Stanchina M, Vieillard-Baron A, Welte T: Weaning from mechanical ventilation. Eur Respir J 2007, 29: 1033-1056. 10.1183/09031936.00010206
Sztrymf B, Chevrel G, Bertrand F, Margetis D, Hurel D, Ricard JD, Dreyfuss D: Beneficial effects of loxapine on agitation and breathing patterns during weaning from mechanical ventilation. Crit Care 2010, 14: R86. 10.1186/cc9015
Wu YK, Tsai YH, Lan CC, Huang CY, Lee CH, Kao KC, Fu JY: Prolonged mechanical ventilation in a respiratory-care setting: a comparison of outcome between tracheostomized and translaryngeal intubated patients. Crit Care 2010, 14: R26. 10.1186/cc8890
Garcia-Delgado M, Touma-Fernandez A, Chamorro-Marin V, Ruiz-Aguilar A, Aguilar-Alonso E, Fernandez-Mondejar E: Alveolar fluid clearance in healthy pigs and influence of positive end-expiratory pressure. Crit Care 2010, 14: R36. 10.1186/cc8914
Briel M, Meade M, Mercat A, Brower RG, Talmor D, Walter SD, Slutsky AS, Pullenayegum E, Zhou Q, Cook D, Brochard L, Richard JC, Lamontagne F, Bhatnagar N, Stewart TE, Guyatt G: Higher vs lower positive end-expiratory pressure in patients with acute lung injury and acute respiratory distress syndrome: systematic review and meta-analysis. JAMA 2010, 303: 865-873. 10.1001/jama.2010.218
Grasso S, Fanelli V, Cafarelli A, Anaclerio R, Amabile M, Ancona G, Fiore T: Effects of high versus low positive end-expiratory pressures in acute respiratory distress syndrome. Am J Respir Crit Care Med 2005, 171: 1002-1008. 10.1164/rccm.200407-940OC
Krebs J, Pelosi P, Tsagogiorgas C, Zoeller L, Rocco PR, Yard B, Luecke T: Open lung approach associated with high frequency oscillatory or low tidal volume mechanical ventilation improves respiratory function and minimizes lung injury in healthy and injured rats. Crit Care 2010, 14: R183. 10.1186/cc9291
Gama de Abreu M, Cuevas M, Spieth PM, Carvalho AR, Hietschold V, Stroszczynski C, Wiedemann B, Koch T, Pelosi P, Koch E: Regional lung aeration and ventilation during pressure support and biphasic positive airway pressure ventilation in experimental lung injury. Crit Care 2010, 14: R34. 10.1186/cc8912
Zhao Z, Steinmann D, Frerichs I, Guttmann J, Moller K: PEEP titration guided by ventilation homogeneity: a feasibility study using electrical impedance tomography. Crit Care 2010, 14: R8. 10.1186/cc8860
Regli A, Hockings LE, Musk GC, Roberts B, Noffsinger B, Singh B, van Heerden PV: Commonly applied positive end-expiratory pressures do not prevent functional residual capacity decline in the setting of intra-abdominal hypertension: a pig model. Crit Care 2010, 14: R128. 10.1186/cc9095
Fan E, Wilcox ME, Brower RG, Stewart TE, Mehta S, Lapinsky SE, Meade MO, Ferguson ND: Recruitment maneuvers for acute lung injury: a systematic review. Am J Respir Crit Care Med 2008, 178: 1156-1163. 10.1164/rccm.200802-335OC
Silva PL, Cruz FF, Fujisaki LC, Oliveira GP, Samary CS, Ornellas DS, Maron-Gutierrez T, Rocha NN, Goldenberg R, Garcia CS, Morales MM, Capelozzi VL, Gama de Abreu M, Pelosi P, Rocco PR: Hypervolemia induces and potentiates lung damage after recruitment maneuver in a model of sepsis-induced acute lung injury. Crit Care 2010, 14: R114. 10.1186/cc9063
Naidu BV, Woolley SM, Farivar AS, Thomas R, Fraga C, Mulligan MS: Simvastatin ameliorates injury in an experimental model of lung ischemia-reperfusion. J Thorac Cardiovasc Surg 2003, 126: 482-489. 10.1016/S0022-5223(03)00699-8
Fischetti F, Carretta R, Borotto G, Durigutto P, Bulla R, Meroni PL, Tedesco F: Fluvastatin treatment inhibits leucocyte adhesion and extravasation in models of complement-mediated acute inflammation. Clin Exp Immunol 2004, 135: 186-193. 10.1111/j.1365-2249.2003.02358.x
Fessler MB, Young SK, Jeyaseelan S, Lieber JG, Arndt PG, Nick JA, Worthen GS: A role for hydroxy-methylglutaryl coenzyme a reductase in pulmonary inflammation and host defense. Am J Respir Crit Care Med 2005, 171: 606-615.
Muller HC, Hellwig K, Rosseau S, Tschernig T, Schmiedl A, Gutbier B, Schmeck B, Hippenstiel S, Peters H, Morawietz L, Suttorp N, Witzenrath M: Simvastatin attenuates ventilator-induced lung injury in mice. Crit Care 2010, 14: R143. 10.1186/cc9209
Mutz C, Mirakaj V, Vagts DA, Westermann P, Waibler K, Konig K, Iber T, Noldge-Schomburg G, Rosenberger P: The neuronal guidance protein netrin-1 reduces alveolar inflammation in a porcine model of acute lung injury. Crit Care 2010, 14: R189. 10.1186/cc9301
Broccard AF, Feihl F, Vannay C, Markert M, Hotchkiss J, Schaller MD: Effects of L-NAME and inhaled nitric oxide on ventilator-induced lung injury in isolated, perfused rabbit lungs. Crit Care Med 2004, 32: 1872-1878. 10.1097/01.CCM.0000139605.38527.1B
Peng X, Abdulnour RE, Sammani S, Ma SF, Han EJ, Hasan EJ, Tuder R, Garcia JG, Hassoun PM: Inducible nitric oxide synthase contributes to ventilatorinduced lung injury. Am J Respir Crit Care Med 2005, 172: 470-479. 10.1164/rccm.200411-1547OC
Haddad IY, Pataki G, Hu P, Galliani C, Beckman JS, Matalon S: Quantitation of nitrotyrosine levels in lung sections of patients and animals with acute lung injury. J Clin Invest 1994, 94: 2407-2413. 10.1172/JCI117607
Beckman JS, Beckman TW, Chen J, Marshall PA, Freeman BA: Apparent hydroxyl radical production by peroxynitrite: implications for endothelial injury from nitric oxide and superoxide. Proc Natl Acad Sci USA 1990, 87: 1620-1624. 10.1073/pnas.87.4.1620
Ohsawa I, Ishikawa M, Takahashi K, Watanabe M, Nishimaki K, Yamagata K, Katsura K, Katayama Y, Asoh S, Ohta S: Hydrogen acts as a therapeutic antioxidant by selectively reducing cytotoxic oxygen radicals. Nat Med 2007, 13: 688-694. 10.1038/nm1577
Huang CS, Kawamura T, Lee S, Tochigi N, Shigemura N, Buchholz BM, Kloke JD, Billiar TR, Toyoda Y, Nakao A: Hydrogen inhalation ameliorates ventilatorinduced lung injury. Crit Care 2010, 14: R234. 10.1186/cc9389
Levine S, Nguyen T, Taylor N, Friscia ME, Budak MT, Rothenberg P, Zhu J, Sachdeva R, Sonnad S, Kaiser LR, Rubinstein NA, Powers SK, Shrager JB: Rapid disuse atrophy of diaphragm fibers in mechanically ventilated humans. N Engl J Med 2008, 358: 1327-1335. 10.1056/NEJMoa070447
Herridge MS, Tansey CM, Matté A, Tomlinson G, Diaz-Granados N, Cooper A, Guest CB, Mazer CD, Mehta S, Stewart TE, Kudlow P, Cook D, Slutsky AS, Cheung AM, Canadian Critical Care Trials Group: Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med 2011, 364: 1293-1304. 10.1056/NEJMoa1011802
Hermans G, Agten A, Testelmans D, Decramer M, Gayan-Ramirez G: Increased duration of mechanical ventilation is associated with decreased diaphragmatic force: a prospective observational study. Crit Care 2010, 14: R127. 10.1186/cc9094
Labbe K, Danialou G, Gvozdic D, Demoule A, Divangahi M, Boyd JH, Petrof BJ: Inhibition of monocyte chemoattractant protein-1 prevents diaphragmatic inflammation and maintains contractile function during endotoxemia. Crit Care 2010, 14: R187. 10.1186/cc9295
Gray A, Goodacre S, Newby DE, Masson M, Sampson F, Nicholl J: Noninvasive ventilation in acute cardiogenic pulmonary edema. N Engl J Med 2008, 359: 142-151. 10.1056/NEJMoa0707992
Aliberti S, Piffer F, Brambilla AM, Bignamini AA, Rosti VD, Maraffi T, Monzani V, Cosentini R: Acidemia does not affect outcomes of patients with acute cardiogenic pulmonary edema treated with continuous positive airway pressure. Crit Care 2010, 14: R196. 10.1186/cc9315
Price LC, Wort SJ, Finney SJ, Marino PS, Brett SJ: Pulmonary vascular and right ventricular dysfunction in adult critical care: current and emerging options for management: a systematic literature review. Crit Care 2010, 14: R169. 10.1186/cc9264
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schunemann HJ: GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008, 336: 924-926. 10.1136/bmj.39489.470347.AD
Ganster F, Burban M, de la Bourdonnaye M, Fizanne L, Douay O, Loufrani L, Mercat A, Cales P, Radermacher P, Henrion D, Asfar P, Meziani F: Effects of hydrogen sulfide on hemodynamics, inflammatory response and oxidative stress during resuscitated hemorrhagic shock in rats. Crit Care 2010, 14: R165.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Fanelli, V., Zhang, H. & Slutsky, A.S. Year in review 2010: Critical Care - respirology. Crit Care 15, 240 (2011). https://doi.org/10.1186/cc10541
Published:
DOI: https://doi.org/10.1186/cc10541