Abstract
Background
Agenesis of the isthmus associated with nontoxic solitary nodular goiter is a rare congenital anomaly. Imaging data exceptionally has been previously reported in the English language literature.
Case presentation
Preoperative assessment of a 22-year-old white man patient showed an asymptomatic nodule of the thyroid at the left lobe, measuring 2.3 × 1.5 cm in diameter without regional lymphadenopathy. At surgical exploration it was seen an absence of the thyroid isthmus.
Conclusion
Thyroid isthmus agenesis does not cause clinical symptoms by itself and most of the times the diagnosis is incidental due to the existence of other thyroid pathology.
Similar content being viewed by others
Background
An isolated thyroid isthmus agenesis is very uncommon. The true incidence of this condition is very difficult to be determined, since the patients have been found in a euthyroid state. Thyroid isthmus agenesis does not cause clinical symptoms by itself and most of the times the diagnosis is incidental due to the existence of other thyroid pathology [1].
Case presentation
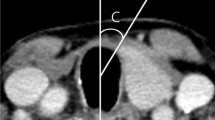
In 2005 a 22-year-old white man patient was referred for treatment of arterial hypertension. On his first physical examination it was seen an asymptomatic nodule at the medium part of the left lobe, measuring 1.5 cm in diameter without regional lymphadenopathy. The ultrasound exam showed a topical thyroid with a solitary 2.3 × 1.5 cm heterogenous nodule with areas of cystic degeneration. The echo/doppler investigation displayed a peripheral flux. On this occasion a fine-needle aspiration cytology was made and results showed papilliferous cells without malignancy features. Immunohistochemical study for cytokeratin-19 marker was positive. One year later, a second ultrasonography showed the enlargement of the nodule by reaching 2.7 × 2.5 cm (Figure 1). Thyroid isthmus agenesis was found (Figure 2) during the access to the gland and a left lobectomy was performed. Histologic examination yielded to the diagnosis of nodular goiter.
Discussion
Most of the descriptions in the literature about congenital thyroid abnormalities are related with hemiagenesis which include one lobe and sometimes the isthmus. Thus congenital thyroid anomalies can involve one or both lobes and the isthmus may be present or not. Over 50.000 thyroid patients operations at Mayo Clinic during 40 years, only five cases of hemiagenesis were described [1]. Mirkosch et al [2] during a 9 years studied 71 500 patients who underwent thyroid investigation. Ten of them had isthmus hemiagenesis. Others surgical studies reported an incidence nearby one in 2000 [1, 3]. Melnick [1] and Mikosch [2] on two reviews of available world literature found, respectively a total of 94 and 256 cases of thyroid hemiagenesis but among these cases the isthmus was absent in only 50% of the patients where the isthmus was specifically mentioned.
There are a variety of diseases associated with thyroid partial agenesis and most of them are cases of hyperthyroidism or hypothyroidism in iodine deficient area and also nontoxic nodular goiter [1, 2, 4, 5].
Mutation of genes has been involved in thyroid morphogenesis [5] but failure of the isthmus fusion in the midline may be the principal cause of an isolate isthmus agenesis.
Ultrasonography is still the key investigation to diagnose isthmus agenesis but the presence of other pathological conditions diverts the attention and misleads the diagnosis. The use of both computed tomography (CT) and magnetic resonance imaging does not offer best results than ultrasonography itself which can be performed easily and quickly, with less cost and no radiation risk as seen at CT. Furthermore taking into account the performance of these three diagnostic methods to identify the morphology of thyroid, the results are equivalent.
In asymptomatic patients with nodular goiters fine-needle aspiration biopsies and eventually immunohistochemistry tests are useful to support the medical decision but when agenesis is present the importance of pre-operative differentiation between benign and malign lesion is critical, considering the surgical procedure and the possibility of impairment of the thyroid function.
Conclusion
Isolate agenesis of the isthmus associated with nontoxic solitary nodular goiter seems to be an unusual condition and imaging data exceptionally has been previously reported in the English language literature.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. If necessary a copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
Melnick JC, Stemkowski PE: Thyroid hemiagenesis (hockey stick sign): A review of the world literature and report of four cases. J Clin Endocrinol Metab. 1981, 52: 247-251.
Mikosch P, Gallowitsch HJ, Kresnik E, Molnar M, Gomez I, Lind P: Thyroid hemiagenesis in an endemic goiter area diagnosed by ultrasonography: Report of sixteen patients. Thyroid. 1999, 9 (11): 1075-84.
Harada T, Nichikawa Y, Ito K: Aplasia of one thyroid lobe. Am J Surg. 1972, 123: 617-619. 10.1016/0002-9610(72)90098-0.
McHenry CR, Walfish PG, Rosen IB, Lawrence AM, Paloyan E: Congenital thyroid hemiagenesis. Am Surg. 1995, 61: 634-638.
Karaby N, Comlekci A, Canda MS, Bayraktar F, Degirmenci B: Thyroid hemiagenesis with miltinodular goiter: A case report and review of the literature. Endocr J. 2003, 50: 409-413. 10.1507/endocrj.50.409.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
AS performed the surgery and PJOJ made substantial contributions to acquisition of data. Both had important contribution in writing the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Schanaider, A., de Oliveira, P.J. Thyroid isthmus agenesis associated with solitary nodule: A case report. Cases Journal 1, 211 (2008). https://doi.org/10.1186/1757-1626-1-211
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1757-1626-1-211