Abstract
Background
Community-Associated Methicillin Resistant Staphylococcus aureus (CA-MRSA) has traditionally been related to skin and soft tissue infections in healthy young patients. However, it has now emerged as responsible for severe infections worldwide, for which vancomycin is one of the mainstays of treatment. Infective endocarditis (IE) due to CA-MRSA with heterogeneous vancomycin-intermediate susceptibility-(h-VISA) has been recently reported, associated to an epidemic USA 300 CA-MRSA clone.
Case Presentation
We describe the occurrence of h-VISA phenotype in a case of IE caused by a strain belonging to an epidemic CA-MRSA clone, distinct from USA300, for the first time in Argentina. The isolate h-VISA (SaB2) was recovered from a patient with persistent bacteraemia after a 7-day therapy with vancomycin, which evolved to fatal case of IE complicated with brain abscesses. The initial isolate-(SaB1) was fully vancomycin susceptible (VSSA). Although MRSA SaB2 was vancomycin susceptible (≤2 μg/ml) by MIC (agar and broth dilution, E-test and VITEK 2), a slight increase of MIC values between SaB1 and SaB2 isolates was detected by the four MIC methods, particularly for teicoplanin. Moreover, Sab2 was classified as h-VISA by three different screening methods [MHA5T-screening agar, Macromethod-E-test-(MET) and by GRD E-test] and confirmed by population analysis profile-(PAP). In addition, a significant increase in cell-wall thickness was revealed for SaB2 by electron microscopy. Molecular typing showed that both strains, SaB1 and SaB2, belonged to ST5 lineage, carried SCCmec IV, lacked Panton-Valentine leukocidin-(PVL) genes and had indistinguishable PFGE patterns (subtype I2), thereby confirming their isogenic nature. In addition, they were clonally related to the epidemic CA-MRSA clone (pulsotype I) detected in our country.
Conclusions
This report demonstrates the ability of this epidemic CA-MRSA clone, disseminated in some regions of Argentina, to produce severe and rapidly fatal infections such as IE, in addition to its ability to acquire low-level vancomycin resistance; for these reasons, it constitutes a new challenge for the Healthcare System of this country.
Similar content being viewed by others
Background
Community-associated methicillin resistant Staphylococcus aureus-(CA-MRSA) has rapidly become the main cause of S. aureus infections worldwide since 1993. These non-multiresistant strains frequently harbor staphylococcal-cassette-chromosome-(SCCmec) types IV or V and Panton-Valentine leukocidin-(PVL) genes. The worldwide increase of CA-MRSA infections is due to the dissemination of some epidemic CA-MRSA clones harboring pvl genes (PVL+), with a specific geographical pattern, these are frequently designated by their multilocus sequence type (MLST) or by their pulsed field gel electrophoresis (PFGE) pattern ( ST1, ST8-USA300, ST30, ST59, ST93 and ST80) [1–4].
Although CA-MRSA was initially related to skin and soft tissue infections, it has now emerged as a cause of severe infections worldwide [1]. Vancomycin has traditionally been the mainstay of therapy for these serious MRSA infections, thereby the emergence of resistance to this agent is of great concern [5, 6]. Heterogeneous vancomycin intermediate S. aureus (h-VISA) is an isolate of S. aureus with a vancomycin MIC within the susceptible range (≤2 μg/ml) when tested by routine methods, containing subpopulations of cells (typically at a frequency of ≤10-5 to 10-6) with intermediate resistance to vancomycin (VISA: MIC 4-8 μg/ml) [5]. This type of resistance is associated with a thickened cell-wall that prevents vancomycin action over its target within the cytoplasmic membrane. The exact mechanisms leading to this thickening have not been determined yet [5].
Lately, cases of infective endocarditis (IE) caused by CA-MRSA, mainly associated with the USA300 genotype have been reported [7–9]. More recently, phenotype h-VISA related to USA300 CA-MRSA clone has also been described [3, 10–12]. On the other hand, t he emergence of a ST5-IV clone PVL+ among CA-MRSA strains in Argentina was detected in 2005 [4, 13].
We report the occurrence of h-VISA phenotype in a case of IE caused by this epidemic CA-MRSA clone for the first time in this country.
Case Presentation
On April 4, 2009, a 73-year-old female with sudden weakness in the extremities was admitted at Institution A. On admission, she was afebrile and the head computed tomography (CT) was normal. She had underlying chronic rheumatic valve disease and chronic atrial fibrillation. She had no previous exposure to healthcare personnel or hospital environment during the previous year. Forty-eight hours after admission, the patient developed fever (38°C) and depression of the sensorium; hence, she was transferred to the Intensive Care Unit (ICU). Abdominal CT scan and echo-Doppler of the carotid vessels were normal.
MRSA grew in three blood cultures (SaB1-strain) and one urine culture (SaU-strain) taken upon admission in the ICU on April 7. A transthoracic echocardiography (TE) showed a filamentous mobile image attached to the ventricular side of the aortic valve, which resembled vegetations, suggesting a MRSA infection that met Duke's criteria for IE [14]. These isolates were susceptible to ciprofloxacin, gentamicin, rifampicin, tetracycline, trimethoprim-sulfamethoxazole-(TMP-SMX) and linezolid by disk diffusion and broth microdilution methods (see Additional file 1, Table S1) [15] and resistant to erythromycin and clindamycin (inducible resistance, D-test positive) [15]. In addition, vancomycin MIC was 1 μg/ml by broth dilution method [15]. Vancomycin treatment (15 mg/kg every 12 h) was initiated on April 7 and the patient was transferred to "Hospital-Militar-Regional-Córdoba-(HMRC)" for further evaluation on April 8. Antibiotic levels in blood were not available, so the same dose of vancomycin was continued; which is recommended to maintain the level of vancomycin in the valley of 10-15 μg/ml. The patient had fever of 39.2°C accompanied by Janeway's lesions on the hands. On April 9, valve replacement was postponed because of a worsening of the neurological symptoms and hypotension. Roth's spots were detected. The brain CT revealed no changes. On April 12, the patient presented hemodynamic and neurological improvement; a transoesophageal echocardiography (TEE) showed a highly mobile vegetation on the aortic valve (Figure 1). On April 14, the patient had altered mental status and persistent fever. Brain magnetic resonance-image-MRI with gadolinium showed multiple abscesses (Additional file 2, Figure S1). On April 15, since the patient worsened, valve replacement was postponed again; treatment failure was suspected and trimethoprim/sulfamethoxazole (15 mg/kg/day) was added to vancomycin. On April 17, the patient remained febrile, three new samples for blood culture taken on April 14 revealed MRSA (strain SaB2) with the same susceptibility to antibiotics, except for vancomycin, which reached a MIC of 2 μg/ml (broth dilution [15]. On April 20, the patient was afebrile. Three additional sets of blood cultures were drawn providing negative results. On April 24, a control TEE (Figure 1) showed a slight decrease of the size of the aortic valve vegetation and a new vegetation on the mitral valve. The patient had evident deterioration of mental and physical status and died on April 25 before surgical intervention.
Transesophageal echocardiography of a patient with infective endocarditis caused by CA-MRSA with phenotype h-VISA, Argentina. Left: On April 12, the highly mobile vegetation on the aortic valve (AV) of 20 × 41 mm (white arrow). Right: On April 24, slight decrease in the aortic valve (AV) vegetation (white arrow) and a new vegetation on the mitral valve (MV) (10 × 4.6 mm) of low motility (white arrow).
The emergence of h-VISA phenotype in a CA-MRSA was suspected based on the rapid and fatal outcome of the patient, the facts that the IE was caused by MRSA without multiresistance to antibiotics, failure of vancomycin therapy (defined as persistent fever and bacteraemia longer than 7 days after onset of therapy) and increase of vancomycin MICs values (1 to 2 μg/ml) within therapy. This prompted us to further analyze these strains. The blood (SaB1 and SaB2) and urine (SaU) MRSA isolates were sent to the CIBICI ("Centro de Investigaciones en Bioquimica Clinica e Inmunologia"; UNC-CONICET); for additional analysis including molecular and genetic characterization.
Phenotypic and genotypic characterizations of MRSA
The slight increase of MIC values between the initial (SaU and SaB1) and subsequent (SaB2) isolates was detected by four MICs methods [15], particularly for teicoplanin (Table 1). The isolates were also sent to the "Instituto-Nacional-de-Enfermedades-Infecciosas Dr. Carlos G. Malbrán" to independently confirm the MIC results for vancomycin and teicoplanin. Moreover, SaB2 was classified as h-VISA by three screening methods, MHA5T-screening agar, Macromethod-E-test-(MET) and GRD E-test (Table 1) [5]. Although MRSA SaB2 was vancomycin susceptible by MIC, it grew in BHI agar containing 4.0 μg/mL of vancomycin at a frequency of 1.6 × 10-6 on population analysis profile-(PAP) [16, 17], which is consistent with h-VISA (Additional file 3, Figure S2). Vancomycin MICs by broth-dilution; agar-dilution and E-test were determined for these derivatives and all were between 4 and 8 μg/ml. Neither MRSA SaB1 isolate nor S. aureus ATCC 29213 grew in BHI agar with 4 μg/ml. In addition, electron microscopy examination [5, 18] of SaB2 and one derivative VISA obtained on PAP, revealed that the cell-wall of both isolates was thicker (p < 0.001) than the parent strain SaB1 (Figure 2), a feature observed for most strains with VISA and h-VISA phenotypes. Moreover, the h-VISA phenotype found in strain SaB2 was unstable, since vancomycin MICs in all isolates with MICs ≥2 μg/ml reverted to MICs ≤1 μg/ml (susceptible phenotype-VSSA) after multiple subcultures in absence of vancomycin. Importantly, the detection by PCR [11] of vanA and vanB genes was negative.
Transmission electron microscopy of initial isolate (SaB1)-VSSA vs. after persistent bacteremia isolate (SaB2)-h-VISA. Comparison of the cell thickness among the pair of strains (SaB2 vs SaB1) and one derivative VISA (CIM 4 μg/ml) obtained on PAP (PAPd4). Quality control strains included S. aureus ATCC 29213 and Mu50, control, negative and positive for VISA, respectively. Magnification: × 60,000. Values given under each image are mean ± SD of the cell wall thickness in nanometers. Student's t test demonstrated that this augment in cell wall thickness was statistically significant (p < 0.001).
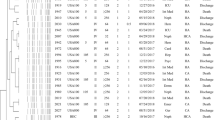
The clinical isolates (SaU, SaB1 and SaB2) and the derivatives obtained on PAP were analyzed by PFGE, MLST, SCCmec and spa typing, in addition to the detection of virulence genes by PCR, as previously reported [4]. Molecular typing revealed that all these isolates had indistinguishable pulsotypes (subtype I2) (Additional file 4, Figure S3) and were characterized as ST5, agr- 2, spa-t045, associated to SCCmec-IV. The egc (seg, sei, sem, sen and seo) and lukED genes were detected among all the virulence genes analyzed by PCR in these three isolates. They do not harbor pvl and sea genes. The results confirmed the isogenic nature of these isolates and their clonality with the CA-MRSA clone (pulsotype I) detected in our country (Additional file 4, Figure S3).
Discussion
Currently, PVL negative CA-MRSA strains belonging to some successful PVL positive CA-MRSA clones (ST1, ST59, ST5) or to the new one (ST72) have been detected, particularly in Europe and Asian-Pacific countries [1, 19–21]. In the case of the CA-MRSA IE reported here, the molecular typing revealed that although these strains share the same successful lineage ST5 with CA-MRSA (ST5-IV) and -HA-MRSA (ST5-I) epidemic clones disseminated in this country, their PFGE pattern is closer to that of the CA-MRSA clone (one band of difference with I1, additional Figure 3). Moreover, this isolate carries the SCCmec type IV and is non-multiresistant to antibiotics. Consequently, results identify a PVL-negative variant (PVL-) of the ST5-IV CA-MRSA epidemic clone detected in Argentina. Importantly, this clone belongs to lineage ST5, which has been demonstrated [5] to develop the VISA phenotype, but so far associated to HA-MRSA clones (ST5-II), unlike our case. These characteristics could confer another selective advantage for its dissemination in Argentina and neighboring countries.
Presently, strains of MRSA demonstrating the h-VISA or VISA phenotype have been reported in many countries worldwide, but in Latin America, cases with these phenotypes have been reported only in Northern countries and Brazil [3, 5]. Furthermore, only one case of CA-MRSA infective endocarditis from Brazil has been reported for South America, but not associated to a h-VISA strain like our case[22]. In Argentina, the h-VISA phenotype in MRSA strains was detected for the first time in 2009. Thus, our case is the first one associated to persistent bacteremia under vancomycin therapy. Three additional cases were independently detected in Buenos Aires during the same year (presented at "Congreso Argentino de Infectología -SADI 2010" and at "XX-Congreso Latinoamericano de Microbiología; Montevideo-2010", unpublished data). Even in infections with "high-risk" of presence of h-VISA phenotype, such as IE, the prevalence of h-VISA varies significantly and is potentially associated with non-clinical factors, such as geographic location [14]. Hence, the knowledge about general and molecular epidemiology of h-VISA phenotype in different countries is essential for effective prevention and therapy.
On the other hand, the cases of CA-MRSA IE subsequently published occurred in healthy young patients without classical risk factors for IE [7]. This report, along with another case of CA-MRSA IE recently described in Italy, [8] support the importance of considering this emergent pathogen as a potential cause of IE for subjects with risk for IE (elderly patients, pre-existing heart diseases, etc). Hence, our report adds new information about CA-MRSA associated to h-VISA phenotype epidemiology, which is a matter of great interest in clinical microbiology and molecular epidemiology worldwide.
In addition, our case highlights the difficulties of laboratory detection of h-VISA-phenotype, particularly when it is unstable and arises from a fully susceptible VSSA isolate (vancomycin MIC ≤1 μg/ml) under treatment with vancomycin. Furthermore, upon detection, the choice of appropriate therapy still remains difficult [5, 6]. Daptomycin, vancomycin, teicoplanin, linezolid, TMP-SMX, and quinupristin-dalfopristin are potential options for the treatment of MRSA bacteraemia [6, 23, 24]. The treatment of our patient raises several questions and reflects the lack of evidence-based data to guide the choice of therapy for CA-MRSA IE caused for isolates expressing h-VISA phenotype with vancomycin MICs of 2 μg/ml [5, 6]. Our patient received vancomycin as first line therapy at recommended doses [6, 23]. However, due to the clinical worsening of the patient, which prevented the valvular surgery, in addition to the presence of brain abscesses, we decided to add TMP-SMX to vancomycin, even before knowing that vancomycin MIC value had risen to 2 μg/ml. TMP-SMX has bactericidal activity in-vitro and it may be considered to be an alternative therapy to vancomycin for MRSA infection [6, 24–26]. In our patient, although the last set of blood cultures may have been negative for different reasons, including changes in renal function, TMP-SMX apparently contributed to bacteraemia clearance. Only few cases of patients with persistent bacteraemia have been treated with TMP-SMX in addition to vancomycin, late in the course of bacteriemia, but these are not enough to assess the clinical outcome [27]. Daptomycin was not considered due to the potential risks in patients with bacteremia, in which a deep focus of infection has not been surgically debrided, as well as for patients with left-side endocarditis [28], two characteristics seen in our patient.
One of the limitations of this report is the absence of measurements of vancomycin serum concentrations due to technical problems of the clinical laboratory at that time. Hence, although we think that, considering the clinical characteristics of the patient, the dose of vancomycin that she received should have been enough to reach or even exceed the recommended therapeutic level [6, 27], we cannot demonstrate it. In summary, the failure of vancomycin to eradicate this CA-MRSA strain was likely due to the presence of several important factors: I) high-bacterial-load during infection, combined with the impossibility to perform the cardiac surgery, II) slow bactericidal mechanism of vancomycin, III) the ability of this CA-MRSA clone to develop h-VISA phenotype and IV) the virulence of the CA-MRSA strain, possibly related to the metastatic complications and rapid progression [5, 23].
Conclusions
This report demonstrates the ability of this epidemic CA-MRSA clone, disseminated in some regions of Argentina, to cause severe and rapidly fatal infections such as infective endocarditis, in addition to its capacity to acquire low-level vancomycin resistance; for this reason, it has become a challenge for the healthcare system in our country. Therefore, systematic surveillance along to molecular epidemiology and quick diffusion of the results in each region are crucial for proper management of these infections.
Consent
Written informed consent was obtained from the patient's son for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal
References
David MZ, Daum RS: Community-associated methicillin-resistant Staphylococcus aureus: epidemiology and clinical consequences of an emerging epidemic. Clin Microbiol Rev. 2010, 23: 616-87. 10.1128/CMR.00081-09
Deurenberg RH, Stobberingh EE: The molecular evolution of hospital- and community-associated methicillin-resistant Staphylococcus aureus. Curr Mol Med. 2009, 9: 100-15. 10.2174/156652409787581637
Reyes J, Rincon S, Diaz L, Panesso D, Contreras GA, Zurita J, Carrillo C, Rizzi A, Guzman M, Adachi J, Chowdhury S, Murray BE, Arias CA: Dissemination of methicillin-resistant Staphylococcus aureus USA300 sequence type 8 lineage in Latin America. Clin Infect Dis. 2009, 49: 1861-7. 10.1086/648426
Sola C, Saka HA, Vindel A, Bocco JL, Cordoba MRSA Collaborative Study Group: Emergence and dissemination of a community-associated methicillin-resistant Panton-Valentine leucocidin-positive Staphylococcus aureus clone sharing the sequence type 5 lineage with the most prevalent nosocomial clone in the same region of Argentina. J Clin Microbiol. 2008, 46: 1826-31. 10.1128/JCM.01949-07
Howden BP, Davies JK, Johnson PD, Stinear TP, Grayson ML: Reduced vancomycin susceptibility in Staphylococcus aureus, including vancomycin-intermediate and heterogeneous vancomycin-intermediate strains: resistance mechanisms, laboratory detection, and clinical implications. Clin Microbiol Rev. 2010, 23: 99-139. 10.1128/CMR.00042-09
Liu C, Bayer A, Cosgrove SE, Daum RS, Fridkin SK, Gorwitz RJ, Kaplan SL, Karchmer AW, Levine DP, Murray BE, Rybak MJ, Talan DA, Chambers HF: Clinical practice guidelines by the infectious diseases society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clin Infect Dis. 2011, 52: e18-55. 10.1093/cid/ciq146
Millar BC, Prendergast BD, Moore JE: Community-associated MRSA (CA-MRSA): an emerging pathogen in infective endocarditis. J Antimicrob Chemother. 2008, 61: 1-7. 10.1093/jac/dkm441
Bassetti M, Nicco E, Malgorzata M, Viscoli C, Valbusa A, Bongiorno D, Campanile F, Stefani S: Community associated methicillin resistant Staphylococcus aureus (CA-MRSA) infective endocarditis in Italy. J Infect. 2010, 61: 353-5.
Lee SY, Kim JY, Kim JH, Kim SY, Park C, Park YS, Seo YH, Cho YK: A case of primary infective endocarditis caused by community-associated methicillin-resistant Staphylococcus aureus in a healthy individual and colonization in the family. Yonsei Med J. 2009, 50: 152-5. 10.3349/ymj.2009.50.1.152
Hageman JC, Patel J, Franklin P, Miscavish K, McDougal L, Lonsway D, Khan FN: Occurrence of a USA300 vancomycin-intermediate Staphylococcus aureus. Diagn Microbiol Infect Dis. 2008, 62: 440-2. 10.1016/j.diagmicrobio.2008.08.005
Graber CJ, Wong MK, Carleton HA, Perdreau-Remington F, Haller BL, Chambers HF: Intermediate vancomycin susceptibility in a community-associated MRSA clone. Emerg Infect Dis. 2007, 13: 491-3. 10.3201/eid1303.060960
Cafiso V, Bertuccio T, Spina D, Campanile F, Bongiorno D, Santagati M, Sciacca A, Sciuto C, Stefani S: Methicillin resistance and vancomycin heteroresistance in Staphylococcus aureus in cystic fibrosis patients. Eur J Clin Microbiol Infect Dis. 2010, 29: 1277-85. 10.1007/s10096-010-1000-5
Gardella N, von Specht M, Cuirolo A, Rosato A, Gutkind G, Mollerach M: Community-associated methicillin-resistant Staphylococcus aureus, eastern Argentina. Diagn Microbiol Infect. 2008, 62: 343-7. 10.1016/j.diagmicrobio.2008.07.008.
Bae IG, Federspiel JJ, Miro JM, Woods CW, Park L, Rybak MJ, Rude TH, Bradley S, Bukovski S, de la Maria CG, Kanj SS, Korman TM, Marco F, Murdoch DR, Plesiat P, Rodriguez-Creixems M, Reinbott P, Steed L, Tattevin P, Tripodi MF, Newton KL, Corey GR, Fowler VG, : Heterogeneous vancomycin-intermediate susceptibility phenotype in bloodstream methicillin-resistant Staphylococcus aureus isolates from an international cohort of patients with infective endocarditis: prevalence, genotype, and clinical significance. J Infect Dis. 2009, 200: 1355-66. 10.1086/606027
Clinical and Laboratory Standards Institute: Performance standards for antimicrobial susceptibility testing. nineteenth informational supplement. CLSI, Wayne, Pennsylvania. 2009, M100-S19.
Sola C, Cortes P, Saka HA, Vindel A, Bocco JL, : Evolution and molecular characterization of methicillin-resistant Staphylococcus aureus epidemic and sporadic clones in Cordoba, Argentina. J Clin Microbiol. 2006, 44: 192-200. 10.1128/JCM.44.1.192-200.2006
Hiramatsu K, Hanaki H, Ino T, Yabuta K, Oguri T, Tenover FC: Methicillin-resistant Staphylococcus aureus clinical strain with reduced vancomycin susceptibility. J Antimicrob Chemother. 1997, 40: 135-6. 10.1093/jac/40.1.135
Petiti JP, De Paul AL, Gutierrez S, Palmeri CM, Mukdsi JH, Torres AI: Activation of PKC epsilon induces lactotroph proliferation through ERK1/2 in response to phorbol ester. Mol Cell Endocrinol. 2008, 289: 77-84. 10.1016/j.mce.2008.04.015
Lee SS, Kim YJ, Chung DR, Jung KS, Kim JS: Invasive infection caused by a community-associated methicillin-resistant Staphylococcus aureus strain not carrying Panton-Valentine leukocidin in South Korea. J Clin Microbiol. 2010, 48: 311-3. 10.1128/JCM.00297-09
Deleo FR, Otto M, Kreiswirth BN, Chambers HF: Community-associated meticillin-resistant Staphylococcus aureus. Lancet. 2010, 375: 1557-68. 10.1016/S0140-6736(09)61999-1
Coombs GW, Monecke S, Ehricht R, Slickers P, Pearson JC, Tan HL, Christiansen KJ, O'Brien FG: Differentiation of clonal complex 59 community-associated methicillin-resistant Staphylococcus aureus in Western Australia. Antimicrob Agents Chemother. 2010, 54: 1914-21. 10.1128/AAC.01287-09
Fortes CQ, Espanha CA, Bustorff FP, Zappa BC, Ferreira AL, Moreira RB, Pereira NG, Fowler VG, Deshmukh H: First reported case of infective endocarditis caused by community-acquired methicillin-resistant Staphylococcus aureus not associated with healthcare contact in Brazil. Braz J Infect Dis. 2008, 12: 541-3. 10.1590/S1413-86702008000600020
Boucher H, Miller LG, Razonable RR: Serious infections caused by methicillin-resistant Staphylococcus aureus. Clin Infect Dis. 2010, 51 (Suppl 2): S183-97.
Goldberg E, Paul M, Talker O, Samra Z, Raskin M, Hazzan R, Leibovici L, Bishara J: Co-trimoxazole versus vancomycin for the treatment of methicillin-resistant Staphylococcus aureus bacteraemia: a retrospective cohort study. J Antimicrob Chemother. 2010, 65: 1779-83. 10.1093/jac/dkq179
Corey GR: Staphylococcus aureus bloodstream infections: definitions and treatment. Clin Infect Dis. 2009, 48 (Suppl 4): S254-9.
Markowitz N, Quinn EL, Saravolatz LD: Trimethoprim-sulfamethoxazole compared with vancomycin for the treatment of Staphylococcus aureus infection. Ann Intern Med. 1992, 117: 390-8.
Maor Y, Hagin M, Belausov N, Keller N, Ben-David D, Rahav G: Clinical features of heteroresistant vancomycin-intermediate Staphylococcus aureus bacteremia versus those of methicillin-resistant S. aureus bacteremia. J Infect Dis. 2009, 199: 619-24. 10.1086/596629
Fowler VG, Boucher HW, Corey GR, Abrutyn E, Karchmer AW, Rupp ME, Levine DP, Chambers HF, Tally FP, Vigliani GA, Cabell CH, Link AS, DeMeyer I, Filler SG, Zervos M, Cook P, Parsonnet J, Bernstein JM, Price CS, Forrest GN, Fatkenheuer G, Gareca M, Rehm SJ, Brodt HR, Tice A, Cosgrove SE, S aureus Endocarditis and Bacteremia Study Group: Daptomycin versus standard therapy for bacteremia and endocarditis caused by Staphylococcus aureus. N Engl J Med. 2006, 355: 653-65. 10.1056/NEJMoa053783
Acknowledgements
This study was supported by the National Council for Scientific Research and Technology of Argentina (CONICET), Agencia Nacional de Promoción Científica y Tecnológica (ANPCyT - PICT 01630 to JLB), Secretaría de Ciencia y Técnica-Universidad Nacional de Córdoba (SECyT-UNC) and Agencia Córdoba Ciencia.
CS and JLB are career investigator members of CONICET. The reference strains Mu3 and Mu50 were kindly provided by Dr. Keiichi Hiramatsu, Department of Bacteriology, Juntendo University, Tokyo, Japan.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
CS participated in the design and coordination of the study, drafted the manuscript and carried out part of the molecular typing of the isolates. RL: participated in clinical infectious disease's diagnosis and treatment, helped drafting the manuscript and revised the manuscript critically for important intellectual content. MC and JG: contributed to clinical care of the patient and the collection and analyses of the clinical data. ALE and VH: carried out the methodology of glycopeptides susceptibility and part of the molecular typing of the isolates. PG, ED and MV: carried out the identification and antibiotic susceptibility of the isolates. AC: contributed to the methodology of glycopeptides susceptibility of the isolates. JPP and AT: carried out the transmission electron microscopy of the isolates.
AV: carried out part of the molecular typing of the isolates. JLB participated in the design of the study, helped drafting the manuscript and revised the manuscript critically for important intellectual content. All authors read and approved the final manuscript.
Electronic supplementary material
12941_2011_218_MOESM1_ESM.DOC
Additional file 1:Table S1: Antimicrobial susceptibility profile of urine-(SaU) isolate and blood isolates obtained before-(SaB1) and during-(SaB2) vancomycin therapy. CLSI: Clinical and Laboratory Standards Institute, MIC: Minimum inhibitory concentration by broth microdilution (VITEK 2) per CLSI guideline, R*: Inducible Clindamycin Resistance. (DOC 34 KB)
12941_2011_218_MOESM2_ESM.PDF
Additional file 2:Figure S1: MRI (two slices) showing brain abscesses (white arrows) in a patient with CA-MRSA infective endocarditis. MRI: magnetic resonance image (with gadolinium). (PDF 128 KB)
12941_2011_218_MOESM3_ESM.PDF
Additional file 3:Figure S2: Vancomycin population analysis profiles of initial isolate-(SaB1)-VSSA and after persistent bacteremia isolate-(SaB2)-h-VISA, despite vancomycin therapy SaB1: initial isolate, prior to vancomycin therapy. Also, hVISA and VISA reference strain Mu3 and Mu50 respectively and VSSA strain ATCC 29213. Briefly, PAP was performed by serial dilution of overnight BHIB culture and inoculation of BHI agar containing 0 to 8 μg/ml of vancomycin. Colonies were counted after incubation for 48 h in air at 35°C and plotted on a graph of the number of CFU/ml versus vancomycin concentration. (PDF 4 KB)
12941_2011_218_MOESM4_ESM.PDF
Additional file 4:Figure S3: PFGE-Analysis confirmed the clonality of the clinical isolates (SaU-SaB1-SaB2), belonging to CA-MRSA clone ST5-IV-PVL+. Sma I restriction patterns were indistinguishable for SaU (urine isolate), SaB1 (initial blood isolate) and SaB2 (later blood isolate), 1-5: five derivatives from SaB2 in PAPs (CIM ≥4 μg/ml), PFGE DNA pattern of representative of major clonal types belonging to ST5 lineage, both CA and HA-MRSA from Argentina, to be compared with subtype I2 CA-MRSA (ST5-IV-PVL¯): CA-MRSA I1 (ST5-IV-PVL+), HA-MRSA A1-Cordobes/Chilean clone (ST5-I) and HA-MRSA C1 Pediatric clone (ST100-IV). I6 refers to the PFGE pattern of a MSSA isolate from Córdoba, which shows a unique band difference with the I2 subtype, isolated from our patient. NC: NCTC 8325 control strain L: DNA molecular size markers in kb (lambda DNA ladder, Promega). (PDF 128 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Sola, C., Lamberghini, R.O., Ciarlantini, M. et al. Heterogeneous vancomycin-intermediate susceptibility in a community-associated methicillin-resistant Staphylococcus aureus epidemic clone, in a case of Infective Endocarditis in Argentina. Ann Clin Microbiol Antimicrob 10, 15 (2011). https://doi.org/10.1186/1476-0711-10-15
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1476-0711-10-15