Abstract
Background
Recovery of upper limb function after stroke is poor. The acute to subacutephase after stroke is the optimal time window to promote the recovery ofupper limb function. The dose and content of training providedconventionally during this phase is however, unlikely to be adequate todrive functional recovery, especially in the presence of severe motordisability. The current study concerns an approach to address thisshortcoming, through evaluation of the SMART Arm, a non-robotic device thatenables intensive and repetitive practice of reaching by stroke survivorswith severe upper limb disability, with the aim of improving upper limbfunction. The outcomes of SMART Arm training with or withoutoutcome-triggered electrical stimulation (OT-stim) to augment movement andusual therapy will be compared to usual therapy alone.
Methods/Design
A prospective, assessor-blinded parallel, three-group randomised controlledtrial is being conducted. Seventy-five participants with a first-everunilateral stroke less than 4 months previously, who present with severe armdisability (three or fewer out of a possible six points on the MotorAssessment Scale [MAS] Item 6), will be recruited from inpatientrehabilitation facilities. Participants will be randomly allocated to one ofthree dose-matched groups: SMART Arm training with OT-stim andusual therapy; SMART Arm training without OT-stim and usualtherapy; or usual therapy alone. All participants will receive 20 hours ofupper limb training over four weeks. Blinded assessors will conduct fourassessments: pre intervention (0-weeks), post intervention (4-weeks), 26weeks and 52 weeks follow-up. The primary outcome measure is MAS item 6. Allanalyses will be based on an intention-to-treat principle.
Discussion
By enabling intensive and repetitive practice of a functional upper limb taskduring inpatient rehabilitation, SMART Arm training with or without OT-stimin combination with usual therapy, has the potential to improve recovery ofupper limb function in those with severe motor disability. The immediate andlong-term effects of SMART Arm training on upper limb impairment, activityand participation will be explored, in addition to the benefit of trainingwith or without OT-stim to augment movement when compared to usual therapyalone.
Trial registration
Similar content being viewed by others
Background
Recovery of the upper limb after stroke is poor. Up to 80% of stroke survivors havesome upper limb disability during the acute to subacute phase after stroke. Byvarious estimates, only 5% to 20% demonstrate complete functional recovery [1–3]. Thus, stroke survivors with upper limb disability appear to be arehabilitation challenge. There is therefore, a pressing need to increase thepotential for functional recovery of the upper limb after stroke.
To drive recovery of function, it is recommended that training commence early and beintensive, repetitive and task-oriented [4–6]. However, stroke survivors with severe motor disability are often unableto participate in task-oriented training as they are incapable of generating levelsof volitional motor activity or control that are sufficient to engage in trainingtasks [7]. Further compounding their situation is a lack of access to interventionsthat make task-oriented practice possible [8]. It is therefore not surprising that priority is rarely given to upperlimb training by stroke survivors [9] or rehabilitation services [10–15] during inpatient rehabilitation. Yet, with stroke survivors spending upto 25% of a physiotherapy session inactive [15], there appears to be considerable scope within current therapeuticregimes to increase the delivery of task-oriented upper limb training.
To capitalise upon this opportunity, a non-robotic training device, the SMART Arm(Sensori-Motor Active Rehabilitation Training of the Arm) (Figure 1), was developed to enable stroke survivors with severe upperlimb disability to undertake intensive and repetitive task-oriented training. Thedevice was specifically designed so that stroke survivors with little to no muscleactivity could practice reaching, a fundamental upper limb function, along astraight-line path consistent with a normal reaching pattern. The device can be usedwith or without electrical stimulation to the lateral head of triceps brachii toaugment elbow extension and enhance completion of the reaching task. To optimise thepotential for motor learning, this device incorporates elements critical to skillacquisition, including active problem solving, augmented real-time feedback ofperformance, task progression that is tailored to each individual, motivation andencouragement.
To date, a 12-hour SMART Arm training program with or without electromyographic(EMG)-triggered electrical stimulation to triceps has been investigated in chronicstroke survivors with severe upper limb disability. Compared with the control group,those who underwent SMART Arm training with or without stimulation showed asignificant improvement in upper limb function (improvement in MAS6 item 6 score)that was sustained at 2 months follow-up [16], an improved ratio of triceps to biceps EMG activity during reaching [17], and greater corticospinal reactivity [18]. There were however, variations in the expression of additional benefitsderived from the use of EMG-triggered electrical stimulation. As this may have beendue to the use, by some individuals, of maladaptive patterns of EMG activity such asco-contraction of biceps and triceps, that could nonetheless trigger stimulation, anew method of outcome-triggered electrical stimulation (OT-stim) was developed.Here, electrical stimulation is triggered when initial goal directed motionsurpasses an individualised threshold. Thus, assistance by means of electricalstimulation (and reinforcement) occurs when the movement generated voluntarily iscommensurate with the desired outcome. In a pilot trial of SMART Arm with OT-stimduring inpatient rehabilitation, SMART Arm training (with or without OT-stim), ledto a significantly greater improvement in upper limb function as compared to usualtherapy alone [19]. In that these improvements were evident early after stroke, furtherinvestigation within the context of a larger trial is warranted [20].
Thus, the primary aim of the current randomised controlled trial (RCT) is todetermine the ability of SMART Arm training with or without OT-stim compared tousual therapy to improve upper limb function in stroke survivors with severe upperlimb disability undergoing inpatient rehabilitation. In addition, we will determinethe impact of the different training programs on upper limb impairment, activity andparticipation.
Methods/Design
Design
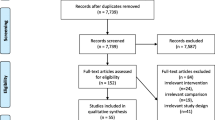
A prospective, assessor-blinded, three group parallel RCT will be conducted with75 stroke survivors with severe upper limb disability who are undertakinginpatient rehabilitation (Figure 2).
Location and setting
We plan to recruit stroke survivors from two inpatient rehabilitation serviceslocated in Brisbane, Australia: the Princess Alexandra Hospital, with a six-bedAcute Stroke Unit, located separately to a 78-bed Geriatric and RehabilitationUnit; and the Queen Elizabeth II Jubilee Hospital, which has a four bed AcuteStroke Unit, co-located within a 24-bed Geriatric and Rehabilitation Unit.Assessment and training will be undertaken in different areas of the samesite.
Population
All stroke survivors admitted to the Acute Stroke Unit at each hospital will bescreened for eligibility. Participants will be eligible if they are adult strokesurvivors (>17 years) with a primary diagnosis of first-ever unilateralstroke (ischaemic or haemorrhagic, including subarachnoid haemorrhage) less thanfour months previously, which has been confirmed either radiographically (CT orMRI) or clinically by the consulting physician; demonstrate severe upper limbdisability equivalent to a score of three or fewer out of a possible six points(inability to hold the upper limb in position when placed at 90° shoulderflexion in sitting) on the MAS item six; and are able to follow single-stagecommands, either with verbal instructions, demonstration or other non-verbalcues.
Participants will be excluded if they are medically unstable as defined by themedical registrar or by location in an acute medical ward; have upper limbcomorbidities that could limit their functional recovery (e.g., arthritis, pain,other neurological disorders); have a contraindication to the use of (e.g.,pacemaker insitu), or inability to tolerate, electrical stimulation (e.g.,hypersensitivity or skin condition); have an infectious disease requiring theuse of personal protective equipment (e.g., methicillin resistant staphylococcusaureus or vancomycin resistant enterococcus) or are unable to sit withoutsupport.
Randomisation and blinding
All participants will provide written informed consent. In the event that aparticipant is unable to provide informed consent, consent will be sought fromtheir legal guardian. After completion of the initial assessment, participantswill be randomised to one of three dose-matched groups (two intervention and onecontrol). The intervention groups are SMART Arm training with OT-stim(SMART Arm OT-stim) and usual therapy; SMART Arm training withoutOT-stim (SMART Arm alone) and usual therapy. The control group will receiveusual therapy only. Concealed randomisation will be prepared by an offsiteinvestigator, not involved in recruitment, intervention or data collection,using a computer generated random number sequence. Consecutively numbered,randomly ordered opaque envelopes containing group allocation in permuted blocksof four or six in a 1:1 ratio will be opened consecutively after baselineassessment in the presence of the participant. Usual therapists will be informedof group allocation.
Research assistants who enrol participants, and conduct pre, post and follow-upassessments will be blinded to group allocation throughout the study.Participant coding will not refer to group allocation and participants will beinstructed not to divulge information regarding their intervention to theassessors during assessment. Participants, SMART Arm trainers and usualtherapists (physiotherapy and occupational therapy) will not be blinded to groupallocation. To control expectancy effects for participants and usual therapists,it will be explained that it is not yet determined which therapy is moreeffective.
Intervention
All participants will receive 20 hours of upper limb therapy, comprising 60minutes duration five days per week for four weeks. The proposed volume oftraining was guided by discussions with each site and reports from these [15] and other facilities [21], along with previous SMART Arm research [16, 19]. All SMART Arm training and usual therapy will be recorded inindividual participant logbooks. If a participant misses a SMART Arm or usualtherapy session due to illness, medical procedure, or extended leave (e.g.,returned to acute medical ward as became unstable), additional days will beadded to ensure all participants are given the opportunity to complete a totalof 20-days of therapy.
SMART Arm training
SMART Arm training will be administered for 30 minutes per day by aphysiotherapist or occupational therapist, trained in the delivery of theintervention. The participant’s treating therapy team will administer30 minutes of usual therapy per day. Training will be typically undertakenfive times per week for four weeks.
On commencement of a SMART Arm training session, the participant will beseated on a (armless) chair beside the device. A harness will be applied torestrict trunk movements to less than 15 degrees and therefore, minimisecompensatory trunk movements and encourage recovery of a pre-morbid patternof reaching [22–24]. The affected upper limb will be positioned in a customisedthermoplastic splint in mid pronation-supination and wrist extension (0degrees to 45 degrees) to mimic a functional reach-to-grasp hand position [25]. To accommodate for any muscle contracture or pain, the splintcan be positioned through the full range of pronation and supination. Thesplint is connected to a manipulandum, which is mounted on a linear slideand encoder belt. The linear slide serves to constrain movement to one planeand to reduce friction and resistance to movement. The elbow is positionedin a standardized start position of 90 degrees of elbow flexion.
Trainers will be provided with guidelines for the administration of SMART Armtraining. To ensure participants perform a consistent minimum number ofrepetitions during the training time period (30 minutes), a goal of aminimum of 60 repetitions in week one and 80 repetitions in weeks twothrough four will be set. This dose was guided by previous research [16, 19]. Progression in training difficulty will occur when consistencyin task practice is evident. Training elements that can be progressedinclude the number of repetitions, track elevation, degree of shoulderexternal rotation, hand position, load, visual and auditory feedback,instruction and level of supervision. The decision-making process withregards to when and how to progress training will be at the discretion ofthe SMART Arm trainer and will be based on the stroke survivor’sperformance during training. To ensure consistency between trainers,monitoring (e.g., benchmarking evaluations of completed training logs forconsistent dose, progressions of practice used) and mentoring (e.g.,peer-supervision, feedback during sessions, and debriefing) will regularlyoccur. All SMART Arm training will be documented in a log, which willcapture dose and training element use.
Outcome-triggered electrical stimulation
The lateral head of triceps brachii is the target muscle of electricalstimulation as it is the prime mover for achievement of full elbowextension. Stimulation to triceps brachii will be delivered via an Empi300PV unit (St Paul, MN, USA). Two surface electrodes (diameter 50 mm)will be applied, one above the area of the triceps brachii motor point(lateral head) and one at the muscle insertion. Stimulation parameterswill consist of a 1 second ascending ramp, and a 4 to 20 second durationof 200-sec pulse width biphasic stimulation at 35 Hz. When training iscommenced, the participant will attempt to initiate the reaching task.As the participants’ reach attempt surpasses their individuallydetermined threshold distance, electrical stimulation to triceps brachiiwill be automatically triggered. The duration of stimulation providedwill be set manually to match the time required by each participant toperform the movement. The stimulus intensity will be set to the maximumthat can be tolerated by the participant.
Usual therapy
Participants allocated to usual therapy alone will participate in 20 therapysessions of 60 minutes duration, typically undertaken five days per week forfour weeks. Usual therapy refers to the combined duration of occupationaltherapy and physiotherapy. It will not be standardized and will likelyconsist of a mix of individual and group sessions administering both passive(e.g. stretching, cyclic electrical stimulation) and active (e.g. range ofmovement, strengthening, modified task practice with electrical stimulation)interventions where possible. All usual therapy will be documented in anupper limb therapy log, which will capture dose (minutes), frequency(sessions) and content of upper limb therapy.
Outcome measures
Arm function (impairment, activity and participation) will be assessed inaccordance with the ICF Classification of Functioning, Disability and Health [26]. All participants will be assessed at four time points: three daysprior to commencement of the intervention (baseline, 0 weeks), within one weekof completion of the intervention (post-intervention, 4 weeks), and followingcompletion of the intervention at 26 and 52 weeks. Assessors will be providedwith guidelines for administering the measures.
Demographic information about participants will be collected from their medicalrecord and will include age, gender, date of stroke onset, type (ischaemic orhaemorrhagic) and location (cortical, subcortical, cortical and subcortical orbrainstem) of stroke, stroke medical intervention (e.g. thrombolysis),co-morbidities and medications.
Primary outcome measure
The primary outcome measure will be performance on the MAS item 6 at the postintervention time period (4 weeks). The MAS is designed to measure recoveryof the affected limb over 3 task-related subscales (upper arm function, handand advanced hand movements) that are scored from 0–6. It is thestroke recovery scale most commonly used in clinical practice in Australiaand takes less than 10 minutes to complete. The reliability and validity ofthis measure with the stroke population has been previously documented [27]. It has been shown to be sensitive to change in performance inpeople with severe upper limb disability after training with SMART Arm [16, 19].
Secondary laboratory outcome measures
The functional force generating capacity of the impaired limb will beassessed using a dynamic and an isometric reaching task similar to previousprotocols [16, 17]. In both tasks, surface EMG activity will be collected fromtriceps brachii lateral head, biceps brachii, anterior deltoid, uppertrapezius, external rotators, lower trapezius and serratus anterior. EMGwill be obtained using single differential pre-amplified (gain 1000)parallel bar electrodes (Bagnoli, DELSYS, 8-channel System, Boston, MA, USA)with a fixed inter-electrode distance of 10 mm and positioned according toSENIAM guidelines [28]. A reference electrode will be attached over the bony prominenceof the seventh cervical spinous process. Signals will be sampled (1000Hz)using a Power 1401 Data Acquisition System (Cambridge Electronics Design,Cambridge, UK) and Spike2 software (version 6.02). Time series data will becollected and stored using Spike2 and processed using custom routines inMatlab (Mathworks Inc., Nattick, MA).
Participants will be seated at a custom-built apparatus with the upper limbin a pendant position, the elbow flexed and the forearm and hand restrainedin pronation via a custom built brace. For all measures a computer monitorpositioned directly in front of the participant will provide visual feedbackon a vertical bar scale. In the dynamic task, the brace will be secured to amanipulandum mounted on a linear slide restricting motion of the upper limbto flexion/ extension of the shoulder and elbow. A potentiometer attached tothe slide will measure transducer, reaching, linear displacement. The upperlimb will be placed at a standardised starting position with the elbow at 90degrees of flexion. Upon presentation of a tone, participants will berequired to ‘reach forward as far as possible’ in five separatetrials. In the isometric task, the participant will be required to pushforwards (elbow extension) in a position of 150 degrees of elbow flexionagainst a manipulandum instrumented to measure force. In five separatetrials, following a tone, participants will be instructed to ‘push ashard as possible’ and to keep pushing for five seconds. In both taskscontinuous visual feedback of the applied force will be provided along withverbal encouragement. During each contraction, force or reach distance andEMG recordings will be obtained. On the basis of these recordings, peakforce, distance, time to peak and the muscle onset times, amplitude(root-mean-square (RMS)) and triceps to biceps ratio of EMG RMS amplitudewill be calculated.
In a subset of the participants, the collection of EMG signals will betriggered and synchronized using an OptiTrack™ 6 camera 120 Hz system,with Tracking Tools™ computer software (NaturalPoint, Inc, OR, USA)which will collect kinematic data. Upper limb movement will be tracked viathe recording of reflective marker clusters placed on theparticipants’ upper arm, distal forearm, sternum, and acromion andacromioclavicular joints. Kinematic data for analysis will includedisplacement, velocity and changes in angles of upper arm segments andmarkers.
Secondary outcome measures: clinical
A range of clinical measures will be collected to measure the presence ofimpairments post stroke. To measure strength, lateral head of tricepsbrachii muscle power will be assessed using manual muscle testing accordingto MRC ratings from 0–5 [29]. To measure the active range of movement of finger flexion andextension, thumb extension and abduction, elbow flexion and extension andshoulder abduction and adduction, assessment according to the protocoldescribed by Uswatte et al. [30] will be performed. To measure the presence of spasticity ofbiceps brachii and resistance to passive elbow extension, the modifiedAshworth Scale [31] and Tardieu Scale [32] will be administered. To evaluate joint tenderness on passivemovement of the hemiplegic shoulder, the Ritchie Articular Index will beadministered [33, 34]. To describe participants at baseline only, the CognitiveLinguistic Quick Test [35] and Nottingham Sensory Assessment [36, 37] will be administered. Motor Assessment Scale items 7 (handmovements) and 8 (advanced hand activities) will be performed to monitor forany carryover improvement in hand function. To examine upper limb functionat the participation level, two self-report measures will be used. TheStroke Impact Scale will be used to measure the impact of the interventionon the stroke survivor’s recovery [38]. The Motor Activity Log will be administered to all subjects torate how well and how much they use the paretic limb spontaneously ineveryday tasks [30].
Data analysis
Data analysis will be performed on an intention-to-treat basis using an alphalevel of 0.05. Descriptive statistics will be used to ensure comparability ofscores between groups at baseline, to describe performance at each phase and totest whether the assumptions for use of parametric statistics have been met. Ifthe assumptions for F or t-tests are violated, equivalent non-parametricstatistics will be utilized. The main hypothesis will be tested using mixedeffects models, in a 3 group (SMART Arm + OT stim, SMART Arm alone, usualtherapy) × 4 phase (0, 4, 26, 52 weeks) model. This will be followed bybetween-groups planned comparisons. All secondary outcomes will be analysed in asimilar manner.
Sample size
The principle endpoint is post intervention (4 weeks). Our previous RCTdemonstrated that stroke survivors using the SMART Arm alone or with electricalstimulation demonstrated significant improvements in MAS-6 scores compared tothe control group [16]. On this basis, we estimate a mean improvement of 1.8 (SD 2) in theusual therapy group, 2.91 (SD 2) in the SMART Arm alone group and 3.91 (SD 2) inthe SMART Arm with OT-stim group. To achieve 80% power and a significance of0.05 with pairwise comparisons, 22 subjects are required per group, to total 66subjects. A 15% dropout rate will be allowed to account for withdrawals, thus 25subjects will be recruited per group, totalling 75.
Ethics approval
The study protocol has been approved by the University of Queensland MedicalResearch Ethics Committee (MREC ID: 2007001628), and the Princess AlexandraHospital Ethics Committee (ID: 2008–046). This study will be conducted inaccordance with the Declaration of Helsinki.
Discussion
This will be the first prospective trial to compare the effect of dose-matchedvolumes of SMART Arm with OT-stim and usual therapy, versus SMART Arm alone withusual therapy versus usual therapy alone during inpatient rehabilitation followingstroke. While it is known that intensive and repetitive, task-oriented training iscritical to drive motor recovery after stroke [39, 40], those with severe impairment and ‘not enough movement to workwith’ require assistance to complete a functional movement pattern. Currently,the most commonly used method is manual assistance by a therapist. The minimal timespent on the upper limb during physiotherapy indicates however, that thistime-inefficient strategy is not prioritised. It is likely that gait trainingrequirements, which are paramount to determining discharge destination, areprioritised. Another option is robotic therapy, however availability is currentlylimited and functional outcomes remain inconclusive [8, 41, 42].
In the event that SMART Arm training, with or without electrical stimulation, leadsto demonstratable significant improvements in upper limb function, reducedimpairments or increased participation, an alternative option for retraining wouldbe presented. Improvements in impairments and activity using the SMART Arm have beenobtained in chronic stroke survivors [16], and the indications from our pilot work are that similar outcomes may beachieved in those undertaking inpatient rehabilitation [19]. If positive changes may be induced during inpatient rehabilitation, thismay allow some stroke survivors to regain levels of function that are sufficient toenable progression to interventions such as constraint induced movement therapy.
This study will also allow the impact of augmenting training with electricalstimulation to be assessed in the context of severe motor disability. This will bethe first large study to determine the effect of outcome-triggered stimulation, incircumstances in which the stroke survivor is rewarded for performing thedesired movement, rather than for simply generating sufficient levels of EMG i.e.regardless of the functional consequences.
Findings from this study will provide insights into the effects of practice onregaining motor skill in those with severe upper limb disability following stroke.The collection of detailed training data will generate new knowledge regarding theimportance of specific training elements, such as load and feedback on performancein the early phase of rehabilitation. These will have implications that extendbeyond the current modes of training investigated and possibly to other populationssuch as those with other forms of brain injury.
Consent
Written informed consent was obtained from the patient for publication of the image(Figure 1). A copy of the written consent isavailable for review by the Editor of this journal.
Abbreviations
- ANCOVA:
-
Analysis of covariance
- EMG:
-
Electromyography
- MAS:
-
Motor assessment scale
- RCT:
-
Randomised controlled trial
- RMS:
-
Root mean square
- SENIAM:
-
Surfaceelectromyography for the non-invasive assessment of muscles
- SPSS:
-
Statisticalprocesses for the social sciences.
References
Gowland C: Recovery of motor function following stroke: Profile and prediction. Physiother Canada. 1982, 34: 77-84. 10.3138/ptc.34.2.077.
Kwakkel G, Kollen BJ, Van der Grond J, Prevo AJ: Probability of regaining dexterity in the flaccid upper limb. The impact ofseverity of paresis and time since onset in acute stroke. Stroke. 2003, 34: 2181-2186. 10.1161/01.STR.0000087172.16305.CD.
Nakayama H, Jorgensen HS, Rasschou HO, Olsen TS: Recovery of upper extremity function in stroke patients: The CopenhagenStroke Study. Arch Phys Med Rehabil. 1994, 75: 394-398. 10.1016/0003-9993(94)90161-9.
National Stroke Foundation: Clinical guidelines for stroke management. 2010, Melbourne, Australia, ISSBN0-978-0-9805933-3-4
Peppen RPS van, Kwakkel G, Harmeling-van-der Wel BC, Kollen BJ, Hobbelen JSM, Buurke JH: KNGF Clinical Practice Guidelines for physical therapy in patients withstroke: Review of the evidence. Dutch J Phys Ther. 2004, 114 (Suppl 5):
Lindsay MP, Gubitz G, Bayley M, Davies-Schinkel C, Singh S, Phillips S: Canadian best practice recommendations for stroke care (Update 2010). Onbehalf of the Canadian Stroke Strategy Best Practice and Standards WritingGroup. 2010, Ottawa, Ontario Canada: Canadian Stroke Network,
Chae J, Yu D: A critical review of neuromuscular stimulation for treatment of motordysfunction in hemiplegia. Assist Tech. 2000, 12: 33-49. 10.1080/10400435.2000.10132008.
Hayward KS, Barker RN, Brauer SG: Interventions to promote upper limb recovery in stroke survivors with severeparesis: A systematic review. Disabil Rehabil. 2010, 32: 1973-1986. 10.3109/09638288.2010.481027.
Barker RN, Brauer SG: Recovery of the upper limb after stroke: The stroke survivors'perspective. Disabil Rehabil. 2005, 27 (20): 1213-1223. 10.1080/09638280500075717.
Goldie P, Matyas T, Kinsella G: In Research report to the Department of Health Housing and CommunityServices. Movement rehabilitation following stroke. 1992, Victoria,
Mackey F, Ada L, Heard RC, Adams R: Stroke rehabilitation:are highly structured units more conducive to physicalactivity than less structured units?. Arch Phys Med Rehabil. 1996, 77: 1066-1070. 10.1016/S0003-9993(96)90070-2.
Ada L, Mackey F, Heard R, Adams RJ: Stroke rehabilitation: Does the therapy area provide a physicalchallenge?. Aust J Physiother. 1999, 45: 33-38.
Bernhardt J, Chan J, Nicola I, Collier JM: Little therapy, little physical activity: Rehabilitation within the first 14days of organized stroke unit care. J Rehabil Med. 2007, 39: 43-48. 10.2340/16501977-0013.
Goldie P, Matyas T, Kinsella G: Movement rehabilitation following stroke. 1992, Victoria: Department of Health, Housing and CommunityServices,
Kuys SS, Brauer SG, Ada L: Routine physiotherapy does not induce a cardiorespiratory training effectpost-stroke, regardless of walking ability. Physiother Res Int. 2006, 11: 219-227. 10.1002/pri.344.
Barker RN, Brauer SG, Carson RG: Training of reaching in stroke survivors with severe and chronic upper limbparesis: A randomised clinical trial. Stroke. 2008, 39: 1800-1807. 10.1161/STROKEAHA.107.498485.
Barker RN, Brauer SG, Carson RG: Training-induced changes in the pattern of triceps to biceps activationduring reaching tasks after chronic and severe stroke. Exp Brain Res. 2009, 196: 483-496. 10.1007/s00221-009-1872-8.
Barker RN, Brauer SG, Barry BK, Gill TJ, Carson RG: Training-induced modifications of corticospinal reactivity in severelyaffected stroke survivors. Exp Brain Res. 2012, 221: 211-221. 10.1007/s00221-012-3163-z.
Hayward KS, Barker RN, Lloyd D, Brauer SG, Horsley SA, Carson RG: SMART Arm with outcome-triggered electrical stimulation: A pilot RCT. Top Stroke Rehabil. In press
Turton A, Pomeroy V: When should upper limb function be trained after stroke? Evidence for andagainst early intervention. Neurorehabil. 2002, 17: 215-224.
Rodgers H, Mackintosh J, Price C, Wood R, McNamee P, Fearon T, Marritt A, Curless R: Does an early increased-intensity interdisciplinary upper limb therapyprogram following acute stroke improve outcome?. Clin Rehabil. 2003, 17: 579-589. 10.1191/0269215503cr652oa.
Michaelsen SM, Dannenbaum R, Levin MF: Task-specific training with trunk restraint on arm recovery in stroke:Randomised controlled trial. Stroke. 2006, 37: 186-192.
Woodbury ML, Howland DR, McGuirk TE, Davis SB, Senesac CR, Kautz S, Richards LG: Effects of trunk restraint combined with intensive task practice onpoststroke upper extremity reach and function: A pilot study. Neurorehabil Neural Repair. 2009, 23: 78-91.
Cirstea MC, Levin M: Compensatory strategies for reaching in stroke. Brain. 2000, 123: 940-953. 10.1093/brain/123.5.940.
Santello M, Flanders M, Soechting JF: Patterns of hand motion during grasping and the influence of sensoryguidance. J Neurosci. 2002, 22: 1426-1435.
World Health Organisation: International Classification of Functioning, Disability and Health. 2001, Geneva: World Health Organisation
Malouin F, Pichard L, Bonneau C, Durand A, Corriveau D: Evaluating motor recovery early after stroke: Comparison of Fugl-Meyerassessment and the Motor Assessment Scale. Arch Phys Med Rehabil. 1994, 75: 1206-1212. 10.1016/0003-9993(94)90006-X.
Hermens HJ, Freriks B, Disselhorst-Klug C, Rau G: Development of recommendations for SEMG sensors and sensor placementprocedures. J Electromyogr Kinesiol. 2000, 10: 361-374. 10.1016/S1050-6411(00)00027-4.
Kendall FP, Kendall EM, Provance PG: Muscle testing and function. 1993, Baltimore: Williams and Wilkins, 4
Uswatte G, Taub E, Morris D, Light K, Thompson PA: The Motor Activity Log-28: Assessing daily use of the hemiparetic arm afterstroke. Neurology. 2006, 67: 1189-1194. 10.1212/01.wnl.0000238164.90657.c2.
Bohannon RW, Smith MB: Inter-rater reliability of a modified Ashworth scale of muscle spasticity. Phys Ther. 1987, 67: 206-207.
Mackey AH, Walt SE, Lobb G, Stott NS: Intra-observer reliability of the modified Tardieu scale in the upper limb ofchildren with hemiplegia. Dev Med Child Neurol. 2004, 46: 267-272.
Bohannon RW, Andrews AW: Shoulder subluxation and pain in stroke survivors. Am J Occ Ther. 1990, 44: 507-509. 10.5014/ajot.44.6.507.
Gustafsson L, McKenna K: Correlation between two measurement scale of hemiplegic shoulder pain. Int J Ther Rehabil. 2003, 10: 247-252.
Helm Estabrooks N: Cognitive Linguistic Quick Test. 2001, San Antonion, TX: Psych Corp
Cambier DC, De Corte E, Danneels LA, Witvrouw EE: Treating sensory impairments in post-stroke upper limb with intermittentpneumatic compression. Results of a preliminary trial. Clin Rehabil. 2003, 17: 14-20. 10.1191/0269215503cr580oa.
Lincoln NB, Parry RH, Vass CD: Randomised, controlled trial to evaluate increased intensity of physiotherapytreatment of arm function after stroke. Stroke. 1999, 30: 573-579. 10.1161/01.STR.30.3.573.
Duncan PW, Wallace D, Min Lai S, Johnson D, Embretson S, Lacobs Laster L: The stroke impact scale version 2.0: Evaluation of reliability, validity andsensitivity to change. Stroke. 1999, 30: 2131-2140. 10.1161/01.STR.30.10.2131.
Hubbard IJ, Parsons MW, Neilson C, Carey LM: Task-specific training: evidence for and translation into clinicalpractice. Occ Ther Int. 2009, 16: 175-189. 10.1002/oti.275.
Timmermans AAA, Spooren AIF, Kingma H, Seelen HAM: Influence of task-oriented training content on skilled arm-hand performancein stroke: A systematic review. Neurorehabil Neural Repair. 2010, 24: 858-870. 10.1177/1545968310368963.
Kwakkel G, Kollen BJ, Krebs HI: Effects of robotic-assisted therapy on upper limb recovery after stroke: Asystematic review. Neurorehabil Neural Repair. 2008, 22: 111-121.
Mehrholz J, Hadrich A, Platz T, Kugler J, Pohl M: Electromechanical and robot-assisted arm training for improving genericactivities of daily living, arm function and arm muscle strength afterstroke. Cochrane Database Syst Rev. 2012, 13 (6): CD006876-
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2377/13/71/prepub
Acknowledgements
This study has been funded by a National Health & Medical Research CouncilProject Grant (ID: 511241). The authors thank the staff at the PrincessAlexandra Hospital and the QEII Hospital. We also thank Dr Stephen Wilson, DrDavid Lloyd and Mr Russell Gee for their contribution to SMART Arm construction;Dr David Lloyd, Dr Craig Tokono, and Dr Christoph Szubski for their contributionto data collection equipment design and construction; and Dr Brenda Ocampo andMs Katrina Kemp for their contribution to project management.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
SG Brauer, KS Hayward, RN Barker and RG Carson are currently involved incommercialisation of the SMART Arm device.
Authors’ contributions
SB, RB, and RC conceived the idea for the study. SB, RB, RC and AC all contributed tothe research design and obtained funding for the study. SB, KH, RB, RC and ACcontributed to the design of the study, intervention and outcome measures. SB, KHand RB were involved in participant recruitment. SB and KH were principallyresponsible for the drafting of the manuscript. All authors assisted in editing thefinal submitted manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative CommonsAttribution License (http://creativecommons.org/licenses/by/2.0), whichpermits unrestricted use, distribution, and reproduction in any medium, provided theoriginal work is properly cited.
About this article
Cite this article
Brauer, S.G., Hayward, K.S., Carson, R.G. et al. The efficacy of SMART Arm training early after stroke for stroke survivors withsevere upper limb disability: a protocol for a randomised controlled trial. BMC Neurol 13, 71 (2013). https://doi.org/10.1186/1471-2377-13-71
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2377-13-71