Abstract
Aim
In order to avoid the complications associated with thromboembolic disease, patients with this condition typically are placed on long-term anticoagulant therapy. This report compares bleeding complications in this patient population by level of achieved INR.
Materials and Methods
During the 6-year period between January 1997 and January 2003, 386 patients with venous thromboembolism of the lower extremities were admitted to the Cardiovascular Surgery Outpatient Clinic of Alsancak State Hospital. Of the 386 patients, 198 (51.2%) were women, and the average age was 52.3 years. All diagnoses of venous thromboembolism were confirmed by means of Doppler ultrasonography. Further investigation showed occult neoplasms in 22 (5.6%) of the cases. We excluded the patients with occult disease, and the remaining 364 constituted our study population.
Results
Oral anticoagulation was standardized at 6 months' duration in all cases. We divided the patients into two groups. Group I consisted of 192 patients (52.7%) with INR values between 1.9 and 2.5; Group II comprised 172 patients with INR values between 2.6 and 3.5. Complications in each group were assessed and compared. The minor hemorrhage rate was 1.04% in Group I and 4.06% in Group II. The major hemorrhage rate was also 1.04% in Group I and was 6.3% in Group II. We determined that the complication rates for both minor and major hemorrhage were significant in patients with INR values above 2.5.
Conclusion
Oral anticoagulation must be followed closely in patients with venous thromboembolism. Higher INR levels are associated with significant increases in hemorrhage and associated complications. INR values of 2.0 to 2.5 are sufficient for long-term anticoagulant therapy, ensuring ideal anticoagulation levels and minimizing the complication rate.
Similar content being viewed by others
Background
Deep vein thrombosis (DVT) is the presence in lower-extremity veins of a thrombus that obstructs the branches and blood flow. The natural course of DVT therapy is associated with significant morbidity and mortality rates [1]. Standard therapy for acute DVT consists of heparin followed by oral warfarin [2]. To monitor therapy with coumadin anticoagulants, prothrombin time (PT) was the standard until as recently as the past decade [3]. Because the therapeutic range of PT depends on many factors, comparing patient results and assessing the significance of those results can be difficult. Therefore, the World Health Organization (WHO) developed an international standardization system known as the international normalized ratio (INR) [4].
We monitored anticoagulation therapy and compared bleeding complications among outpatients with lower-extremity DVTs who were taking oral anticoagulants (OACs) and who exhibited two different ranges of INR values.
Materials and Methods
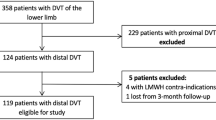
Between January, 1997 and January, 2003, 386 patients with a preliminary diagnosis of venous thromboembolism were admitted to the Cardiovascular Surgery Outpatient Clinic at Alsancak State Hospital. Of these patients, 198 (51.2%) were women and 188 (48.4%) were men. The average age of all patients was 52.3 years (range, 23–81 years). In all cases, the diagnosis of venous thromboembolism was confirmed by means of Doppler ultrasonography (USG). When admitted, no patients in the study group were known to have malignant disease as the etiologic factor of DVT. We excluded patients with superficial thrombophlebitis, thrombosis, and recurrent DVT. To investigate for tumors and establish the diagnoses, we used chest radiographs and laboratory tests (erythrocyte sedimentation rate, C-reactive protein, complete blood count, urea, creatinine, serum glutamic oxaloacetic transaminase [SGOT], serum glutamic pyruvic transaminase [SGPT], gamma glutamyl transferase [gamma GT], alkaline phosphatase [ALP], bilirubin, electrophoresis, total protein, alpha fetoprotein [α-FP], fibrinogen, cancer antigen 19-9 [CA-19-9], and in men prostate-specific antigen [PSA]). Abdominal ultrasonography was also used if indicated. We identified previously unrecognized neoplasms in 22 (5.6%) patients (Table 1). We referred these patients to oncology clinics and limited our study population to the remaining 364 patients. Of this group, 42 (11.5%) were hospitalized for an average of 5.2 days and received intravenous (IV) heparin plus oral anticoagulants. We combined low-molecular-weight heparin (LMWH) with oral anticoagulants for the other patients and followed them in our outpatient clinic. For long-term anticoagulation we used the same drug (coumadin) and monitored results as INR values.
Results
We standardized oral anticoagulant therapy for a 6-month period in all patients and followed them at our outpatient clinic with bleeding profile tests. We classified the patients according to INR values. The INR level was between 1.9 and 2.5 in Group I and between 2.6 and 3.5 in Group II. Group I comprised 192 (52.7%) patients; Group II consisted of 172 (47.3%) patients. During the 6-month control period, no mortality or major morbidity such as pulmonary embolus occurred in either group, and we found no recurrent DVT among the 343 (94.2%) patients during that period. In Group I, two patients (1.04%) experienced minor hermorrhagic complications (subconjunctival hemorrhage and epistaxis), and two patients (1.04%) had major hemorrhagic complications (gastrointestinal [GI] bleeding and hemarthrosis). In Group II, seven patients (4.06%) had minor hemorrhagic complications including skin necrosis in three, epistaxis in three, and subconjunctival hemorrhage in three. Eleven patients (6.3%) in Group II experienced major hemorrhagic complications including GI bleeding in six, vaginal bleeding in three, hemarthrosis in one, and gluteal hematoma in one (Table 2). We noted no instances of noncompliance and no major hematologic problems such as hemolysis during follow-up. Among six patients with GI bleeding, endoscopy demonstrated peptic ulcer disease in four (66.6%) and acute erosive gastritis in two (33.3%). In three patients with vaginal bleeding, two cases were due to myoma uteri and one was a result of chronic cervicitis. None of the hemorrhagic complications was secondary to malignancy in either Group I or Group II. The patients in Group II, whose INR values were between 2.6 and 3.5, had significantly more minor and major bleeding complications than did patients in Group I.
Discussion
In 1977, the Committee on Thrombosis and Hemostasis and the National Institute of Biological Standards and Control (NIBSC) in London prepared a thromboplastin material from human brain. This material was coded as "67/40" and was accepted as an international reference preparation by the WHO [5]. Because PT results are dependent upon a number of factors, rates and activity percentages with different thromboplastins may be inconsistent for an individual patient. The WHO introduced an international standardization system [6], and in 1983 the Expert Committee on Biological Standardization of the WHO accepted the international normalized ratio (INR) for PT standardization (Table 3).
Since 1983, INR values have been calculated based on randomized study results involving laboratory evaluation of OAC therapy. Based on these study findings, the optimal therapeutic range was narrowed. In 1989, a new guide was prepared by the American College of Chest Physicians. We are now using that guide [7].
Warfarin is the most frequently used OAC because of its perfect bioavailability and consistent effect in both acute and chronic disease [8]. Today, INR values are used at many institutions to evaluate OAC therapy (2,4,5,7,9). Anticoagulants are used in two different concentrations: low doses for INR values between 2.0 and 2.5 and high doses for INR values between 2.5 and 3.5. A low-dose regimen is used in the treatment of venous thrombosis or pulmonary embolus as well as prophylactically to prevent venous thrombosis. High-dose regimens are recommended for high-risk patients with mechanical prosthetic cardiac valves. Low doses have been shown to be safer than high doses and just as effective for following patients who undergo DVT therapy [3, 7, 9, 10].
In patients whose INR levels exceed 2.5, the incidence of hemorrhagic complications increases significantly [8, 9, 11]. An occult GI lesion accounted for 70% of the GI bleeds, and in 10%, bleeding during anticoagulant therapy was due to malignancy [4]. Even with ideal anticoagulant doses, GI and genitourinary bleeding are seen as a result of underlying disease [4, 12]. In our study, GI bleeding occurred in both groups, and vaginal bleeding occurred as a complication in Group II (Table 2).
Hasenkam and associates proposed an INR between 2.0 and 2.7, even for patients with valve replacements, to minimize the incidence of bleeding as a complication and the risk of thromboembolus [13].
Many studies address the effectiveness of LMWH in treating DVT, and this form of heparin therapy should be seriously considered. LMWH eliminates many problems related to the use of nonfractionated IV heparin [1, 8, 14]. Its bioavailability is high, and the once-daily subcutaneous injection regimen is sufficient because of its longer half-life. LMWH decreases major hemorrhagic complications and thrombocytopenia as well as the incidence of osteoporosis associated with heparin administration. The single LMWH injection without the necessity of monitoring anticoagulation offers a very attractive treatment method. DVT can be treated without hospitalization, and patients can return to daily activities and to work much more quickly [14, 15]. We used LMWH for 88.5% of our patients.
In conclusion, OAC therapy must be closely monitored during both acute and chronic periods. To compare and standardize results reported by different centers, values should be reported as INR. Bleeding and related complications increase as INR levels are increased. We suggest that, ideally, the anticoagulant dosage should be adjusted to achieve an INR between 2 and 2.5 in patients with DVT. This dose level minimizes complications and is sufficient to control anticoagulant therapy.
References
Oger E, EPI-GETBP Study Group: Incidence of venous thromboembolism: A community-based study in Western France. Thromb Haemost. 2000, 83: 657-60.
Kearon C: Duration of therapy for acute venous thromboembolism. Clin Chest Med. 2003, 24 (1): 63-72. 10.1016/S0272-5231(02)00076-X. Review
Hirsh J, Fuster V: Guide to anticoagulant therapy. Part 2. Oral anticoagulants. Circulation. 1994, 89: 1469-1480.
Karabay Ö, Sarýosmanoğlu N, Çatalyürek H, Hazan E, Açýkel Ü, Oto Ö: Anticoagulation With Different INR Level On The Effect Of Postoperative Bileaflet Mitral Prosthesis Valve Cases. Journal of Turkish Thoracic and Cardiovascular Surgery. 1997, 5: 311-4.
International Committee for standardization in Haematology, International Committee on Thrombosis and Haemostasis: ICSH / ICTH reommendations for reporting prothrombin time in oral anticoagulant control. Thromb Haemost. 1985, 53: 155-6.
Ridker PM, Goldhaber SZ, Danielson E, et al: Long-term, low-intensity warfarin therapy for the prevention of recurrent venous thromboembolism. N Engl J Med. 2003, 348 (15): 1425-34. 10.1056/NEJMoa035029.
Litin SC, Gastineau DA: Current concepts in anticoagulant therapy. Mayo Clin Proc. 1995, 70 (3): 266-72. Review
Tufano A, Cerbone AM, Di Minno G: The use of antithrombotic drugs in older people. Minerva Med. 2002, 93 (1): 13-26.
Rosenbaum CC, Woods SE, Hasselfeld KA: Correlation of the change in the International Normalized Ratio and decreasing the Coumadin dosage following total joint arthroplasty. Orthopedics. 2002, 25 (12): 1359-63.
Ageno W, Steidl L, Ultori C, et al: The initial phase of oral anticoagulation with warfarin in outpatients with deep venous thrombosis. Blood Coagul Fibrinolysis. 2003, 14 (1): 11-4. 10.1097/00001721-200301000-00003.
Caprini JA, Arcelus JI, Reyna JJ, et al: Deep vein thrombosis outcome and the level of oral anticoagulation therapy. J Vasc Surg. 1999, 30 (5): 805-11.
Levesque H: Risk of hemorrhage with oral anticoagulants for deep vein thrombosis. J Mal Vasc. 2002, 27 (3): 129-36. Review
Hasenkam JM, Kimose HH, Knudsen L, et al: Self management of oral anticoagulant therapy after heart valve replacement. Eur J Cardiothorac Surg. 1997, 11: 935-42. 10.1016/S1010-7940(97)01204-9.
Lindmarker P, Holmström M, Granqvist S, et al: Comparison of once-daily subcutaneous Fragmin with continuous intravenous unfractionated heparin in the treatment of deep vein thrombosis. Thromb Haemost. 1994, 72: 186-90.
Mannucci PM, Poller L: Venous thrombosis and anticoagulant therapy. Br J Haematol. 2001, 114 (2): 258-70. 10.1046/j.1365-2141.2001.02961.x. Review
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Yetkin, U., Karabay, Ö. & Önol, H. Effects of oral anticoagulation with various INR levels in deep vein thrombosis cases. Trials 5, 1 (2004). https://doi.org/10.1186/1468-6708-5-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1468-6708-5-1