Key summary points
The aim was to examine the predictive value of the record-based MPI in terms of mortality, readmission and LOS.
AbstractSection FindingsThe record-based MPI assessed at discharge predicted mortality and readmission risk in medical inpatients aged ≥ 75 years. Higher MPI risk scores were also associated with longer hospital stay, higher age and female sex.
AbstractSection MessageThe record-based MPI is valuable in predicting mortality and other frailty-related, negative health outcomes in older medical inpatients, and the method is applicable as an alternative to bedside MPI in older hospitalized medical patients.
Abstract
Purpose
To examine the predictive value of the record-based Multidimensional Prognostic Index (MPI) on mortality, readmission and length of hospital stay (LOS) among older medical inpatients.
Methods
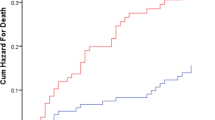
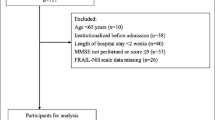
A cohort of medical inpatients aged ≥ 75 years was rated using the record-based MPI to assess frailty retrospectively. 90-day and 1-year mortality hazard ratios (HRs) were calculated in a sex- and age-adjusted Cox proportional hazards model. 30-day readmission relative risk (RR) estimates were calculated in a binary regression model with mortality as a competing risk. Discrimination was expressed by the area under the receiver operating characteristic (ROC) curve. Median LOS was calculated using the non-parametric Kruskal–Wallis one-way ANOVA.
Results
In total, 1190 patients with a median age of 83 years were included. 50% were male. 335 patients (28%) were categorized as non-frail (MPI score 0.0–0.33), 522 (44%) moderately frail (MPI score 0.34–0.66) and 333 (28%) severely frail (MPI score 0.67–1.0). 90-day mortality HR was 7.4 (95% confidence interval (CI) 2.9–18.6, p < 0.001) for the moderately frail and 18.5 (95% CI 7.5–46.1, p < 0.001) for the severely frail compared with the non-frail. ROC area was 0.76 (95% CI 0.72–0.80). Similarly, 1-year mortality HR was 3.3 (95% CI 2.2–5.0, p < 0.001) for the moderately frail and 7.1 (95% CI 4.7–10.6, p < 0.001) for the severely frail. 30-day readmission RR was 2.1 (95% CI 1.5–2.9, p < 0.001) for the moderately frail and 1.8 (95% CI 1.3–2.6, p = 0.001) for the severely frail. LOS was significantly longer with increasing MPI score (p < 0.001).
Conclusion
The record-based MPI assessed at discharge predicts dose-dependent post-discharge mortality and readmission risk and is associated with LOS in older medical inpatients.



Similar content being viewed by others
Availability of data and material
Anonymized data are available on request. To maintain confidentiality, the medical record material is not available. The study protocol (in Danish) is available on request.
Code availability
Stata code is available on request.
References
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K (2013) Frailty in elderly people. Lancet 381(9868):752–762
Kahlon S, Pederson J, Majumdar SR, Belga S, Lau D, Fradette M et al (2015) Association between frailty and 30-day outcomes after discharge from hospital. Can Med Assoc J 187(11):799–804
Stillman GR, Stillman AN, Beecher MS (2019) Frailty is associated with early hospital readmission in older medical patients. J Appl Gerontol. https://doi.org/10.1177/0733464819894926
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J et al (2001) Frailty in older adults: evidence for a phenotype. J Gerontol Ser A Biol Sci Med Sci 56(3):M146–M156
Ellis G, Gardner M, Tsiachristas A, Langhorne P, Burke O, Harwood RH et al (2017) Comprehensive geriatric assessment for older adults admitted to hospital. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD006211.pub3
Parker SG, McCue P, Phelps K, McCleod A, Arora S, Nockels K et al (2018) What is comprehensive geriatric assessment (CGA)? An umbrella review. Age Ageing 47(1):149–155
Pilotto A, Ferrucci L, Franceschi M, D’Ambrosio LP, Scarcelli C, Cascavilla L et al (2008) Development and validation of a multidimensional prognostic index for 1-year mortality from comprehensive geriatric assessment in hospitalized older patients. Rejuvenation Res 11:151–161
Angleman SB, Santoni G, Pilotto A, Fratiglioni L, Welmer AK (2015) Multidimensional prognostic index in association with future mortality and number of hospital days in a population-based sample of older adults: results of the EU Funded MPI-AGE project. PLoS ONE 10(7):89. https://doi.org/10.1371/journal.pone.0133789
Cruz-Jentoft AJ, Daragjati J, Fratiglioni L, Maggi S, Mangoni AA, Mattace-Raso F et al (2020) Using the Multidimensional Prognostic Index (MPI) to improve cost-effectiveness of interventions in multimorbid frail older persons: results and final recommendations from the MPI_AGE European Project. Aging Clin Exp Res 32(5):861–868
Gregersen M, Hansen TK, Jørgensen BB, Damsgaard EM (2020) Frailty is associated with hospital readmission in geriatric patients: a prognostic study. Eur Geriatr Med. https://doi.org/10.1007/s41999-020-00335-w
Meyer AM, Becker I, Siri G, Brinkkötter PT, Benzing T, Pilotto A et al (2019) New associations of the Multidimensional Prognostic Index. Zeitschrift Gerontol Geriatr 52(5):460–467
Pata G, Bianchetti L, Rota M, Marengoni A, Chiesa D, Cassinotti E et al (2020) Multidimensional Prognostic Index (MPI) score has the major impact on outcome prediction in elderly surgical patients with colorectal cancer: the FRAGIS study. J Surg Oncol. https://doi.org/10.1002/jso.26314
Pilotto A, Rengo F, Marchionni N, Sancarlo D, Fontana A, Panza F et al (2012) Comparing the prognostic accuracy for all-cause mortality of frailty instruments: a multicentre 1-year follow-up in hospitalized older patients. PLoS ONE 7:1–9
Pilotto A, Sancarlo D, Pellegrini F, Rengo F, Marchionni N, Volpato S et al (2016) The Multidimensional Prognostic Index predicts in-hospital length of stay in older patients: a multicentre prospective study. Age Ageing 45(1):90–96
Pilotto A, Veronese N, Daragjati J, Cruz-Jentoft A, Polidori MC, Mattace-Raso F et al (2019) Using the Multidimensional Prognostic Index to predict clinical outcomes of hospitalized older persons: a prospective, multicenter, international study. J Gerontol Ser A Biol Sci Med Sci 74:1643–1649
Volpato S, Bazzano S, Fontana A, Ferrucci L, Pilotto A (2015) Multidimensional Prognostic Index predicts mortality and length of stay during hospitalization in the older patients: a multicenter prospective study. J Gerontol Ser A Biol Sci Med Sci 70:325–331
Dent E, Kowal P, Hoogendijk EO (2016) Frailty measurement in research and clinical practice: a review. Eur J Intern Med 31:3–10
Warnier RMJ, van Rossum E, van Velthuijsen E, Mulder WJ, Schols JMGA, Kempen GIJM (2016) Validity, reliability and feasibility of tools to identify frail older patients in inpatient hospital care: a systematic review. J Nutr Health Aging 20:218–230
Cella A, Ferrari A, Rengo G, Solfrizzi V, Veronese N, Puntoni M et al (2020) Agreement of a Short Form of the Self-Administered Multidimensional Prognostic Index (SELFY-MPI-SF): a useful tool for the self-assessment of frailty in community-dwelling older people. Clin Interv Aging 15:493–499
Pilotto A, Custodero C, Maggi S, Polidori MC, Veronese N, Ferrucci L (2020) A multidimensional approach to frailty in older people. Ageing Res Rev 60:98. https://doi.org/10.1016/j.arr.2020.101047
Pilotto A, Veronese N, Guerrero KLQ, Zora S, Boone ALD, Puntoni M et al (2019) Development and validation of a self-administered Multidimensional Prognostic Index to predict negative health outcomes in community-dwelling persons. Rejuvenation Res 22:299–305
Hansen TK, Damsgaard EM, Shahla S, Bruun JM, Gregersen M (2020) A reliable and record-based frailty assessment method for older medical inpatients. Eur Geriatr Med. https://doi.org/10.1007/s41999-020-00345-8
Zuckerman JD, Koval KJ, Aharonoff GB, Skovron ML (2000) A functional recovery score for elderly hip fracture patients: II. Validity and reliability. J Orthop Trauma 14:26–30
Pfeiffer E (1975) A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc 23(10):433–441
Bliss MR, McLaren R, Exton-Smith AN (1966) Mattresses for preventing pressure sores in geriatric patients. Mon Bull Ministry Health Public Health Lab Serv 25:238–268
Miller MD, Towers A (1991) A manual of guidelines for scoring the Cumulative Illness Rating Scale for Geriatrics (CIRS-G). p 31
Sancarlo D, D’Onofrio G, Franceschi M, Scarcelli C, Niro V, Addante F et al (2011) Validation of a modified-multidimensional prognostic index (m-MPI) including the mini nutritional assessment short-form (MNA-SF) for the prediction of 1-year mortality in hospitalized elderly patients. J Nutr Health Aging 15:169–173
Statistikbanken (2019) Statistics Denmark. https://www.statistikbanken.dk/FOLK1A. Accessed 19 June 2020
Charlson ME, Pompei P, Ales KA, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L et al (2019) The REDCap consortium: building an international community of software platform partners. J Biomed Inform 95:103208. https://doi.org/10.1016/j.jbi.2019.103208
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42(2):377–381
Sundhedsstyrelsen MMT (2009) Genindlæggelser af ældre i Danmark 2008. København 2009
Collins GS, Ogundimu EO, Altman DG (2016) Sample size considerations for the external validation of a multivariable prognostic model: a resampling study. Stat Med 35(2):214–226
Pedersen LH, Gregersen M, Barat I, Damsgaard EM (2017) Early geriatric follow-up after discharge reduces mortality among patients living in their own home. A randomised controlled trial. Eur Geriatr Med 8(4):330–336
StataCorp (2019) Stata Statistical Software. Release 16. College Station, StataCorp LCC
WHO (2010) International Statistical Classification of Diseases and Related Health Problems 10th Revision. World Health Organization. https://icd.who.int/browse10/2010/en. Accessed 17 Aug 2020
Gilbert T, Neuburger J, Kraindler J, Keeble E, Smith P, Ariti C et al (2018) Development and validation of a Hospital Frailty Risk Score focusing on older people in acute care settings using electronic hospital records: an observational study. Lancet 391:1775–1782
Clegg A, Bates C, Young J, Ryan R, Nichols L, Ann Teale E et al (2016) Development and validation of an electronic frailty index using routine primary care electronic health record data. Age Ageing 45:353–360
Clegg A, Bates C, Young J, Ryan R, Nichols L, Teale E et al (2017) Development, internal validation and independent external validation of an electronic frailty index using routine primary care electronic health record data. Age Ageing 46:i35. https://doi.org/10.1093/ageing/afx068.129
Heggestad T, Lilleeng SE (2003) Measuring readmissions: focus on the time factor. Int J Qual Health Care 15(2):147–154
Andreasen J, Aadahl M, Sørensen EE, Eriksen HH, Lund H, Overvad K (2018) Associations and predictions of readmission or death in acutely admitted older medical patients using self-reported frailty and functional measures. A Danish cohort study. Arch Gerontol Geriatr 76:65–72
Artetxe A, Beristain A, Graña M (2018) Predictive models for hospital readmission risk: a systematic review of methods. Comput Methods Progr Biomed 164:49–64
Kansagara D, Englander H, Salanitro A, Kagen D, Theobald C, Freeman M et al (2011) Risk prediction models for hospital readmission: a systematic review. J Am Med Assoc 306(15):1688–1698
Wou F, Gladman JR, Bradshaw L, Franklin M, Edmans J, Conroy SP (2013) The predictive properties of frailty-rating scales in the acute medical unit. Age Ageing 42(6):776–781
Veronese N, Siri G, Cella A, Daragjati J, Cruz-Jentoft AJ, Polidori MC et al (2019) Older women are frailer, but less often die than men: a prospective study of older hospitalized people. Maturitas 128:81–86
Acknowledgements
We would like to thank the multidisciplinary staff in the MD, ED and the four municipalities for their meticulous medical record-keeping and intersectoral cooperation.
Funding
This work was part of a PhD project supported by A.P. Møller Fonden (DKK 45,000), Helsefonden (DKK 350,000) and the Health Research Fund of Central Denmark Region (DKK 100,000).
Author information
Authors and Affiliations
Contributions
The authors fulfil the ICMJE criteria for authorship. Study concept and design: Troels Kjærskov. Hansen (TKH), Seham Shahla (SS), Else Marie Damsgaard (EMD), Sofie Ran Lindhardt Bossen (SRLB), Jens Meldgaard Bruun (JMB), Merete Gregersen (MG); Acquisition of data: TKH, SRLB; Analysis and interpretation of data: TKH, SS, EMD, SRLB, JMB, MG.
Corresponding author
Ethics declarations
Conflict of interest
The authors had no conflicts of interest.
Ethics approval
The project was approved as a quality development project by the Regional Research Ethics Committee (197/2017) and the local hospital administration; hence, no further approval or consent was needed.
Informed consent
No patient received less than usual care, any extra treatment, examination or exposure because of the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
See Fig. 4.
Box-and-whiskers plots showing median LOS as function of MPI risk grade 1, 2 and 3 (left) and the aggregated MPI score (right). The overall median LOS was 3 days. LOS was not significantly affected by sex (p = 0.73). The Kruskal–Wallis hypothesis test showed significantly longer LOS in older patients (p = 0.037), with increasing MPI risk grades (p < 0.001), also when the analysis was based on the MPI score (p < 0.001). MPI Multidimensional Prognostic Index, LOS length of hospital stays. The plots show the mean values (line in box), interquartile ranges (box), and upper and lower values within 1.5 times the interquartile ranges (whiskers), as well as outliers beyond the whiskers (circles). Four outliers had a LOS > 30 days (located outside the plotted area); their LOS were 95 days (MPI = 2); 41 days (MPI = 2); 37 days (MPI = 3) and 34 days (MPI = 3). Only three patients had a MPI score = 1
Rights and permissions
About this article
Cite this article
Hansen, T.K., Shahla, S., Damsgaard, E.M. et al. Mortality and readmission risk can be predicted by the record-based Multidimensional Prognostic Index: a cohort study of medical inpatients older than 75 years. Eur Geriatr Med 12, 253–261 (2021). https://doi.org/10.1007/s41999-021-00453-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-021-00453-z