Abstract
Background
A majority of older adults in the United States (US) use prescription medications. Comprehensive population-level approaches to examine medication safety, effectiveness, and costs among older adults are needed.
Objectives
The objectives of this study were to develop a framework of quality measures spanning the domains of safety, effectiveness, and efficiency of prescription medication use among older adults, and to apply those measures using pharmacy claims data.
Methods
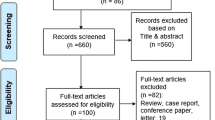
We performed a retrospective study among adults age 65 years and older of a US East Coast state who filled at least one prescription from a particular pharmacy chain during 2016 (N = 99,056). Firstly, we performed an environmental scan to identify quality measures and potentially relevant measures addressing prescription medication use. These measures were reviewed and rated by local geriatric pharmacotherapy experts. After evaluating feasibility, evidence, and relevance, a total of 19 measures representing the domains of safety (n = 7), effectiveness (n = 7), and efficiency (n = 5) were identified. These measures were then applied to an older adult population using prescription data for the year 2016 provided by a national pharmacy chain. All measures were configured such that a score of 100% corresponded to optimal performance.
Results
For the domain of safety, 12.8% of patients received a benzodiazepine chronically, 23.6% received central nervous system depressants, 16.7% received fluoroquinolones as first-line antibiotic therapy, and 21.9% of those who were prescribed opioids received them in excessive quantities. For the domain of effectiveness, one-fourth of the diabetes patients did not receive statins and angiotensin-acting medications, while 18.0% were not adherent to oral anticoagulant medications and 54% were not adherent to respiratory inhalers. For the domain of efficiency, 12.0% of the patients received prescriptions from five or more unique prescribers. Overall, 85.7%, 76.1%, and 87.9% of the older adults showed safe, effective, and efficient prescription medication use, respectively.
Conclusion
A novel approach to comprehensively examine the quality of medication use among older adults using prescription claims data is provided in our study. A considerable proportion of the older adults in our study received safe, effective, and efficient prescription medications. However, within each domain, several opportunities for improving the alignment of prescription medication use with current recommendations were identified.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
A novel approach/measurement framework to comprehensively assess safe, effective, and efficient prescription medication use among older adults using pharmacy claims data is presented. |
Overall, 14%, 24%, and 12% of older adults did not show safe, effective, and efficient prescription medication use, respectively. |
Many opportunities for quality improvement within the domains of safety, effectiveness, and efficiency of prescription medication use among older adults were identified. |
1 Introduction
Most older adults in the United States (US) utilize prescription medication, and approximately 40% are prescribed five or more medications [1]. While medication is intended to extend life or improve quality of life, its adverse effects can increase morbidity and mortality [2]. Conversely, optimal health outcomes are unrealized when patients fail to receive or to adhere to their medications. Additionally, medication cost is an increasing concern confronting patients and the health system. Comprehensive population-level approaches to assess and improve medication safety, effectiveness, and efficiency among older adults are needed, particularly in the US, where care fragmentation and lack of effective care coordination can lead to medication misuse and underuse.
Performance measurement is integral to quality improvement. Measures addressing medication use among older adults have been developed by several entities. Foremost, the Pharmacy Quality Alliance (PQA) has developed a range of quality measures of prescription medication utilization, including measures addressing medication safety and patient adherence [3]. The US Medicare program provides a privately administered prescription drug benefit, and has developed a star rating system for evaluating quality among drug plan sponsors, using a scheme that includes several of the PQA’s measures. Other prominent efforts to evaluate the quality of medication use among older adults include the Assessing Care of Vulnerable Elders (ACOVE) initiative [4, 5] and the Beers criteria [6]. The ACOVE measures assess the quality of medication use across 22 health conditions [4, 5]. The Beers criteria for potentially inappropriate medication use in older adults identifies higher-risk medications that should generally be avoided overall, or avoided or dose adjusted among particular patients [6]. Other notable efforts include the Medication Appropriateness Index (MAI) [7] and the START/STOPP criteria [8].
There are shortcomings to performance measurement. It is challenging to scale patient-level approaches to screen populations, particularly those that rely upon reviews of medication lists or patient interviews. For measures that utilize administrative claims data, calculating measure rates often requires the integration of pharmacy and medical databases, and can involve complex measure specifications. Moreover, given the breadth of medication use across the myriad health conditions that are prevalent among older adults, it is unlikely that any sole measure will have a dramatic impact on population health outcomes.
We envisioned a quality measurement framework addressing medication use among older adults, aligned with the core domains for health technology assessment of safety, effectiveness, and cost (efficiency), comprised of measures that can be calculated using pharmacy data solely. While pharmacy claims data lack information about medical diagnoses and procedures, there are many health conditions that can be identified with acceptable specificity according to the medication prescribed. We sought an approach that would simplify the complexity associated with analysis of integrated medical, hospital, pharmacy and eligibility data common to many performance measures. We sought to identify or develop quality measures of medication use among older adults derived from pharmacy claims, and to apply these measures to determine their suitability for population-level analyses. This study presents our S–E–E (Safety–Effectiveness–Efficiency) measurement framework and describes its application using pharmacy data for a population of older adults.
2 Methods
The first phase of the two-phase study was to identify or develop measures relevant to our purpose; the second phase involved applying these measures to calculate results, overall and according to patient characteristics.
The process of identifying suitable quality measures involved a targeted search of the published literature, identifying measures currently used with the US healthcare system, and brainstorming ideas for new measures with geriatric pharmacotherapy experts from our institution. A targeted literature review was performed by querying PubMed using the search terms “Beers,” “ACOVE,” and “START/STOPP,” as informed by the authors’ prior awareness of these efforts. This search yielded reviews of these quality measurement initiatives and other efforts described in their reference lists that were then examined for their relevance to older adults and applicability to pharmacy claims data. We also reviewed extant measures cataloged in the National Quality Measures Clearinghouse, developed by the US Agency for Healthcare Research and Quality (AHRQ). Additional candidate measures were brainstormed by the research team, drawing from their experience in pharmacoepidemiologic research (e.g., awareness of relevant US Food and Drug Administration alerts and clinical practice guidelines). Our measure review was limited to US sources. The candidate measures identified through these steps were then reviewed by three clinical geriatric pharmacotherapy experts who rated the dimensions of each candidate measure as “Yes,” “No,” or “Uncertain” according to (1) feasibility of adaptation to pharmacy claims data, (2) whether the measure was evidence-based, and (3) whether the measure was applicable to older adults. From the 42 candidate measures identified, 19 were selected by all reviewers as a “Yes” for all three of these dimensions. These spanned the domains of safety (n = 7), effectiveness (n = 7), and efficiency (n = 5) (Table S1 in the Electronic supplementary material, ESM). The measures were configured so that a score of 100% indicated optimal performance. For example, for a safety measure about avoiding the chronic use of benzodiazepines, we determined the proportion of older adults without ≥ 60 days’ supply of benzodiazepines during a measurement year, where 100% indicated optimal performance for that measure. Additionally, the observations within each domain were aggregated to determine an overall average score representing the total number of opportunities to avoid a quality problem for each domain.
The measures were operationally defined by the project team and pilot tested using pharmacy data provided by a national pharmacy chain. This data source included all older adults (age 65 or older) residing in an East Coast state who received at least one medication dispensed by that pharmacy chain during 2016. Medication attributes were identified using National Drug Codes. Where relevant, study eligibility criteria included the requirement that patients had received at least one dispensing of any medication within the first and last quarters of the measurement year. This criterion was intended to increase the likelihood that the study patients continued to receive their medication from the same pharmacy system that provided the data. Measure numerators and denominators and associated specifications were defined in a narrative document which guided the development of the analysis plan.
We excluded patients who received cancer medications, as many of our measures were not intended for end-of-life care. Patient demographics included age, gender, region of the state from which the prescription was dispensed, and payment type. We also identified the top five medical provider groups in the state by patient population, and attributed patients to these groups using a deidentified National Provider Identifier code. These groups represented leading medical practice organizations within the state. For the variables defining region, payment type, and provider group, the most frequent observation was used.
Descriptive statistics included patient age, gender, region, and payment type. Confidence intervals for the measures were derived from the standard error and denominator size. We performed a multivariable logistic regression analysis for each measure to determine if results differed significantly according to covariates. Statistical analyses were conducted using the software SAS 9.4 (SAS Institute Inc., Cary, North Carolina).
3 Results
3.1 Quality Measures
Detailed specifications of the S–E–E measures are included in Table S1 of the ESM. Seven measures addressed medication safety—avoiding the chronic use of benzodiazepines or central nervous system (CNS) depressants, avoiding the concurrent use of nonsteroidal anti-inflammatory medications (NSAIDS) and anticoagulants, avoiding the concurrent use of anticholinergic medications with anti-dementia medications, avoiding the use of fluoroquinolones as initial therapy, avoiding the chronic use of opioids after the initial opioid prescription, and avoiding selected high-risk medications. The high-risk medications included a condensed version of medications listed in the Beers and the Healthcare Effectiveness Data and Information Set criteria, deemed by our team to represent medications that present higher risk than therapeutic alternatives (e.g., first-generation antihistamines, tertiary tricyclic antidepressants; see Table S2 of the ESM for a complete listing).
The domain of effectiveness included five measures addressing patient adherence and two measures addressing the use of evidence-based medications in diabetes. One additional measure was tested that addressed the prioritization of recommended medications for hypertension: avoiding alpha- and beta-adrenergic blockers in the absence of compelling comorbidities. This measure was eventually abandoned due to its complexity. The effectiveness measures of patient adherence addressed the following chronic therapies: direct oral anticoagulant (DOAC) medications, oral antidiabetic medications, antidepressants, statins, and maintenance respiratory inhalers. Adherence was specified using a medication possession ratio (MPR) approach. We considered patients to be adherent if MPR was 0.8 or higher, indicating that the patient had medication supplied for at least 80% of the days between the first prescription of the relevant medication and the last day of the measurement year. A MPR of 0.8 or higher is a widely used threshold of medication adherence [9]. The measures of evidence-based medication use in diabetes identified patients who received at least one dispensing for an oral or injectable diabetes medication during 2016. Among this group, we identified the proportion who also received at least one dispensing for (1) a statin medication and (2) an angiotensin-acting medication.
The measures within the domain of efficiency addressed health system use and the utilization of generic medications. The former included measures determining the patient’s total number of prescribers and the total number of medications prescribed. We set a threshold of five or more prescribers as indicating a higher risk of medication-related problems associated with care fragmentation, and the patient’s receipt of an average of ten or more medications per month as a somewhat arbitrary threshold for a patient receiving a substantial number of medications which might trigger the need for regimen review. We also included measures of generic medication use, measured as an overall generic utilization rate, and including generic utilization rates for medications for diabetes and depression. Most US states either mandate or permit the substitution of generic formulations, yet opportunities may exist to increase the use of lower cost generics as alternatives to newer and higher-priced brand-name medications within the same therapeutic class when clinically appropriate.
3.2 Quality Measures in the Patient Population
The measures were applied to the eligible older population (N = 99,056). A majority of the patients were aged > 70 years (60.5%), female (56.5%), and had public insurance (Medicare) identified as the primary payment type (75.9%) (Table 1).
Results indicated a range of opportunities to improve medication use among older adults (Fig. 1). For the domain of safety, 12.8% of patients received a benzodiazepine chronically, while 23.6% received chronic CNS depressant medication. Additionally, among all new antibiotic prescriptions (no previous antibiotic prescription in the previous 60 days), fluoroquinolones represented 16.7% of dispensings. The safety measure addressing opioid use determined the number of patients with at least one opioid prescription who received at least 200 opioid dosage units, and 21.9% were found to have received at least this amount.
Within the domain of effectiveness, 71.7% of patients were adherent to DOAC, 82.8% to antidiabetic medications, 76.3% to antidepressants, 80.4% to cholesterol medications, and 46.1% to chronic respiratory inhalers. Approximately three of four patients with medications for diabetes also received at least one dispensing of a statin (74.4%) and at least one dispensing of an angiotensin-acting medication (73.6%). For the domain of efficiency, 78.3% of patients received prescriptions from less than five unique prescribers, and 93.3% utilized less than an average of ten medications per month. Additionally, among all of the dispensings that occurred in 2016, 87.4% were for generic medications, 88.7% of the dispensings for antidiabetic medications were for generics, while 98.7% of the dispensings for antidepressants were for generic products.
The aggregated results indicated that, overall, 85.7%, 76.1%, and 87.9% of the study population showed safe, effective, and efficient prescription medication use, respectively (Fig. 1).
3.3 Predictors of Optimal Performance
3.3.1 Safety
Measure rates were generally similar regardless of patient age group and gender, although some significant differences were identified. Compared to older adults aged 65–70 years, those who were > 80 years old had significantly higher odds of avoiding benzodiazepines [adjusted odds ratio (AOR) = 1.21, 95% confidence interval (CI) 1.13–1.29] and avoiding the use of CNS depressant agents (AOR = 1.21, 95% CI 1.15–1.28) (Table 2). Older adults aged > 80 years with dementia were almost twice as likely to avoid anticholinergics compared with those aged 65–70 years (AOR = 1.98, 95% CI 1.05–3.72). Additionally, patients above 70 years of age were significantly more likely to avoid current NSAIDs and anticoagulants (AORs were 1.45 and 2.17 for the 71–80 years group and those above 80 years of age, respectively), and also more likely to avoid high risk medications. Older adults aged > 70 years were significantly less likely to avoid receiving fluoroquinolones as initial therapy compared to those 65–70 years of age (AOR = 0.79). Compared to males, females were significantly less likely to avoid benzodiazepines (AOR = 0.55) or CNS depressants (AOR = 0.68), fluoroquinolones as initial therapy (AOR = 0.81), or opioids in larger quantities (AOR = 0.83).
3.3.2 Effectiveness
Compared to older adults aged 65–70 years, those aged 71–80 years were significantly more likely to adhere to oral antidiabetic (AOR = 1.16, 95% CI 1.02–1.32) and cholesterol (AOR = 1.08, 95% CI 1.02–1.16) medications, and those aged > 80 years were more likely to adhere to cholesterol medications (AOR = 1.18, 95% CI 1.10–1.28) (Table 3). Among patients with diabetes, those in the 71–80 years age group were significantly more likely to receive a prescription of a statin (AOR = 1.16) compared to those aged 65–70 years. However, those above 80 years of age were significantly less likely to receive a prescription for a statin (AOR = 0.86, 95% CI 0.77–0.99) or an ACEI/ARB (AOR = 0.79, 95% CI 0.71–0.89). Females were significantly less likely to adhere to cholesterol medications than males (AOR = 0.89, 95% CI 0.84–0.95).
3.3.3 Efficiency
Compared to older adults aged 65–70 years, those aged > 70 years were significantly less likely to have fewer (≤ 5) prescribers (AORs were 0.82 and 0.92 for the 71–80 years group and for those above 80 years, respectively) (Table 4). Additionally, females were significantly less likely to avoid receiving at least ten medications than males (AOR = 0.84, 95% CI 0.76–0.94).
4 Discussion
Given the ubiquity of medication use among older adults and its substantial potential for both benefit and harm, assessing the quality of medication use is vital to optimize patient health outcomes. At the provider level, this task is complicated by a fragmented health care system and often a lack of physician constancy. Population-level approaches to evaluate the quality of medication use among older adults are needed. Although several leading entities incorporate prescription medication use measures into their quality improvement efforts, evaluating and improving medication use among older adults remains a formidable challenge. In our comprehensive population-level study of the use of prescription medications among older adults, we found considerable room for improvement, with deficits from optimal performance ranging from 12.1% for the domain of efficiency, 14.3% for the domain of safety, and 23.9% for the domain of effectiveness.
Several measures stood out in terms of opportunity for improvement. Within the domain of safety, almost one-fourth of the study population (76.4%) received at least 60 days’ supply of CNS depressant medication. Bernardy et al. found that 12% of older veterans with post-traumatic stress disorder concurrently received three or more classes of CNS depressants [10]. Additionally, we found that women were less likely than males to avoid CNS depressants, a finding consistent with that reported by Bernardy et al. [10]. Given the increased risk of cognitive decline and falls associated with the use of CNS depressants in older adults [11], our finding raises concerns about increased potential adverse events among these patients. We considered it important to include a measure of opioid utilization in the safety domain. This measure reflects the ratio of short-term to chronic opioid utilizers, consistent with the aim that if opioids are prescribed, they should be used as briefly as possible and at the lowest dosage possible [12]. Furthermore, 13% of the study population were prescribed benzodiazepines chronically, a finding generally consistent with that reported in US-based studies [13,14,15]. A study conducted among older Medicare enrollees entering home healthcare services reported that 19% were prescribed a benzodiazepine [13], while another study reported that the prevalence of benzodiazepine use was approximately 10% among older veterans [14]. Yet another study by Maust et al. found that 13% of older adults reported using benzodiazepines [15]. Our result was substantially lower than the percentages reported by non-US studies [16, 17]: a Canadian study found that 25% of community-dwelling older adults used benzodiazepines [16], while a Brazilian study reported that the prevalence of benzodiazepine use among older adults was 21–27% [17]. Our finding is potentially alarming given the risks of these medications, which include cognitive impairment, delirium, falls, and fractures [18], leading to the recommendation that benzodiazepines should be avoided in this vulnerable population [6]. Our finding that females were less likely to avoid benzodiazepine use is consistent with an earlier report [19], indicating that efforts to reduce benzodiazepine use in this subgroup are needed.
For the domain of effectiveness, the measures of medication adherence indicated that a substantial percentage of patients do not refill prescriptions regularly. The lowest rate was among patients utilizing chronic inhalers for respiratory disease. Poor consistency in the refilling of chronic inhalers among older adults has been reported previously [20, 21]. Our finding may also suggest that some patients did not have chronic respiratory illness and were prescribed the inhaler on a short-term basis. Adherence to DOAC medication was 71.7%, a finding consistent with that reported in a published study [22]. A slightly higher percentage (76.3%) of the patients were adherent to antidepressant medications. Placing this result in the context of the literature on adherence with antidepressants is complicated by the predominance of research that focuses on treatment persistence in new therapy initiators only. Such research excludes the majority of patients who utilize antidepressant medications chronically, and while these medications may not need to be taken indefinitely, they should not be taken sporadically, as poor adherence patterns reveal. We believe that reporting adherence rates among all patients prescribed antidepressants, not just new therapy initiators, is a better approach. Approximately 80% of the patients were adherent to antidiabetic medications and cholesterol medications, underscoring the continuing need to promote adherence to these vital therapies. In addition, the finding that approximately one in four patients receiving medication for diabetes did not also receive a statin or an angiotensin-acting medication justifies the continued emphasis on these important elements of diabetes care [23,24,25].
For the domain of efficiency, we found that 21.7% of patients filled prescriptions from five or more unique prescribers. Having multiple prescribers has been shown to increase the risk of adverse drug events [26] and is associated with unnecessary medication use in older adults [27]. Our measure of receiving an average of ten or more medications per month may be considered extreme, as others have defined polypharmacy as five concurrent medications [28]. Yet, rather than classify a large proportion of patients as receiving a substantial number of medications, our higher threshold of at least ten prescribed medications identifies a smaller percentage of patients (6.7%) who would be at a higher risk for adverse drug events and associated health care costs. Measures addressing the utilization of generics revealed a limited opportunity for improvement. The overall generic utilization rate of 87.4% indicates that a substantial proportion of the medications utilized by older adults were not higher-cost branded products.
In our study, we offer a novel approach to the comprehensive assessment of medication use among older adults, which can augment other efforts to address quality of medication use in this population. The Beers criteria is well recognized as an important guide for prescribers, yet the medications it includes represent only a portion of all commonly prescribed medications that have the potential for untoward effects, while medication cost is beyond its scope [29,30,31]. The MAI does not directly address adherence patterns or cost using claims data [32]. Another notable framework, the START/STOPP criteria [33], contains a comprehensive validated array of standards that address inappropriate medication use and underuse. The START/STOPP criteria are intended for application in clinical settings, rather than for population-level analysis using administrative data sources. Many of the quality measures in the ACOVE project address medication use, yet the measures that can be calculated using administrative data require medical diagnoses beyond what is available in pharmacy data. Lastly, the PQA [3] has developed measures within the domains of adherence, appropriate medication use, safety, medication therapy management, and quality improvement, and many of their measures address similar dimensions of medication use to those in our framework. However, we sought to include only measures that can be reported using pharmacy claims solely, that address medication use among older adults exclusively, and can be aggregated to provide a profile score for each domain of medication use.
Several limitations of our study are important to note. Our review of relevant measures was restricted to the US; we did not review relevant quality measures or initiatives from other nations. We also note that the measures described here should not be interpreted as explicit criteria. Clinical circumstances can warrant, for example, the chronic use of benzodiazepines or the need for large quantities of opioid medications. For instance, among several factors, comorbidities, disease severity, physical function, and frailty may affect the quality of medication use in older adults. Thus, our measures should only be applied at larger units of analysis and to identify substantial differences across groups of similar patient populations. Also, measures described here are not universally accepted criteria. However, we describe a comprehensive framework that can be applied using prescription medication pharmacy claims and can examine the quality of prescription medication use in older adults. Additionally, pharmacy claims data are limited by a lack of information about patient diagnoses, disease severity, race/ethnicity, household income, and education, so these factors could not be assessed. Also, the findings may not be generalized to older adults from a different US region or pharmacy retailer. Finally, we did not formally evaluate the reliability and validity of the measures described in this study. An important next phase of this study is to determine if patient health outcomes differ according to the results for each domain. Further validation is warranted before the wide-scale application of this measurement framework for the purpose of accountability.
5 Conclusion
We provide a novel method to comprehensively evaluate quality of medication use among older adults using real-world prescription claims data. We found that a majority of older adults received safe, effective, and efficient prescription medications. However, our results also revealed a range of opportunities within each domain to better align medication use with current recommendations. Future studies are required to ascertain the validity of the measure set considering adverse events, health outcomes, and healthcare utilization.
References
Charlesworth CJ, Smit E, Lee DS, Alramadhan F, Odden MC. Polypharmacy among adults aged 65 years and older in the United States: 1988–2010. J Gerontol A Biol Sci Med Sci. 2015;70(8):989–95.
Steinman MA, Hanlon JT. Managing medications in clinically complex elders: “There’s got to be a happy medium”. JAMA. 2010;304(14):1592–601.
Pharmacy Quality Alliance. Measures overview. https://www.pqaalliance.org/assets/Measures/PQA%20Measure%20Overview%20082018.pdf. Accessed 18 Jan 2019.
Higashi T, Shekelle PG, Solomon DH, et al. The quality of pharmacologic care for vulnerable older patients. Ann Internal Med. 2004;140(9):714–20.
RAND Corporation. Developing quality of care indicators for the vulnerable elderly: the ACOVE Project (RB-4545-1). 2004. http://www.rand.org/pubs/research_briefs/RB4545-1/. Accessed 18 Jan 2019.
American Geriatrics Society. 2019 Updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. 2019. https://doi.org/10.1111/jgs.15767.
Hanlon JT, Schmader KE, Samsa GP, et al. A method for assessing drug therapy appropriateness. J Clin Epidemiol. 1992;45(10):1045–51.
Gallagher P, Ryan C, Byrne S, Kennedy J, O’Mahony D. STOPP (Screening Tool of Older Person’s Prescriptions) and START (Screening Tool to Alert doctors to Right Treatment). Consensus validation. Int J Clin Pharmacol Ther. 2008;46(2):72–83.
Hess LM, Raebel MA, Conner DA, Malone DC. Measurement of adherence in primary administrative databases: a proposal for standard definitions and preferred measures. Ann Pharmacother. 2006;40(7–8):1280–8.
Bernardy NC, Lund BC, Alexander B, Friedman MJ. Increased polysedative use in veterans with post-traumatic stress disorder. Pain Medicine. 2014;15(7):1083–90.
Huang AR, Mallet L, Rochefort CM, Eguale T, Buckeridge DL, Tamblyn R. Medication-related falls in the elderly: causative factors and preventive strategies. Drugs Aging. 2012;29(5):359–76.
Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain—United States, 2016. MMWR Recomm Rep. 2016;65(1):1–49.
Cotton BP, Lohman MC, Brooks JM, et al. Prevalence of and factors related to prescription opioids, benzodiazepines, and hypnotics among Medicare home health recipients. Home Healthc Now. 2017;35(6):304–13.
Brett J, Maust DT, Bouck Z, et al. Benzodiazepine use in older adults in the United States, Ontario, and Australia from 2010 to 2016. J Am Geriatr Soc. 2018;66(6):1180–5.
Maust DT, Lin LA, Blow FC. Benzodiazepine use and misuse among adults in the United States. Psychiatr Serv. 2019;70(2):97–106.
Voyer P, Preville M, Cohen D, Berbiche D, Beland S. The prevalence of benzodiazepine dependence among community-dwelling older adult users in Quebec according to typical and atypical criteria. Can J Aging. 2010;29(2):205–13.
Alvarenga J, de Layola F, Firmo J, Maria L-C, Elizabeth U. A population based study on health conditions associated with the use of benzodiazepines among older adults. Cad Saúde Pública. 2009;25(3):605–12.
Díaz-Gutiérrez MJ, Martínez-Cengotitabengoa M, Sáez de Adana E, et al. Relationship between the use of benzodiazepines and falls in older adults: a systematic review. Maturitas. 2017;101:17–22.
Marra EM, Mazer-Amirshahi M, Brooks G, van den Anker J, May L, Pines JM. Benzodiazepine prescribing in older adults in US ambulatory clinics and emergency departments (2001–2010). J Am Geriatr Soc. 2015;63(10):2074–81.
Turon O, Turan PA, Mirici A. Parameters affecting inhalation therapy adherence in elderly patients with chronic obstructive lung disease and asthma. Geriatr Gerontol Int. 2017;17(6):999–1005.
Albrecht JS, Park Y, Hur P, et al. Adherence to maintenance medications among older adults with chronic obstructive pulmonary disease. The role of depression. Ann Am Thorac Soc. 2016;13(9):1497–504.
Crivera C, Nelson WW, Bookhart B, et al. Pharmacy Quality Alliance measure: adherence to non-warfarin oral anticoagulant medications. Curr Med Res Opin. 2015;31(10):1889–95.
Vanderholm T, Renner HM, Stolpe SF, Adams AJ. An innovative approach to improving the proposed CMS star rating “Statin use in persons with diabetes.” J Manag Care Spec Pharm. 2018;24(11):1126–9.
Renner HM, Hollar A, Stolpe SF, Marciniak MW. Pharmacist-to-prescriber intervention to close therapeutic gaps for statin use in patients with diabetes: a randomized controlled trial. J Am Pharm Assoc. 2017;57(3S):S236–42.
Hurwitz JT, Grizzle AJ, Augustine J, Rehfeld R, Wild A, Abraham I. Accepting medication therapy management recommendations to add ACEIs or ARBs in diabetes care. J Manag Care Spec Pharm. 2016;22(1):40–8.
Jano E, Aparasu RR. Heathcare outcomes associated with Beers’ criteria: a systematic review. Ann Pharmacother. 2007;41(3):438–47.
Hajjar ER, Cafiero AC, Hanlol JT. Polypharmacy in elderly patients. Am J Geriatr Pharmacother. 2007;5(4):345–51.
Masnoon N, Shakib S, Kalisch-Ellett L, Caughey GE. What is polypharmacy? A systematic review of definitions. BMC Geriatrics. 2017;17(1):230.
Steinman MA, Rosenthal GE, Landefeld CS, Bertenthal D, Sen S, Kaboli PJ. Conflicts and concordance between measures of medication prescribing quality. Med Care. 2007;45:95–9.
Steinman MA, Rosenthal GE, Landefeld CS, Bertenthal D, Kaboli PJ. Agreement between drugs-to-avoid criteria and expert assessments of problematic prescribing. Arch Intern Med. 2009;169(14):1326–32.
Budnitz DS, Shehab N, Kegler SR, Richards CL. Medication use leading to emergency department visits for adverse drug events in older adults. Ann Intern Med. 2007;147(11):755–65.
Roth MT, Weinberger M, Campbell WH. Measuring the quality of medication use in older adults. J Am Geriatr Soc. 2009;57(6):1096–102.
O’Mahony D, O’Sullivan D, Byrne S, et al. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing. 2015;44(2):213–8.
Funding
This project was supported by an unrestricted grant provided by the University of Rhode Island Foundation. Dr. Kogut is partially supported by Institutional Development Award Number U54GM115677 from the National Institute of General Medical Sciences of the National Institutes of Health, which funds Advance Clinical and Translational Research (Advance-CTR). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
Study concept and design: SK, AV, NO, EP, NB. Acquisition of data: SK. Analysis and interpretation of data: EP, NB, SK, AV. Preparation of manuscript: SK, AV, EP, NO, NB. The authors would like to acknowledge Dr. Phillip G. Clark, Director of the Rhode Island Geriatric Education Center at the University of Rhode Island, for his technical assistance on the project.
Corresponding author
Ethics declarations
Conflict of interest
Drs. Kogut, Vyas, and Owens as well as Emily Patry and Nicholas Belviso have no conflicts of interest that are directly relevant to the content of this article.
Ethical approval
This study utilized deidentified retrospective data and was therefore not considered to be research on human subjects by the University of Rhode Island Institutional Review Board.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Vyas, A., Patry, E., Owens, N. et al. Development and Application of a Measurement Framework to Evaluate Safe, Effective and Efficient Medication Use Among Older Adults. Drugs - Real World Outcomes 6, 173–181 (2019). https://doi.org/10.1007/s40801-019-00162-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40801-019-00162-x