Abstract
Purpose of Review
Certain immunocompromised individuals are at risk for protracted COVID-19, in which SARS-CoV-2 leads to a chronic viral infection. However, the pathogenesis, diagnosis, and management of this phenomenon remain ill-defined.
Recent Findings
Herein, we review key aspects of protracted SARS-CoV-2 infection in immunocompromised individuals, or the so-called long persisters, and describe the clinical presentation, risk factors, diagnosis, and treatment modalities of this condition, as well as intra-host viral evolution. Based on the available data, we also propose a framework of criteria with which to approach this syndrome.
Summary
Protracted COVID-19 is an uncharacterized syndrome affecting patients with B-cell depletion; our proposed diagnostic approach and definitions will inform much needed future research.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction: Defining the Syndrome and Its Risk Factors
Despite major advances in our understanding, treatment, and prevention of coronavirus disease 2019 (COVID-19), there continues to be a lack of consensus surrounding how to define and approach immunocompromised individuals with persistent and protracted severe acute respiratory syndrome coronavirus 2 (SARS‑CoV‑2) infection, also known as “long persisters.” This phenomenon should be distinguished from “long COVID-19” or a “post-COVID-19 condition,” which is defined by the World Health Organization as a syndrome which occurs in individuals (regardless of underlying host status) who contracted COVID-19 within the prior 3 months and have at least 2 months of ongoing symptoms (such as fatigue, dyspnea, and cognitive dysfunction), with no alternative diagnosis [1]. Since the literature describing long persisters consists almost entirely of case reports and case series, little can be concluded about the risk factors, natural history, and optimal treatment of these patients. Nonetheless, several case studies have shown compelling evidence of persistent infection, by demonstrating either successful isolation of infectious SARS-CoV-2 weeks to months after the initial infection [2, 3, 4•, 5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20], and/or intra-host evolution of virus with clonal relatedness to the initial infecting strain (thus ruling out superinfection) [2, 3, 4•, 5,6,7,8,9,10, 12,13,14,15,16,17,18,19,20, 21•, 22,23,24,25,26,27,28,29,30,31,32], often with evidence of absent humoral immunity despite protracted illness. Symptoms of these patients have varied from recurrent severe pneumonia [4•, 6, 8, 11, 24] to asymptomatic courses [2, 15, 23, 25]. To avoid confusion with long COVID-19 syndrome, we will refer to this condition as “protracted COVID-19/SARS-CoV-2 infection.”
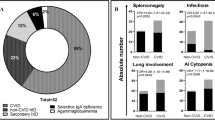
The underlying host factors that predispose to protracted SARS-CoV-2 infection remain to be defined. The literature consists of a predominance of individuals with B-cell depletion from a range of conditions, such as hematological malignancies, Chimeric Antigen Receptor (CAR)-modified T-cell therapy, hematopoietic cell transplantation (HCT), or anti-CD20 monoclonal antibodies to treat rheumatologic and other conditions [2, 3, 4•, 5,6,7,8,9,10,11, 13, 14, 17, 18, 20, 21•, 22, 24,25,26, 28,29,30, 32,33,34]. A few reported cases provide compelling evidence of prolonged infection in solid organ transplant (SOT), AIDS, and/or other conditions [7, 9, 10, 12, 15, 16, 23, 27, 31]. However, these reports are limited by publication bias, with clinicians opting to only publish “interesting” and “noteworthy” cases. Thus, although it is biologically plausible that B-cell depletion may be the major risk factor for protracted SARS-CoV-2 infection as neutralizing antibodies are required for control of SARS-CoV-2 [35], any individual with severe immunodeficiency and COVID-19 should be considered at risk for protracted infection until larger studies are carried to better define this syndrome. In addition, a precise definition of severe immunodeficiency is difficult, as the net state of immunosuppression can only be approximated. Nonetheless, in order to help standardize the approach to defining protracted SARS-CoV-2 infection in an immunocompromised individual, and to differentiate the approach to these patients from that of patients with long COVID-19, we propose the preliminary framework outlined in Table 1. This framework relies on virologic criteria (i.e., the requirement of persistently positive SARS-CoV-2 PCR testing beyond 21 days), clinical and radiographic criteria, and host criteria. We underscore however that these criteria are based on case reports and case series and are expected to change over time as new evidence emerges and as our understanding of the biology of SARS-CoV-2 infection in immunocompromised individuals evolves.
Treatment Options
Direct Acting Antivirals
Several antivirals have been approved for treatment of COVID-19. Remdesivir (RDV), an inhibitor of the viral RNA-dependent RNA polymerase, was approved for treatment of hospitalized patients >12 years of age in October 2020. In the ACTT-1 trial, hospitalized patients were randomized to 5 days of intravenous RDV or placebo [36]. There was a significant reduction in time to clinical recovery (11 days vs 15 days for placebo) and a non-significant trend toward decreased mortality (8% for RDV and 11.6% for placebo [36]). Diaz et al subsequently demonstrated a mortality benefit [37]. Duration of treatment with RDV varies from 3 to 10 days, showing benefits even with shorter 3-day courses provided it is initiated early during infection [38, 39].
Most data regarding the use of RDV for treatment of protracted COVID-19 come from case series or reports [22, 40, 41•, 42]. RDV monotherapy has been rarely described and is reported to be ineffective [4•]. Thus, RDV is often used in combination with passive humoral therapy. In some cases, RDV resulted in partial improvement and was then followed by convalescent plasma (CCP) infusion [43]. Brown et al. described 31 immunocompromised individuals with a median duration of symptoms of 62 days; all patients were considered “B-cell depleted” due to either a primary immunodeficiency leading to hypogammaglobulinemia or treatment with an anti-CD20 targeted drug. In total, 65% of patients (20/31) cleared the infection. Over half of the patients received a combination of RDV and an antibody-based therapy (monoclonal antibody [mAb] or CCP), whereas 7 patients received RDV monotherapy. None of the patients included received antibody-based monotherapy. The use of combination therapy was associated with increased odds of clearing the infection compared to RDV monotherapy (odds ratio of 23.1 (95% CI = 1.3–424.9 [p=0.035]) [41•]. Interestingly, the authors reported high rates of viremia in the subgroup of patients in whom it was measured (7/12 patients, 58.3%). Emergence of resistance has also been reported with RDV [44].
Molnupiravir and the combination of nirmatrelvir with ritonavir were granted emergency use authorization (EUA) by the US Food and Drug Administration (FDA) in December of 2021; neither of these agents has been used in immunocompromised individuals with protracted COVID-19.
Passive Humoral Therapy
Convalescent Plasma
Literature regarding the benefits of CCP in the treatment of COVID-19 has been controversial, and data on immunocompromised individuals is scarce. A subgroup analysis of 126 immunodeficient patients from the REMAP-CAP Investigators showed a possible benefit [45]. Some investigators have used serial doses of CCP for treatment of protracted COVID-19 in patients with absent humoral immunity. Hueso el al. reported on 17 patients with B-cell depletion and/or hypogammaglobulinemia with protracted symptoms (median of 56 days) that responded to two transfusions of CCP [46•]. The vast majority experienced improvement in symptoms; moreover, SARS-CoV-2 RNAemia decreased within 7 to 14 days in all 9 patients in whom it was measured [46•].
Lang-Meli et al. evaluated 16 patients with primary immunodeficiencies treated with CCP between 8 and 132 days after onset of symptoms; about half of the patients received RDV. Treatment resulted in an increase in the cycle threshold (Ct) for SARS-CoV-2 PCR on nasopharyngeal (NP) swabs as well as symptomatic improvement in all patients [47]. The results of full-length SARS-CoV-2 genome sequencing were available in only 3 patients; emergence of a new viral subpopulation was noted in one patient who received a second course of CCP which ultimately resulted in viral clearance. As described in the “Direct Acting Antivirals” section, Brown et al suggested that combination of RDV and passive humoral therapy is superior to RDV alone for clearing protracted infections [41•]; however, Hueso et al. used CCP alone with success [46•]. Smaller case series and case reports have shown clinical improvement and/or viral clearance [48,49,50,51,52,53], while others have failed to show effectiveness [2, 6].
Monoclonal Antibodies
Another approach for the management of suspected protracted SARS-CoV-2 infection is the use of monoclonal antibodies (mAb). In some cases, treatment courses of RDV and/or CP failed to clear the virus, resulting in the use of different mAb such as sotrovimab [54]and casirivimab/imdevimab [26, 55, 56]. There have been reports of bamlanivimab use, but rapid development of resistance did not allow further use as monotherapy [25, 28, 33, 57].
Unfortunately, the use of mAb in the USA is limited by the criteria defined in the FDA’s EUA document, which has generally restricted their use for treating COVID-19 only among non-hospitalized individuals who do not require supplemental oxygen support, and who are within 7–10 days of their diagnosis (FDA fact sheet). Thus, clinicians in the USA are unable to deviate from these criteria, unless the manufacturer of the drug offers a compassionate use program, where the drug can be used outside the EUA on a case-by-case basis. Additionally, the emergence of new variants has resulted in resistance to all prior mAb, such that only two are in current use, one for treatment within 7 days of symptom onset (bebtelovimab) and another one for pre-exposure prophylaxis (tixagevimab-cilgavimab).
Other Combination Therapy
Combination antiviral therapy may have theoretical advantages. Indeed, using drugs that bind to multiple viral targets may aid in viral clearance, similarly to HIV and HCV. In vitro studies have shown increased antiviral activity when combining nirmatrelvir/ritonavir with remdesivir and molnupiravir as well as with molnupiravir-based regimens [58, 59]; however, none of these regimens has been tested in humans. These combinations may be particularly helpful in individuals with protracted COVID-19, as they may prevent emergence of resistance and/or new variants. Intravenous immunoglobulin (IVIg) replacement has been occasionally used in combination with RDV and/or CCP [8, 60, 61]
SARS-CoV2-Specific T-Cells
Although neutralizing antibodies are required for control of SARS-CoV-2 infection [35], preliminary data suggest that T-cells may be able to protect against mAb-resistant SARS-CoV-2 variants, even in the absence of a neutralizing antibody response [62]. Additionally, Spike proteins from novel variants may not escape T-cell-mediated immunity elicited by the wild-type S protein [62]. Thus, there is interest in utilizing banked or “off-the-shelf” SARS-CoV-2 viral-specific T-cells (VSTs) for the treatment of COVID-19 in immunocompromised individuals. There is indeed precedent supporting this approach with other intractable viral infections, such as Epstein-Barr virus (EBV), cytomegalovirus (CMV), and adenovirus in HCT recipients [63], CMV infection in SOT recipients [64], and even progressive multifocal leukoencephalopathy in a small case series of individuals with varied causes of immunodeficiency [65]. The results of these and other studies, while promising, are also mixed, with some patients responding to VSTs and others exhibiting no response, and with multiple lingering unknowns such as optimal dosing and frequency of administration, the durability of VSTs in an immunodeficient host (particularly those receiving iatrogenic immunosuppression which is expected to dampen the activity of VSTs), and the underlying biology of treatment successes versus failures.
In the only published case report of SARS-CoV-2 VSTs to date, investigators described a heart transplant recipient with refractory COVID-19 pneumonia, whose condition progressed despite remdesivir, corticosteroids, and tocilizumab [66]. The patient subsequently received three doses of an off-the-shelf partially HLA matched SARS-CoV-2 VST (2 × 107 cells per dose, approximately 14 ± 4 days apart), which resulted in eradication of the virus and clinical remission. A recent presentation at the American Transplant Congress meeting suggested a potential role of SARS-CoV-2 VSTs in six patients with hematologic malignancies or SOT, though the results were mixed [67].
Although there is much to be learned about the efficacy of SARS-CoV-2 VSTs, including issues related to cost, manufacturing, access, HLA-matching, and patient candidacy, administration of VSTs does appear to be safe, with newer products demonstrating either no safety concerns or only minimal grade 1 graft-versus-host disease in HCT [68]. Since many VST products appear to be long-lasting, with some VSTs being detectable for as long as 9 years after infusion [68], whether SARS-CoV-2 VSTs can be used for primary prophylaxis of COVID-19 should be evaluated in clinical trials. Indeed, because immune escape of SARS-CoV-2 from T-cells has not been a major phenomenon [69] (in contrast immune escape of novel variants from mAb), the use of VSTs for COVID-19 prophylaxis may circumvent the issue of emergence of SARS-CoV-2 variants with reduced susceptibility to other prophylactic interventions such as monoclonal antibodies [70]. However, whether prophylactic VSTs will persist in the absence of ongoing viral stimulation is unknown.
Other
A single case report exists of therapeutic vaccination with the BNT162b2 mRNA vaccine in a patient with Wiskott-Aldrich syndrome. The authors demonstrated enhanced cellular responses and seroconversion after vaccination, with viral clearance 72 days after the first vaccine dose [71]. A new COVID-19 peptide vaccine that induces T-cell immunity is being evaluated in patients with B cell or antibody deficiency; an open-label phase I trial showed potent T-cell responses and a favorable safety profile in healthy adults [72]. However, peptide-based COVID-19 vaccines have not been used in protracted infections.
Interferon gamma has been proposed as therapy to stimulate cellular immunity against viral infections. Van Laarhoven et al. used this approach in 5 patients with COVID-19; most had previously received RDV, CP, or IVIg [73]. Four patients cleared SARS-CoV-2, and one patient passed away after a prolonged hospital stay after. Another case was successfully treated with interferon beta-1b in combination with RDV and IVIg [74].
Role of Cycle Threshold Values and Viral Loads to Guide Management
Cycle Threshold
Understanding the level of infectivity in patients with prolonged SARS-CoV-2 nucleic acid test positivity using a quantitative test result is crucial, to guide both therapy and public health policy, as immunocompromised individuals may remain test-positive and infectious for weeks and thus contribute to ongoing community spread of the virus [75]. The SARS-CoV-2 reverse transcriptase quantitative PCR (RT-qPCR) test provides a quantitative value, the cycle threshold (Ct) value, which inversely correlates with viral loads [76]. Determining a correlation between Ct values and replication-competent virus may help distinguish between infectious virus and non-viable virus which is no longer infectious. Although many reports have demonstrated a correlation between decreases in Ct values with recurrence of symptoms and culture positivity in immunocompromised individuals [2, 3, 4•, 11], the use of Ct values in the clinical setting is not currently endorsed by the Infectious Diseases Society of America (IDSA) or the Association of Molecular Pathology due to lack of standardization and discrepant results [77]. A standardized quantitative test is urgently needed to help differentiate infectious versus non-viable virus, and perhaps to guide treatment.
Viral Load
It is now becoming increasingly understood that plasma SARS-CoV-2 viremia correlates with the severity of pneumonia. In one study, SARS-CoV-2 viral RNA was detected in plasma of 100%, 52.6%, and 11.1% of individuals in the intensive care unit (ICU), regular floor, and outpatient setting, respectively [78], and plasma viral RNA levels were significantly higher in ICU patients than in non-ICU patients and correlated with higher disease severity scores. Plasma SARS-CoV-2 RNA also served as a biomarker for disease severity, with levels > 6000 copies/mL being strongly associated with mortality. Furthermore, it appears as though plasma RNA levels also correlate with lower respiratory tract SARS-CoV-2 RNA levels [79], suggesting that it may have a role as a surrogate for overall SARS-CoV-2 disease burden. In another study, plasma SARS-CoV-2 RNA levels at the time of presentation predicted both severe disease and 28-day mortality [80], with upregulation of prominent proteomic pathways such as those related to SARS-COV-2 entry, tissue damage, and coagulation pathways. High plasma SARS-CoV-2 RNA levels have not surprisingly also been reported in immunocompromised individuals with COVID-19 [4•, 6, 8, 28].
Although measurement of plasma viral loads is not clinically available, its use as a surrogate endpoint for COVID-19 outcomes in immunocompromised individuals should be evaluated in clinical trials. Given that we are now in the era of direct-acting antivirals that target SARS-CoV-2, it is imperative to determine whether treating immunocompromised individuals with antivirals (such as RDV, nirmatrelvir/ritonavir, and molnupiravir) until suppression of their plasma SARS-CoV-2 viremia will improve clinical outcomes and prevent protracted infection compared to standard practice whereby all individuals receive a fixed duration of these drugs. A precedent for such an approach already exists with other opportunistic viruses such as cytomegalovirus [81], in which durations of therapy vary based on the viral response to antivirals.
Emergence of Variants
SARS-CoV-2 evolution may also develop in an immunocompromised individuals, resulting in emergence of mutations within the Spike gene and other areas of the genome [2, 3, 4•, 5,6,7,8,9,10, 12, 15,16,17, 19, 20, 21•, 22, 25,26,27,28,29,30,31,32, 82]. Indeed, it is speculated that many of the circulating variants of concern may have emerged as a result of intra-host evolution in immunocompromised individuals with protracted infection, followed by spread to the general population [6, 83]. In one case report, a CAR-T-cell recipient with over 70 days of active SARS-CoV-2 infection exhibited the evolution of mutations in the Spike gene (namely a Y144 deletion and a D215G substitution) that would eventually be identified months later in what were then referred to as the UK (alpha) and South African (beta) variants, long after the patient’s death [6]. Other case reports and case series have also demonstrated the simultaneous existence of multiple mixed populations of SARS-CoV-2 variants that emerged in the setting of severe immunosuppression [24, 27], or of mutations in the Spike gene (such as E484Q) resulting in reduced susceptibility to monoclonal antibodies such as bamlanivimab [28, 33].
Immune escape may also develop during the course of natural infection in the certain hosts. For example, in a patient with advanced HIV infection (CD4 count = 6 cells/uL) and over 190 days of COVID-19 [12], the patient’s original infecting SARS-CoV-2 strain developed mutations found in Omicron and other variants and showed evidence of immune escape against self-plasma, Pfizer BNT162b2, and antibodies elicited by Delta. Of additional concern is a recent report demonstrating treatment-emergent mutations in the Spike gene conferring resistance to sotrovimab that developed within 2 weeks of therapy in 4 immunocompromised individuals (lung transplant, common variable immunodeficiency, kidney transplant, and myelodysplasia) [16].
Hospital Precautions and Self-quarantine: When Is It Safe to Discontinue?
It is well-established that healthy people generally do not harbor infectious virus beyond 10 days of initial infection [84]. Additionally, although SARS-CoV-2 RNA from healthy individuals may be detected for up to 28 days or longer [85], this phenomenon represents the identification of inert, non-infectious, non-replicating RNA fragments [84]. Thus, the CDC recommends quarantine for at least 5 days for otherwise healthy individuals, while wearing a mask in public for a total of 10 days [86].
However, hospital systems continue to struggle with the optimal approach for infection prevention practices among immunocompromised individuals with COVID-19 due to the lack of readily available or accurate diagnostic modalities that can distinguish between infectious virus and non-viable RNA with a high degree of certainty. Practice guidance from the CDC regarding this issue has evolved over time, with the most recent recommendation suggesting a composite approach utilizing a PCR test-based strategy, beginning at 20 days after the initial positive SARS-CoV-2 test, with consultation with an infectious disease specialist [87]. This contrasts with transmission-based recommendations for other hosts, in whom a time-based strategy (generally up to 10 days since symptom onset) is employed. Although this approach is easily implemented, it may result in some immunocompromised individuals being isolated for longer than is necessary, given the difficulty in determining whether a positive PCR test represents infectious virus or not. Further complicating this matter is the phenomenon of intermittent SARS-CoV-2 PCR positivity, which has been demonstrated in immunocompromised individuals with protracted courses [3, 4•].
Although it appears that low Ct values (generally < 25) may correlate with infectivity [88], these values are not recommended for clinical use in the USA, and isolating SARS-CoV-2 by culture is cumbersome, expensive, and not readily available. Recently, it has been suggested that SARS-CoV-2 antigen positivity correlates better with infectious virus than does PCR positivity [88]. Whether the use of SARS-CoV-2 antigen testing in immunocompromised individuals can streamline infection prevention practices such that those with negative antigen results are designated “non-infectious” remains to be determined. Until more data are available, clinical judgement and an understanding of the behavior of SARS-CoV-2 in immunocompromised individuals are recommended when devising local infection prevention policies. An example of what may be considered is outlined in Table 2, although it is understood that these suggestions should not be taken as formal recommendations but rather as a framework with which institutions struggling to cope with infection prevention policies may approach this problem. It is also expected that these policies may shift depending on the stage of the pandemic and bed capacity, and that they will need to be reappraised as new data emerge.
When to Proceed with Immune/Chemotherapy and Transplantation
Decisions around when to proceed with further immunotherapy, chemotherapy, or transplantation should consider the risks of progression of the underlying condition while avoiding additional immunosuppression during active COVID-19, versus further decreasing immune responses that are crucial to containing/eradicating viral infections. Urgent transplantation can be a life-saving procedure, and timing of organ donation is difficult to predict. Similarly, prolonged delays in CAR-T-cell therapy or HCT may not be feasible in certain hematologic malignancy patients, who may die as a result of their underlying malignancy. A thoughtful and thorough discussion among health care personnel and the patient (and/or patient’s proxy) should be held prior to any procedure that further weakens immune responses, as it could lead to worsening SARS-CoV-2 infection with devastating consequences.
Emerging data suggests that it might be feasible to proceed with immune/chemotherapy in some circumstances where a multidisciplinary team with expertise in these highly vulnerable patients exist, as well as non-lung solid organ transplant [89, 90]. However, all these experiences and recommendations are based on acute COVID-19 in otherwise healthy donors or in recovered candidates, and the optimal timing to proceed with immunosuppressive treatments for patients with protracted COVID-19 is unknown. We refer the reader to professional societies recommendations, which are frequently updated (AST COVID-19 resources, OPTN network, ASTCT COVID-19 resource community, ASH COVID-19 resources).
Future Directions
The morbidity and mortality associated with COVID-19 have decreased since the onset of the pandemic, largely due to widespread vaccination and safe and effective treatments, as well as the progress that has been achieved in our general understanding of the biological aspects of SARS-CoV-2 infection. However, several key questions remain about immunocompromised individuals with protracted COVID-19. It is imperative for the scientific community to define the prevalence of protracted infection and the risks factors that predispose to this condition. It is also critical to improve our understanding of intra-host viral evolution and the emergence of novel variants, as this may have a tremendous impact on public health. Finally, it is of paramount importance to optimize the treatment of these patients, in whom the virus behaves not as an acute but rather as a chronic viral infection. To accomplish this, the scientific community must conduct trials that both enhance our knowledge and either lead to newer therapies or to the use of combinations of existing drugs with different mechanisms of action that are given until remission of infection. It is hoped that these approaches will reduce COVID-19-related morbidity and mortality in these patients and allow them to safely proceed with life-saving immunosuppressive treatments that they ultimately need.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
World Health Organization (WHO) clinical case definition working group on post COVID-19 condition. A clinical case definition of post COVID-19 condition by a Delphi consensus, 6 October 2021. https://www.who.int/publications/i/item/WHO-2019-nCoV-Post_COVID-19_condition-Clinical_case_definition-2021.1.
Avanzato VA, Matson MJ, Seifert SN, et al. Case study: prolonged infectious SARS-CoV-2 shedding from an asymptomatic immunocompromised individual with cancer. Cell. 2020;183(7):1901-1912. e9.
Baang JH, Smith C, Mirabelli C, et al. Prolonged severe acute respiratory syndrome coronavirus 2 replication in an immunocompromised patient. J Infect Dis. 2021;223(1):23–7.
• Choi B, Choudhary MC, Regan J, et al. Persistence and evolution of SARS-CoV-2 in an immunocompromised host. N Engl J Med. 2020;383(23):2291–3. Highlights potential for persistent infection and accelerated viral evolution in immunocompromised hosts.
Aydillo T, Gonzalez-Reiche AS, Aslam S, et al. Shedding of viable SARS-CoV-2 after immunosuppressive therapy for cancer. N Engl J Med. 2020;383(26):2586–8.
Hensley MK, Bain WG, Jacobs J, et al. Intractable coronavirus disease 2019 (COVID-19) and prolonged severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) replication in a chimeric antigen receptor-modified T-cell therapy recipient: a case study. Clin Infect Dis. 2021;73(3):e815–21.
Tarhini H, Recoing A, Bridier-Nahmias A, et al. Long-term severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infectiousness among three immunocompromised patients: from prolonged viral shedding to SARS-CoV-2 superinfection. J Infect Dis. 2021;223(9):1522–7.
Sepulcri C, Dentone C, Mikulska M, et al. The longest persistence of viable SARS-CoV-2 with recurrence of viremia and relapsing symptomatic COVID-19 in an immunocompromised patient—a case study. Open Forum Infect Dis 2021;8(11):ofab217. https://doi.org/10.1093/ofid/ofab217
Sung A, Bailey AL, Stewart HB, et al. Isolation of SARS-CoV-2 in viral cell culture in immunocompromised patients with persistently positive RT-PCR results. Front Cell Infect Microbiol 2022;12:804175. https://doi.org/10.3389/fcimb.2022.804175
Morel A, Imbeaud S, Scemla A, et al. Severe relapse of SARS-CoV-2 infection in a kidney transplant recipient with negative nasopharyngeal SARS-CoV-2 RT-PCR after rituximab. Am J Transplant Off J Am Soc Transplant Am Soc Transplant Surg. 2022;22(8):2099–103.
Thornton CS, Huntley K, Berenger BM, et al. Prolonged SARS-CoV-2 infection following rituximab treatment: clinical course and response to therapeutic interventions correlated with quantitative viral cultures and cycle threshold values. Antimicrob Resist Infect Control. 2022;11(1):1–6.
Cele S, Karim F, Lustig G, et al. SARS-CoV-2 prolonged infection during advanced HIV disease evolves extensive immune escape. Cell Host Microbe. 2022;30(2):154-162. e5.
Leung WF, Chorlton S, Tyson J, et al. COVID-19 in an immunocompromised host: persistent shedding of viable SARS-CoV-2 and emergence of multiple mutations: a case report. Int J Infect Dis. 2022;114:178–82.
Pallett SJ, Wake R, Youngs J, et al. Adjunctive viral cell culture supports treatment decision-making in patients with secondary humoral immunodeficiency and persistent SARS-CoV-2 infection. Br J Haematol. 2021;196(5):1170–4.
Weigang S, Fuchs J, Zimmer G, et al. Within-host evolution of SARS-CoV-2 in an immunosuppressed COVID-19 patient as a source of immune escape variants. Nat Commun. 2021;12(1):1–12.
Rockett R, Basile K, Maddocks S, et al. Resistance mutations in SARS-CoV-2 delta variant after sotrovimab use. N Engl J Med. 2022;386(15):1477–9.
Gordon CL, Smibert OC, Holmes NE, et al. Defective severe acute respiratory syndrome coronavirus 2 immune responses in an immunocompromised individual with prolonged viral replication. Open Forum Infect Dis. 2021;8(9):ofab359. https://doi.org/10.1093/ofid/ofab359
Pérez-Lago L, Aldámiz-Echevarría T, García-Martínez R, et al. Different within-host viral evolution dynamics in severely immunosuppressed cases with persistent SARS-CoV-2. Biomedicines. 2021;9(7):808.
Truong TT, Ryutov A, Pandey U, et al. Increased viral variants in children and young adults with impaired humoral immunity and persistent SARS-CoV-2 infection: a consecutive case series. EBioMedicine. 2021;67: 103355.
Monrad I, Sahlertz SR, Nielsen SSF, et al. Persistent severe acute respiratory syndrome coronavirus 2 infection in immunocompromised host displaying treatment induced viral evolution. Open Forum Infect Dis. 2021;8(7):ofab295. https://doi.org/10.1093/ofid/ofab295
• Kemp SA, Collier DA, Datir RP, et al. SARS-CoV-2 evolution during treatment of chronic infection. Nature. 2021;592(7853):277–82. Selection of mutations on SARS-CoV-2 during convalescent plasma therapy, associated with the emergence of viral variants with reduced susceptibility to neutralizing antibodies in immunosuppressed individuals; caution advised when using this approach in this patient population.
Morishita M, Suzuki M, Matsunaga A, et al. Prolonged SARS-CoV-2 infection associated with long-term corticosteroid use in a patient with impaired B-cell immunity. J Infect Chemother. 2022;28(7):971–4.
Spinicci M, Mazzoni A, Borchi B, et al. AIDS patient with severe T cell depletion achieved control but not clearance of SARS-CoV-2 infection. Eur J Immunol. 2022;52(2):352.
Nussenblatt V, Roder AE, Das S, et al. Yearlong COVID-19 infection reveals within-host evolution of SARS-CoV-2 in a patient with B-cell depletion. J Infect Dis. 2022;225(7):1118–23.
Bronstein Y, Adler A, Katash H, Halutz O, Herishanu Y, Levytskyi K. Evolution of spike mutations following antibody treatment in two immunocompromised patients with persistent COVID-19 infection. J Med Virol. 2022;94(3):1241–5.
Bailly B, Péré H, Veyer D, et al. Persistent coronavirus disease 2019 (COVID-19) in an immunocompromised host treated by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)-specific monoclonal antibodies. Clin Infect Dis. 2022;74(9):1706–7.
Chen L, Zody MC, Di Germanio C, et al. Emergence of multiple SARS-CoV-2 antibody escape variants in an immunocompromised host undergoing convalescent plasma treatment. Msphere. 2021;6(4):480.
Truffot A, Andréani J, Le Maréchal M, et al. SARS-CoV-2 variants in immunocompromised patient given antibody monotherapy. Emerg Infect Dis. 2021;27(10):2725.
Lynch M, Macori G, Fanning S, et al. Genomic evolution of SARS-CoV-2 virus in immunocompromised patient, Ireland. Emerg Infect Dis. 2021;27(9):2499.
Borges V, Isidro J, Cunha M, et al. Long-term evolution of SARS-CoV-2 in an immunocompromised patient with non-Hodgkin lymphoma. Msphere. 2021;6(4):244.
Hoffman SA, Costales C, Sahoo MK, et al. SARS-CoV-2 neutralization resistance mutations in patient with HIV/AIDS, California, USA. Emerg Infect Dis. 2021;27(10):2720.
Reuken PA, Stallmach A, Pletz MW, et al. Severe clinical relapse in an immunocompromised host with persistent SARS-CoV-2 infection. Leukemia. 2021;35(3):920–3.
Destras G, Assaad S, Bal A, et al. Bamlanivimab as monotherapy in two immunocompromised patients with COVID-19. Lancet Microbe. 2021;2(9): e424.
Truong TT, Bard JD, Butler-Wu SM. Rapid antigen assays for SARS-CoV-2: promise and peril. Clin Lab Med. 2022;42(2):203–22.
Dispinseri S, Secchi M, Pirillo MF, et al. Neutralizing antibody responses to SARS-CoV-2 in symptomatic COVID-19 is persistent and critical for survival. Nat Commun. 2021;12(1):1–12.
ACTT-1 Study Group. Remdesivir for the treatment of COVID-19: final report. N Engl J Med. 2020;383(19):1813–26.
Diaz GA, Christensen AB, Pusch T, et al. Remdesivir and mortality in patients with coronavirus disease 2019. Clin Infect Dis. 2022;74(10):1812–20.
Goldman JD, Lye DC, Hui DS, et al. Remdesivir for 5 or 10 days in patients with severe COVID-19. N Engl J Med. 2020;383(19):1827–37.
Gottlieb RL, Vaca CE, Paredes R, et al. Early remdesivir to prevent progression to severe COVID-19 in outpatients. N Engl J Med. 2022;386(4):305–15.
Kajova M, Kekäläinen E, Anttila V, Paajanen J. Successful treatment with a short course of remdesivir in a case of prolonged COVID-19 in a lymphoma patient. Infect Dis. 2022;54(6):455–9.
• Brown LK, Moran E, Goodman A, et al. Treatment of chronic or relapsing COVID-19 in immunodeficiency. J Allergy Clin Immunol. 2022;149(2):557-561.e1. https://doi.org/10.1016/j.jaci.2021.10.031. Highlights role of passive humoral therapy in the treatment of protracted COVID-19 in patients with B-cell depletion.
Fujii H, Tsuji T, Sugitani M, et al. Prolonged persistence of SARS-CoV-2 infection during A AVD therapy for classical Hodgkin’s lymphoma: a case report. Curr Probl Cancer. 2021;45(6): 100739.
Casarola G, D’Abbondanza M, Curcio R, et al. Efficacy of convalescent plasma therapy in immunocompromised patients with COVID-19: a case report. Clin Infect Pract. 2021;12: 100096.
Martinot M, Jary A, Fafi-Kremer S, et al. Emerging RNA-dependent RNA polymerase mutation in a remdesivir-treated B-cell immunodeficient patient with protracted coronavirus disease 2019. Clin Infect Dis. 2021;73(7):e1762–5.
Abdelhady H, Abdelrazik M, Abdi Z, et al. Effect of convalescent plasma on organ support–free days in critically ill patients with COVID-19: a randomized clinical trial. JAMA. 2021;326(17):1690–702.
• Hueso T, Pouderoux C, Pere H, et al. Convalescent plasma therapy for B-cell-depleted patients with protracted COVID-19. Blood. 2020;136(20):2290–5. https://doi.org/10.1182/blood.2020008423.Convalescent plasma appears to be a promising approach for treatment of protracted COVID-19 in B-cell-depleted patients who are unable to mount a specific humoral response to SARS-CoV-2.
Lang-Meli J, Fuchs J, Mathé P, et al. Case series: convalescent plasma therapy for patients with COVID-19 and primary antibody deficiency. J Clin Immunol. 2022;42(2):253–65.
Delgado-Fernández M, García-Gemar GM, Fuentes-López A, et al. Treatment of COVID-19 with convalescent plasma in patients with humoral immunodeficiency–three consecutive cases and review of the literature. Enferm Infecc Microbiol Clin. 2022;40(9):507–516. https://doi.org/10.1016/j.eimc.2021.01.013
Ferrari S, Caprioli C, Weber A, Rambaldi A, Lussana F. Convalescent hyperimmune plasma for chemo-immunotherapy induced immunodeficiency in COVID-19 patients with hematological malignancies. Leuk Lymphoma. 2021;62(6):1490–6.
Capoluongo E, Nardelli C, Esposito MV, et al. Case report: discovery a novel SARS-CoV-2 variant in a six-months long-term swab positive female suffering from non-Hodgkin lymphoma. Front Oncol. 2021;11(705948):2880.
Nyström K, Hjorth M, Fust R, et al. Specific T-cell responses for guiding treatment with convalescent plasma in severe COVID-19 and humoral immunodeficiency: a case report. BMC Infect Dis. 2022;22(1):1–7.
Moore JL, Ganapathiraju PV, Kurtz CP, Wainscoat B. A 63-year-old woman with a history of non-Hodgkin lymphoma with persistent SARS-CoV-2 infection who was seronegative and treated with convalescent plasma. Am J Case Rep. 2020;21: 927812.
Moutinho-Pereira S, Calisto R, Sabio F, Guerreiro L. High-titre convalescent plasma therapy for an immunocompromised patient with systemic lupus erythematosus with protracted SARS-CoV-2 infection. BMJ Case Rep CP. 2021;14(8): e244853.
Montejano R, Marcelo C, Falces-Romero I, et al. Efficacy of sotrovimab for persistent coronavirus disease-2019 in a severely immunocompromised person living with HIV. AIDS. 2022;36(5):751–3.
Drouin AC, Theberge MW, Liu SY, et al. Successful clearance of 300 day SARS-CoV-2 infection in a subject with B-cell depletion associated prolonged (B-DEAP) COVID by REGEN-COV anti-spike monoclonal antibody cocktail. Viruses. 2021;13(7):1202.
Luitel P, Vais D, Gidron A. Successful treatment of persistent coronavirus disease 2019 infection in a patient with hypogammaglobulinemia with REGN-COV2: a case report. Open Forum Infect Dis. 2021;8(8):ofab335. https://doi.org/10.1093/ofid/ofab335
Daher A, Müller T, Spiesshoefer J, Dreher M, Panse J. Successful treatment of prolonged COVID-19 with bamlanivimab in a patient with severe B-cell aplasia due to treatment with an anti-CD20 monoclonal antibody: a case report. Respir Med Case Rep. 2021;34: 101560.
Jonsdottir HR, Siegrist D, Julien T, et al. Molnupiravir combined with different repurposed drugs further inhibits SARS-CoV-2 infection in human nasal epithelium in vitro. Biomed Pharmacother. 2022;150. https://doi.org/10.1016/j.biopha.2022.113058
Schultz DC, Johnson RM, Ayyanathan K, et al. Pyrimidine inhibitors synergize with nucleoside analogues to block SARS-CoV-2. Nature. 2022;604(7904):134–40.
Chaudhry B, Didenko L, Chaudhry M, Malek A, Alekseyev K. Longest reported case of symptomatic COVID-19 reporting positive for over 230 days in an immunocompromised patient in the United States. SAGE Open Med Case Rep. 2021;9:2050313X211040028.
Yasuda H, Mori Y, Chiba A, et al. Resolution of one-year persisting COVID-19 pneumonia and development of immune thrombocytopenia in a follicular lymphoma patient with preceding rituximab maintenance therapy: a follow-up report and literature review of cases with prolonged infections. Clin Lymphoma Myeloma Leuk. 2021;21(10):e810–6.
Kingstad-Bakke B, Lee W, Chandrasekar SS, et al. Vaccine-induced systemic and mucosal T cell immunity to SARS-CoV-2 viral variants. Proc Natl Acad Sci. 2022;119(20): e2118312119.
Leen AM, Bollard CM, Mendizabal AM, et al. Multicenter study of banked third-party virus-specific T cells to treat severe viral infections after hematopoietic stem cell transplantation. Blood, J Am Soc Hematol. 2013;121(26):5113–23.
Smith C, Beagley L, Rehan S, et al. Autologous adoptive T-cell therapy for recurrent or drug-resistant cytomegalovirus complications in solid organ transplant recipients: a single-arm open-label phase I clinical trial. Clin Infect Dis. 2019;68(4):632–40.
Muftuoglu M, Olson A, Marin D, et al. Allogeneic BK virus–specific T cells for progressive multifocal leukoencephalopathy. N Engl J Med. 2018;379(15):1443–51.
Martits-Chalangari K, Spak CW, Askar M, et al. ALVR109, an off-the-shelf partially HLA matched SARS-CoV-2–specific T cell therapy, to treat refractory severe COVID-19 pneumonia in a heart transplant patient: case report. Am J Transplant. 2022;22(4):1261–5.
Haidar G, Jacobs J, Hughes K, McCormick K, Naqvi A, Agha M, Bogdanovich T, Johnson B, Kozar J, Lendermon E, Marino C, Raptis A, Silveira F, Marshall W, Miller M, Atillasoy E, Mellors J. Early clinical experience with Alvr109, a partially Hla-matched Sars-cov-2 specific T-cell therapy, in immunocompromised patients with COVID-19. Am J Transplant. 2022;22(suppl 3):598–9.
Houghtelin A, Bollard CM. Virus-specific T cells for the immunocompromised patient. Front Immunol. 2017;8:1272.
Geers D, Shamier MC, Bogers S, et al. SARS-CoV-2 variants of concern partially escape humoral but not T cell responses in COVID-19 convalescent donors and vaccine recipients. Sci Immunol. 2021;6(59):eabj1750.
U.S. Food and Drug Administration. FDA authorizes revisions to Evusheld dosing. https://www.fda.gov/drugs/drug-safety-and-availability/fda-authorizes-revisions-evusheld-dosing. Accessed 7/19/, 2022.
Bradley RE, Ponsford MJ, Scurr MJ, Godkin A, Jolles S. Persistent COVID-19 infection in Wiskott-Aldrich syndrome cleared following therapeutic vaccination: a case report. J Clin Immunol. 2022;42(1):32–5.
Heitmann JS, Bilich T, Tandler C, et al. A COVID-19 peptide vaccine for the induction of SARS-CoV-2 T cell immunity. Nature. 2022;601(7894):617–22.
van Laarhoven A, Kurver L, Overheul GJ, et al. Interferon gamma immunotherapy in five critically ill COVID-19 patients with impaired cellular immunity: a case series. Med. 2021;2(10):1163-1170. e2.
Horiuchi H, Sasaki H, Miyazaki K, Miyata N, Yoshimura Y, Tachikawa N. Recovery from severe persistent COVID-19 without evidence of an anti-SARS-CoV-2 antibody response in a man with mantle cell lymphoma treated with rituximab. J Infect Chemother. 2022;28(2):329–32.
Xiao AT, Tong YX, Zhang S. Profile of RT-PCR for SARS-CoV-2: a preliminary study from 56 COVID-19 patients. Clin Infect Dis. 2020;71(16):2249–51.
Tom MR, Mina MJ. To interpret the SARS-CoV-2 test, consider the cycle threshold value. Clin Infect Dis. 2020;71(16):2252–4.
Infectious Diseases Society of America. IDSA and AMP joint statement on the use of SARS-CoV-2 PCR cycle threshold (Ct) values for clinical decision-making. https://www.idsociety.org/globalassets/idsa/public-health/covid-19/idsa-amp-statement.pdf.
Jacobs JL, Bain W, Naqvi A, et al. Severe acute respiratory syndrome coronavirus 2 viremia is associated with coronavirus disease 2019 severity and predicts clinical outcomes. Clin Infect Dis. 2022;74(9):1525–33.
Jacobs JL, Naqvi A, Shah FA, et al. Plasma SARS-CoV-2 RNA levels as a biomarker of lower respiratory tract SARS-CoV-2 infection in critically ill patients with COVID-19. J Infect Dis. 2022; https://doi.org/10.1093/infdis/jiac157. Online ahead of print.
Li Y, Schneider AM, Mehta A, et al. SARS-CoV-2 viremia is associated with distinct proteomic pathways and predicts COVID-19 outcomes. J Clin Invest. 2021;131(13): e148635.
Razonable RR, Humar A. Cytomegalovirus in solid organ transplant recipients—guidelines of the American Society of Transplantation Infectious Diseases Community of Practice. Clin Transplant. 2019;33(9): e13512.
Pérez-Lago L, Aldámiz-Echevarría T, García-Martínez R, et al. Different within-host viral evolution dynamics in severely immunosuppressed cases with persistent SARS-CoV-2. Biomedicines. 2021;9(7):808.
Haidar G, Mellors JW. Improving the outcomes of immunocompromised patients with coronavirus disease 2019. Clin Infect Dis. 2021;73(6):e1397–401.
Killingley B, Mann AJ, Kalinova M, et al. Safety, tolerability and viral kinetics during SARS-CoV-2 human challenge in young adults. Nat Med. 2022;28(5):1031–41.
Phillips SP, Wei X, Kwong JC, et al. Duration of SARS-CoV-2 shedding: a population-based, Canadian study. PLoS One. 2021;16(6): e0252217.
Centers for Disease Control and Prevention. Ending isolation and precautions for people with COVID-19: interim guidance. https://www.cdc.gov/coronavirus/2019-ncov/hcp/duration-isolation.html.
Centers for Disease Control and Prevention. Interim infection prevention and control recommendations for healthcare personnel during the coronavirus disease 2019 (COVID-19) pandemic. 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html. Accessed 7/12/2022
Pickering S, Batra R, Merrick B, et al. Comparative performance of SARS-CoV-2 lateral flow antigen tests and association with detection of infectious virus in clinical specimens: a single-centre laboratory evaluation study. Lancet Microbe. 2021;2(9):e461–71.
Garneau WM, Liang T, Wang K, et al. Clinical outcomes of patients previously treated with B-cell depletion therapy hospitalized with COVID-19: results from the Johns Hopkins Crown Registry. Available at SSRN 4030554. 2022.
Koval CE, Poggio ED, Lin Y, Kerr H, Eltemamy M, Wee A. Early success transplanting kidneys from donors with new SARS-CoV-2 RNA positivity: a report of 10 cases. American Journal of Transplantation. 2021.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
V.D. has no disclosures or COI. S.S-A. is recipient of Fulbright Grant and IMFAHE Foundation Excellence Fellowship Grant. V.D. is an investigator for Regeneron Pharmaceuticals and AlloVir. G.H. is a recipient of research grants from Allovir, Karius, and AstraZeneca. G.H. also serves on the scientific advisory board of Karius.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on COVID-19 and Transplantation
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dioverti, V., Salto-Alejandre, S. & Haidar, G. Immunocompromised Patients with Protracted COVID-19: a Review of “Long Persisters”. Curr Transpl Rep 9, 209–218 (2022). https://doi.org/10.1007/s40472-022-00385-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40472-022-00385-y