Abstract
Purpose of Review
The intended goal of this paper is to review current indications, available devices, and future directions of total artificial heart therapies. Throughout the paper, we sought to help clinicians identify appropriate patients who might be considered for total artificial heart therapy, highlighting the most current data regarding outcomes and adverse events.
Recent Findings
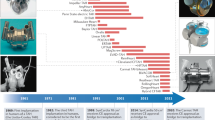
The INTERMACS report on the total artificial heart has recently been published in the Journal of Heart and Lung Transplantation and represents the largest study to date on available TAH therapies. Notable findings include better outcomes at experienced centers, likely a result of appropriate patient selection, timing, and management of device therapy.
Summary
There are multiple new types of total artificial hearts under development. Having learned from prior experience, and with increasing use and standardization of peri- and post-operative management, there is hope of ongoing success in improving care for those with advanced heart disease and biventricular failure with the use of this technology.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Cooley DA, Liotta D, Hallman GL, Bloodwell RD, Leachman RD, Milam JD. Orthotopic cardiac prosthesis for two-staged cardiac replacement. Am J Cardiol. 1969;24(5):723–30.
Cooley DA, Akutsu T, Norman JC, Serrato MA, Frazier OH. Total artificial heart in two-staged cardiac transplantation. Cardiovasc Dis. 1981;8(3):305–19.
Jarvik RK. The total artificial heart. Sci Am. 1981;244(1):74–80.
DeVries WC, Anderson JL, Joyce LD, Anderson FL, Hammond EH, Jarvik RK, et al. Clinical use of the total artificial heart. N Engl J Med. 1984;310(5):273–8. https://doi.org/10.1056/NEJM198402023100501.
DeVries WC. The permanent artificial heart. Four case reports. JAMA. 1988;259(6):849–59.
Copeland JG, Levinson MM, Smith R, Icenogle TB, Vaughn C, Cheng K, et al. The total artificial heart as a bridge to transplantation. A report of two cases. JAMA. 1986;256(21):2991–5.
Carpentier A, Latremouille C, Cholley B, Smadja DM, Roussel JC, Boissier E, et al. First clinical use of a bioprosthetic total artificial heart: report of two cases. Lancet. 2015;386(10003):1556–63. https://doi.org/10.1016/S0140-6736(15)60511-6.
Kleinheyer M, Timms DL, Greatrex NA, Masuzawa T, Frazier OH, Cohn WE. Pulsatile operation of the BiVACOR TAH - motor design, control and hemodynamics. Conf Proc IEEE Eng Med Biol Soc. 2014;2014:5659–62. https://doi.org/10.1109/EMBC.2014.6944911.
Pelletier B, Spiliopoulos S, Finocchiaro T, Graef F, Kuipers K, Laumen M, et al. System overview of the fully implantable destination therapy--ReinHeart-total artificial heart. Eur J Cardiothorac Surg. 2015;47(1):80–6. https://doi.org/10.1093/ejcts/ezu321.
Kobayashi M, Horvath DJ, Mielke N, Shiose A, Kuban B, Goodin M, et al. Progress on the design and development of the continuous-flow total artificial heart. Artif Organs. 2012;36(8):705–13. https://doi.org/10.1111/j.1525-1594.2012.01489.x.
Glynn J, Song H, Hull B, Withers S, Gelow J, Mudd J, et al. The OregonHeart total artificial heart: design and performance on a mock circulatory loop. Artif Organs. 2017;41(10):904–10. https://doi.org/10.1111/aor.12959.
Abe Y, Isoyama T, Saito I, Inoue Y, Ishii K, Sato M, et al. Animal experiments of the helical flow total artificial heart. Artif Organs. 2015;39(8):670–80. https://doi.org/10.1111/aor.12543.
Wells D, Villa CR, Simon Morales DL. The 50/50 cc total artificial heart trial: extending the benefits of the total artificial heart to underserved populations. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. 2017;20:16–9. https://doi.org/10.1053/j.pcsu.2016.09.004.
Copeland JG, Copeland H, Gustafson M, Mineburg N, Covington D, Smith RG, et al. Experience with more than 100 total artificial heart implants. J Thorac Cardiovasc Surg. 2012;143(3):727–34. https://doi.org/10.1016/j.jtcvs.2011.12.002.
Jaroszewski DE, Anderson EM, Pierce CN, Arabia FA. The SynCardia freedom driver: a portable driver for discharge home with the total artificial heart. J Heart Lung Transplant. 2011;30(7):844–5. https://doi.org/10.1016/j.healun.2011.03.014.
Dowling RD, Gray LA Jr, Etoch SW, Laks H, Marelli D, Samuels L, et al. Initial experience with the AbioCor implantable replacement heart system. J Thorac Cardiovasc Surg. 2004;127(1):131–41. https://doi.org/10.1016/j.jtcvs.2003.07.023.
Latremouille C, Carpentier A, Leprince P, Roussel JC, Cholley B, Boissier E, et al. A bioprosthetic total artificial heart for end-stage heart failure: results from a pilot study. J Heart Lung Transplant. 2018;37(1):33–7. https://doi.org/10.1016/j.healun.2017.09.002.
Cohn WE, Arabia F, Timms DL, Greatrex N, Kleinheyer M, Nestler F, et al. (12) - Pulsatile outflow in cows supported long-term with the BiVACOR Rotary TAH. J Heart Lung Transplant. 2017;36(4, Supplement):S14. https://doi.org/10.1016/j.healun.2017.01.023.
Arabia FA, Moriguchi JD. Machines versus medication for biventricular heart failure: focus on the total artificial heart. Futur Cardiol. 2014;10(5):593–609. https://doi.org/10.2217/fca.14.47.
Kormos RL, Teuteberg JJ, Pagani FD, Russell SD, John R, Miller LW, et al. Right ventricular failure in patients with the HeartMate II continuous-flow left ventricular assist device: incidence, risk factors, and effect on outcomes. J Thorac Cardiovasc Surg. 2010;139(5):1316–24. https://doi.org/10.1016/j.jtcvs.2009.11.020.
Copeland JG 3rd, Smith RG, Arabia FA, Nolan PE, Mehta VK, MS MC, et al. Comparison of the CardioWest total artificial heart, the novacor left ventricular assist system and the thoratec ventricular assist system in bridge to transplantation. Ann Thorac Surg. 2001;71(3 Suppl):S92–7. discussion S114–5
Kirklin JK, Pagani FD, Kormos RL, Stevenson LW, Blume ED, Myers SL, et al. Eighth annual INTERMACS report: special focus on framing the impact of adverse events. J Heart Lung Transplant. 2017;36(10):1080–6. https://doi.org/10.1016/j.healun.2017.07.005.
Raina A, Patarroyo-Aponte M. Prevention and treatment of right ventricular failure during left ventricular assist device therapy. Crit Care Clin. 2018;34(3):439–52. https://doi.org/10.1016/j.ccc.2018.03.001.
• Morine KJ, Kiernan MS, Pham DT, Paruchuri V, Denofrio D, Kapur NK. Pulmonary artery pulsatility index is associated with right ventricular failure after left ventricular assist device surgery. J Card Fail. 2016;22(2):110–6. https://doi.org/10.1016/j.cardfail.2015.10.019. This represents an important paper because it compares various methods of evaluation of RV function which is critical for appropriate TAH patient selection.
•• Arabia FA, Cantor RS, Koehl DA, Kasirajan V, Gregoric I, Moriguchi JD, et al. Interagency registry for mechanically assisted circulatory support report on the total artificial heart. J Heart Lung Transplant. 2018. https://doi.org/10.1016/j.healun.2018.04.004. This is a very important paper because it represents the largest evaluation of TAH therapy to date, with key findings including outcomes and adverse events.
• Gohar S, Taimeh ZA, Morgan JA, Frazier OH, AA F, Civitello AB, et al. Use of remote pulmonary artery pressure monitoring (CardioMEMS System) in total artificial heart to assess pulmonary hemodynamics for heart transplantation. ASAIO J. 2018;64(4):e75–e7. https://doi.org/10.1097/MAT.0000000000000726. This paper highlights the use of PA pressure monitoring systems prior to TAH implantation, which may be of particular importance in helping manage patients and for monitoring PA pressures for suitability for heart transplantation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Francisco Arabia is a survival trainer for SymCardia and a consultant for Carmat and Bivacor. Robert Cole declares no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Thoracic Transplantation
Rights and permissions
About this article
Cite this article
Cole, R.M., Arabía, F.A. Total Artificial Heart Technology: Where Are We Now?. Curr Transpl Rep 5, 315–318 (2018). https://doi.org/10.1007/s40472-018-0211-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40472-018-0211-z