Abstract
Naloxone is a well-established essential medicine for the treatment of life-threatening heroin/opioid overdose in emergency medicine. Over two decades, the concept of ‘take-home naloxone’ has evolved, comprising pre-provision of an emergency supply to laypersons likely to witness an opioid overdose (e.g. peers and family members of people who use opioids as well as non-medical personnel), with the recommendation to administer the naloxone to the overdose victim as interim care while awaiting an ambulance. There is an urgent need for more widespread naloxone access considering the growing problem of opioid overdose deaths, accounting for more than 100,000 deaths worldwide annually. Rises in mortality are particularly sharp in North America, where the ongoing prescription opioid problem is now overlaid with a rapid growth in overdose deaths from heroin and illicit fentanyl. Using opioids alone is dangerous, and the mortality risk is clustered at certain times and contexts, including on prison release and discharge from hospital and residential care. The provision of take-home naloxone has required the introduction of new legislation and new naloxone products. These include pre-filled syringes and auto-injectors and, crucially, new concentrated nasal sprays (four formulations recently approved in different countries) with speed of onset comparable to intramuscular naloxone and relative bioavailability of approximately 40–50%. Choosing the right naloxone dose in the fentanyl era is a matter of ongoing debate, but the safety margin of the approved nasal sprays is superior to improvised nasal kits. New legislation in different countries permits over-the-counter sales or other prescription-free methods of provision. However, access remains uneven with take-home naloxone still not provided in many countries and communities, and with ongoing barriers contributing to implementation inertia. Take-home naloxone is an important component of the response to the global overdose problem, but greater commitment to implementation will be essential, alongside improved affordable products, if a greater impact is to be achieved.
Similar content being viewed by others
Take-home naloxone is an effective public health intervention to prevent deaths and organ damage from opioid overdose. |
Four naloxone nasal spray products that have been developed for layperson use are now approved, all with approximately 40–50% bioavailability relative to parenteral references. They are increasingly available in clinical practice in a growing number of countries |
Ongoing implementation challenges include naloxone cost as well as politico-social (e.g. stigma) and legal barriers (e.g. prescription status), although prescription-free distribution is now permitted in several countries (e.g. Australia, Canada, Italy, the UK). |
1 Introduction
With an increasing global problem of opioid use and dependence, the mortality rate from opioid overdose continues to rise, and there are more than 100,000 deaths globally per annum [1]. Heroin is the most common drug involved in opioid overdose in much of the world, although prescription drugs and illicitly manufactured fentanyl (IMF) and analogues are increasingly implicated, particularly in North America. In the USA, 20,000 deaths from prescription opioids and 13,000 deaths from heroin were registered in 2015 alone [2].
These deaths occur primarily in the community and, while sometimes the patient is alone, he/she often in the presence of others (especially with heroin overdose) [3,4,5,6]. As such, these deaths are potentially preventable with timely detection and administration of naloxone, along with wider resuscitation measures, by non-medical members of the general public.
Naloxone is a remarkable antidote that is opioid specific and actively displaces heroin and other opioids from the mu-opioid receptor (MOR). It is a long-established medicine that is essential in the hospital emergency department and the ambulance medication kit. Naloxone administration reverses heroin/opioid overdose within minutes with rapid re-establishment of independent breathing and return of consciousness (and, in individuals who are dependent on opioids, risk of precipitation of an opioid withdrawal syndrome).
‘Take-home naloxone’ (THN) for the reversal of heroin/opioid overdose involves the pre-provision of an emergency naloxone kit, to non-medical persons along with training in basic overdose management, naloxone administration and after-care. The concept of THN constitutes an example of technology transfer, in that it tells us to take the solution (emergency naloxone kit) from the hospital into the community where the emergency (overdose) occurs, with the aim to reduce any harm (i.e. potential death) that could occur during the time delay while awaiting the arrival of an ambulance. This follows the example of technology transfer for other medical emergencies, such as diabetic coma or severe anaphylactic reactions, where potentially life-saving medicines (adrenalin/epinephrine, glucagon, snake anti-venom) are also pre-provided to the at-risk patient or individual, along with instructions to family members.
‘Take-home naloxone’ may be provided as part of comprehensive clinical care of patients in treatment for opioid use disorder in primary or specialty care or through dedicated THN schemes. Researchers have found that both peers and family members are highly willing to act as first responders providing interim emergency care whilst awaiting the arrival of ambulance (or other emergency medical care) [7, 8].
Support for THN has increased greatly in recent years, including guidelines from the World Health Organization [9] and endorsement from the United Nations [10], as well as from various national governments. Nevertheless, intervention inertia around THN continues to exist, with countries, services and clinicians uncertain what they can, or cannot, provide. In the meantime, lives continue to be lost, including in situations where the overdose victim was still alive at the point of discovery (and therefore death was likely preventable).
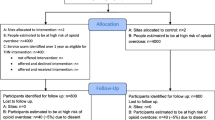
In this review, we provide the reader with the evidence for THN as a public health response to opioid overdose as well as presenting evidence on naloxone’s properties and the recent development of novel naloxone formulations and devices for layperson use as well as exploring ongoing challenges for implementation. To achieve a balanced reflection of the wider developments in the field of THN, we have deliberately brought together a team of co-authors with different areas of expertise who have led on the sections of this review. This paper draws on peer-reviewed and grey literature identified through a desk-based review of THN and naloxone formulations. English-language peer-reviewed literature was identified through searches of MEDLINE, EMBASE (via the OVID platform) and PubMed. Given the wide scope of this review, search terms included opioids, opiates, overdose, mortality, prevention, naloxone, intranasal (IN) and nasal. This general search strategy was then adapted by our co-authors to meet the specific focus of their respective section(s). Key literature (including grey literature) cited within the retrieved material was also consulted, and as a general principle, more recent literature was preferred over older data (1960–2009). Data from published papers and reports were extracted and synthesised as narrative reviews. We also refer the interested reader to earlier reviews with a more limited focus, including THN programmes [11, 12] and naloxone delivery systems [13, 14].
1.1 Structure
Sections 2 and 3 discuss the prevalence of opioid mortality and situational risk factors for overdose. Section 4 describes the discovery of naloxone and history of its use in medical practice as background for Sect. 5, which covers the study of pharmacokinetics and development of non-injectable formulations of naloxone. This is followed by a discussion of the pharmacodynamics of naloxone and its efficacy and safety for the emergency management of opioid overdose in Sect. 6. In Sects. 7 and 8, we review the effectiveness of THN and ongoing implementation barriers, leading up to concluding remarks in Sect. 9.
2 Epidemiology of Opioid Overdose Deaths
To understand the levels and variations in opioid overdose deaths, it is important to understand one of the important drivers in high-income countries, namely, prescription opioid utilisation [15]. North America, Oceania and some western European countries account for more than 95% of the worldwide consumption of analgesic opioids [15], as illustrated in Fig. 1, despite accounting for only about 15% of the world’s population [15].
Mean availability of opioids for pain management in 2011–2013 (Source: [15]). S-DDD defined daily doses for statistical purposes
2.1 USA
2.1.1 Increasing Opioid Prescribing
The USA had a substantial increase in opioid prescribing for chronic non-cancer pain [16], with opioid analgesic use in North America rising from about 2.4 billion DDD (defined daily dose; i.e. “the assumed average maintenance dose per day for a drug used for its main indication in adults”)Footnote 1 per annum in 2001–2003 to about 5.3 billion DDD per annum in 2011–2013 [15].
In recent years, a number of policies have been introduced to reduce the problem of excessive opioid prescribing [17]. These have included educating professionals and the general public about appropriate prescription opioid use, implementation of prescription drug monitoring programmes, attempts to reduce egregious prescribing (by so-called “pill mills”—clinics devoted entirely to opioid prescribing) and developing novel abuse-deterrent opioid formulations. Despite an overall reduction in per capita prescribing since 2010, the oral morphine equivalent amount prescribed in 2015 was still approximately three times as high as in 1999 [18]. The unintended consequences of these supply-side interventions need to be considered. With access reduced and demand still high, individuals began to turn to the black market [19].
2.1.2 Increasing Opioid-Related Overdoses
The rise in opioid analgesic use in the USA has been associated with substantial increases in non-fatal and fatal overdose. Since 2000, there has been a steady increase in the rate of opioid overdose deaths (see Fig. 2). From 1999 to 2015, more than 183,000 people died from overdoses related to prescription opioids. In 2016 alone, there were over 63,000 drug-related deaths, of which 66% involved opioids (either prescription or illicit). In fact, the escalation in opioid overdose deaths has been a significant factor in reduced US life expectancy in 2015 and 2016, particularly for white Americans [20].
2.1.3 Re-emergence and Increase of Heroin Use
Despite concerted public health efforts to reduce opioid prescribing (see above), opioid-related deaths continued to increase by 16% from 2014 to 2015 [18]. These significant increases in mortality were largely driven by opioids other than methadone, predominantly IMF (see below) and heroin [21].
A population-based study reported that the prevalence of heroin use increased from 0.3% in 2001–2002 to 1.6% in 2012–2013 [22], and heroin-related overdose increased from 1842 deaths in 2000 to 10,574 deaths in 2014 [17] (see Fig. 2). The increased availability of high-purity heroin combined with its low price (compared with diverted prescription opioids) have been major drivers of the upward trends in heroin use and overdose deaths [21]. Nonmedical use of prescription opioids is considered a significant risk factor for heroin use [17].
2.1.4 Increasing Availability of Potent Illicit Opioids
In recent years, deaths from illicit synthetic opioids have outstripped deaths due to heroin and prescribed opioids in the USA. In 2015, the Drug Enforcement Administration and Centers for Disease Control and Prevention issued nationwide alerts identifying IMF as a threat [23].
Illicitly manufactured fentanyl and its analogues are significantly more potent than morphine: carfentanil, for example, is approximately 10,000 times more potent, gram for gram. Fentanyl is more likely to lead to overdose than other opioids and is thought to have reduced cross-tolerance to other opioids [24]. A much smaller dose of fentanyl than heroin is required to achieve the same drug effect: thus errors at the level of the illicit manufacture and distribution, as well as errors at the level of the end user, result in frequent accidental errors of dosage whose implications are far more profound than errors where the dose alteration is less severe [24]. The high potency of fentanyl makes it often both cheaper and easier to trade (and access) than heroin given its much smaller bulk [19, 25]. Illicitly manufactured fentanyl is also increasingly found as adulterant in non-opioid drugs (e.g. cocaine) and considered a key factor for the more recent increases in opioid overdose mortality [21, 25, 26] (see Fig. 2).
In Massachusetts (2014–2016), 36% of fentanyl deaths had evidence of an overdose occurring within seconds to minutes after drug use, and 90% of fentanyl overdose decedents were pulseless upon emergency medical services (EMS) arrival [27]. It has been speculated whether massive overdoses are able to benefit from naloxone at all [28].
Fentanyl and its analogues differ from many other opioids by their propensity to induce muscle rigidity [29], including chest wall rigidity (sometimes called ‘wooden chest syndrome’), which makes assisted ventilation and breathing difficult [24] and may increase mortality risk and lead to rapid death [30]. Notably, muscle rigidity can be reversed by naloxone [30, 31]. Therefore, the same principles of response with THN initiatives apply to the prevention of deaths from fentanyl overdose, although early administration of naloxone is likely crucial.
2.2 Canada
Canada has the second highest level of prescribed opioid use globally after the USA, and consumption is increasing faster than in the USA, with a 203% increase from the 2-year period of 2000–2002 (8713 defined daily doses for statistical purposesFootnote 2) to 2008–2010 (26,380 defined daily doses for statistical purposes) [15]. From 1991 to 2004, annual prescriptions for opioids increased from 458 to 591 per 1000 individuals [32], with opioid-related deaths doubling, from 13.7 to 27.2 per million in 2004. There are also recent indications of the use of IMF and analogues and associated overdoses [33], localised to certain provinces, such as British Columbia and Alberta [33].
2.3 Europe
Although pharmaceutical opioid use is increasing gradually in Western Europe, the prevalence is four times lower than in North America [34]. In general, heroin remains the most prevalent illicit opioid in Europe. However, in some countries, such as Estonia and Finland, where the heroin market plummeted in the early 2000s, heroin has been entirely displaced by fentanyl (mostly illicit) and buprenorphine, respectively [35].
In 2015, there were 8440 drug overdose deaths (any substance; occurring most commonly in the UK, followed by Germany and Sweden) in the European Union (plus Turkey and Norway), a total that continues to rise [36]. Most drug-related deaths (79%) involved opioids, predominantly heroin, though potent synthetic opioids such as fentanyl and its newer derivatives seem to play an increasing role [37]. For example, in Estonia there was a spike in overdose deaths in 2012 that was mainly attributable to fentanyl. On the European boundary, there have also been reports of fentanyl use in parts of Russia owing to heroin shortages. Of the 9263 drug-related deaths reported in Russia in 2010, 6324 were attributed to opioid use [38]. (N.B.: Comparisons across different countries are hampered by differences in data collection [39]).
2.4 Australia
In Australia, annual opioid analgesic use increased from 23 million DDD in 2001–2003 to 106 million DDD in 2011–2013 [15]. In 2016, there were 1045 opioid-related deaths in Australia, accounting for approximately 75% of all drug-related deaths [40]. Whilst the rate of heroin-related deaths has remained stable, overdose deaths from prescription opioids are now more common, having increased by 127% from 2006 to 2016 [40]. Deaths related to synthetic opioids (fentanyl, tramadol and pethidine, excluding methadone) have also been increasing, from approximately 5% (1999) to 17% (2016) of opioid-related deaths [40].
3 Clusters of Deaths and Crucial At-Risk Populations
Various factors are associated with increased risk of overdose death in people who use opioids (PWUO). These include individual and behavioural risk factors, such as male sex, older age, intravenous (IV) use, co-administration of other sedative drugs (e.g. benzodiazepines, alcohol), and irregular patterns of use (probably due to variability of dose) [41]. Sadly, many overdose deaths conform to Hans Fallada’s book title “Every Man Dies Alone”, as a significant number (approximately 30%) of opioid overdose fatalities happens when the drug is taken in the absence of other people [42]. It is also a serious problem that that those around the individual often do not understand that the victim is not sleeping, but in imminent danger from an overdose [27].
Different types of opioid overdose victims die at different times after injection. In heroin overdose, the time course of opioid metabolites in post-mortem cases indicated that most victims stayed alive for more than 30 min, indicating a window for intervention within at least this time frame [43, 44]. However, in 44% of the 145 fatal cases, signs of rapid-onset collapse were also observed. The time frame for intervention may nevertheless be shorter with fentanyl overdoses, as anecdotal reports of immediate deaths in 14 subjects with needle/tourniquet in place (along with characteristic fentanyl/metabolite ratios) suggest [45]. In the case of immediate deaths from fentanyl or heroin, it is possible that these may not be secondary to respiratory depression, but rather the direct effect of primary cardiovascular collapse in susceptible undernourished and dehydrated individuals.
Situational factors are important, with the prison release population identified as a particularly high-risk group. For prisoners with a previous history of heroin use by injection, one in 200 will be dead within a fortnight of their release from prison, with most deaths being caused by opioid overdose [46,47,48]. These deaths likely occur during post-release deliberate intoxication, where, following a period of abstinence and consequent loss of tolerance, a previously regular dose may now lead to fatal overdose.
A similar clustering of deaths is seen after discharge from hospital or abstinence-based residential rehabilitation [49, 50], and the explanation is likely similar. In addition, those in abstinence-based outpatient treatment are at increased risk if they then relapse [51].
The importance of this clustering characteristic is that it should direct both policymakers and clinicians to points of transition in care and setting that would benefit from preventive measures and emergency interventions, including THN. The target population for THN crucially also includes PWUO who are outside the treatment system. We need to remember that treatment markedly reduces the risk of overdose death.
A different type of clustering is seen with outbreaks of overdose deaths in communities, which occur with the presumed arrival and distribution of a particularly potent batch of heroin or contaminated supply (e.g. with added fentanyl). Certainly, this accounts for some of the clusters of deaths, but it is unclear why this does not then lead to modification of drug-taking behaviour (e.g. avoiding this supply, or taking a smaller dose), and it is likely that other factors, as yet unidentified, lie behind some of these time-limited geographical clusters.
4 History of Naloxone for the Emergency Management of Opioid Overdose
4.1 Initial Development and Testing (1960s)
Naloxone (N-alyllnoroxy-morphone) hydrochloride (CAS Number: 357-08-4) was first synthesised from thebaine in New York in 1960 by Dr. Jack Fishman and Dr. Mozes J. Lewenstein, whose patent described naloxone as a “more potent antagonist to the respiratory depressive effects of potent analgesics than the antagonists hitherto known” [52, 53]. Its molecular formula is C19H21NO4HCl (molecular weight 363). Naloxone hydrochloride is a white-to-slightly-off-white powder and is soluble in water, dilute acids and strong alkali. It is slightly soluble in alcohol and practically insoluble in ether and chloroform. Naloxone has a fat-water partition coefficient 20 times that of morphine and similar to meperidine. Its pKaFootnote 3 is 7.94 [54]. The chemical structure of naloxone is shown in Fig. 3.
4.2 Entry into Clinical Practice (1970s Onwards)
The US Food and Drug Administration (FDA) approved naloxone in 1971 as a prescription-only medication for intravenous (IV), intramuscular (IM) and subcutaneous administration for reversing the effects of opioids. Naloxone entered international clinical practice in the following years and was included as a specific antidote (i.e. in the formulation of 0.4 mg in 1-mL ampoules) in the World Health Organization’s Model List of Essential Medicines in 1983 [55, 56]. Owing to its unique effectiveness and safety profile, naloxone has become the treatment of choice for reversing opioid overdose in hospital emergency departments and ambulance services.
4.3 Community-Based Naloxone (1990s)
The first serious consideration of THN occurred in a 1996 BMJ editorial [57], which described how emergency naloxone kits could be pre-provided for emergency use to the following groups:
-
1.
individuals at high risk of overdose, e.g. those leaving emergency care following overdose and those who lost tolerance as a result of detoxification, incarceration or abstinence-based treatment;
-
2.
patients enrolled in treatment programmes; and
-
3.
active users.
People who use opioids were described as the primary target group for THN because they are at risk of future overdose themselves and highly likely to be in a position to intervene in someone else’s overdose. Indeed, PWUO voiced strong support of THN provision. A London-based survey of PWUO [7] estimated that two thirds of witnessed overdose deaths could have been avoided with THN, and nearly 90% of respondents who had witnessed an overdose stated that they would have used the medication had it been available. Subsequent studies identified the willingness of PWUO [58, 59] and family members [8] to be trained in overdose management and naloxone administration.
Early implementation of THN was made possible through user advocates working with physicians willing to prescribe naloxone despite medicolegal uncertainty or explicit barriers. Take-home naloxone provision first occurred in the late 1990s and early 2000s, in the USA (Chicago, San Francisco), Germany (Berlin), the UK (Jersey) and Italy (Turin, Bologna, Padua) [60,61,62,63,64,65,66,67,68,69]. The identification of legal pathways for THN provision from the mid-2000s onwards facilitated the introduction of first national and state-wide programmes in parts of Europe and USA.
5 Pharmacokinetics and the Development of New Non-injectable Naloxone
5.1 Notion of Non-injectable Formulations: Potential for more Acceptable Implementation
Because injectable naloxone was not developed for layperson use, non-injectable naloxone formulations have been considered to have several implementation advantages for THN programmes. First, injectable medications are intimidating for laypersons to use [70] and present logistical barriers: they require product assembly (e.g. needle and syringe) and training in administration. Surprisingly, even among experienced PWUO, nearly three out of four (74%) preferred naloxone nasal spray to injectable devices [71]. Second, with use of naloxone by injection, there is the risk of needle-stick injury. Third, non-injectable naloxone could likely overcome regulatory obstacles (e.g. prescription-only status for injectable medications) and be provided to a wider workforce (e.g. hostel staff, outreach workers, police).
5.2 Routes of Administration
Naloxone was originally developed and FDA approved as an injectable formulation for use by medical professionals (see above). The IV route requires skilled personnel and takes time to establish. Intramuscular is now the widely preferred parenteral route because IV carries a greater risk of exposure to contaminated blood as well as risks of withdrawals and potential aggression. Intranasal is the simplest and fastest procedure, and it circumvents the contamination hazard. While IV provides by far the most rapid and reliable response when measured from the time of administration, IM comes as a good second, followed closely by IN (see Table 1). However, when time from contact with the patient is the starting point in the emergency situation, IN [72] and subcutaneous [73] have been found to be as fast as IV. A potential shortcoming with the IN route is that effective uptake may be reduced by septal abnormalities, bleeding, nasal mucous, trauma and use of nasal vasoconstrictors [74].
5.3 Improvised Nasal Naloxone Kits
In the absence of licensed non-injectable naloxone formulations, ‘improvised’ nasal kits (i.e. a 2-mg/2-mL pre-filled syringe with a nasal mucosal atomizer device [MAD] attached) were being distributed by some North American THN programmes from 2006 onwards (and later also in parts of Scandinavia and Scotland), despite not having been formally tested for safety or efficacy. This followed their use by EMS as well as fire fighters and police officers. (The safety of use of the improvised kits in medical practice is discussed in more detail in Sect. 6.6.)
These ‘improvised’ kits were used in many successful overdose reversals, and reports of problems using the kits were uncommon [75, 76]. For instance, in Norway, just over 2000 ‘improvised’ THN kits were distributed in 2014–2015, with 277 reports of successful reversals [77, 78].
However, concern was expressed about the reliance on such improvised nasal sprays because the naloxone concentration in the spray was dilute (1 mg/mL) [79]. Specifically, given the existence of licensed injectable products, the question was raised [79] whether it was acceptable for clinicians to supply unlicensed improvised nasal naloxone kits for take-home use, where no back-up of injectable naloxone would be available in the case of non-response (unlike the ambulance or hospital setting). This stirred a challenging debate among international experts in the field [80, 81].
Subsequent examination of patent records located data confirming only poor bioavailability (approximately 10% of dose administered) [82] and recent direct pharmacokinetic comparison of the improvised kits vs. the new concentrated naloxone nasal spray formulations found bioavailability of only approximately 20% with the improvised kits vs. more than 40% with the new concentrated naloxone sprays [83]. Nevertheless, the evident successful reversals of opioid overdoses with these improvised kits [75,76,77] should raise questions about the dose necessary for layperson reversal which, in these instances, appears to have been achieved with much lower absorbed concentrations of naloxone.
5.4 Regulatory Criteria for the Development of Non-injectable Naloxone Products
In response to rising overdose mortality rates, the US FDA, Centers for Disease Control and Prevention, National Institute on Drug Abuse, and Office of the Assistant Secretary for Health and Human Services sponsored a stakeholder meeting in 2012 to encourage the development of non-injectable naloxone products suitable for layperson use in community-based settings. Following the meeting, the National Institute on Drug Abuse announced that it would provide funding for the development of user-friendly naloxone devices (i.e. IN rather than injection) [84].
The key regulatory criteria for any New Drug Application [85, 86] involved that naloxone would need to be absorbed into the bloodstream rapidly, given the emergency situation, and in a quantity sufficient to effect quick reversal of opioid-induced respiratory depression. The reference for any candidate non-injectable product would be injectable naloxone, administered by the licensed IM, IV and subcutaneous routes [9].
5.4.1 Identification of Candidate Routes of Administration for Non-injectable Products
Naloxone has a very low oral and rectal bioavailability of 1–2% and 15%, which makes these routes unsuitable for emergency naloxone [87]. Strang et al. [88] thus explored candidate routes of administration for THN use. Only the transmucosal routes IN, buccal and sublingual met the required characteristics. Transmucosal uptake bypasses first-pass hepatic elimination. Among these three routes, approved products only exist for IN administration (see below). In the following section, we describe the pharmacokinetics of injectable naloxone as the reference for the development of non-injectable products.
5.5 Naloxone Pharmacokinetics
Naloxone is rapidly and extensively metabolised mainly by glucuronidation to the inactive compound naloxon-3-glucuronide (N3G) thought to be primarily by the liver at that time [89]. Ngai et al. [90] and Berkowitz [91] reported initial distribution and terminal half-lives of 4 and 64 min. Recent pharmacokinetic studies [92,93,94,95] confirmed terminal elimination half-lives of 60–120 min after IV administration of 0.4–1.0 mg (see Table 2). It should be noted that arterial and venous serum concentrations are similar [95]. Older studies have shown a volume of distribution of 200 L and a total clearance of about 2 L/min [89, 96]. However, Yassen et al. [97] and Skulberg et al. [94, 98] reported volumes of distribution of about 320 L and clearances between 3 and 4 L/min. This is two to three times higher than the maximal liver clearance; consequently, naloxone must be exposed to significant extrahepatic metabolism.
For IM naloxone (see Table 4), the mean time to maximum concentration and mean dose-corrected maximum serum concentration (Cmax) varied from 8 to 24 min and 1.55–4.66 ng/mL, respectively. The latter is far lower than those of IV 14.1–18.6 ng/mL (Table 2). However, dose-corrected area under the curves (AUCs) were as expected rather similar for injectable naloxone (see Tables 2, 4), although AUCs were both AUCinf and AUC 0–t for IM.
5.5.1 Intranasal Route of Administration
The nose is readily available and presents the advantage that laypeople are already familiar with the use of nasal sprays. People who use opioids generally preferred nasal spray over injectable naloxone [71]. The mucosa of the nose is extensively perfused. Its endothelial lining is very open to the external environment. Moreover, its mucosa is constantly cleared by mucociliary transport, requiring that uptake takes place within about 15 min. However, the nose cannot accommodate spray volumes greater than 0.15 mL, as excess volume will be lost as nasal drip or post-nasally [99]. For this reason, many THN programmes have moved from using ‘improvised’ nasal kits (i.e. 2-mL syringes with attached MAD) to distributing approved nasal spray products, which deliver a volume of 0.1 mL.
5.5.2 Approved Nasal Spray Products
Four high-concentrate and approved products, Narcan® [100], Nyxoid® [92], Nalscue® (in France), and Ventizolve® (12 European countries) [94] utilise the Aptar Pharma (hereafter referred to as ‘Aptar’) unit dose spray (0.1 mL, see Table 3). Narcan® by Adapt Pharma (hereafter referred to as “Adapt”) was the first approved nasal spray product, having received FDA approval in November 2015 [101] and Health Canada approval in October 2016. Adapt subsequently also received regulatory approval for a 2-mg/0.1-mL version of the spray, but this product is not commercially available at the time of writing.Footnote 4
A competitor product by Indivior (Nalscue®; 0.9-mg/0.1-mL formulation, also in the Aptar device) failed to receive FDA approval because the nasal spray was found not to be absorbed sufficiently rapidly relative to IM naloxone [102]. Nonetheless, this product secured a marketing authorisation in France in July 2017.
In Europe, Mundipharma received European Medicines Agency approval in November 2017 for a 2-mg/0.1-mL naloxone hydrochloride dihydrate (i.e. 1.8-mg naloxone base; Nyxoid®) concentrated nasal spray for delivery by the same Aptar device as the other new nasal sprays, and has subsequently been rolled out progressively across much of Europe. The pharmacokinetics of the spray formulation have been published [92].
In June 2018, the Norwegian company AS Den Norske Eterfabrikk received regulatory approval in 12 European countries for a 1.26-mg base (1.4 mg hydrochloride) naloxone nasal spray (Ventizolve®); its pharmacokinetics has been published [94].
5.5.3 Intranasal Naloxone: Pharmacokinetics
As part of the development of these high-concentrate naloxone spray products (and their application for regulatory approval), a number of recent studies have explored the pharmacokinetics of IN naloxone (see Table 4). Nasal naloxone doses in these studies ranged from 0.8 to 8 mg. (In the small study [n = 6] by Gufford et al. [103], 0.1- and 0.2-mL volumes were used. Edwards et al. [74] also studied the MAD delivering 2.0 mL).
The high-concentrate IN formulations all have reasonably rapid uptake with a mean time to maximum concentration of 15–30 min, which is somewhat slower than the 8–24 min for the IM formulations (Tables 3, 4; see also Fig. 4). The mean dose-corrected Cmax for IN varied from 1.29 to 2.04 ng/mL, which is lower than for IM (mean 1.55–4.66 ng/mL). A dose–serum concentration relationship was repeatedly reported. Dose-corrected AUCs were far lower (1.40–3.34 ng/mL) than for injectable formulations. This conforms with the relative bioavailability of IN to IM of about 44–54% for the high-concentrate formulations, while only 10–15% was found for the dilute formulations [74]. However, Skulberg et al. [98] found a far higher bioavailability (75%) in subjects under exposure to the opioid remifentanil for 2 hours of the 6-hour study. Whether this is a specific remifentanil or generic opioid effect remains unknown, but a potential higher bioavailability under an opioid may have implications for future regulatory studies of nasal administration.
Absolute bioavailability for concentrate nasal sprays varied from 47 to 54% [92, 93]. Most importantly, these high-concentrate sprays deliver therapeutic doses (0.4–2.0 mg) in a single 0.1-mL spray, and a second spray gives a proportionate rise in serum concentrations. In contrast, dilute nasal spray (2 mg/2 mL) administered via the MAD only had 11–20% absolute bioavailability, implying that a sub-therapeutic dose of approximately 0.2–0.4 mg was delivered [74, 82, 83]. A recent study confirmed that, even after two administrations, dilute nasal spray (2 mg/2 mL, administered via a MAD) failed to achieve naloxone plasma concentrations comparable to concentrate nasal sprays (2 mg/0.1 mL, 4 mg/0.1 mL) at any time [83].
When comparing IV with IM and IN, it is evident that a comparable dose given IV generates immediate and far higher initial serum concentrations. It is also important to acknowledge that the Cmax for the 2- to 4-mg doses of IM (e.g. Evzio®) and IN are far higher than those of the 0.4-mg IM comparator. This is relevant for the discussion below on the risk of withdrawal symptoms.
Skulberg et al. [94] used pharmacokinetic modelling to illustrate the relationship between first-responder nasal naloxone dosing and subsequent IM administrations by ambulance paramedics 10 min later. First-responder dosing of 1.4 mg IN produced plasma concentrations that were higher than 0.4 mg IM 10 min later all the time up to 20 min but lower than for 0.8 mg IM in the first 15 min. However, the combined 1.4 mg IN and 0.4 mg IM 10 min later were higher than 0.8 mg IM alone at the same time. It was concluded that it was beneficial to administer IN for up to 2 min before an ambulance paramedic delivered a 0.4-mg IM dose.
6 Pharmacodynamics, and Efficacy and Safety of Naloxone for the Emergency Management of Opioid Overdose
6.1 Pharmacodynamics
Naloxone is essentially a pure competitive MOR antagonist. Its affinity compares well with the opioid agonists such as morphine, methadone and fentanyl, thus being capable of reversing their actions (see Table 5) [104]. It is estimated that a dose of 0.9 mg/70 kg occupies about 50% of brain receptors in opioid-naïve subjects [105].
Animal testing characterised naloxone as a “potent, rapid-acting, and relatively pure narcotic antagonist”, which counteracted the effects of a range of opioid agonists, including morphine and methadone, without agonist activity of its own [106, 107]. In humans, it was found that 0.35 mg/70 kg of naloxone had a greater effect on opioid-induced respiratory depression than 150 and 20 mg/kg of nalorphine and levallorphan, respectively [108]. Naloxone did not, in contrast to the two others, induce respiratory depression in subjects not given an opioid. Therefore, it was recommended that naloxone should be the opioid antagonist of choice for clinical use [108].
The partial agonist buprenorphine is different (see Table 6). It has a high affinity to MOR and dissociates slowly, in contrast to the much faster dissociation of naloxone [109]. Thus, naloxone reversal of the action of buprenorphine is slow and far larger doses are required [110].
Naloxone equilibrates rapidly with the site of action in the brain as shown by its blood-effect site equilibration half-life of 6.5 min [97], a little slower than that of fentanyl [111]. It is speculated whether an active transport system is involved in this uptake process [112]. In a very recent, positron emission tomography study of nasal naloxone in healthy volunteers, carfentanil was used for initial characterisation of MOR availability. The MOR occupancy was slightly delayed to serum concentrations, and half of peak occupancy was reached at 10 min. The 4-mg IN dose gave up to 85% MOR occupancy [113]. These experimental findings concord with the clinically observed rapid onset of action of naloxone.
Berkowitz [91] showed in the rat that brain concentrations of subcutaneous naloxone rose as rapidly as serum concentrations and stayed steadily above these during a parallel decline. For the agonist morphine, both uptake and egress from the brain lagged its serum concentrations all the time.
Kaufman et al. [114] reported that naloxone in healthy men had a dose-dependent duration of about 1.5 hours on morphine-induced respiratory depression. Onset of action after about 0.35 mg/70 kg IV was 2–3 min, peaking at 25 min. A dose of about 0.33 mg/70 kg was required to reduce the effect of 12 mg of morphine to that of 4 mg.
Pupilometers were used by Gufford et al. [103] to study the attenuating effect of naloxone (2 mg IM and IN) on 4 mg of oral alfentanil (with or without grapefruit juice). However, only moderate increases (about 20%) of the pupil diameter were found. Skulberg et al. [98] used target-controlled infusion of remifentanil to create steady-state opioid agonism. Intramuscular naloxone (0.8 mg) reversed pupil size significantly and was superior to the same IN dose. In a subsequent paper from the same group [95], the duration of action of 1 mg of naloxone IV was 120 min. Moreover, a minimum effective concentration of naloxone in steady state of 0.5 ng/mL was established.
Middleton et al. [115] compared subjective effects and pupil diameter in ten non-dependent PWUO after giving 2 mg and 8 mg of buprenorphine, alone or in combination with 0.5 mg and 2 mg of naloxone. No statistically significant differences were found between formulations. Experimental studies of the effects of naloxone in opioid addicts are rare. Loimer et al. [116] provoked abstinence with naloxone for diagnostic and therapeutic purposes in dependent PWUO in Pakistan, assessing withdrawal using an Objective Opioid Withdrawal Scale. Peak onset of action was within a few minutes for IV, and about 15 min for IM and IN. Durations of actions exceeded 90 min for all administrations.
Overall, several factors affect the outcome of naloxone antagonism (see Table 7). Most of these factors are unknown in an overdose situation, where it is not clear what drugs were consumed. Therefore, naloxone should always be titrated to restore adequate respiration and cognitive function.
6.2 Clinical Effects
Naloxone can reverse serious effects of opioids such as respiratory depression and stupor. Naloxone does not cause physical or psychological dependence and has virtually no effect in a healthy non-dependent person. Naloxone doses up to 1 mg/kg have been tolerated, while 4 mg/kg was found to provoke undesired behavioural effects [117]. As noted above, naloxone also reverses skeletal muscle rigidity from fentanyl and its analogues [30, 31].
The most rewarding use of naloxone is in opioid overdose. Opioid overdose is characterised by stupor, impaired respiration and pin-point (miotic) pupils. Respiratory failure may lead to hypercapnia (also called hypercarbia) and hypoxemia, which may eventually be fatal. The best predictor of a successful response to naloxone in overdose is the miotic pupil [118].
6.3 Recurrence of Toxicity
Naloxone is a short-acting drug compared to the duration of action of many of the opioids [119]. In overdose, the duration of action of methadone, extended-release morphine, buprenorphine, extended-release oxycodone and fentanyl may exceed 12 hours. Thus, the effect of naloxone may wane before the respiratory depression by these opioids has ended [120]. In such cases, hospitalisation and repeat doses or continuous infusion of naloxone may be required [121]. Fortunately, the mortality rate from re-intoxication is low (< 1%) [122, 123].
6.4 Acute Opioid Withdrawal Symptoms
In opioid-dependent subjects, administration of naloxone may produce acute onset of withdrawal symptoms such as agitation, nausea, vomiting, piloerection, diarrhea, lacrimation, yawning and rhinorrhea [116]. Tachycardia and hypertension are potentially serious circulatory effects, while violent behaviour and drug craving are far from trivial. Opioid withdrawal is not considered life threatening [124].
Buajordet et al. [125] conducted a prospective observational study in 1192 episodes of opioid overdose. Suspected adverse events from naloxone were reported in 45% of cases. Thirty-three percent had opioid withdrawal (gastrointestinal disorders, aggressiveness, tachycardia shivering, sweating and tremor), and 15% had headaches and seizures. Only 0.3% were hospitalised for an adverse event. The initial naloxone doses administered were 0.4–0.8 mg IM combined with an IV dose of 0.4 mg.
6.5 Dosing Guidelines for Opioid Overdoses
Recently, a comprehensive review paper (recommended for the interested reader) on naloxone dosing for opioid reversal was published [28]. The initial doses of naloxone commonly recommended for overdose are 0.4–2.0 mg IV or IM [124], with doses surpassing 0.8 mg potentially increasing the risk of significant withdrawal symptoms [9]. The duration of action of naloxone is 20–90 min depending on dose and the situation of the patient [119]. As reported above, a duration of action of about 90–120 min of 1 mg of naloxone was found in healthy volunteers and opioid-dependent individuals [95, 116]. Doses should be titrated every 2–3 min according to response for a total dose of up to 10 mg.
6.5.1 Special Populations
Care should be taken in the elderly, patients with preexisting cardiovascular disease and in those receiving potentially cardiotoxic drugs. The limited available data on naloxone use in pregnant women are not sufficient to inform a drug-associated risk. However, there are risks to the foetus of the opioid-dependent mother with the use of naloxone (Evzio summary of product characteristics). Children (aged 5 years and below) require relatively higher doses such as 0.1 mg/kg because of more severe intoxications [119]. However, lower initial doses (0.01 mg/kg) are also recommended, possible because opioid withdrawal may be life threatening in neonates.
6.5.2 Dosing of ‘Take Home Naloxone’
The situation is different when it comes to THN. The advantage of THN is that naloxone can be administered at an earlier stage, prior to ambulance arrival, similar to layperson use of defibrillators in cardiac arrest. At present, the naloxone dose required in this situation is controversial (see below).
6.5.3 Naloxone Dosing for Fentanyl Overdoses
Severe intoxications of long duration resulting from swallowing fentanyl-adulterated hydrocodone/paracetamol (acetaminophen) tablets were reported [121]. One of the 18 overdose victims died. Seventeen required naloxone boluses, and four needed a prolonged infusion (26–39 hours) of naloxone.
Examination of about 95,000 cases in the national EMS data has also documented an overall increase in the severity of US opioid overdoses [126]. The use of multiple naloxone doses increased from about 15% in 2012 to 18% in 2015 [126]. In contrast, Bell et al. [127] found that systemic dosing of 0.4 mg naloxone (IM) did not increase from 2013 to 2016, despite an increase in fentanyl-related deaths from 4 to 69% in the same period. More than 90% of the reversals were successful after two naloxone doses (0.8 mg).
As for the intoxications resulting in immediate deaths, only anecdotal reports are available on the effect of nasal naloxone on fentanyl overdoses. Somerville et al. [27] summarised characteristics of assumed fentanyl overdoses in Massachusetts during 2014–2016. In 5% of deaths, laypersons administered naloxone. Among those who received nasal naloxone (2 mg/2 mL), respondents reported that 83% required two (equivalent to about a 0.4- to 0.8-mg systemic dose) or more doses before a response was seen. In addition to the limited use of naloxone by laypersons, rapid bystander response was inhibited by a lack of bystanders (18%), spatial separation of decedents from bystanders (e.g. person was in another room of the house [58%]), lack of awareness of the decedent’s drug use (24%), intoxication of bystanders themselves (12%), failure to recognise overdose symptoms (11%) or bystander assumption that the decedent had gone to sleep (15%). Clear evidence that a bystander was unimpaired, witnessed the drug consumption and was present during an overdose (i.e. able to respond immediately) was reported in 1% of the fentanyl overdose decedent charts. Moderate titrated doses of nasal naloxone appeared effective when given.
6.6 Safety and Efficacy of Non-approved Nasal Formulations
6.6.1 Randomised Controlled Studies
A few open-label randomised clinical studies in the pre-hospital setting have evaluated IN vs. IM naloxone. Both Kerr et al. [128] and Kelly et al. [129] compared an upper-level initial dose of 2 mg IM with a 2-mg IN dose. Primary outcomes in these studies were similar, with adequate respiration and Glasgow Coma Scale response at 8–10 min. In the study by Kelly et al. [129], IM did somewhat better than IN (2-mg/5-mL formulation; 82% vs. 63% successful reversals), compared to 78% and 72% reported in the Kerr et al. [128] paper (2-mg/2-mL IN formulation). The safety of IN naloxone was not inferior to IM. This is somewhat surprising, given that for dilute IN formulations (≤ 1 mg/mL) the time to maximum concentration is slower and dose-corrected Cmax/AUCs are generally lower.
6.6.2 Observational Studies
A retrospective study from Boston, USA, examined the use of nasal naloxone (2 mg/2 mL by MAD syringe) by basic life support providers [130]. After dosing, patients were transported to an emergency department. Nasal naloxone reversed overdose in 95% of 793 patients, and only 9% required additional naloxone. Ninety-seven percent of patients had taken heroin, 3% had taken other opioids.
In another retrospective study, 2 mg/2 mL of nasal naloxone (MAD syringe) was administered by law enforcement officers and basic life supporters. The overdose victims (n = 2166) were subsequently managed by paramedics [131], and 9% needed at least one additional naloxone dose.
Despite somewhat different follow-up procedures in these studies, low rates for re-dosing (9%) were reported. This indicates that nasal systemic doses equivalent to 0.2–0.4 mg IV/IM [74, 82], which may be below the lowest World Health Organization-recommended starting dose of 0.4 mg [9], seem both safe and effective in most circumstances when given in medical settings (in contrast to layperson administration).
6.7 Safety of Approved Nasal Formulations
As the basis for approval of naloxone nasal sprays, the FDA requires that any new formulation must prove that it obtains a serum concentration similar to, or higher than the 0.4-mg IM reference in healthy volunteers [132]. It should be noted that there is a discussion within the FDA whether the comparator dose should be increased [133]. The focus of the FDA is on the first 10–15 min after administration. To achieve this goal, owing to the somewhat slower IN uptake, a nasal formulation must systemically deliver relatively more naloxone than IM leading to a considerable “overshoot” of the Cmax and the AUC (i.e. amount entering the systemic circulation). This carries a significant risk for naloxone overdosing that may provoke withdrawal symptoms. Although opioid withdrawal is not considered fatal, it is not trivial. Experiencing withdrawal is feared among people who use opioids. Qualitative interviews in Scottish and US cohorts of PWUO identified negative views on naloxone administration in the emergency room and the harm caused, such as acute withdrawal, aggression, self-discharge and further drug seeking activity [134, 135]. These attitudes were missed by ordinary observational studies. Indeed, these behaviours and further drug seeking activity perhaps constitute behaviourally mediated toxicity [136].
The relatively high success rates reported by first responders using one or two sub-therapeutic doses of naloxone (systemic equivalents of about 0.2–0.8 mg) raises the possibility that many overdoses may be over-treated with the new approved devices delivering naloxone in the upper recommended range (e.g. to about 2 mg by injection). In a report concerning Narcan® (4 mg), 74 of the 196 reported cases of community use had events that may, but not necessarily, conform to opioid withdrawal; none were life threatening [137]. If an intervention turns out to be labelled “withdrawal hazard” by the user community, this may well affect their decision to use the product.
Moreover, in their review of new naloxone products, regulatory bodies did not consider that characteristics of the nose may differ in the target population compared to healthy volunteers or the unexpected observation by Skulberg et al. [98] of a higher nasal bioavailability under opioid infusion. However, we know that all the approved nasal sprays deliver far higher systemic doses than doses supplied by the unapproved dilute nasal sprays. This should secure a very broad safety margin. The nasal (systemic) doses given in the ambulance-based randomised controlled trial in Australia were far lower than the IM comparator [128], yet the two groups performed similarly, except that about one in five overdose cases needed “rescue naloxone” (i.e. a second naloxone dose, this time by injection) following non-response to improvised naloxone nasal spray (2 mg/mL). As a moderate “overtreatment” with naloxone is hard to document, it can be argued that the comparator dose was higher than required for overdose reversal. This complies well with the observational studies that demonstrated unexpected high success rates, also in fentanyl overdoses. Therefore, the new purpose-developed concentrated naloxone nasal sprays which are being approved (dose range 1.4–4.0 mg), all with an option for titration with an accompanying second dose, are likely to offer a higher margin of safety with opioid overdoses, even in the era of illicit fentanyl. Nevertheless, the suitability of the different products will likely depend on the patterns of opioid use in a community, with higher strength formulations potentially needed for the reversal of overdoses from potent synthetic opioids (e.g. fentanyl and its analogues). Last, ventilator support given as rescue breathing is the cornerstone of opioid-induced respiratory failure.
As stated above, there are basically no safety data on the approved products. Pharmacovigilance may answer some of the important questions related to the new products. There is an urgent need for high-quality randomised comparisons of IM vs. IN naloxone administration in overdose. Moreover, observational studies independent of industry examining the efficacy of the new potent nasal naloxone sprays in overdose are warranted. Any consideration of significantly higher initial doses (than those that worked in the past) should be based not on anecdotes but on hard facts.
7 Reviewing the Effectiveness of Take Home Naloxone: Application of the Bradford-Hill Criteria
Twenty years after the 1996 BMJ editorial in which the notion of THN was first mooted [57], it remained unclear whether THN programmes would reduce the rate of opioid overdose deaths. The absence of published data from randomised controlled trials meant that uncertainty regarding the potential public health benefit of THN programmes persisted, leading to implementation delays and lack of political support in many jurisdictions. A small meta-analysis [138] had found a significantly increased odds of recovery from overdose for naloxone administration by bystanders compared with no naloxone administration (odds ratio 8.58, 95% confidence interval 3.90–13.25), but this analysis was only based on nine studies and 66 overdose events, and hence likely not representative of the majority of THN programmes.
To address this evaluation gap, a systematic review [139] was carried out to assess the effectiveness of THN, in terms of impact of opioid overdose mortality. Because of a lack of randomised controlled trials and a wide range in the methodological quality of the research studies, a meta-analysis was dismissed in favour of an analysis using the Bradford Hill [140] criteria: [1] Strength of the Association, [2] Consistency, [3] Specificity, [4] Temporality, [5] Biological Gradient, [6] Plausibility, [7] Coherence, [8] Experiment and [9] Analogy.
Based on their analysis, the authors [139] concluded that THN programmes lead to improved survival rates among programme participants and to reduced overdose mortality rates in the community. A later publication, which also based its analysis on the Bradford Hill criteria, reached a close-to-identical conclusion [141].
8 Barriers to Wider Implementation
Successful implementation of THN would result in widespread acceptability and availability of the intervention, such that it is accessed by relevant target populations and embedded in usual practice in drug treatment and mainstream health services. A number of papers have explored legal [142] and workforce [143, 144] barriers. These have been country and region specific. To date, there has not been a consolidated analysis of barriers to effective THN implementation. The first reason is that there is not a singular model of THN. The second reason is that a comprehensive analysis of implementation barriers requires a conceptual framework.
For the purposes of the analysis here, we refer to two broad types of models of THN implementation. Peer-led (PL) models were initially developed by and for PWUO, to provide training and supply naloxone directly to people who are likely to witness overdoses [138, 145,146,147]. These PL models are provided through organisations oriented to the needs of PWUO. In contrast, mainstream healthcare practitioner (MHCP) models harness medical services (doctors and pharmacies) to supply naloxone to patients and carers. Despite some overlap, they are very different approaches, involve different types of negotiation, and bring different advantages and disadvantages. They also vary in their suitability for different countries or states at different points in time.
Here, we use Greenhalgh et al.’s conceptual framework [148] to consider determinants of THN implementation across the two models. Based on the framework, achieving scaled-up implementation of THN involves considerations regarding the features of the innovation (such as efficacy, product, compatibility); the outer context (including socio-political climate, legal regime and policies, incentives and mandates); the system antecedents and readiness for change (such as organisational structures); the role of individual adopters (such as match with needs, motivation); communication and influence (such as social networks, champions); and the implementation process itself (formalised decision making, logistics and costs). This framework is not a prescription for successful diffusion of innovation, but an aid to considering the multiple aspects, behaviours, and determinants and their interactions.
8.1 Innovation Itself
Several determinants of successful implementation reside in the innovation itself, including the nature of the naloxone product. The injectable naloxone products present some barriers, with concerns including those relating to needle-stick injuries [76]. The newer IN formulations represent a significant advance in the product formulation and address previous concerns about IN bioavailability [11, 92, 149]. With recent reports of synthetic fentanyl not being responsive to usual doses of naloxone [150], we should also not be complacent about efficacy issues (please consult the THN safety discussion, Sect. 6.7)
The prescription status of THN is a significant feature impacting on implementation. Prescription products almost always require medical scripting and pharmacy dispensing and a trained, resourced and supported workforce (see below). Availability via OTC [151] and standing orders [152] address some barriers but not without other barriers arising such as workforce, the potential cost to patients (in some countries) and access [152, 153]. Currently, there are also major issues with stock and supply in many countries including the USA, UK and Australia [153, 154].
Implementation success is also subject to the compatibility of the intervention with the groups delivering it. In theory, THN is highly compatible with the values, norms, and needs of peers and carers (saving friends and loved ones), as well as healthcare professionals (reduced mortality). Yet for both PL and MHCP, there may be some incompatibility with goals. For the PL models, a recently published qualitative study of the views of PWUO highlighted the complex judgement about when to use naloxone given concern about “ruining someone’s high” (p. 34) [155]. There was no consensus on defining the line between a good high and an overdose [155]. For MHCP, there are concerns that providing such a life-saving intervention may encourage less safety in drug use [156,157,158]. Heavey et al. [155] found that some participants reported that naloxone access changed the quantity and frequency of use: “chase a bigger high” (page 32; but see also [159]). A recent working paper [156] that suggested a ‘moral hazard’ problem with THN provoked a furor, although most commentators consider the analysis weak and conclude that the evident logic and benefit of THN remain clear [160, 161]. Nevertheless, the intensity of debate from this paper reveals that there is more work to do in ensuring that THN is seen as compatible with health caring roles, as well as managing the perceived risks associated with THN.
8.2 Outer Context
The second domain of implementation in Greenhalgh et al.’s framework is the “outer context” including the socio-political climate and policy context. The legal frameworks are important in introducing and sustaining THN, including laws concerned with indemnity for consumers (from being charged with offence), and medical personnel (prescribers/dispensers) immunity from being sued [142, 162,163,164,165]. The legal barriers differ between PL and MHCP models. The extent to which these legal regimes are directly associated with increased uptake has yet to be empirically demonstrated [166]. Nonetheless, a conducive legal environment is a prerequisite for widespread implementation.
A key barrier within the outer context domain is the broad stigma and marginalisation of people who use opioids. The general community largely has negative attitudes towards PWUO [167, 168], and this is compounded by internalised stigma [169].
The outer context in the Greenhalgh et al. framework also covers system incentives and mandates. These are the formalised policies and procedures that regulate and support THN programmes. While international documents reference the importance of THN [9, 170], beyond these, there appear to be few formal organisational incentives, directives and mandates in place currently. Mandatory co-prescribing of naloxone with opioid prescriptions has been proposed to address prescription opioid overdoses, and pilot studies have tested this in clinical practice, finding it feasible and associated with reduced opioid-related adverse events [171].
8.3 System Antecedents and Readiness for Change
In Greenhalgh et al.’s framework, both system antecedents and readiness for change are key determinants of implementation success. A receptive context for change, with leadership and vision by the medical profession and by drug user organisations is a pre-requisite for success. Drug user organisations are often under-resourced, and specific funding to provide PL programmes is required. For the MHCP model, the systems and structures for prescribing and dispensing naloxone are certainly well developed. However, barriers remain with respect to adoption by the workforce (see Sect. 8.4).
8.4 Adopters
There are three essential groups of “adopters” whose needs, motivations, values and goals need to align with the intervention to ensure effective widespread availability of THN: people with an opioid-overdose risk; peers and carers; and healthcare professionals. One barrier for potential adopters is stigma, including negative perceptions of PWUO by healthcare providers [172], as well as the stigma of being identified as a person who may use drugs [173]. Stigma reduction programmes targeted at the potential adopters (as well as the general community, see Sect. 8.3) may be required [174,175,176]. The universal supply of naloxone to all with a risk of opioid overdose as part of standard care (and with a patient ‘opt out’ model [177]) has been proposed to address stigma, and also address clinicians’ duty of care where overdose risk is identified. The cost effectiveness of universal supply models is unknown.
There are also significant barriers in relation to knowledge and skills including the need for education and training of potential healthcare providers to enable adoption of THN in the MHCP model [144, 178]. While PWUO often have considerable knowledge of overdose signs and symptoms, knowledge gaps exist amongst different populations with opioid-overdose risk [155, 173, 179].
8.5 Implementation Processes
The process of implementation presents two key barriers here for THN: the workflow logistics and cost. Healthcare professionals have limited time, and THN needs to be incorporated into their workflow, including how to get the THN kit to the patient and the timing of this [152]. There is an opportunity cost for time-pressured healthcare professionals, where training patients on naloxone use may leave less time for other needs. For general medical practitioners and pharmacists, this can be compounded by the systems that pay for their time. For PL models, significant resources are required to deliver training programmes, which peer organisations may not have.
A further substantial implementation barrier is cost, which relates to the medication itself and who is expected to pay. As a prescription medicine, the costs may be covered centrally as part of regular treatment, or subsidised through private health insurance plans, Medicare and Medicaid [142] and/or through grants to harm reduction programmes to purchase THN and then provide it free of charge to clients. In Australia, a script for THN will be affordable to a concession card holder, but OTC (i.e. not subsidised) supply significantly increases the cost to the consumer [153]. Thus, while new supply routes (such as OTC) and formulations (IN) reduce some barriers, they simultaneously present other barriers (in these cases, the cost).
8.6 Communication and Influence
At present, THN largely remains an isolated initiative led by individual champions, harm reduction advocates or health professionals experienced in drug dependence. For it to become a mainstay of usual care, much wider dissemination and diffusion of the technology need to take place. Here, the system variables discussed earlier become most important: widespread stigma against PWUO, the lack of systematic endorsement across all settings and the absence of wide access (such as OTC) that can be provided at low cost.
8.7 Understanding Barriers and Developing Integrated Responses
Across the analysis conducted here using one conceptual implementation framework, it becomes clear that THN implementation has barriers related to the intervention itself (notably the product and its prescription status), the outer context (stigma and a lack of formalised policies and procedures), the adopters (in particular attitudes, knowledge and skills of adopters), and in the practicalities of implementation, especially the cost and the logistics. These determine the extent of THN diffusion such that it becomes a part of regular practice.
9 Conclusions
9.1 Potentially Transformative Public Health Intervention
Naloxone is a well-established emergency medicine for the treatment of life-threatening heroin/opioid overdose. In recent years, with interest in technology transfer, the concept of ‘THN’ has evolved, comprising pre-provision of the supply of naloxone to individuals who may be in the position to intervene and provide essential interim care whilst awaiting the arrival of an ambulance.
9.2 Better Naloxone Products Required for More Effective Take-Home Naloxone
New naloxone products (auto-injector and nasal spray) have been developed in the last few years that have good bioavailability, can provide therapeutic doses in a single step, and hence are suitable for use by lay responders and other non-medical personnel. Four concentrated nasal spray products have now reached the stage of regulatory approval,Footnote 5 with several already introduced in some countries globally: Narcan® 4 mg (USA, Canada, approved and introduced in 2016–2017)Footnote 6, Nalscue® 1 mg (approved and introduced in France in 2017), Nyxoid®Footnote 7 2 mg (European Medicines Agency approval in 2017, introduced across much of Europe from 2018 onwards) and Ventizolve® 1.4-mg spray (developed in Norway and approved for 12 European countries in June 2018).
9.3 Elephant in the Room: Cost and Affordability
When comparing the different naloxone devices, including ampoules and vials as the most basic, there is a clear trade-off between usability and cost. With all products containing the same medication (naloxone), this point is perhaps best illustrated with the example of the FDA-approved auto-injector (Evzio®). At approximately US$600–4500 per unit, the auto-injector is at risk of being considered almost irrelevant for community-wide provision. New concentrated nasal sprays, if costs are kept low, might be particularly suitable for much wider public pre-provision. The cost of twin packs of the new approved naloxone nasal sprays varies between countries from approximately US$30 (equivalent) to several hundred dollars, compared with less than a dollar for ampoules vs. several thousand dollars for auto-injectors. The affordability of new naloxone products will likely define their real-world availability and accessibility for the target population.
9.4 Over-the-Counter Status
As discussed above (see Sect. 8), re-scheduling of naloxone to OTC medication could remove several logistical and legal barriers. However, the issue of THN costs overlaps with the issue of OTC status as high cost could render the product unattainable, even if technically available OTC. By analogy, in the prevention of sexually transmitted infections, cost is a barrier to condom use [180], and free-of-charge condom distribution to target high-risk populations is recommended [181, 182]. A dual implementation model is likely optimal for naloxone access: potential OTC sales should best be considered as operating alongside free-of-charge THN programmes.
9.5 Opioid Overdose Prevention in Low- and Middle-Income Countries
The question of the cost of non-injectable naloxone (vs. injectable forms of the same medicine) becomes particularly relevant for global health. With support from the Global Fund, several countries currently procure naloxone ampoules at the low cost of approximately US$0.50 per ampoule (0.4 mg/mL). Local non-governmental organisations typically hand out two take-home ampoules per client, i.e. equivalent to a total medicine cost of US$1.00 per person. Given the cost disparity between the nasal spray and local ampoule supply, the purchase of naloxone nasal spray is likely not sustainable for low- and middle-income countries at present. However, bulk buying and the production of generics could lower costs in the long term, as has been achieved for second-line antiretroviral therapy for human immunodeficiency virus/acquired immune deficiency syndrome in low- and middle-income countries, where medication costs have been dramatically reduced.
9.6 Need for Continued Research
Surprisingly little attention has been paid to study these new naloxone products with participants from the relevant target population of individuals with substance use disorders, hence uncertainty remains. Will damage to nasal membranes from long-term drug use alter the speed and effectiveness of absorption? Are the findings from healthy volunteers generalisable to overdose victims with potentially very low body weight, near-universal chronic smoker status or varying degrees of hepatic impairment? Is nasal bioavailability of naloxone higher under opioid influence? Can dose titration be taught effectively? What is a safe starting dose, the dose that together with a similar follow-up dose within 3 min that reverse most respiratory failures without provoking too much withdrawals? Such studies may be challenging to devise and conduct, but they would ordinarily be considered necessary steps with the development of new interventions with other clinical populations. There is also a need for stronger study designs to guide further improvements in THN provision.
9.7 Final Remarks
Take-home naloxone has established itself as a major new strand of our response to opioid overdose deaths. This has required new policies and practices, alongside new naloxone formulations and products. These have been developed successfully, and continue to be refined for new challenges, new countries and contexts, and for new opioid drug problems. More research is, of course, needed—with stronger research designs as well as the need for new products and new methods of provision; but this new research must be conducted alongside the introduction of the best products and practices that already exist. With a large and growing problem of heroin/opioid overdose deaths, we have a responsibility to expect the best of science, policy and practice to guide our local, national and global responses.
Notes
pKa is defined as the negative base-10 logarithm of the acid dissociation constant (Ka) of a solution. The lower the pKa value, the stronger the acid.
A generic version of the 4-mg/0.1-mL Narcan nasal spray by Teva Pharmaceuticals also received FDA approval in April 2019 in the US but has not yet been introduced; and an application in the US from InSys for an 8-mg/0.1-mL naloxone nasal spray was accepted for consideration by FDA in July 2019.
A 2-mg version of Narcan® was also approved in North America but was never introduced in clinical practice—see footnote to Table 3.
See footnote to Table 3 for explanation of dose of Nyxoid.
References
UNODC. World drug report. 2016. https://www.unodc.org/wdr2016/. Accessed 17 June 2019.
Rudd R, Seth P, David F, Scholl L. Increases in drug and opioid-involved overdose deaths: United States, 2010–2015. MMWR Morb Mortal Wkly Rep. 2016;65(50–51):1445–52.
Bohnert AS, Tracy M, Galea S. Characteristics of drug users who witness many overdoses: implications for overdose prevention. Drug Alcohol Depend. 2012;120(1–3):168–73.
Zador D, Sunjic S, Darke S. Heroin-related deaths in New South Wales, 1992: toxicological findings and circumstances. Med J Aust. 1996;164(4):204–7.
Powis B, Strang J, Griffiths P, Taylor C, Williamson S, Fountain J, et al. Self-reported overdose among injecting drug users in London: extent and nature of the problem. Addiction. 1999;94(4):471–8.
Tracy M, Piper TM, Ompad D, Bucciarelli A, Coffin PO, Vlahov D, et al. Circumstances of witnessed drug overdose in New York City: implications for intervention. Drug Alcohol Depend. 2005;79(2):181–90.
Strang J, Powis B, Best D, Vingoe L, Griffiths P, Taylor C, et al. Preventing opiate overdose fatalities with take-home naloxone: pre-launch study of possible impact and acceptability. Addiction. 1999;94(2):199–204.
Strang J, Manning V, Mayet S, Titherington E, Offor L, Semmler C, et al. Family carers and the prevention of heroin overdose deaths: unmet training need and overlooked intervention opportunity of resuscitation training and supply of naloxone. Drugs Educ Prev Policy. 2008;15(2):211–8.
WHO. Community management of opioid overdose. 2014. http://apps.who.int/iris/bitstream/10665/137462/1/9789241548816_eng.pdf?ua=1&ua=1. Accessed 25 Jan 2016.
UNODC/WHO. Opioid overdose: preventing and reducing opioid overdose mortality. Vienna: United Nations; 2013. http://www.unodc.org/docs/treatment/overdose.pdf. Accessed 17 June 2019.
Lewis CR, Vo HT, Fishman M. Intranasal naloxone and related strategies for opioid overdose intervention by nonmedical personnel: a review. Subst Abuse Rehabil. 2017;8:79–95.
McAuley A, Aucott L, Matheson C. Exploring the life-saving potential of naloxone: a systematic review and descriptive meta-analysis of take home naloxone (THN) programmes for opioid users. Int J Drug Policy. 2015;26(12):1183–8.
Elzey MJ, Fudin J, Edwards ES. Take-home naloxone treatment for opioid emergencies: a comparison of routes of administration and associated delivery systems. Expert Opin Drug Deliv. 2017;14(9):1045–58.
Kim HK, Nelson LS. Reducing the harm of opioid overdose with the safe use of naloxone : a pharmacologic review. Expert Opin Drug Saf. 2015;14(7):1137–46.
Berterame S, Erthal J, Thomas J, Fellner S, Vosse B, Clare P, et al. Use of and barriers to access to opioid analgesics: a worldwide, regional, and national study. Lancet. 2016;387(10028):1644–56.
Boudreau D, Von Korff M, Rutter CM, Saunders K, Ray GT, Sullivan MD, et al. Trends in de-facto long-term opioid therapy for chronic non-cancer pain. Pharmacoepidemiol Drug Saf. 2009;18(12):1166–75.
Compton WM, Jones CM, Baldwin GT. Relationship between nonmedical prescription-opioid use and heroin use. N Engl J Med. 2016;374(2):154–63.
Guy GP Jr, Zhang K, Bohm MK, et al. Vital signs: changes in opioid prescribing in the United States, 2006–2015. MMWR Morb Mortal Wkly Rep. 2017;66:697–704.
Beletsky L, Davis CS. Today’s fentanyl crisis: prohibition’s iron law, revisited. Int J Drug Policy. 2017;46:156–9.
Woolf SH, Aron L. Failing health of the United States. BMJ. 2018;360:k496.
Rudd RA, Seth P, David F, Scholl L. Increases in drug and opioid-involved overdose deaths: United States, 2010–2015. MMWR Morb Mortal Wkly Rep. 2016;65:1445–52.
Martins SS, Sarvet A, Santaella-Tenorio J, Saha T, Grant BF, Hasin DS. Changes in US lifetime heroin use and heroin use disorder: prevalence from the 2001–2002 to 2012–2013 National Epidemiologic Survey on alcohol and related conditions. JAMA Psychiatry. 2017;74(5):445–55.
Gladden R, Martinez P, Seth P. Fentanyl law enforcement submissions and increases in synthetic opioid-involved overdose deaths: 27 States, 2013–2014. MMWR (Morbidity and Mortality Weekly Report). 2016;65:837–43. https://doi.org/10.15585/mmwr.mm6533a2.
Gill H, Kelly E, Henderson G. How the complex pharmacology of the fentanyls contributes to their lethality. Addiction. 2019. https://doi.org/10.1111/add.14614 (Epub ahead of print).
Dai Z, Abate MA, Smith GS, Kraner JC, Mock AR. Fentanyl and fentanyl-analog involvement in drug-related deaths. Drug Alcohol Depend. 2019;196:1–8.
Pichini S, Solimini R, Berretta P, Pacifici R, Busardo FP. Acute intoxications and fatalities from illicit fentanyl and analogues: an update. Ther Drug Monit. 2018;40(1):38–51.
Somerville NJ, O’Donnell J, Gladden RM, Zibbell JE, Green TC, Younkin M, et al. Characteristics of fentanyl overdose: Massachusetts, 2014–2016. MMWR Morb Mortal Wkly Rep. 2017;66(14):382–6.
Rzasa Lynn R, Galinkin JL. Naloxone dosage for opioid reversal: current evidence and clinical implications. Ther Adv Drug Saf. 2018;9(1):63–88.
Kinshella MW, Gauthier T, Lysyshyn M. Rigidity, dyskinesia and other atypical overdose presentations observed at a supervised injection site, Vancouver, Canada. Harm Reduct J. 2018;15(1):64.
Burns G, DeRienz RT, Baker DD, Casavant M, Spiller HA. Could chest wall rigidity be a factor in rapid death from illicit fentanyl abuse? Clin Toxicol. 2016;54(5):420–3.
Coruh B, Tonelli MR, Park DR. Fentanyl-induced chest wall rigidity. Chest. 2013;143(4):1145–6.
Dhalla IA, Mamdani MM, Sivilotti MLA, Kopp A, Qureshi O, Juurlink DN. Prescribing of opioid analgesics and related mortality before and after the introduction of long-acting oxycodone. Can Med Assoc J. 2009;181(12):891–6.
Fischer B, Vojtila L, Rehm J. The ‘fentanyl epidemic’ in Canada: some cautionary observations focusing on opioid-related mortality. Prev Med. 2018;107:109–13.
van Amsterdam J, van den Brink W. The misuse of prescription opioids: a threat for Europe? Curr Drug Abuse Rev. 2015;8(1):3–14.
United Nations Office ion drugs and Crime (UNODC). Global overview of the drug demand and supply: latest trends, cross-cutting issues. World Drug Report 2018 (United Nations publication, Sales No. E.18.XI.9).
European Monitoring Centre for Drugs and Drug Addiction. European drug report 2017: trends and developments. Luxembourg: Publications Office of the European Union; 2017.
EMCDDA. Perspectives on drugs: preventing overdose deaths in Europe. EMCDDA (European Monitoring Centre for Drugs and Drug Addiction), Lisbon, Portugal, 2017.
UNODC. World drug report, 2012. United Nations, 2012.
Hickman M, Larney S, Peacock A, Jones H, Grebely J, Degenhardt L. Competing global statistics on prevalence of injecting drug use: why does it matter and what can be done? Addiction. 2018;113(10):1768–74.
Roxburgh A, Dobbins T, Degenhardt L, Peacock A. Opioid, amphetamine, and cocaine-induced deaths in Australia. 2018. https://ndarc.med.unsw.edu.au/resource/opioid-amphetamine-and-cocaine-induced-deaths-australia-august-2018. Accessed 17 June 2019.
Darke S. The life of the heroin user: typical beginnings, trajectories and outcomes. Cambridge: Cambridge University Press; 2011.
Sherman SG, Cheng Y, Kral AH. Prevalence and correlates of opiate overdose among young injection drug users in a large US city. Drug Alcohol Depend. 2007;88(2–3):182–7.
Darke S, Duflou J. The toxicology of heroin-related death: estimating survival times. Addiction. 2016;111(9):1607–13.
Tas B, McDonald R. Commentary on Darke and Duflou (2016): heroin-related deaths: identifying a window for intervention. Addiction. 2016;111(9):1614–5.
Poklis J, Poklis A, Wolf C, Mainland M, Hair L, Devers K, et al. Postmortem tissue distribution of acetyl fentanyl, fentanyl and their respective nor-metabolites analyzed by ultrahigh performance liquid chromatography with tandem mass spectrometry. Forensic Sci Int. 2015;257:435–41.
Merrall EL, Kariminia A, Binswanger IA, Hobbs MS, Farrell M, Marsden J, et al. Meta-analysis of drug-related deaths soon after release from prison. Addiction. 2010;105(9):1545–54.
Seaman S, Brettle R, Gore S. Mortality from overdose among injecting drug users recently released from prison: database linkage study. BMJ. 1998;316(7129):426–8.
Strang J, Bird SM, Parmar MK. Take-home emergency naloxone to prevent heroin overdose deaths after prison release: rationale and practicalities for the N-ALIVE randomized trial. J Urban Health. 2013;90:983–6.
Merrall ELC, Bird SM, Hutchinson SJ. A record-linkage study of drug-related death and suicide after hospital discharge among drug-treatment clients in Scotland, 1996–2006. Addiction. 2013;108(2):377–84.
Ravndal E, Amundsen EJ. Mortality among drug users after discharge from inpatient treatment: an 8-year prospective study. Drug Alcohol Depend. 2010;108(1):65–9.
Cornish R, Macleod J, Strang J, Vickerman P, Hickman M. Risk of death during and after opiate substitution treatment in primary care: prospective observational study in UK general practice research database. BMJ. 2010;341:c5475.
The Garfield E. John Scott Award goes to Jack Fishman and Harold Blumberg for synthesis and investigation of naloxone. Essay Inf Sci. 1982;1983(6):121–30.
Lewenstein MJ, Fishman J. Morphine derivative. US patent 3,254,088 (1966).
Kaufman JJ, Semo NM, Koski WS. Microelectrometric titration measurement of the pKa’s and partition and drug distribution coefficients of narcotics and narcotic antagonists and their pH and temperature dependence. J Med Chem. 1975;18(7):647–55.
WHO. 19th WHO model list of essential medicines. 2015. http://www.who.int/medicines/publications/essentialmedicines/EML2015_8-May-15.pdf. Accessed 1 Apr 2017.
WHO. Comparative table of core and complementary medicines on the WHO essential medicines list from 1977–2011. 2011. http://www.who.int/medicines/publications/essentialmedicines/EMLsChanges1977_2011.xls?ua=1. Accessed 1 Apr 2017.
Strang J, Darke S, Hall W, Farrell M, Ali R. Heroin overdose: the case for take-home naloxone. BMJ. 1996;312(7044):1435.
Bennett GA, Higgins DS. Accidental overdose among injecting drug users in Dorset, UK. Addiction. 1999;94(8):1179–89.
Strang J, Best D, Man L-H, Noble A, Gossop M. Peer-initiated overdose resuscitation: fellow drug users could be mobilised to implement resuscitation. Int J Drug Policy. 2000;11(6):437–45.
Baca CT, Grant KJ. Take-home naloxone to reduce heroin death. Addiction. 2005;100(12):1823–31.
Bigg D. Data on take home naloxone are unclear but not condemnatory. BMJ. 2002;324(7338):678.
Dettmer K, Saunders B, Strang J. Take home naloxone and the prevention of deaths from opiate overdose: two pilot schemes. BMJ. 2001;322(7291):895–6.
Giuliano R. Peer-intervention protocol among young injectors. In: Paper presented at preventing heroin overdose: pragmatic approaches, 13–14 January 2000, Seattle (WA).
Seal KH, Kral AH, Gee L, Moore LD, Bluthenthal RN, Lorvick J, et al. Predictors and prevention of nonfatal overdose among street-recruited injection heroin users in the San Francisco Bay Area, 1998–1999. Am J Public Health. 2001;91(11):1842–6.
Heller DI, Stancliff S. Providing naloxone to substance users for secondary administration to reduce overdose mortality in New York City. Public Health Rep. 2007;122(3):393–7.
ForumDroghe. Preventing opioid overdose deaths: a research on the Italian naloxone distribution model. 2016. http://formazione.fuoriluogo.it/ricerca/naloxone/naloxone-foreword/. Accessed 17 June 2019.
Schifano F. Take home naloxone: a contribution for ongoing debate. BMJ. 2001;322(7291):895–6.
Strang J. Take home naloxone for opiate addicts. BMJ. 2001;323(7318):934.
Trujols J. Take home naloxone: life-saving intervention, medico-legal concern and heroin users’ competence. BMJ. 2001;322:895–6.
Beletsky L, Rich JD, Walley AY. Prevention of fatal opioid overdose. JAMA. 2012;308(18):1863–4.
Kerr D, Dietze P, Kelly AM, Jolley D. Attitudes of Australian heroin users to peer distribution of naloxone for heroin overdose: perspectives on intranasal administration. J Urban Health. 2008;85(3):352–60.
Robertson TM, Hendey GW, Stroh G, Shalit M. Intranasal naloxone is a viable alternative to intravenous naloxone for prehospital narcotic overdose. Prehosp Emerg Care. 2009;13(4):512–5.
Wanger K, Brough L, Macmillan I, Goulding J, MacPhail I, Christenson JM. Intravenous vs subcutaneous naloxone for out-of-hospital management of presumed opioid overdose. Acad Emerg Med. 1998;5(4):293–9.
Edwards ES, Kessler C, Kelley G, Gapasin A, Mardari G, Goldwater R. Pharmacokinetics of 2.0 mg intranasal and intramuscular naloxone HCl administration and the impact of vasoconstrictor use on the bioavailability of intranasal naloxone HCl. In: Poster presented at the 2016 AAPM annual meeting, 31 July–4 August 2016, Washington, DC. http://www.painmed.org/2016posters/posterlb002.pdf. Accessed 17 June 2019.
Walley AY, Xuan Z, Hackman HH, Quinn E, Doe-Simkins M, Sorensen-Alawad A, et al. Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: interrupted time series analysis. BMJ. 2013;346:f174.
Doe-Simkins M, Walley AY, Epstein A, Moyer P. Saved by the nose: bystander-administered intranasal naloxone hydrochloride for opioid overdose. Am J Public Health. 2009;99(5):788–91.
Madah-Amiri D, Clausen T, Lobmaier P. Rapid widespread distribution of intranasal naloxone for overdose prevention. Drug Alcohol Depend. 2017;173:17–23.
Madah-Amiri D, Gjersing L, Clausen T. Naloxone distribution and possession following a large-scale naloxone programme. Addiction. 2019;114(1):92–100.
Strang J, McDonald R, Tas B, Day E. Clinical provision of improvised nasal naloxone without experimental testing and without regulatory approval: Imaginative shortcut or dangerous bypass of essential safety procedures? Addiction. 2016;111(4):574–82.
Dale O. Ethical issues and stakeholders matter. Addiction. 2016;111(4):587–9.
Doe-Simkins M, Banta-Green C, Davis CS, Green TC, Walley AY. Comments on Strang et al. (2016):‘Clinical provision of improvised nasal naloxone without experimental testing and without regulatory approval: imaginative shortcut or dangerous bypass of essential safety procedures?’. Addiction. 2016;111(10):1879–80.
McDonald R, Glende ØD, Dale O, Strang J. International patent applications for non-injectable naloxone for opioid overdose reversal: exploratory search and retrieve analysis of the PatentScope database. Drug Alcohol Rev. 2018;37(2):205–15. https://doi.org/10.1111/dar.12571.
Krieter PA, Chiang CN, Gyaw S, McCann DJ. Comparison of the pharmacokinetic properties of naloxone following the use of FDA-approved intranasal and intramuscular devices versus a common improvised nasal naloxone device. J Clin Pharmacol. 2019. https://doi.org/10.1002/jcph.1401 (Epub ahead of print).
Volkow ND, Frieden TR, Hyde PS, Cha SS. Medication-assisted therapies: tackling the opioid-overdose epidemic. N Engl J Med. 2014;370(22):2063–6.
Hertz S. Naloxone for outpatient use: data required to support an NDA. Silver Spring, MD; 2012. http://www.fda.gov/downloads/Drugs/NewsEvents/UCM300874.pdf. Accessed 17 June 2019.
Nadel J. Clinical and regulatory perspectives on naloxone products intended for use in the community. 2016. http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/AnestheticAndAnalgesicDrugProductsAdvisoryCommittee/UCM524332.pdf. Accessed 17 June 2019.
Smith K, Hopp M, Mundin G, Bond S, Bailey P, Woodward J, et al. Low absolute bioavailability of oral naloxone in healthy subjects. Int J Clin Pharmacol Ther. 2012;50(5):360–7.
Strang J, McDonald R, Alqurshi A, Royall P, Taylor D, Forbes B. Naloxone without the needle: systematic review of candidate routes for non-injectable naloxone for opioid overdose reversal. Drug Alcohol Depend. 2016;163:16–23.
Fishman J, Roffwarg H, Hellman L. Disposition of naloxone-7,8,3H in normal and narcotic-dependent men. J Pharmacol Exp Ther. 1973;187(3):575–80.
Ngai SH, Berkowitz BA, Yang JC, Hempstead J, Spector S. Pharmacokinetics of naloxone in rats and in man: basis for its potency and short duration of action. Anesthesiology. 1976;44(5):398–401.
Berkowitz BA. The relationship of pharmacokinetics to pharmacological activity: morphine, methadone and naloxone. Clin Pharmacokinet. 1976;1(3):219–30.
McDonald R, Lorch U, Woodward J, Bosse B, Dooner H, Mundin G, et al. Pharmacokinetics of concentrated naloxone nasal spray for opioid overdose reversal: phase I healthy volunteer study. Addiction. 2018;113(3):484–93.
Tylleskar I, Skulberg AK, Nilsen T, Skarra S, Jansook P, Dale O. Pharmacokinetics of a new, nasal formulation of naloxone. Eur J Clin Pharmacol. 2017;73(5):555–62.
Skulberg AK, Asberg A, Khiabani HZ, Rostad H, Tylleskar I, Dale O. Pharmacokinetics of a novel, approved, 1.4-mg intranasal naloxone formulation for reversal of opioid overdose: a randomized controlled trial. Addiction. 2019. https://doi.org/10.1111/add.14552 (Epub ahead of print).
Tylleskar I, Skulberg AK, Skarra S, Nilsen T, Dale O. Pharmacodynamics and arteriovenous difference of intravenous naloxone in healthy volunteers exposed to remifentanil. Eur J Clin Pharmacol. 2018;74(12):1547–53.
Albeck H, Woodfield S, Kreek MJ. Quantitative and pharmacokinetic analysis of naloxone in plasma using high-performance liquid chromatography with electrochemical detection and solid-phase extraction. J Chromatogr. 1989;488(2):435–45.
Yassen A, Olofsen E, van Dorp E, Sarton E, Teppema L, Danhof M, et al. Mechanism-based pharmacokinetic–pharmacodynamic modelling of the reversal of buprenorphine-induced respiratory depression by naloxone : a study in healthy volunteers. Clin Pharmacokinet. 2007;46(11):965–80.
Skulberg AK, Tylleskar I, Nilsen T, Skarra S, Salvesen O, Sand T, et al. Pharmacokinetics and -dynamics of intramuscular and intranasal naloxone: an explorative study in healthy volunteers. Eur J Clin Pharmacol. 2018;74(7):873–83.
Dale O, Hjortkjaer R, Kharasch ED. Nasal administration of opioids for pain management in adults. Acta Anaesthesiol Scand. 2002;46(7):759–70.
Krieter P, Chiang N, Gyaw S, Skolnick P, Crystal R, Keegan F, et al. Pharmacokinetic properties and human use characteristics of an FDA approved intranasal naloxone product for the treatment of opioid overdose. J Clin Pharmacol. 2016;56(10):1243–53.
FDA. FDA moves quickly to approve easy-to-use nasal spray to treat opioid overdose. 2015. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm473505.htm. Accessed 17 June 2019.
Indivior. Indivior receives complete response letter from FDA not approving naloxone nasal spray new drug application for opioid overdose. 2015. http://www.indivior.com/investor-news/indivior-receives-complete-response-letter-from-fda-not-approving-naloxone-nasal-spray-new-drug-application-for-opioid-overdose/. Accessed 17 June 2019.
Gufford BT, Ainslie GR, White JR Jr, Layton ME, Padowski JM, Pollack GM, et al. Comparison of a new intranasal naloxone formulation to intramuscular naloxone: results from hypothesis-generating small clinical studies. Clin Transl Sci. 2017;10(5):380–6.
Yaksh TL, Wallace MS. Opioids, analgesia and pain management. In: Brunton L, Chabner B, Knollman B, editors. Goodman & Gilman’s The pharmacological basis of therapeutics. 12th ed. 2011, McGraw-Hill Medical, New York, p. 483–4.
Melichar JK, Nutt DJ, Malizia AL. Naloxone displacement at opioid receptor sites measured in vivo in the human brain. Eur J Pharmacol. 2003;459(2–3):217–9.
Blumberg H, Dayton HB, George M, Rapaport DN. N-allylnoroxymorphine: a potent narcotic antagonist. Fed Proc. 1961;20:311.
Blumberg H, Dayton HB, Wolf PS. Counteraction of narcotic antagonist analgesics by the narcotic antagonist naloxone. Proc Soc Exp Biol Med. 1966;123(3):755–8.
Foldes FF, Duncalf D, Kuwabara S. The respiratory, circulatory, and narcotic antagonistic effects of nalorphine, levallorphan, and naloxone in anaesthetized subjects. Can Anaesth Soc J. 1969;16(2):151–61.
Cassel JA, Daubert JD, DeHaven RN. [(3)H]Alvimopan binding to the micro opioid receptor: comparative binding kinetics of opioid antagonists. Eur J Pharmacol. 2005;520(1–3):29–36.
van Dorp E, Yassen A, Sarton E, Romberg R, Olofsen E, Teppema L, et al. Naloxone reversal of buprenorphine-induced respiratory depression. Anesthesiology. 2006;105(1):51–7.
Scott JC, Stanski DR. Decreased fentanyl and alfentanil dose requirements with age: a simultaneous pharmacokinetic and pharmacodynamic evaluation. J Pharmacol Exp Ther. 1987;240(1):159–66.
Suzuki T, Ohmuro A, Miyata M, Furuishi T, Hidaka S, Kugawa F, et al. Involvement of an influx transporter in the blood–brain barrier transport of naloxone. Biopharm Drug Dispos. 2010;31(4):243–52.
Johansson J, Hirvonen J, Lovro Z, Ekblad L, Kaasinen V, Rajasilta O, et al. Intranasal naloxone rapidly occupies brain mu-opioid receptors in human subjects. Neuropsychopharmacology. 2019. https://doi.org/10.1038/s41386-019-0368-x (Epub ahead of print).
Kaufman RD, Gabathuler ML, Bellville JW. Potency, duration of action and pA2 in man of intravenous naloxone measured by reversal of morphine-depressed respiration. J Pharmacol Exp Ther. 1981;219(1):156–62.
Middleton LS, Nuzzo PA, Lofwall MR, Moody DE, Walsh SL. The pharmacodynamic and pharmacokinetic profile of intranasal crushed buprenorphine and buprenorphine/naloxone tablets in opioid abusers. Addiction. 2011;106(8):1460–73.
Loimer N, Hofmann P, Chaudhry HR. Nasal administration of naloxone is as effective as the intravenous route in opiate addicts. Int J Addict. 1994;29(6):819–27.
Cohen MR, Cohen RM, Pickar D, Weingartner H, Murphy DL, Bunney WE Jr. Behavioural effects after high dose naloxone administration to normal volunteers. Lancet. 1981;2(8255):1110.
Friedman MS, Manini AF. Validation of criteria to guide prehospital naloxone administration for drug-related altered mental status. J Med Toxicol. 2016;12(3):270–5.
Boyer EW. Management of opioid analgesic overdose. N Engl J Med. 2012;367(2):146–55.
Watson WA, Steele MT, Muelleman RL, Rush MD. Opioid toxicity recurrence after an initial response to naloxone. J Toxicol Clin Toxicol. 1998;36(1–2):11–7.
Sutter ME, Gerona RR, Davis MT, Roche BM, Colby DK, Chenoweth JA, et al. Fatal fentanyl: one pill can kill. Acad Emerg Med. 2017;24(1):106–13.
Rudolph SS, Jehu G, Nielsen SL, Nielsen K, Siersma V, Rasmussen LS. Prehospital treatment of opioid overdose in Copenhagen: is it safe to discharge on-scene? Resuscitation. 2011;82(11):1414–8.
Levine M, Sanko S, Eckstein M. Assessing the risk of prehospital administration of naloxone with subsequent refusal of care. Prehosp Emerg Care. 2016;20(5):566–9.
Clarke SF, Dargan PI, Jones AL. Naloxone in opioid poisoning: walking the tightrope. Emerg Med J. 2005;22(9):612–6.
Buajordet I, Næss AC, Jacobsen D, Brørs O. Adverse events after naloxone treatment of episodes of suspected acute opioid overdose. Eur J Emerg Med. 2004;11(1):19–23.
Faul M, Lurie P, Kinsman JM, Dailey MW, Crabaugh C, Sasser SM. Multiple naloxone administrations among emergency medical service providers is increasing. Prehosp Emerg Care. 2017;21(4):411–9.
Bell A, Bennett AS, Jones TS, Doe-Simkins M, Williams LD. Amount of naloxone used to reverse opioid overdoses outside of medical practice in a city with increasing illicitly manufactured fentanyl in illicit drug supply. Subst Abus. 2018. https://doi.org/10.1080/08897077.2018.1449053 (Epub ahead of print).
Kerr D, Kelly AM, Dietze P, Jolley D, Barger B. Randomized controlled trial comparing the effectiveness and safety of intranasal and intramuscular naloxone for the treatment of suspected heroin overdose. Addiction. 2009;104(12):2067–74.
Kelly AM, Kerr D, Dietze P, Patrick I, Walker T, Koutsogiannis Z. Randomised trial of intranasal versus intramuscular naloxone in prehospital treatment for suspected opioid overdose. Med J Aust. 2005;182(1):24–7.
Weiner SG, Mitchell PM, Temin ES, Langlois BK, Dyer KS. Use of intranasal naloxone by basic life support providers. Prehosp Emerg Care. 2017;21(3):322–6.
Klebacher R, Harris MI, Ariyaprakai N, Tagore A, Robbins V, Dudley LS, et al. Incidence of naloxone redosing in the age of the new opioid epidemic. Prehosp Emerg Care. 2017;21(6):682–7.
Hertz S. Naloxone for outpatient use: data required to support an NDA. Silver Spring, MD, 2012. http://www.fda.gov/downloads/Drugs/NewsEvents/UCM300874.pdf. Accessed 17 June 2019.
FDA. Joint meeting of the Anesthetic and Analgesic Drug Products Advisory Committee and the Drug Safety and Risk Management Meeting Announcement. 5 October 2016. https://www.fda.gov/AdvisoryCommittees/Calendar/ucm516000.htm. Accessed 17 June 2019.
Neale J, Strang J. Naloxone: does over-antagonism matter? Evidence of iatrogenic harm after emergency treatment of heroin/opioid overdose. Addiction. 2015;110(10):1644–52.
Elliott L, Bennett AS, Wolfson-Stofko B. Life after opioid-involved overdose: survivor narratives and their implications for ER/ED interventions. Addiction. 2019. https://doi.org/10.1111/add.14608 (Epub ahead of print).
Strang J, Neale J, McDonald R, Kalk N. Toxicity: exploring and expanding the concept. Addiction. 2018;113(4):592–4.
Avetian GK, Fiuty P, Mazzella S, Koppa D, Heye V, Hebbar P. Use of naloxone nasal spray 4 mg in the community setting: a survey of use by community organizations. Curr Med Res Opin. 2018;34(4):573–6.
Giglio RE, Li G, DiMaggio CJ. Effectiveness of bystander naloxone administration and overdose education programs: a meta-analysis. Inj Epidemiol. 2015;2(1):10.
McDonald R, Strang J. Are take-home naloxone programmes effective? Systematic review utilizing application of the Bradford Hill criteria. Addiction. 2016;111(7):1177–87.
Hill AB. The environment and disease: association or causation? Proc R Soc Med. 1965;58(5):295–300.
Olsen A, McDonald D, Lenton S, Dietze PM. Assessing causality in drug policy analyses: how useful are the Bradford Hill criteria in analysing take-home naloxone programs? Drug Alcohol Rev. 2018;37(4):499–501.
Davis CS, Carr D. Legal changes to increase access to naloxone for opioid overdose reversal in the United States. Drug Alcohol Depend. 2015;157:112–20.
Peckham AM, Niculete ME, Steinberg H, Boggs DL. A survey of prescribers’ attitudes, knowledge, comfort, and fear of consequences related to an opioid overdose education and naloxone distribution program. J Public Health Manage. 2018;24(4):310–7.
Nielsen S, Van Hout MC. What is known about community pharmacy supply of naloxone? A scoping review. Int J Drug Policy. 2016;32(Suppl. C):24–33.
Maxwell S, Bigg D, Stanczykiewicz K, Carlberg-Racich S. Prescribing naloxone to actively injecting heroin users: a program to reduce heroin overdose deaths. J Addict Dis. 2006;25(3):89–96.
Lancaster K, Ritter A. Making change happen: a case study of the successful establishment of a peer-administered naloxone program in one Australian jurisdiction. Int J Drug Policy. 2014;25(5):985–91.
Wheeler E, Davidson PJ, Jones TS, Irwin KS. Community-based opioid overdose prevention programs providing naloxone: United States, 2010. MMWR Morb Mortal Wkly Rep. 2012;61(6):101–5.
Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q. 2004;82(4):581–629.
Robinson A, Wermeling DP. Intranasal naloxone administration for treatment of opioid overdose. Am J Health Syst Pharm. 2014;71(24):2129–35.
Morgan J, Jones AL. The role of naloxone in the opioid crisis. Toxicol Commun. 2018;2(1):15–8.
Lenton SR, Dietze PM, Jauncey M. Australia reschedules naloxone for opioid overdose. Med J Aust. 2016;204(4):146–7.
Drainoni ML, Koppelman EA, Feldman JA, Walley AY, Mitchell PM, Ellison J, et al. Why is it so hard to implement change? A qualitative examination of barriers and facilitators to distribution of naloxone for overdose prevention in a safety net environment. BMC Res Notes. 2016;9(1):465.
Pricolo A, Nielsen S. Naloxone rescheduling in Australia: Processes, implementation and challenges with supply of naloxone as a ‘pharmacist only’ over-the-counter medicine. Drug Alcohol Rev. 2018;37(4):450–3.
Hawley KL, Mazer-Amirshahi M, Zocchi MS, Fox ER, Pines JM. Longitudinal trends in US drug shortages for medications used in emergency departments (2001–2014). Acad Emerg Med. 2016;23(1):63–9.
Heavey SC, Chang Y-P, Vest BM, Collins RL, Wieczorek W, Homish GG. Naloxone access and changes in opioid use behaviours. Int J Drug Policy. 2018;51:27–35.
Doleac JL, Mukherjee A. The Moral Hazard of Lifesaving Innovations: Naloxone Access, Opioid Abuse, and Crime (version March 31, 2019). Available at SSRN: https://ssrn.com/abstract=3135264 or https://doi.org/10.2139/ssrn.3135264
Fenichel RR. Which drugs should be available over the counter? The criteria are clear and include safety, timeliness, and opportunity cost. BMJ. 2004;329(7459):182–3.
Green TC, Bowman SE, Zaller ND, Ray M, Case P, Heimer R. Barriers to medical provider support for prescription naloxone as overdose antidote for lay responders. Subst Use Misuse. 2013;48(7):558–67.
Jones JD, Campbell A, Metz VE, Comer SD. No evidence of compensatory drug use risk behavior among heroin users after receiving take-home naloxone. Addict Behav. 2017;71:104–6.
Frank R, Humphreys K, Pollack HA. Does naloxone availability increase opioid abuse? The case for skepticism. 2018. Health Affairs, March 2018, at https://www.healthaffairs.org/do/10.1377/hblog20180316.599095/full/#.Wq_oPlJaD2c.twitter
Tas B, Humphrey K, McDonald R, Strang J. Does take-home naloxone availability increase opioid use? Addiction. 2019. https://doi.org/10.1111/add.14637 (Epub ahead of print).
Burris S, Beletsky L, Castagna CA, Coyle C, Crowe C, McLaughlin JM. Stopping an invisible epidemic: legal issues in the provision of naloxone to prevent opioid overdose. Drexel Law Rev. 2009;1(2):273–339.
Davis C, Webb D, Burris S. Changing law from barrier to facilitator of opioid overdose prevention. J Law Med Ethics. 2013;41:33–6.
Legal Science. Naloxone overdose prevention laws. 2017. http://pdaps.org/datasets/laws-regulating-administration-of-naloxone-1501695139
Rees DI, Sabia JJ, Argys LM, Latshaw J, Dave D. With a little help from my friends: the effects of naloxone access and good samaritan laws on opioid-related deaths. NBER Working Paper Series No. 23171. Cambridge: National Bureau of Economic Research; 2017.
Koester S, Mueller SR, Raville L, Langegger S, Binswanger IA. Why are some people who have received overdose education and naloxone reticent to call emergency medical services in the event of overdose? Int J Drug Policy. 2017;48(Suppl. C):115–24.
Ahern J, Stuber J, Galea S. Stigma, discrimination and the health of illicit drug users. Drug Alcohol Depend. 2007;88(2–3):188–96.
Barry CL, McGinty EE, Pescosolido BA, Goldman HH. Stigma, discrimination, treatment effectiveness, and policy: public views about drug addiction and mental illness. Psychiatr Serv. 2014;65(10):1269–72.
Cama E, Brener L, Wilson H, von Hippel C. Internalized stigma among people who inject drugs. Subst Use Misuse. 2016;51(12):1664–8.
UNODC. Informal scientific network statement: United Nations General Assembly Special Session on Drugs (UNGASS 2016). 2016. http://www.unodc.org/documents/ungass2016//Contributions/Civil/Informal_Scientific_Network_Statement/POST_SN_meeting_draft_FINAL.pdf. Accessed 17 June 2019.
Coffin PO, Behar E, Rowe C, Santos G-M, Coffa D, Bald M, et al. Non-randomized intervention study of naloxone co-prescription for primary care patients on long-term opioid therapy for pain. Ann Intern Med. 2016;165(4):245–52.
Winstanley EL, Clark A, Feinberg J, Wilder CM. Barriers to implementation of opioid overdose prevention programs in Ohio. Subst Abuse. 2016;37(1):42–6.
Nielsen S, Peacock A, Lintzeris N, Bruno R, Larance B, Degenhardt L. Knowledge of opioid overdose and attitudes to supply of take-home naloxone among people with chronic noncancer pain prescribed opioids. Pain Med. 2018;19(3):533–40.
Buechter R, Pieper D, Ueffing E, Zschorlich B. Interventions to reduce experiences of stigma and discrimination of people with mental illness and their caregivers. Cochrane Database Syst Rev. 2013;. https://doi.org/10.1002/14651858.CD010400.
Corrigan PW, Morris SB, Michaels PJ, Rafacz JD, Rüsch N. Challenging the public stigma of mental illness: a meta-analysis of outcome studies. Psychiatr Serv. 2012;63(10):963–73.
Link BG, Phelan JC. Conceptualizing stigma. Ann Rev Sociol. 2001;27:363–85.
Strang J, McDonald R, editors. Preventing opioid overdose deaths with take-home naloxone. Lisbon: EMCDDA; 2016.
Binswanger IA, Koester S, Mueller SR, Gardner EM, Goddard K, Glanz JM. Overdose education and naloxone for patients prescribed opioids in primary care: a qualitative study of primary care staff. J Gen Intern Med. 2015;30(12):1837–44.
Goldman-Hasbun J, DeBeck K, Buxton JA, Nosova E, Wood E, Kerr T. Knowledge and possession of take-home naloxone kits among street-involved youth in a Canadian setting: a cohort study. Harm Reduct J. 2017;14(1):79.
Ubrihien A, Davies SC, Driscoll T. Is cost a structural barrier preventing men who have sex with men accessing condoms? A systematic review. AIDS Care. 2016;28(11):1473–80.
Iacobucci G. Free condoms should be targeted at people with high STI risk, says NICE. BMJ. 2017;357:j1751.
NICE. NICE guideline [NG68]: sexually transmitted infections: condom distribution schemes. 2017. https://www.nice.org.uk/guidance/ng68/chapter/Recommendations. Accessed 17 June 2019.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were received for the preparation of this article.
Conflict of interest
John Strang, through his university, is working with the pharmaceutical industry to identify new or improved treatments and his employer (King’s College London) has received grants, travel costs and/or consultancy payments; this includes investigation of new naloxone formulations and has included work with in the past 3 years, Martindale, Indivior and Mundipharma (all of whom have naloxone products). His employer (King’s College London) has also registered intellectual property on a novel buccal naloxone formulation, naming John Strang et al., and he was earlier named in a patent registration by a pharmaceutical company regarding a concentrated nasal naloxone spray. John Strang et al. have worked as consultants for the United Nations Office on Drugs and Crime, supporting them with a project introducing take-home naloxone to four central and western Asian countries as well as contributing to local take-home naloxone schemes. For a fuller account, see John Strang’s web-page at http://www.kcl.ac.uk/ioppn/depts/addictions/people/hod.aspx. Rebecca McDonald has undertaken an unpaid student industry placement with Mundipharma Research Ltd. and has received conference-related travel funding and an honorarium from IOTOD (Improving Opioid Outcomes in the Treatment of Opioid Dependence). Rebecca McDonald has been involved in the development of a tablet formulation on which the university (King’s College London) has registered intellectual property. Rebecca McDonald has worked as a consultant for the United Nations Office on Drugs and Crime. Gabrielle Campbell is supported by a National Health and Medical Research Council fellowship (No. 1119992). The National Drug and Alcohol Research Centre at the University of New South Wales is supported by funding from the Australian Government under the Substance Misuse Prevention and Service Improvements Grant Fund. Gabrielle Campbell has received investigator‐initiated untied educational grants from Reckitt Benckiser/Indivior for a study of opioid substitution therapy uptake among patients with chronic non-cancer pain. None of these are directly relevant to the current article. Louisa Degenhardt is supported by National Drug and Alcohol Research Centre research fellowships (No. 1109366 and No. 1041472/No. 1 135 991) and by the National Institutes of Health grant NIDA R01DA1104470. The National Drug and Alcohol Research Centre at the University of New South Wales is supported by funding from the Australian Government under the Drug and Alcohol Program. Louisa Degenhardt has received investigator-initiated untied educational grants from Reckitt Benckiser/Indivior for studies of buprenorphine‐naloxone, buprenorphine depot, naloxone, the development of an opioid‐related behaviour scale and a study of opioid substitution therapy uptake among patients with chronic non‐cancer pain. Louisa Degenhardt has received an untied educational grant from Seqirus for a post‐marketing study of tapentadol and an untied educational grant from Mundipharma for a post‐marketing study of oxycodone. These bodies had no involvement in or knowledge of the current article. Suzanne Nielsen has been a named investigator on untied educational grants from Indivior and Seqirus and has delivered training on opioid dependence for Indivior for which honoraria were paid to her institution. Suzanne Nielsen has participated in an advisory board meeting by Mundipharma relating to naloxone for which she declined a sitting fee. Suzanne Nielsen is a current recipient of a National Health and Medical Research Council Research Fellowship (No. 1163961). Alison Ritter is funded through a National Health and Medical Research Council Research Fellowship (GNT1136944). She has received no funding or untied educational grants from any pharmaceutical company in the last 15 years. This article covers (among others) a naloxone formulation that has been approved by 12 European countries from 16 June, 2018 under the name of Ventizolve® (Respinal® in Sweden), produced by Sanivo Pharma AS. The sponsor of this trial was AS Den Norske Eterfabrikk. Ola Dale was engaged by AS Den Norske Eterfabrikk as the principal investigator in this study, for which Ola Dale receives no personal honorarium. Ola Dale’s employer, the Norwegian University of Science and Technology and its subsidiary Technical Transfer Office have signed cooperation and licensing contracts with DNE PHARMA to seek commercialisation of this nasal naloxone formulation. This regulates potential royalties for Ola Dale through the Norwegian University of Science and Technology. DNE Pharma AS has compensated Ola Dale for business travel from Trondheim to Oslo.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Strang, J., McDonald, R., Campbell, G. et al. Take-Home Naloxone for the Emergency Interim Management of Opioid Overdose: The Public Health Application of an Emergency Medicine. Drugs 79, 1395–1418 (2019). https://doi.org/10.1007/s40265-019-01154-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-019-01154-5