Abstract
Introduction
The prevalence of chronic hypertension is increasing in pregnant women. Beta-blockers are among the most prevalent anti-hypertensive agents used in early pregnancy.
Objective
The objective of this study was to investigate whether first-trimester use of beta-blockers increases the risk of specific congenital anomalies in offspring.
Methods
A population-based case-malformed control study was conducted in 117,122 registrations of congenital anomalies from 17 European Concerted Action on Congenital Anomalies and Twins (EUROCAT) registries participating in EUROmediCAT with data for all or part of the period between 1995 and 2013. Associations previously reported in the literature (signals) were tested and an exploratory analysis was performed to identify new signals. Odds ratios of exposure to any beta-blocker or to a beta-blocker subgroup were calculated for each signal anomaly compared with two control groups (non-chromosomal, non-signal anomalies and chromosomal anomalies). The exploratory analyses were performed for each non-signal anomaly compared with all the other non-signal anomalies.
Results
The signals from the literature (congenital heart defects, oral clefts, neural tube defects and hypospadias) were not confirmed. Our exploratory analysis revealed that multi-cystic renal dysplasia had significantly increased odds of occurring after maternal exposure to combined alpha- and beta-blockers (adjusted odds ratio 3.8; 95% confidence interval 1.3–11.0).
Conclusion
Beta-blocker use in the first trimester of pregnancy was not found to be associated with a higher risk of specific congenital anomalies in the offspring, but a new signal between alpha- and beta-blockers and multi-cystic renal dysplasia was found. Future large epidemiological studies are needed to confirm or refute our findings.
Similar content being viewed by others
The results of this large EUROmediCAT study refute the signals reported in the literature but do suggest that multi-cystic renal dysplasia might be associated with combined alpha- and beta-blocker use in the first trimester of pregnancy. |
Future large studies are needed to confirm or refute these findings. |
The individual risk for a pregnant woman will be low and should be balanced against the benefits of beta-blocker treatment during pregnancy. |
1 Introduction
The prevalence of chronic hypertension is increasing in general but also in pregnant women, with obese (body mass index ≥ 30) and older mothers (aged ≥ 35 years) at an increased risk [1, 2]. Chronic hypertension, defined as hypertension (blood pressure ≥ 140/90 mmHg) present before pregnancy or diagnosed before the 20th week of gestation, occurs in approximately 1–5% of all pregnancies but this may be an underestimation [1, 3, 4]. For severe hypertension, anti-hypertensive treatment is necessary to prevent serious complications in both mother and child [4]. Beta-blockers are among the most prevalent classes of anti-hypertensive agents used in early pregnancy, as evidenced by a drug utilisation study in USA where 30% of all anti-hypertensive medications used in the first trimester were beta-blockers [5]. In addition, the use of beta-blockers increased over time in two American studies [5, 6]. From studies in the UK and USA, it is estimated that 0.6% of all pregnant women are exposed to beta-blockers in the first trimester of pregnancy [6, 7].
Despite the increased use of beta-blockers in pregnancy, there is only limited information on their possible teratogenic effects. Beta-blockers could reduce uteroplacental blood flow and could therefore lead to congenital anomalies in the offspring. Most beta-blockers were given the former Pregnancy Letter Category C by the US Food and Drug Administration, meaning that “risk cannot be ruled out” [8] because experimental animal studies have shown an adverse effect on the foetus or there have been no adequate and well-controlled studies in humans. A recent meta-analysis showed that first-trimester beta-blocker use was associated with congenital heart defects [when diabetes was excluded or adjusted for, odds ratio (OR) 2.72, 95% confidence interval (CI) 1.90–3.90], cleft lip/palate (OR 3.11, 95% CI 1.79–5.43) and neural tube defects (RR 3.56, 95% CI 1.19–10.67) [9]. However, it is difficult to establish whether there is a true causal relationship between beta-blocker use and congenital anomalies, as many of the studies were underpowered, potentially biased and heterogeneous.
We therefore aimed to investigate whether first-trimester use of beta-blockers increases the risk of specific congenital anomalies in offspring by using data from EUROmediCAT, a very large database, which has not previously been used to study the effects of beta-blockers. The EUROmediCAT network was set up to evaluate the safety of medication use in pregnancy in relation to the risk of congenital anomalies; it builds on an existing network of population-based congenital anomaly registries in Europe (European Concerted Action on Congenital Anomalies and Twins, EUROCAT), which also have data on maternal medication exposure in the first trimester of pregnancy [10].
2 Methods
2.1 Study Design
We performed a case-malformed control study using data from the EUROmediCAT database, in which we performed both a signal analysis to test associations that had previously been reported in the literature and an exploratory analysis to identify possible new associations [11].
2.2 Literature Review
We first performed a literature review to identify associations that had been previously reported on maternal first-trimester use of beta-blockers and congenital anomalies. All original papers that were included in the meta-analysis of Yakoob et al. were scrutinised [9]. In total, four original studies (three case-control studies and one cohort study) found statistically significant associations between first-trimester use of all or specific beta-blockers and specific congenital anomalies in the offspring [12,13,14,15] (Table 1).
In addition, we searched PubMed to identify original studies that were published after Yakoob et al.’s literature search in August 2011 [9]. The following search terms were used: (“Pregnancy”[Mesh] OR “Pregnancy trimester, First”[Mesh] OR pregnan*[tiab]) AND (“Adrenergic beta-Antagonists”[Mesh] OR “Adrenergic beta-Antagonists”[Pharmacological Action] OR beta adrenergic antag*[tiab] OR adrenergic beta antag*[tiab] OR beta block*[tiab] OR betablock*[tiab] OR beta adrenergic block*[tiab] OR beta adrenergic receptor block*[tiab] OR beta receptor block*[tiab] OR alprenolol[tiab] OR oxprenolol[tiab] OR pindolol[tiab] OR propranolol[tiab] OR timolol[tiab] OR sotalol[tiab] OR nadolol[tiab] OR mepindolol[tiab] OR carteolol[tiab] OR tertatolol[tiab] OR bopindolol[tiab] OR bupranolol[tiab] OR penbutolol[tiab] OR cloranolol[tiab] OR practolol[tiab] OR metoprolol[tiab] OR atenolol[tiab] OR acebutolol[tiab] OR betaxolol[tiab] OR bevantolol[tiab] OR bisoprolol[tiab] OR celiprolol[tiab] OR esmolol[tiab] OR epanolol[tiab] OR s-atenolol[tiab] OR nebivolol[tiab] OR talinolol[tiab] OR labetalol[tiab] OR carvedilol[tiab] OR “Antihypertensive Agents”[Mesh] OR antihypertensive*[tiab]) AND (“Congenital Abnormalities”[Mesh] OR “Prenatal Exposure Delayed Effects”[Mesh] OR congenital*[tiab] OR deformit*[tiab] OR defect*[tiab] OR malformation*[tiab] OR anomal*[tiab] OR side effect*[tiab] OR “adverse effects” [Subheading] OR “chemically induced” [Subheading] OR adverse[tiab] OR abnormalit*[tiab] OR safety[tiab] OR outcome[tiab] OR expos*[tiab] OR teratogen*[tiab]) NOT (“Animals”[Mesh] NOT “Humans”[Mesh]). On 22 December, 2016 there were 378 hits with a publication date between 1 August, 2011 and present, of which 347 were written in English (Fig. 1). This search identified one additional original study reporting a possible association between first-trimester use of non-selective beta-blockers and severe hypospadias (OR 3.22, 95% CI 1.47–7.05), although the effect was non-significant after multiple testing adjustment [16] (Table 1).
2.3 Study Population
EUROCAT is a European network of population-based registries set up in 1979 to perform epidemiological surveillance of congenital anomalies [17]. EUROCAT registries collect data on all pregnancy outcomes: live births, foetal deaths ≥ 20 weeks of gestational age (including stillbirths) and terminations of pregnancy for foetal anomalies (TOPFAs) with a major congenital anomaly. Cases with a minor congenital anomaly are excluded from the EUROCAT database [18]. EUROCAT methodology and details of the member registries have been published previously [19, 20]. The congenital anomalies are coded using the International Classification of Diseases, 9th or 10th Revisions, with British Paediatric Association one-digit extension and are grouped into EUROCAT subgroups of congenital anomalies [17]. Up to nine congenital anomalies can be registered together with text information. EUROmediCAT is a daughter of EUROCAT [10] and contains data from EUROCAT registries that also have data on first-trimester medication exposure coded with the Anatomical Therapeutic Chemical code (ATC code [21]). There is no limit to the number of medications that can be registered and text information can also be registered for each medication exposure.
All EUROCAT registries participating in EUROmediCAT with data over all or part of the period 1995–2013 and with at least one registration in this period with a confirmed first-trimester exposure to a beta-blocker were eligible for inclusion in this study. We included 17 registries in 13 countries in this study with a total coverage of 4,528,994 births: Odense (Denmark), Paris (France), Isle de La Reunion (France), Tuscany (Italy), Emilia Romagna (Italy), Northern Netherlands, Vaud (Switzerland), Zagreb (Croatia), Malta, Antwerp (Belgium), Saxony Anhalt (Germany), Mainz (Germany), Wales (UK), Norway, South East Ireland, Basque Country (Spain) and Valencia Region (Spain) (Table 2).
2.4 Exclusions and Definitions of Cases and Controls
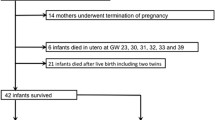
For this study, we excluded registrations with genetic syndromes, teratogenic syndromes, skeletal dysplasias and congenital skin disorders (n = 5777). In addition, we excluded registrations in which the timing of beta-blocker use was unknown (n = 41), registrations with maternal hypertension but no use of anti-hypertensive medication (n = 222), registrations with maternal diabetes and/or insulin use during pregnancy (n = 1723), maternal epilepsy and/or anti-epileptic medication use during pregnancy (n = 1180) and registrations with the use of highly teratogenic medication (US Food and Drug Administration former Pregnancy Letter Category X, n = 17). In total, we excluded 8713 (6.9%) registrations based on one or more of these criteria. All exclusions are presented in the flowchart in Fig. 2.
Flowchart of inclusions and exclusions for the signal analysis. The sum of the separate exclusions is higher than the total number of exclusions because some cases had more than one exclusion criterion. CHD congenital heart defect, CL/P cleft lip with or without cleft palate, CP cleft palate, FDA US Food and Drug Administration, NTD neural tube defect
For the signal analysis, cases were defined as registrations with a congenital anomaly reported in the literature as associated with beta-blocker use in the first trimester of pregnancy: congenital heart defects, with atrial septal defects and pulmonary valve stenosis as specific subgroups; cleft lip with or without cleft palate (CL/P), cleft palate (CP); neural tube defects (NTD) and hypospadias. Registrations with the Pierre Robin sequence were excluded from the CP group. Controls were all other EUROmediCAT registrations and were divided into a non-chromosomal non-signal anomaly group and a chromosomal anomaly group according to the EUROCAT subgroups of congenital anomalies [18]. For the hypospadias analysis, only male control subjects were used in the analyses.
For the exploratory analysis, we only included registrations in the non-chromosomal non-signal control group to search for possible new signals not yet reported in the literature. One by one, all EUROCAT anomaly subgroups were analysed as cases with a changing control group consisting of all other registrations. Registrations with bladder exstrophy, epispadias, prune belly or urethral valves were excluded from the hydronephrosis group because the hydronephrosis is secondary to the underlying anomaly.
2.5 Exposure Definition
The EUROmediCAT registries included in this study obtain the information on medication exposure from the mother’s medical files (mostly these are only files relating to the pregnancy) and from the child’s, except for the Tuscany registry, which only collects data on medication use via a questionnaire that is sent to the mother after birth of the malformed child [22, 23] [Table 1 of the Electronic Supplementary Material (ESM)]. In the Northern Netherlands, pharmacy prescription data were also available. Norway’s medication exposure data are solely based on the Norwegian prescription database. The first trimester of pregnancy is defined as the period from the first day of the last menstrual period to the end of gestational week 12.
In this study, exposure was defined as the use of a beta-blocker (ATC code C07) in the first trimester of pregnancy. All registries were asked to check whether the beta-blockers were indeed used in the first trimester of pregnancy. We further categorised the beta-blockers into three groups: non selective beta-blockers (ATC code C07AA), selective beta-blockers (ATC code C07AB), and combined alpha- and beta-blockers (ATC code C07AG) (Table 3). Non-exposure was defined as no use of any beta-blocker in the first trimester.
2.6 Statistical Analyses
For the signal analysis, we performed logistic regression analysis with SPSS, Version 23 to calculate ORs and 95% CIs of exposure to any beta-blocker or to each of the beta-blocker subgroups for each of the signal anomalies compared with exposure in both control groups. Odds ratios were adjusted for registry, maternal age (categorised as age < 20 years, 20–24 years, 25–29 years, 30–34 years, 35–39 years and ≥ 40 years), use of other anti-hypertensive medications (ATC codes C02, C03, C08, C09), birth year (in 5-year intervals) and pregnancy outcome. Adjustment for pregnancy outcome was performed because in the total study population the exposure rate to beta-blockers was lower in TOPFA cases compared with live births and stillbirths. Additionally, the distribution of pregnancy outcome was different between the case group and the two control groups (with the highest TOPFA rate in the chromosomal control group). Finally, two registers (Emilia Romagna and Valencia) did not have information on maternal medication use for TOPFA cases, partly explaining the lower overall exposure rate in TOPFA cases. In addition, three sensitivity analyses were performed, in which we: (1) restricted the analyses to isolated congenital anomalies (we classified cases as isolated or multiple congenital anomalies based on the EUROCAT Multiple Congenital Anomaly Algorithm [18]), (2) used chromosomal controls without a signal anomaly present, or (3) excluded women who used beta-blockers in combination with other anti-hypertensive medications.
For the exploratory analysis (in the non-chromosomal non-signal group), we calculated the ORs of exposure to any beta-blocker or to each of the beta-blocker subgroups for each of the EUROCAT subgroups of congenital anomalies [18]. The analysis was restricted to subgroups with at least three exposed cases. Odds ratios were adjusted for registry, maternal age, use of other anti-hypertensive medications, birth year and pregnancy outcome, as above.
3 Results
In the period 1995–2013, there were 125,835 registrations of congenital anomalies in the 17 participating EUROmediCAT registries (Fig. 2). After exclusions, we had 117,122 registrations for analysis (93%). These registrations were categorised into a signal anomaly group and two control groups. The signal anomaly group included 49,243 registrations with a congenital anomaly previously reported to be associated with beta-blocker use in the first trimester of pregnancy (neural tube defects, cleft lip with or without CP, CP, congenital heart defects and hypospadias). The first control group comprised 50,709 registrations with non-chromosomal non-signal anomalies and the second control group comprised 17,170 registrations with a chromosomal anomaly.
In this study, the overall exposure to a beta-blocker in the first trimester of pregnancy was 0.27% (320 exposed registrations, Table 2). The exposure rate varied between registries from 0.03% in Valencia to 0.58% in Saxony Anhalt. In a minority of registrations exposed to beta-blockers in the first trimester, use of other anti-hypertensive medications was also registered (n = 55/320, 17.2%, data not shown). The selective beta-blockers (C07AB) were most widely used (in 45.3%), followed by the combined alpha- and beta-blockers (C07AG, in 32.2%, almost exclusively consisting of labetalol) (Table 3). There were 133 registrations exposed to beta-blockers in the signal anomaly group (0.27%), vs. 47 in the chromosomal controls (0.27%) and 140 in the non-chromosomal non-signal controls (0.28%) (Table 4).
The results of the signal analysis are shown in Table 4. We did not find any significantly increased ORs of exposure to beta-blockers for any of the signal anomalies. There were very few exposures to non-selective beta-blockers, which resulted in high ORs with large CIs, in particular when using the chromosomal control group. The next highest ORs were found for selective beta-blockers and CP, but the association remained non-significant when compared with both control groups (adjusted OR 2.0, 95% CI 0.8–5.1 for the non-chromosomal non-signal controls and adjusted OR 1.8, 95% CI 0.6–5.4 for the chromosomal controls). We did find a significantly decreased OR for combined alpha- and beta-blockers and hypospadias (adjusted OR 0.3, 95% CI 0.1–0.8) using the chromosomal controls. In our dataset, there were only two registrations with pulmonary valve stenosis that had been exposed to beta-blockers and we therefore did not include pulmonary valve stenosis as a separate subgroup in the signal analysis.
Sensitivity analyses using only isolated cases, or using chromosomal controls without a signal anomaly, did not meaningfully change the adjusted ORs (Tables 2 and 3 of the ESM). The decreased OR for hypospadias and use of combined alpha- and beta-blockers was no longer significant using chromosomal controls without a signal anomaly present (adjusted OR 0.4, 95% CI 0.1–2.0) (Table 3 of the ESM). In the last sensitivity analysis, in which we excluded women who had used beta-blockers and other anti-hypertensive medications, we found a significantly increased OR for CP after the use of any beta-blocker using non-chromosomal/non-signal controls (adjusted OR 2.1, 95% CI 1.1–4.1) (Table 4 of the ESM).
The results of the exploratory analysis are presented in Table 5. We analysed 13 EUROCAT congenital anomaly subgroups with three or more registrations exposed to beta-blockers and found multi-cystic renal dysplasia (MCRD) to be significantly associated with first-trimester use of beta-blockers (adjusted OR 2.5, 95% CI 1.3–5.1, p = 0.008). This was driven by exposure to combined alpha- and beta-blockers (adjusted OR 3.8, 95% CI 1.3–11.0, p = 0.012).
4 Discussion
In our large EUROmediCAT dataset, we did not confirm the signals reported in the literature between the use of beta-blockers in the first trimester of pregnancy and specific congenital anomalies. It must be noted that the two literature signals with the highest ORs [pindolol and neural tube defects (OR 5.8) and labetalol and ostium secundum atrial septal defects (OR 5.9)] were based on only two and four exposed cases, respectively [12, 14]. In our data, CP was the signal anomaly most likely to be associated with beta-blocker exposure in the first trimester, but the association was only significant when women who used other anti-hypertensive medications were excluded. In total, ten cases with CP (six isolated CP cases, one with multiple congenital anomalies, and three from Norway where the EUROCAT Multiple Congenital Anomaly Algorithm was not applied and therefore could not be classified as either isolated or multiple) were exposed to beta-blockers. The signal reported in the literature was based on three CP cases who were all exposed to oxprenolol (a non-selective beta-blocker currently used infrequently) and was only significant when compared with population controls [15]. No other studies have reported an increased risk of congenital anomalies after exposure to oxprenolol, but experience with its use in the first trimester is limited [24]. Oxprenolol was not present in our dataset. The ten CP cases in our dataset had been exposed to propranolol (n = 3), atenolol (n = 3), metoprolol (n = 2), labetalol (n = 1) and a beta-blocker combination (n = 1). None of the exposed CP cases were also exposed to other anti-hypertensive medications.
It must be noted that all previous studies in which associations were found between beta-blocker use and specific congenital anomalies had certain limitations. Of the four case-control studies, exposure data were solely based on retrospective maternal interviews in two studies of the National Birth Defects Prevention Study [12, 16] and are therefore subject to recall bias. The other two case-control studies, both from Hungary, combined prospective information (from the medical records) with retrospective data (parental questionnaire, nurse visit to non-responding families) [14, 15]. The National Birth Defects Prevention Study used healthy controls, whereas the Hungarian studies used both population controls without congenital anomalies and patient controls with other defects. For all case-control studies, information on certain important confounders (e.g. folic acid, smoking, alcohol and body mass index) was lacking. The cohort study used data from the Swedish Medical Birth Register, which contained information on drug use from the midwife interview at the first antenatal interview (which is before week 12 in 90% of women) [13]. For this study, all non-diabetic women who used anti-hypertensive drugs in early pregnancy were included in the cohort. However, if a women was prescribed beta-blockers, she was only included in the study if she also had a diagnosis of hypertension (because beta-blockers can also be prescribed for other conditions). Therefore, 45% of beta-blocker users were excluded.
In the exploratory analysis, we identified a not previously reported association between first-trimester exposure to combined alpha- and beta-blockers and MCRD (adjusted OR 3.8, 95% CI 1.3–11.0, p = 0.012). This association was based on four isolated MCRD cases from three different registries that had all been exposed to labetalol. Because we performed many tests, the possibility of a chance finding cannot be ruled out and it is therefore important to study this possible association in another dataset. Furthermore, as the prevalence of non-genetic MCRD is low (3.91 per 10,000 births in EUROCAT registries between 2011 and 2015 [25]), the individual risk for a pregnant women using these medications, if any, will be low. With a five-fold increased risk, the absolute risk for MCRD in the offspring is approximately 1 in 500. The possibility of a small increased risk of MCRD must be balanced against the benefits of using labetalol, which is the anti-hypertensive medication of second choice (after methyldopa) for chronic hypertension in pregnancy [4]. Uncontrolled hypertension might harm both the mother and the unborn child, but a blood pressure that is too low might decrease foetoplacental perfusion and could increase the risk of intrauterine growth retardation [4].
The strength of our study is that we used the very large, population-based EUROmediCAT database, which contained over 100,000 registrations with a congenital anomaly with information on medication use in the first trimester of pregnancy. A standard coding system is used by all the registries and ensures detailed and uniform coding of congenital anomalies [18]. As EUROCAT registries record all major congenital anomalies born in the areas they cover, and not just those that are considered important by clinicians, the under-reporting and bias are minimalised. Because we used malformed controls, there is limited potential for recall or other information bias. A difficulty of the case-malformed control study design, however, is the possibility that some of the malformations of the controls are associated with the exposure of interest, which can lead to underestimation of the risk (teratogen non-specificity bias). To protect against this, we have first conducted a literature review to identify all malformations previously associated with beta-blocker exposure (signals), which we excluded from the controls. The controls were divided into two groups, the first consisting of all non-signal non-chromosomal controls and the second consisting of all chromosomal controls. The rationale for using chromosomal controls is that the malformations in these controls have a known aetiology most likely not related to medication use. A consequence of the use of malformed controls is however that the ORs are relative to other malformations and may therefore not be translated directly to the general population. The EUROCAT registries ascertain cases with congenital anomalies in their registration area via multiple sources. In addition, all pregnancy outcomes are included, which is important because terminations of pregnancies constitute a large proportion of some congenital anomalies (e.g. neural tube defects) in some registries. The quality of the EUROCAT data is regularly assessed via data quality indicators [26].
The registrations with an exposure to beta-blockers were all validated and confirmed by the registries. However, the number of congenital anomaly cases exposed to beta-blockers was relatively low (n = 320). In total, 0.27% of registrations were exposed to beta-blockers in the first trimester, which is lower than the 0.6% reported in the literature (drug utilisation studies in USA and the UK [6, 7]). It is possible that beta-blockers are prescribed less in the area covered by the EUROCAT registries that participated in this study, but under-registration of beta-blockers in the EUROmediCAT database is also a possibility, in particular, in the earlier years of our study period, as hospital records on which the exposure information is based can be incomplete. Under-ascertainment of some medications (e.g. antidepressants, anti-asthmatic medications, antibacterials and ovulation stimulants) in the EUROmediCAT database is known to occur and this might also extend to beta-blockers [22, 27]. However, if under-registration of beta-blocker exposure is present, the prospective recording of medication exposure is expected to be similar between cases and malformed controls and should not lead to major bias. Additionally, we have adjusted for registry in our analyses to adjust for variation in exposure ascertainment between the different registries. There was also no information on medication dose and duration of medication use.
We were not able to investigate some of the specific signals reported in the literature: we investigated hypospadias (and not severe hypospadias because the degree of severity was not always available) and atrial septal defects (and not ostium secundum atrial septal defects). Information about the indication for beta-blocker prescription was lacking. From the literature, it is known that beta-blockers are predominantly used to treat hypertension, but can also be prescribed for other conditions such as migraine prophylaxis, angina, after myocardial infarction, arrhythmias, atrial fibrillation, chronic heart failure and essential tremor [28]. In our study population, there were 53 women with reported migraine as a chronic disease but only one of them used a beta-blocker. The other conditions for which beta blockers are prescribed are rare in women of fertile age. Limited information was available on possible confounding factors, including folic acid intake, body mass index, smoking and alcohol use. However, we did exclude women with diabetes or insulin use and epilepsy or anti-epileptic drug use, as well as women who used other highly teratogenic medications.
Finally, we were not able to distinguish between the effect of the disease (in most cases, this would have been chronic hypertension) and the effect of the medication (beta-blocker). It is possible that the likelihood of beta-blocker use depends on the severity of the hypertension. Several papers reported that untreated hypertension is associated with congenital anomalies (e.g. congenital heart defects, neural tube defects, severe hypospadias, oesophageal atresia) in the offspring [12, 16, 29,30,31,32]. The underlying pathogenesis could be that untreated chronic hypertension can lead to uteroplacental insufficiency and therefore decreased blood flow to the foetus and possible vascular disruption [30, 33].
Women with chronic hypertension and of child-bearing age should be counselled about the potential risks of chronic hypertension and of anti-hypertensive treatment during pregnancy. Most anti-hypertensive medications are generally considered safe during pregnancy, with the exception of angiotensin-converting-enzyme inhibitors and angiotensin receptor antagonists [34]. These medications are associated with a characteristic foetopathy (renal failure and hypocalvaria) when used in the second and third trimesters of pregnancy [35]. However, when these medications are used in the first trimester of pregnancy, there does not appear to be an increased risk of structural congenital anomalies compared with the use of other anti-hypertensive medications [36]. The only beta-blocker with positive evidence of risk (US Food and Drug Administration former Letter Category D) is atenolol. Its use in the second trimester of pregnancy has been associated with intrauterine growth retardation. Severe hypertension in pregnancy needs to be treated, but there is no consensus as to whether mild-to-moderate hypertension should also be treated. First-line agents are methyldopa (a centrally acting antiadrenergic agent) and labetalol (a combined alpha- and beta-blocker), but treatment should always be considered on an individual basis [34, 37, 38]. Other considerations are side effects or a history of them, potential interactions with other medications or other diseases, patient preference and cost [34]. Exposure to beta-blockers late in pregnancy might be associated with an increased risk of hypotension, bradycardia, hypoglycaemia, respiratory depression and lower birth weight in the offspring [39, 40]. Our study shows that the risk of congenital anomalies after first-trimester exposure to beta-blockers is probably low, but further studies are needed to confirm this.
5 Conclusion
In this study, no evidence was found that beta-blocker use in the first trimester of pregnancy is associated with an increased risk of specific congenital anomalies in the offspring. The new signal we identified between alpha- and beta-blockers and MCRD needs further investigation. Future large epidemiological studies, ideally based on prospective exposure data and information on the indication of beta-blocker use, are needed to confirm or refute our findings.
References
Bateman BT, Bansil P, Hernandez-Diaz S, Mhyre JM, Callaghan WM, Kuklina EV. Prevalence, trends, and outcomes of chronic hypertension: a nationwide sample of delivery admissions. Am J Obstet Gynecol. 2012;206(134):e1–8.
Kuklina EV, Ayala C, Callaghan WM. Hypertensive disorders and severe obstetric morbidity in the United States. Obstet Gynecol. 2009;113:1299–306.
Bramham K, Parnell B, Nelson-Piercy C, Seed PT, Poston L, Chappell LC. Chronic hypertension and pregnancy outcomes: systematic review and meta-analysis. BMJ. 2014;348:g2301.
Seely EW, Ecker J. Chronic hypertension in pregnancy. Circulation. 2014;129:1254–61.
Bateman BT, Hernandez-Diaz S, Huybrechts KF, Palmsten K, Mogun H, Ecker JL, et al. Patterns of outpatient antihypertensive medication use during pregnancy in a Medicaid population. Hypertension. 2012;60:913–20.
Andrade SE, Raebel MA, Brown J, Lane K, Livingston J, Boudreau D, et al. Outpatient use of cardiovascular drugs during pregnancy. Pharmacoepidemiol Drug Saf. 2008;17:240–7.
Cea Soriano L, Bateman BT, Garcia Rodriguez LA, Hernandez-Diaz S. Prescription of antihypertensive medications during pregnancy in the UK. Pharmacoepidemiol Drug Saf. 2014;23:1051–8.
US National Library of Medicine. Dailymed. http://dailymed.nlm.nih.gov/dailymed/. Accessed 11 May 2017.
Yakoob MY, Bateman BT, Ho E, Hernandez-Diaz S, Franklin JM, Goodman JE, et al. The risk of congenital malformations associated with exposure to beta-blockers early in pregnancy: a meta-analysis. Hypertension. 2013;62:375–81.
EUROmediCAT. Medication safety in pregnancy. http://euromedicat.eu/. Accessed 10 Apr 2017.
Garne E, Hansen AV, Morris J, Zaupper L, Addor MC, Barisic I, et al. Use of asthma medication during pregnancy and risk of specific congenital anomalies: a European case-malformed control study. J Allergy Clin Immunol. 2015;136:1496–502.
Caton AR, Bell EM, Druschel CM, Werler MM, Lin AE, Browne ML, et al. Antihypertensive medication use during pregnancy and the risk of cardiovascular malformations. Hypertension. 2009;54:63–70.
Lennestal R, Otterblad Olausson P, Kallen B. Maternal use of antihypertensive drugs in early pregnancy and delivery outcome, notably the presence of congenital heart defects in the infants. Eur J Clin Pharmacol. 2009;65:615–25.
Medveczky E, Puho E, Czeizel EA. The use of drugs in mothers of offspring with neural-tube defects. Pharmacoepidemiol Drug Saf. 2004;13:443–55.
Puho EH, Szunyogh M, Metneki J, Czeizel AE. Drug treatment during pregnancy and isolated orofacial clefts in Hungary. Cleft Palate Craniofac J. 2007;44:194–202.
Van Zutphen AR, Werler MM, Browne MM, Romitti PA, Bell EM, McNutt LA, et al. Maternal hypertension, medication use, and hypospadias in the National Birth Defects Prevention Study. Obstet Gynecol. 2014;123:309–17.
EUROCAT. European surveillance of congenital anomalies. http://www.eurocat-network.eu/. Accessed 6 Jun 2017.
EUROCAT. Guide 1.4: instructions for the registration and surveillance of congenital anomalies. Updated 20 December 2016. http://www.eurocat-network.eu/content/Full%20Guide%201%204%20v5%2020_Dec2016.pdf. Accessed 6 Jun 2017.
Greenlees R, Neville A, Addor MC, Amar E, Arriola L, Bakker M, et al. Paper 6: EUROCAT member registries: organization and activities. Birth Defects Res A Clin Mol Teratol. 2011;91(Suppl. 1):S51–100.
Boyd PA, Haeusler M, Barisic I, Loane M, Garne E, Dolk H. Paper 1: the EUROCAT network-organization and processes. Birth Defects Res A Clin Mol Teratol. 2011;91(Suppl. 1):S2–15.
WHO Collaborating Centre for Drug Statistics Methodology. ATC/DDD Index 2017. http://www.whocc.no/atc_ddd_index/. Accessed 11 May 2017.
Bakker M, de Jonge L. EUROCAT special report: sources of information on medication use in pregnancy. 2014. http://www.eurocat-network.eu/content/Special-Report-Medication-Use-In-Pregnancy.pdf. Accessed 12 Jan 2017.
EUROmediCAT. Medication safety in pregnancy, profiles of current registries (February 2017). http://www.euromedicat.eu/content/Partners-Registry-Descriptions-February-2017.pdf. Accessed 25 Sep 2017
Briggs GG, Freeman RK, Yaffe SJ. Drugs in pregnancy and lactation, a reference guide to fetal and neonatal risk. 9th ed. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins; 2011.
EUROCAT. Prevalence tables [data uploaded 7 Apr 2017]. http://www.eurocat-network.eu/accessprevalencedata/prevalencetables. Accessed 11 May 2017.
Loane M, Dolk H, Garne E, Greenlees R. EUROCAT Working Group. Paper 3: EUROCAT data quality indicators for population-based registries of congenital anomalies. Birth Defects Res A Clin Mol Teratol. 2011;91(Suppl 1):S23–30.
de Jonge L, Garne E, Gini R, Jordan SE, Klungsoyr K, Loane M, et al. Improving information on maternal medication use by linking prescription data to congenital anomaly registers: a EUROmediCAT Study. Drug Saf. 2015;38:1083–93.
Larochelle P, Tobe SW, Lacourciere Y. Beta-blockers in hypertension: studies and meta-analyses over the years. Can J Cardiol. 2014;30(5 Suppl.):S16–22.
Bateman BT, Huybrechts KF, Fischer MA, Seely EW, Ecker JL, Oberg AS, et al. Chronic hypertension in pregnancy and the risk of congenital malformations: a cohort study. Am J Obstet Gynecol. 2015;212(337):e1–14.
Caton AR, Bell EM, Druschel CM, Werler MM, Mitchell AA, Browne ML, et al. Maternal hypertension, antihypertensive medication use, and the risk of severe hypospadias. Birth Defects Res A Clin Mol Teratol. 2008;82:34–40.
Li DK, Yang C, Andrade S, Tavares V, Ferber JR. Maternal exposure to angiotensin converting enzyme inhibitors in the first trimester and risk of malformations in offspring: a retrospective cohort study. BMJ. 2011;343:d5931.
van Gelder MM, van Bennekom CM, Louik C, Werler MM, Roeleveld N, Mitchell AA. Maternal hypertensive disorders, antihypertensive medication use, and the risk of birth defects: a case-control study. BJOG. 2015;122:1002–9.
van Gelder MM, van Rooij IA, Miller RK, Zielhuis GA, de Jong-van den Berg LT, Roeleveld N. Teratogenic mechanisms of medical drugs. Hum Reprod Update. 2010;16:378–94.
Magee LA. Treating hypertension in women of child-bearing age and during pregnancy. Drug Saf. 2001;24:457–74.
Bullo M, Tschumi S, Bucher BS, Bianchetti MG, Simonetti GD. Pregnancy outcome following exposure to angiotensin-converting enzyme inhibitors or angiotensin receptor antagonists: a systematic review. Hypertension. 2012;60:444–50.
Walfisch A, Al-maawali A, Moretti ME, Nickel C, Koren G. Teratogenicity of angiotensin converting enzyme inhibitors or receptor blockers. J Obstet Gynaecol. 2011;31:465–72.
ACOG Committee on Practice Bulletins. ACOG practice bulletin No. 29: chronic hypertension in pregnancy. Obstet Gynecol. 2001;98(suppl 1):177–85.
Redman CW. Hypertension in pregnancy: the NICE guidelines. Heart. 2011;97:1967–9.
Davis RL, Eastman D, McPhillips H, Raebel MA, Andrade SE, Smith D, et al. Risks of congenital malformations and perinatal events among infants exposed to calcium channel and beta-blockers during pregnancy. Pharmacoepidemiol Drug Saf. 2011;20:138–45.
Nakhai-Pour HR, Rey E, Berard A. Antihypertensive medication use during pregnancy and the risk of major congenital malformations or small-for-gestational-age newborns. Birth Defects Res B Dev Reprod Toxicol. 2010;89:147–54.
Acknowledgements
We thank all the people in Europe who were involved in providing and processing information, including affected families, clinicians, health professionals, medical record clerks and registry staff. We thank Jackie Senior for her editorial assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study is a part of the EUROmediCAT project, which was supported by the European Union under the Seventh Framework Programme (HEALTH-F5-2011-260598). EUROCAT registries are funded as described by Greenlees et al. [19]. EUROCAT Northern Netherlands is funded by the Dutch Ministry of Welfare, Health and Sports.
Conflict of interest
Jorieke E.H. Bergman, L. Renée Lutke, Rijk O.B. Gans, Marie-Claude Addor, Ingeborg Barisic, Clara Cavero-Carbonell, Ester Garne, Miriam Gatt, Kari Klungsoyr, Nathalie Lelong, Catherine Lynch, Olatz Mokoroa, Vera Nelen, Amanda J. Neville, Anna Pierini, Hanitra Randrianaivo, Anke Rissmann, Awi Wiesel, Helen Dolk, Maria Loane and Marian K. Bakker have no conflicts of interest directly relevant to the content of this article. David Tucker declares that he is a shareholder in GlaxoSmithKline.
Ethics approval
This study was performed on anonymised patient data and ethics committee approval was therefore not required.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Bergman, J.E.H., Lutke, L.R., Gans, R.O.B. et al. Beta-Blocker Use in Pregnancy and Risk of Specific Congenital Anomalies: A European Case-Malformed Control Study. Drug Saf 41, 415–427 (2018). https://doi.org/10.1007/s40264-017-0627-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-017-0627-x