Abstract
Purpose of Review
This review seeks to highlight the common and unique factors that impact the kidney health of Indigenous children in Australia, Aotearoa New Zealand, and Canada with a particular interest on efforts to improve their kidney health outcomes and the framework to pursue future efforts.
Recent Findings
In the period since the adoption of the United Nations (UN) Declaration on the Rights of Indigenous People (UNDRIP) there has been a number of studies documenting poorer renal health outcomes and potential causes amongst Indigenous paediatric populations in Australia, Aotearoa New Zealand, and Canada. There is a shortage of studies that look at interventions to improve these outcomes.
Summary
Poorer kidney health outcomes amongst Indigenous children are rarely genetic and appear to be more related to societal inequities. Reported efforts to improve outcomes are few but have demonstrated the ability to make change and with sustained focus on reducing inequities there is hope to improve the renal health of Indigenous children.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Indigenous people live in some 90 countries around the world and are made up of more than 370 million people. Although there is no official definition of an Indigenous person, the UN recognizes an Indigenous person as one that self-identifies with a society that existed prior to colonial encroachment and is a minority group in their current country. They often have strong ties to geographic areas or particular natural resources therein and espouse distinct social, economic, political, language, and cultural practices and beliefs [1].
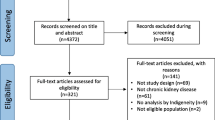
In 2007, the United Nations (UN) Declaration on the Rights of Indigenous Peoples (UNDRIP) was adopted by the UN General Assembly [2•]. This document lays out the foundation for the protection of Indigenous peoples worldwide and includes a recognition that their health must be protected. With this recognition in mind, we sought paediatric studies which describe renal specific diseases, renal health inequities, and efforts to improve renal health outcomes amongst well-recognized indigenous groups from three countries — Aboriginals and Torres Strait Islanders of Australia, Māori of Aotearoa New Zealand, and First Nations, Métis, and Inuit of Canada.
Australia—Aboriginal and Torres Strait Islanders
The indigenous population of Australia are of Aboriginal and Torres Strait Islander origin; they equal over 3% of the Australia population [3], consisting of hundreds of groups with their own distinct languages and traditions. The rates of end-stage kidney disease (ESKD) in the Indigenous adult population of Australia have been described as an epidemic — the rate of ESKD is 20-fold higher for Indigenous than non-Indigenous adults [4]. Aboriginal Australians and Torres Strait Islander have an earlier onset of kidney disease to non-Indigenous people. These worrying trends continue when we look at the literature for young children in Australia. A review of The Australia and New Zealand Dialysis and Transplant Registry (ANZDATA) in 2021 of all patients starting renal replacement therapy before the age of 25 between 1963 and 2017 identified an increasing incidence rates of ESKD in the Aboriginal and Torres Strait Islander children and young adults (ATCYAs) compared to other children and young adults (OCYAs). The incidence of ESKD is significantly higher in the ATCYA cohort 15.1 per million population (PMP) compared to the OCYAs where the incidence is 10.9 PMP [5•].
This observational review of ANZDATA continues to highlight more worrying trends in the management of these patients. The ATCYA cohort spend more time on dialysis and have fewer transplants, only 56% receiving a transplant compared to 89% of the OCYA group. Almost 2/3 of ACYA patients with ESKD transitioned to adult medicine on dialysis compared to less than a third of the OCYA cohort. Far fewer of them receive a pre-emptive (3.4%) or living related donor transplant, with no pre-emptive transplants in the ATCYA population since the 1993–1997 cohort.
Several studies have tried to identify risk factors for this increasing incidence of ESKD and to consider strategies to identify those at risk of CKD earlier. ANZDATA shows that incidence of diabetic nephropathy and hypertension as causes of ESKD is increasing, diabetic nephropathy accounted for ESKD in 4.5% cases of those developing ESKD < 25 years of age in 1982–1986, to more recently 18% of cases in 2013–2017 [5•]. A study of urban Aboriginal children from New South Wales found that 15.6% had hypertension and 12% pre-hypertension, compared to international data of 3–5% and 15% pre-hypertension [6]. Predictors of high blood pressure were paternal high blood pressure and body mass index (BMI).
A prospective population-based cohort study in New South Wales — The Antecedents of Renal Disease in Aboriginal Children (ARDAC) Study, initiated in 2002, aimed to determine whether Aboriginal children have an increased risk of albuminuria in childhood, the ultimate goal being to identify factors that can reduce the incidence of Aboriginal CKD [7]. This large study did not show race to be associated with albuminuria, compared to female gender and lower birth weight which were found to associated with an increased risk of persistent albuminuria. However, overweight Aboriginal children were at slightly higher risk of albuminuria with 2.5% higher prevalence of albuminuria compared to non-Aboriginal children. Unfortunately, this study was unable to access medical history data so no assessment of prior renal disease in either group was possible raising the possibility that previous renal disease could confound the results.
Aboriginal children in Australia have the highest incidence of post-infectious glomerulonephritis (PIGN) in the world; recent studies from Central Australia reported an incidence of 229/100,000 person years [8]. Furthermore, rates in parts of Australia continue to be elevated despite reduction in PIGN rates in many other parts of the world [9]. This is concerning for young people’s future kidney health as studies in adults have found that having had PIGN at least 5 years previously is significantly associated with albuminuria compared to those who have not had PIGN, specifically in women [10]. A history of PIGN, alongside birth weight, and BMI are independent predictors of albuminuria, and the effects are amplified when combined [11].
These data illustrate that for ATCYA there are significant concerns regarding the risk of ESKD and lower rates of transplantation.
Aotearoa New Zealand—Māori
Māori are the Indigenous people of Aotearoa New Zealand with an estimated 875,000 people of Māori descent living in Aotearoa New Zealand and composing 17.1% of the national population [12]. Te Tiriti o Waitangi (the Treaty of Waitangi), the founding document of New Zealand, codifies the rights of Māori to health equity, but despite this, they have long suffered from health inequities in comparison with their non-Indigenous counterparts. The incidence of kidney failure per million of population is higher amongst Māori compared to non-Māori [13]; however, paediatric data does not suggest an increased rate of ESKD amongst Māori children when compared to their non-Māori counterparts [16•]. When examined through a paediatric lens, the ambit of evidence focuses on ESKD outcomes, post-streptococcal glomerulonephritis (PSGN), nephrotic syndrome, and systemic lupus erythematosus (SLE).
There is a paucity of new literature examining ethnicity specific paediatric ESKD data; however, historically, disparities have been described in kidney transplant access and outcomes. A retrospective review of the national paediatric kidney transplant programme from 1982 to 2006 showed that Māori children proportionally received more deceased donor grafts and suffered shorter mean graft survival time when compared to NZ European children. Strikingly, Māori only made up 6% of pre-emptive transplants during this time [14]. This was reiterated in a study from 2005 to 2017, during which 15 pre-emptive kidney transplants were performed, none of which were to Māori children. When compared to New Zealand (NZ) Europeans, Māori children had higher rates of deceased donor transplants [15]. Between 1998 and 2012, Māori also had a lower 5-year graft survival rate of 61% compared to 88% in NZ Europeans [16•]. Preliminary results of an ongoing study show that between 2002 and 2018, Māori have seen an improvement in 5-year graft survival to 79% with no change in NZ European graft survival rates [17]. The specific factors which have fostered this improvement are unclear, but New Zealand has seen the beginnings of systemic change with the government issuing a statement of support for the UNDRIP and acknowledging a need-based model for addressing multiple health and social inequities facing Māori.
It is hypothesized that Māori are disproportionately affected by the lack of potential live donors due to higher prevalence of contraindications such as obesity, diabetes, and hypertension [15]. Primary health statistics show that Māori were more likely than non-Māori to not collect prescriptions due to cost and have an unmet primary health need due to cost or transportation. This poor access to health services underpins poor baseline health characteristics which potentially limits donor eligibility.
PSGN overrepresentation in Māori has been attributed to higher rates of socioeconomic deprivation, overcrowding, poor access, and decreased utilisation of health services. Between 2007 and 2009, Māori children accounted for 39% of identified PSGN cases in Aotearoa New Zealand with an incidence rate ratio of 6.2 (CI, 3.9–10, p < 0.0001) compared to non-Māori children [18]. A follow-up study from 2005 to 2017 reviewing admission rates for PSGN showed that Māori children still had 7 times the risk of admission compared to children of European/Other ethnicity despite rates of admission trending downward by 9% per year. Multivariate analysis models including ethnicity and deprivation suggest that part of the risk conferred by ethnicity may be directly related to deprivation [19]. A study published in 2009, reviewed all cases of PSGN severe enough to require a renal biopsy over the span of 12 years, found that Māori represented 41% of these cases [20]. However, this may directly reflect the prevalence of PSGN in Māori rather than an ethnic correlation to severe disease.
A subset of Māori children with congenital nephrotic syndrome (CNS) has been observed to follow a different clinical course compared to NZ Europeans. A landmark national study between 1975 and 2011 examined the clinical, genetic, and long-term outcomes of all children with CNS. This showed that the median renal survival of Māori patients with CNS was 30 years compared to 0.7 years in NZ Europeans. Māori patients who exhibited a NPHS1 homozygous missense variant of codon 2131 in exon 16 had prolonged native renal function. These patients also showed increased therapeutic efficacy to combination angiotensin-converting enzyme inhibitors and non-steroidal anti-inflammatory agents, characteristically being albumin infusion independent by their second birthday [21•].
Lupus nephritis has been observed to be more frequent and severe in Māori children compared to NZ European. From 2000 to 2010 there were 32 children diagnosed with juvenile SLE with Māori children having twice the number of children per 100,000 per year diagnosed (0.60 vs 0.31) compared to NZ Europeans. Māori children were also more likely to have lupus nephritis and WHO class 4 or 5 lesions at diagnosis and any time throughout the study period [22]. No postulated hypotheses have been put forward to explain these disparities.
Canada—Inuit, First Nations, and Métis
The Canadian Constitution recognizes three Indigenous peoples whose population totals approximately 5% of the Canadian population [23]. The Inuit, whose traditional communities are in the circumpolar region of the north, are the smallest group; the First Nations (FN) people (North American Indians), a culturally diverse but united community who now live in over 600 Nations across Canada; and the Métis, a community that was established from mixed offspring of European traders and First Nations women in the eighteenth century.
The increased burden of kidney disease amongst adult Indigenous Canadians has been established for decades; unfortunately, their children display an increased risk as well. Assessment of the Canadian Organ Replacement Registry (CORR) showed that Indigenous children represented 12.3% of incident kidney disease patients despite representing only 6% of the paediatric population [24]. Incidence rate ratios (IRR) for end-stage kidney disease (ESKD) in young Indigenous patients (< 22 years) compared to White counterparts were 1.82 for boys and 3.24 for girls. Glomerulonephritis (GN) was the aetiology of ESKD amongst Indigenous children at a rate twofold higher than in White children, with IgA nephropathy, rapidly progressing/crescentic GN, and lupus nephritis all occurring at a higher rate amongst Indigenous young people [25]. This supported the results of early regional studies showing the increased incidence of a number GNs, including IgA nephropathy amongst Indigenous children [26, 27].
Samuels et al. showed a lower IRR of ESKD secondary to congenital anomalies (CAKUT) amongst Indigenous children [25]. However, a retrospective analysis of 30 years of maternal-infant data (n = 411,055) from the province of Saskatchewan showed a similar incidence of CAKUT between FN and non-FN births. Of particular concern was the 5-year incidence of CAKUT increased amongst FN births over the study period and was highest in children born to FN mothers with pre-gestational diabetes. Furthermore, follow-up data showed that FN infants with CAKUT had a higher mortality rate, particularly in the first year of life [28•]. It is highly unlikely that these children would have been captured by CORR and are not represented in Samuel’s analyses. This also highlights that the risk of grouping all Indigenous Canadians into a single entity as the community isolation and local environmental factors may impact health. The role of type 2 diabetes mellitus (T2DM) in paediatric FN kidney disease may demonstrate similar regional trends as well.
The provinces of Saskatchewan and Manitoba have the highest burden of kidney disease in Canada. They also have the highest proportion of FN per capita. In Saskatchewan, between 1980 and 2005 the rate of diabetes tripled amongst FN children, with FN girls being most highly affected. Whilst this data did not distinguish between type 1 (T1DM) and T2DM, the age at onset was more in keeping with T2DM affecting FN youth [29]. The cause of T2DM in these children is predominantly multifactorial; however, there are some unique genetic factors, with a well-described FN community in Manitoba with mature-onset diabetes in the young (MODY) secondary to an HNF1a gene variant [30•]. Diabetic nephropathy is generally held as a disease that occurs after prolonged exposure to T2DM. However, a 2-year national surveillance program showed persistent albuminuria in 5.1% of cases of youth with T2DM and 80% were FN with the median duration of diabetes to albuminuria being 21 days [31]. The long-term renal health implications of youth onset diabetes in Manitoba [32] and Saskatchewan [33] have been studied. The Manitoba data demonstrate that youth with T2DM have a fourfold increased risk of kidney failure compared to those with T1DM and a 24-fold increased risk compared to matched controls. The Saskatchewan data show that FN patients with youth onset diabetes had a 2.6-fold increase in end-stage renal disease compared to non-FN, likely reflecting, in part, T2DM as the cause of diabetes in FN.
In addition to the increased disease risk, there are kidney care access issues that disadvantage Indigenous children. They are 46% less likely to receive a transplant by the same time post-dialysis initiation as White children [24]. They are also less likely to receive a live donor kidney. Distance to transplant centres has been shown to impact likelihood of transplantation amongst all Canadian children, and Indigenous children tend to live in more remote communities. However, this is not the sole factor as non-White children who live < 50 km from a transplant centre are less likely to receive a transplant than their White counterparts [34], raising the likelihood of systemic inequities as a contributing factor to this difference.
Knowledge to Action
The Indigenous peoples of Australia, Aotearoa New Zealand, and Canada are ethnically distinct groups and as one would expect, there are unique aspects of paediatric kidney disease that manifest amongst them. However, the trauma and societal repercussions of colonialism are a unifying experience. The ongoing social inequities in these countries are manifested by similar deprivations in access to aspects of paediatric kidney care. As illustrated in the previous sections, concerns are well documented; however, there are a paucity of studies documenting action and efforts to improve outcomes in these groups.
There are large-scale interventions being undertaken. For example, in Aotearoa New Zealand, sweeping changes to the health care system are being implemented. Key to this reform is the creation of Te Aka Whai Ora (Māori Health Authority) with the charge to improve health outcomes for Māori by focusing on the Māori view of health, developing partnerships with Māori communities, and measuring health outcomes for Māori [35]. On a more nephrologic front, in Australia, the Minister for Indigenous Health assigned an expert panel to undertake a comprehensive review into the hurdles, gaps, and challenges faced by Aboriginal and Torres Strait Islander patients receiving treatment for kidney disease. As a result, a National Indigenous Kidney Transplantation Taskforce was founded to evaluate cultural biases and start initiatives to improve patient equity and access [36]. However, at this point, there are no published studies demonstrating improved outcomes—paediatric or otherwise from these programs.
Efforts to improve indigenous health must proceed in such a way that the rights of Indigenous peoples to control access to their health information is paramount, avoiding colonial-like practices in data gathering and utilisation. The Global Indigenous Data Alliance has a framework to be honoured in the study of Indigenous populations [37••]. Adherence to The CARE Principles for Indigenous Data Governance (Table 1) ensure that data is collected and stored in such a manner that Indigenous peoples can derive a Collective benefit from the data. It recognises their Authority to control how the data is used. Those working with Indigenous peoples must recognise their Responsibility to be transparent in how the data will be used to support the community, and finally the Ethics of putting the rights and well-being of Indigenous peoples as the primary focus of any study using their data.
An example of such a project is the First Nations Community Based Screening to Improve Kidney Health and Prevent Dialysis (FINISHED) project [38••]. Responding to the observations described above that FN youth in Manitoba, Canada have a high burden of kidney disease, the FINISHED project was developed as an early screening program for chronic kidney disease risk factors. The project was designed in collaboration with FN communities and adhered to First Nations Information Governance Centre principles of ownership, control, access, and possession of data [39]. Point-of-care screening tests were performed over a 2-year period in 11 communities, many of which were remote and without road access, at schools, nursing stations, and health centres. Overall, screening rate of children 10–17 years of age was 22.4%. Obesity was present in 21.4% of those screened. Prehypertension was present in 11.9% and hypertension in 5.4% of the children. Urine albumin:creatinine ratio (ACR) was > 3 mg/mmol in 10.5%. Estimated glomerular filtration rate (eGFR) was < 90 mL/min/1.73 m2 in 6.2%. Key to this study is the authors used blood pressure (BP), eGFR, ACR, and haemoglobin A1c (HgA1c) to create a risk prediction model (Table 2), which was provided to patients, often the same day, and which was, in turn, used to guide further treatment of these children and youth. Further care included lifestyle counselling, nutrition and exercise advice, guidance to primary care providers, enrolment in annual re-screening, and referral to paediatric nephrology care when indicated. A subsequent evaluation of the patients screened in the FINISHED program demonstrated that the rate of primary care screening in this group was significantly increased in the 18 months following the initial FINISHED screen when compared to the 18-month period preceding it [40••]. The rate of comprehensive testing (at least one eGFR, ACR, and HbA1c test) doubled in the 18-month post-FINISHED period. Primary care visit rate increased from 52.8% prior to FINISHED to 79.3% by the end of the observation period. The FINISHED study has evolved into an established program with ongoing screening in FN communities. Documenting improved hypertension, CKD, and diabetes outcomes amongst those screened will be the true measure of success for the program.
Conclusion
Increased interest in indigenous paediatric kidney health has been demonstrated in the years following UNDRIP. However, there remains a great deal of work to ensure equitable care for these children. We recognise that the groups focused on here are but a subset of the whole Indigenous population worldwide and are those who live in countries with health care systems that are well developed and offer universal access. We would postulate that groups in lower resource countries experience even more disparate care and systems that lack the means to even describe disease risks. When it comes to disease specific risk, our review highlights the importance of recognising the distinct groups that are captured under the heading Indigenous people with unique genetic, environmental, and social factors that contribute to each group. There is a danger of indigenous communities being grouped under a common label that fails to recognise their community’s risk. For example, the Inuit in Canada are remarkably absent from any of the studies reviewed and are frequently grouped with FN patients in database studies.
Whilst having descriptive data is important, what is critical are studies looking at interventions that bring about change for Indigenous children and their renal health. It will fall upon the research community to apply CARE principles [37••] to their efforts and for there to be recognition of the importance of publishing even local studies that serve to improve care of these vulnerable populations. Funding sources and publishing avenues, which may traditionally look for broader patient groups, need to recognise the societal benefit of these types of studies within their structures. This serves to focus efforts and remove research inequities. An increased number of studies being done and access to publication has the potential to provide sharing of strategies and efforts that make a difference in the health of Indigenous children worldwide.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
United Nations Secretariat of the Permanent Forum on Indigenous Issues. [Online].; 2006. Available from: HYPERLINK "https://www.un.org/esa/socdev/unpfii/documents/5session_factsheet1.pdf" https://www.un.org/esa/socdev/unpfii/documents/5session_factsheet1.pdf .
• United Nations Department of Economic and Social Affairs. United Nations Declaration on the Rights of Indigenous People. [Online].; 2007 [cited 2022 July 25. Available from: HYPERLINK "https://www.un.org/development/desa/indigenouspeoples/wp-content/uploads/sites/19/2018/11/UNDRIP_E_web.pdf" https://www.un.org/development/desa/indigenouspeoples/wp-content/uploads/sites/19/2018/11/UNDRIP_E_web.pdf. Internationally accepted declaration that serves as the basis for improving Indigenous health.
Australian Bureau of Statistics. Estimates and Projections, Aboriginal and Torres Strait Islander Australians. [Online].; 2019 [cited 2022 July 27. Available from: HYPERLINK "https://www.abs.gov.au/statistics/people/aboriginal-and-torres-strait-islander-peoples/estimates-and-projections-aboriginal-and-torres-strait-islander-australians/latest-release" https://www.abs.gov.au/statistics/people/aboriginal-and-torres-strait-islander-peoples/estimates-and-projections-aboriginal-and-torres-strait-islander-australians/latest-release .
Spencer JL, Hoy WE, Silva DT, Snelling P. An epidemic of renal failure among Australian Aboriginals. Med J Aust. 1988;168(11):537–41.
• Chaturvedi S, Ullah S, LePage AK, Hughes JT. Rising incidence of end-stage kidney disease and poorer access to kidney transplant among Australian aboriginal and Torres Strait Islander children and young adults. Kidney International Reports. 2021;1(6):1704–10. Recent analysis documenting the serious inequities in pediatric nephrology care in Australia.
Larkins N, Teixeira-Pinto A, Banks E, Gunasekera H, Cass A, Kearnes J, et al. Blood pressure among Australian Aboriginal children. J Hypertens. 2017;35(9):1801–7.
Kim S, Macaskill P, Hodson EM, Daylight J, Williams R, Kearns R, et al. Beginning the trajectory to ESKD in adult life: albuminuria in Australian aboriginal children and adolescents. Pediatr Nephrol. 2017;32(1):119–29.
Dowler J, Wilson A. Acute post-streptococcal glomerulonephritis in Central Australia. Aust J Rural Health. 2020;28(1):74–80.
Chaturvedi S, Boyd R, Krause V. Acute post-streptococcal glomerulonephritis in the Northern Territory of Australia: a review of data from 2009 to 2016 and comparison with the literature. Am J Trop Med Hyg. 2018;99(6):1643–8.
Hoy WE, White AV, Dowling A, Sharma SK, Bloomfield H, Tipiloura BT, et al. Post-streptococcal glomerulonephritis is a strong risk factor for chronic kidney disease in later life. Kidney Int. 2012;81(10):1026–32.
Hoy WE, White AVTB. The multideterminant model of renal disease in a remote Australian Aboriginal population in the context of early life risk factors: lower birth weight, childhood post-streptococcal glomerunlonephritis, and current body mass index inflence levels of. Clin Nephrol. 2015;83:s75-81.
Stats NZ. 2018 Census ethnic group summaries-Māori. [Online].; 2018 [cited 2022 July 25. Available from: HYPERLINK "https://www.stats.govt.nz/tools/2018-census-ethnic-group-summaries/m%C4%81ori" https://www.stats.govt.nz/tools/2018-census-ethnic-group-summaries/m%C4%81ori .
Australia & New Zealand Dialysis and Transplant Registry. Chapter 11—Kidney failure among Māori in Aotearoa New Zealand. 43rd Annual ANZDATA Report. ; 2020.
Kara T, Wong W, Morris MC, Ronaldson J, Weston P. Ethinic differences in renal transplant access and outcome in New Zealand children. Pediatr Transplant. 2011;15:42–42.
Westrate H, Ronaldson J, Yonge G, Dickens A, Erickson R, Wong W, et al. Barriers to pre-emptive kidney transplantation in New Zealand children. J Paediatr Child Health. 2021;57(9):1490–7.
• Grace BS, Kara T, Kennedy SE, McDonald SP. Racial disparities in pediatric kidney transplantation in New Zealand. Pediatr Transplant. 2014;18(7):689–97. First study demonstrating poorer outcomes amongst Māori children with ESKD.
Mussa M, Dickens ARW, Erickson RL, Collins M, Prestidge C. Long term outcomes of pediatric transplantation in New Zealand children. Manuscript in preparation. 2022.
Wong W, Lennon DR, Crone S, Neutze JM, Reed PW. Prospective population-based study on the burden of disease from post-streptococcal glomerulonephritis of hospitalised children in New Zealand: epidemiology, clinical features and complications. J Paediatr Child Health. 2013;49(10):850–5.
Vogel AM, Lennon DR, van der Werf B, Diack M, Neutze JM, Horsfall M, et al. Post-streptococcal glomerulonephritis: some reduction in a disease of disparities. J Paediatr Child Health. 2019;55(6):652–8.
Wong W, Morris MC, Zwi J. Outcome of severe acute post-streptococcal glomerulonephritis in New Zealand children. Pediatr Nephrol. 2009;24:1021–6.
• Wong W, Morris MC, Kara T. Congenital nephrotic syndrome with prolonged renal survival without renal replacement therapy. Pediatr Nephrol. 2013;28:2313–21. Describes the genetic variant causing congenital nephrotic syndrome in Māori.
Concannon A, Rudge S, Yan J, Reed P. The incidence, diagnostic clinical manifestations and severity of juvenile systemic lupus erythematosus in New Zealand Maori and Pacific Island children: the Starship experience (2000–2010). Lupus. 2013;22(11):1156–61.
Government of Canada. Aboriginal Peoples Highlight Tables, 2016 Census. [Online].; 2016 [cited 2022 July 11. Available from: HYPERLINK "https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/hlt-fst/abo-aut/Table.cfm?Lang=Eng&T=101&S=99&O=A" https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/hlt-fst/abo-aut/Table.cfm?Lang=Eng&T=101&S=99&O=A .
Samuel SM, Foster BJ, Tonelli MA, Nettel-Aguirre A, Soo A, Alexander RT, et al. Dialysis and transplantation among Aboriginal children with kidney failure. CMAJ. 2011;183(10):e665–672.
Samuel SM, Foster BJ, Hemmelgarn BR, Nettel-Aguirre A, Crowshoe L, Alexander RT, et al. Incidence and causes of end-stage renal disease among Aboriginal children and young adults. CMAJ. 2012;184(14):E758–64.
Bulloch B, Postl BD, Ogborn MR. Excess prevalence of non diabetic renal disease in native American children in Manitoba. Pediatr Nephrol. 1996;10:702–4.
Casiro OG, Stanwick RS, Walker RD. The prevalence of IgA nephropathy in Manitoba. Can J Public Health. 1988;79(5):308–10.
• Dyck RF, Karunanayake C, Pahwa P, Stang M, Erickson RL, Osgood ND. Congenital Anomalies of the Kidney and Urinary Tract (CAKUT): an emerging relationship with pregestational diabetes mellitus among first nations and non-first nations people in Saskatchewan—results from the DIP: ORRIIGENSS Project. Can J Diabetes. 2021;45(4):346–54. Large population assessment of CAKUT incidence over time. Demonstrates evolving concerns amongst FN births.
Dyck R, Osgood N, Gao A, Stang MR. The epidemiology of diabetes mellitus among first nations and non-first nations children in Saskatchewan. Can J Diabetes. 2012;36(1):19–24.
• Sellers EAC, Triggs-Raine B, Rockman-Greenberg C, Dean HJ. The prevalence of the HNF-1a G319S mutation in Canadian Aboriginal youth with type 2 diabetes. Diabetes Care. 2002;25(12):2202–6. Describes a genetic variant causing early onset diabetes in First Nations children.
Sellers EAC, Hadjiyannakis S, Amed S, Dart AB, Dyck RF, Hamilton J, et al. Persistent albuminuira in children with type 2 diabetes: a Canadian paediatric surveillance program study. J Pediatr. 2016;168:112–7.
Dart AB, Sellers EA, Martens PJ, Rigatto C, Brownell MD, Dean HJ. High burden of kidney disease in youth-onset type 2 diabetes. Diabetes Care. 2012;35(6):1265–71.
Dyck RF, Jiang Y, Osgood ND. The long-term risks of end stage renal disease and mortality among first nations and non-first nations people with youth-onset diabetes. Can J Diabetes. 2014;38(4):237–43.
Samuel SM, Hemmelgarn B, Nettel-Aguirre A, Foster B, Soo A, Alexander RT, et al. Association between residence location and likelihood of transplantation among pediatric dialysis patients. Pediatr Transplant. 2012;16(7):735–41.
Government of New Zealand. Te Aka Whai Ora-Māori Health Authority. [Online].; 2022 [cited 2022 July 27. Available from: HYPERLINK "http://www.teakawhaiora.nz"
Transplant Society of Australia and New Zealand. National Indigenous Kidney Transplantation Taskforce. [Online].; 2022 [cited 2022 July 27. Available from: HYPERLINK "https://tsanz.com.au/committees/niktt.htm" https://tsanz.com.au/committees/niktt.htm .
•• Carroll SR, Garba I, Figueroa-Rodriguez OL, Holbrook J, Lovett R, Materechera S, et al. The CARE principles for indigenous data governance. Data Science Journal. 2020;19(1):43. Describes the key principles that should guide researchers in seeking to carry out research amongst Indigenous peoples.
•• Dart A, Lavallee B, Chartrand C, McLeod L, Ferguson TW, Tangri N, et al. Screening for kidney disease in Indigenous Canadian children: the FINISHED screen, triage and treat program. Paediatr Child Health. 2018;23(7):e134–42. An example of a study that seeks to adhere to CARE principles and bring about change in Indigenous childrens’ renal health.
First Nations Information Governance Centre. The First Nations Principles of OCAP. [Online].; 2022 [cited 2022 July 27. Available from: HYPERLINK "https://fnigc.ca/ocap-training/" https://fnigc.ca/ocap-training/ .
•• Frejuk KL, Harasemiw O, Komenda P, Lavallee B, McLeod L, Chartrand C, et al. Impact of a screen, triage and treat program for identifying chronic disease risk in Indigenous children. CMAJ. 2021;193(36):e1415–22. Follow up on initial screening program looking at improvement in care brought on by the screening program in First Nations children.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Renal
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Erickson, R.L., Selvathesan, N. & Dickens, A.R.W. Kidney Health of Indigenous Children: Insights from Australia, Aotearoa New Zealand, and Canada. Curr Pediatr Rep 10, 227–234 (2022). https://doi.org/10.1007/s40124-022-00274-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40124-022-00274-z