Abstract
Purpose of Review
The purpose of this review is to highlight the major advances of pediatric and neonatal acute kidney injury (AKI) research over the last 5 years with particular interest in describing renal physiology, the definition of AKI, risk factors, epidemiology, interventions, and outcomes.
Recent Findings
The utilization of standardized definitions of AKI has revolutionized our understanding of the incidence and impact of AKI. This has culminated in the seminal Assessment of Worldwide Acute Kidney Injury, Renal Angina and Epidemiology in critically ill children (AWARE), and Assessment of Worldwide Acute Kidney Injury Epidemiology in Neonates (AWAKEN) publications in pediatric and neonatal AKI, respectively. These studies have clearly shown an independent association of AKI with mortality in critically ill children and neonates. Recent work aimed at the prevention of AKI has demonstrated that nephrotoxic medication-induced AKI occurs commonly and can be prevented with protocolized renal function monitoring. This review also highlights advances in the early identification of patients at risk for the development of AKI via scoring systems (renal angina index), functional tests (furosemide stress test), or novel biomarkers. Furthermore, fluid overload has clearly been shown to impact outcomes in those with the most severe forms of AKI requiring renal replacement therapy. Recent single-center studies have highlighted that children with AKI are at increased risk of chronic kidney disease.
Conclusions
The incidence and adverse impact of AKI on outcomes across critically ill pediatric and neonatal populations have been clearly established The importance of fluid overload in children with severe AKI requiring renal replacement therapy is clear. Children with AKI are at increased risk of chronic kidney disease and require long-term outpatient follow-up. As the impact of AKI has become clear, efforts have shifted to prevention of nephrotoxic-induced AKI, early identification, risk stratification (renal angina), and the development of novel biomarkers.
Similar content being viewed by others
Introduction
Acute kidney injury (AKI) is a sudden decrease in kidney function resulting in decreased glomerular filtration rate (GFR), build-up of nitrogenous waste products, abnormalities in electrolyte homeostasis, and dysregulation of fluid balance. Over the last 5 years, our understanding of the epidemiology and impact of AKI in a variety of pediatric populations have grown exponentially. It is now clear that even small disturbances in renal function can have a significant deleterious impact on outcomes. The purpose of this review is to highlight the major advances of pediatric and neonatal AKI research over the last 5 years with particular interest in describing renal physiology, the definition of AKI, risk factors, epidemiology, interventions, and outcomes.
Renal Physiology
To appreciate the risk factors and pathophysiology of neonatal and pediatric AKI, a basic discussion of normal pediatric and neonatal renal physiology as well as the pathophysiology of AKI is necessary. The complex physiology of the kidney is controlled through multiple feedback loops affecting renal blood flow (RBF), which in turn drives glomerular filtration, processing of solute and free water, and oxygen delivery to the individual filtering units of the kidney known as the glomeruli. The gatekeepers of the kidney are the afferent and efferent arterioles, controlling the blood flow to and from the glomeruli. Through the response to afferent dilatory factors (prostaglandins, nitric oxide, and bradykinin), and efferent constrictive factors (sympathetic activation, endothelin, and angiotensin II), the kidney attempts to maintain stable blood flow and steady glomerular filtration rate (GFR). Various disease processes and medications can alter this tight control and lead to injury through distorted renal perfusion or direct injury [1, 2].
An appreciation of the nuances of renal development and physiology is critical to understanding the mechanism and management of AKI in the neonatal period [3•]. Following birth, neonates undergo significant changes in RBF, GFR, and tubular function. As RBF increases, there are corresponding increases in the GFR, from a GFR of 10–20 ml/min/1.73 m2 in neonates to 30–40 ml/min/1.73 m2 by 2 weeks of life to an adult GFR by 2 years of age [4, 5]. The significantly reduced GFR in neonates may make this population particularly susceptibility to the development of AKI, especially when exposed to nephrotoxic medications.
With decreased RBF, the kidney compensates by attempting to expand extracellular volume by increasing water resorption. The resorption of water is driven by the increases absorption of sodium and urea. Sodium retention is driven by renin angiotensin system and increased sympathetic nerve activity. Antidiuretic hormone drives the reabsorption of urea. These reflex mechanisms explain the utility of the fractional excretion of sodium and urea to help differentiate the etiologies of AKI (pre-renal vs. intrinsic, Table 1). The immaturity of these compensatory mechanisms in neonates explains why neonates have unique urinary findings (ex: fractional excretion of sodium) in AKI.
Akin to the selective vulnerability zones in ischemic brain injury, the kidney has particularly vulnerable areas of damage. The most highly susceptible area of damage in the kidney are the third segment of the proximal tubule and the medullary thick ascending limb of the Loop of Henle, while the glomeruli are relatively preserved. These areas are particularly impacted because of their high metabolic demand and decreased ability to convert to anaerobic metabolism. The most conspicuous morphologic features of AKI involve the proximal tubule. These changes include the loss of the proximal tubule brush border, patchy loss of tubule cells, focal areas of proximal tubule dilation with distal tubular casts, and areas of cellular regeneration [6].
Definition
Acute Kidney Injury
The most critical advance in AKI research over the last 30 years has been development and utilization of standardized definitions for AKI to better describe the spectrum of organ injury that can occur. During this time, the definition of AKI has evolved from more than 35 divergent definitions to the currently utilized modern Kidney Disease: Improving Global Outcomes (KDIGO) AKI definition (Table 2). Since 2004, there have been a series of definitions followed by refinements to systematically define AKI including: the Risk, Injury, Failure, Loss of Kidney Function, and End-stage kidney disease (RIFLE, 2004), pediatric RIFLE (2007), and the Acute Kidney Injury Network (AKIN, 2010) definitions [7,8,9]. Most recently, the KDIGO AKI definition has been put forth as a harmonized consensus definition, incorporating important aspects of each of the previous definitions [10••]. All of these systems define AKI according to stage of severity based on graded changes in serum creatinine (SCr) or estimated creatinine clearance from a defined baseline and/or urine output. The KDIGO definition has been validated in single-center studies and the international multicenter Assessment of Worldwide Acute Kidney Injury, Renal Angina and Epidemiology in critically ill children (AWARE) study [11, 12••]. Consensus expert opinion has endorsed the KDIGO AKI definition as the definition that should be utilized for research and clinical care in pediatric patients going forward [13, 14].
Just as the definition of pediatric AKI has evolved, the neonatal AKI definition has similarly progressed, particularly over the last 5–10 years. As interest in neonatal AKI has increased, investigators have abandoned the previously utilized, arbitrary definition of neonatal AKI (defined by a single SCr > 1.5 mg/dl) and adopted the staged definition put forth by Jetton et al., the neonatal modified KDIGO AKI definition (Table 2) [3•, 15]. This system is based upon a rise SCr above a previous trough. The neonatal modified KDIGO AKI criteria is currently the most widely accepted definition for neonatal AKI after a 2013 National Institute of Diabetes and Digestive and Kidney Diseases-sponsored neonatal AKI workshop endorsed this definition [16]. It has subsequently been validated in the multicenter Assessment of Worldwide Acute Kidney injury Epidemiology in Neonates (AWAKEN) study [17••]. While the neonatal modified KDIGO definition remains the current definition to utilize in clinical care and for research purposes, this definition will likely be refined with further study.
Importantly, the AWARE and AWAKEN studies have highlighted the contribution of urine output to the diagnosis of AKI. While oliguria has consistently been a poor prognostic indicator in critically ill children, urine output was often not reported or collected in single-center studies evaluating the epidemiology of AKI [18,19,20,21,22,23]. These AWARE and AWAKEN studies clearly demonstrate that urine output measures are critical to the identification of clinically relevant AKI that would be missed if SCr alone was assessed [12••, 17••].
Fluid Overload
Pediatricians have led the way in identifying fluid overload (FO) as an independent risk factor for adverse outcomes in critically ill patients. This effort began by demonstrating a clear association between the degree of FO at continuous renal replacement therapy (CRRT) initiation and increased mortality and now has extended across all of critical care. The two commonly utilized methods to calculate FO include cumulative fluid balance since ICU admission and a weight-based methodology [24, 25]. The earliest and most commonly utilized method defines FO based on cumulative fluid balance since ICU admission [24]:
A second method to define FO utilizes change in weight from a baseline weight (ICU admission weight, hospital admission weight, or birthweight) [25,26,27,28]:
In order to accurately calculate FO based on changes in weight, it is critical to have standardized methods for the measurement of daily weights [29]. While either fluid balance methodology or weight-based methodology may be utilized in pediatric patients, in the neonatal population, weight-based method is favored [30, 31].
Risk Factors, Epidemiology, and Outcomes
Over the last two decades, there has been an increasing divergence in the etiologies and outcomes of AKI in hospitalized children in developed countries when compared to developing countries. Dehydration and primary renal diseases remain the most common etiologies for AKI in developing countries, but major epidemiologic studies are lacking. A global effort with a particular focus on low- to middle-income countries termed “0by25 initiative” has been undertaken and will increase our understanding of the epidemiology and outcomes of AKI in developing countries. This effort aims to eliminate preventable deaths from AKI by 2025 by employing strategies that allow for the timely diagnosis and treatment of potentially reversible AKI [32]. In developed countries, the etiology of AKI is more clear and most often multifactorial in nature reflecting the increasing medical complexity in neonatal and pediatric patients. Our understanding of risk factors, epidemiology, and outcomes associated with AKI across a variety of neonatal and pediatric populations has expanded exponentially over recent years. Here, we will highlight some of these advances in particular groups.
General Pediatric Critical Care
Among critically ill pediatric populations, the incidence of AKI is variable depending on the sub-population studied, with an incidence as high as 82% in the sickest patients (those requiring mechanical ventilation) [9]. Three large single-center, retrospective studies have shown the incidence of AKI in more general pediatric critical care populations to range from 10 to 19.1% [11, 21, 23]. Each of these studies document an association between AKI and adverse outcomes, including increased length of mechanical ventilation, intensive care unit (ICU) length of stay, and mortality. In a study of 3009 critically ill children, Selewski et al. reported an association between AKI and increased mortality (OR 3.4), confirming the findings previously reported by Alkanderi et al. in 2106 children [11, 21]. Varying incidence with similar associations has been reported in a variety of other critically ill pediatric sub-populations including, but not limited to, those with sepsis, cardiac arrest, and respiratory failure [19, 33,34,35,36,37]. These studies were often limited in their size or single center in nature, which makes generalizability challenging.
In 2017, the AWARE study was published; this international prospective, multicenter study of children and young adults (3 months to 25 years) evaluated the incidence and impact of AKI over a 3-month period in 32 centers across 4 continents [12••]. The overall incidence of AKI in this population was 26.9%, with 11.6% having severe AKI (stage 2 or 3). Severe AKI conferred an increased risk of death by day 28 after adjustment for 16 covariates (aOR, 1.77) and was also associated with increased length of mechanical ventilation. Furthermore, this is the largest study to date to evaluate the contribution of urine output to the diagnosis of AKI. In this study, 67% of patients that developed AKI by urine output criteria did not meet SCr-based AKI criteria; the diagnosis of AKI would have been missed had SCr alone been used to diagnose AKI in these children. More importantly, these patients had worse outcomes than those without AKI. This study suggests that it is essential to incorporate accurate urine output measurement into AKI diagnosis in critically ill patients. The AWARE study has cemented the findings of multiple single-center studies demonstrating definitively that AKI is associated with increased length stay, duration of mechanical ventilation, and mortality.
Congenital Cardiac Surgery
AKI associated with congenital cardiac surgery (CS-AKI) has been well studied over the last 15 years, and it is clear that CS-AKI has defined risk factors (cardiopulmonary bypass (CPB), surgical complexity, and perioperative morbidities) and is associated with adverse outcomes [18, 22, 38,39,40,41,42,43]. Interestingly, the frequency of CS-AKI varies dramatically by study, ranging from 15 to over 50% despite seemingly similar surgical complexity [18, 22, 38,39,40,41,42]. Recently, a secondary analysis of the Safe Pediatric Euglycemia after Cardiac Surgery (SPECS) trial evaluating the incidence and impact of CS-AKI in 799 patients provided insight into potential explanations for this phenomenon [18]. The SPECS trial was a randomized controlled trial comparing the impact of tight glycemic control on outcomes following cardiac surgery at two centers. The incidence of CS-AKI was 36% in the study, with significant differences between institutions (66% at University of Michigan vs 15% Boston Children’s Hospital, p < 0.001). Perioperative characteristics were similar between the centers with the exception of the utilization of intraoperative modified ultrafiltration (91% at University of Michigan vs 8% Boston Children’s Hospital, p < 0.001). CS-AKI at the University of Michigan resolved quicker and did not confer the same negative consequence as it did at Boston Children’s. The authors theorized that modified ultrafiltration may prevent the development of FO while resulting in a short-lived rise in SCr on postoperative day 1 potentially driven by fluid shifts [18]. While this study suggests that all CS-AKI is not created equal, it will be important to further delineate the impact of intra-operative practices on the development of CS-AKI and to investigate incorporation of biomarkers into its definition, to help identify sub-phenotypes that could drive post-CS-AKI care.
Extracorporeal Membrane Oxygenation
Children receiving extracorporeal membrane oxygenation (ECMO) represent some of the most critically ill patients and are at high risk of developing AKI for reasons inherent to their underlying disease process (hypotension, sepsis, cardiac failure, nephrotoxic medication exposure) as well as for factors related to provision of ECMO (blood flow characteristics, systemic inflammation, hypercoagulable state, hemolysis) [44]. Early single-center reports confirmed this by documenting that infants requiring ECMO following congenital heart surgery and neonates with congenital diaphragmatic hernia (CDH) receiving ECMO have an incidence of AKI of up to 72% [45, 46]. In a large 14-year study of 242 ECMO-treated neonates, 64% experienced AKI [47]. Each of these single-center studies demonstrated an association between severe AKI and worsened outcomes. The Kidney Interventions During Extracorporeal Membrane Oxygenation (KIDMO) study group performed a retrospective, observational, multicenter cohort study of 834 neonatal and pediatric patients receiving ECMO at 6 centers over 5 years [48••]. In this cohort, the incidence of AKI was 74%, with 93% of episodes occurring within 48 h of cannulation. There was also a significant association between AKI and outcomes including mortality (aOR 2.5) and length of ECMO [48••].
Subsequently, the KDIMO study group evaluated the epidemiology and impact of FO on outcomes [49•]. This study showed that FO is common in children on ECMO with median peak FO of 30.9% (IQR 15.4–54.8); additionally, peak FO predicted in-hospital mortality and increased length of ECMO after multivariable analysis [49•]. This data, coupled with previous work demonstrating that earlier CRRT initiation improves fluid management and prevents FO in neonates on ECMO, raises questions about the role for early initiation of CRRT in children on ECMO [50, 51]. A multicenter trial evaluating this question is greatly needed.
Neonates
Over the past 10 years, neonatal AKI has seen a rapid expansion of our knowledge on the subject with dozens of studies examining risk factors, epidemiology, and outcomes associated with AKI in a variety of at-risk populations (Table 3). Specific neonatal populations that have been studied include sick term/near term infants, neonates with perinatal asphyxia, very low birthweight infants (VLBW), extremely low birthweight infants, and neonates with concurrent disease processes including necrotizing enterocolitis (NEC), CDH, and intraventricular hemorrhage (IVH). In each of these studies, AKI occurred commonly and was associated with adverse outcomes (length of stay, mechanical ventilation, mortality). Furthermore, in those with perinatal asphyxia undergoing therapeutic hypothermia, AKI has been shown to be independently associated with adverse neurologic outcomes including hypoxic-ischemic MRI findings at postnatal days 7–10 [70]. While these studies provide important epidemiologic information, they are limited in their single-center nature, again making generalizations difficult.
In 2017, the AWAKEN study was published by the Neonatal Kidney Collaborative [17••]. This study was performed at 24 centers worldwide and included all neonates admitted to a level II or III neonatal intensive care units (NICU) who received intravenous fluids for ≥ 48 h between January 1 and March 31, 2014. The incidence of AKI was 30% in the 2022 neonates and differed by gestational age (48% in those < 29 weeks, 18% in those 29 weeks to < 36 weeks, 37% in those ≥ 36 weeks). Multivariable analysis documented a clear association between AKI and outcomes including mortality (aOR 4.6, p < 0·0001) and increased length of stay (adjusted parameter estimate 8.8 days, p < 0·0001). This was the first study to systematically evaluate the inclusion of urine output criteria in the definition of neonatal AKI and showed that urine output contributes significantly to the definition of AKI in neonates. Another critical finding in this study is the broad center-level variability in serum creatinine testing, varying from a median of 1 SCr measurement per neonate (IQR 1.1) to 11 [3•, 26] during the entirety of NICU admission. Furthermore, 10 centers had a median number of SCr checked of ≤3. The AWAKEN study provides critical epidemiologic data and will serve to continue to expand our knowledge about multiple topics including a refinement of the definition of neonatal AKI, the impact of fluid balance, and the impact of AKI on a variety of outcomes (bronchopulmonary dysplasia, IVH) [17••].
General Pediatric and Specific Populations
With the recognition of the incidence and impact of AKI on outcomes in critically ill populations, there has been increasing interest in studying the impact of AKI outside of the critical care setting. In a study of 13,914 non-critically ill pediatric admissions between 2011 and 2012 at a tertiary care hospital, the incidence of AKI was found to be at least 5%. More importantly, this study showed that 17% of admissions had ≥ 2 serum creatinine values checked. Of those that had two or more SCr checked, the incidence of AKI was 30%. The authors argue that there needs to be improved surveillance and recognition of AKI on general pediatric floors [75]. In a single-center study of pediatric emergency department visits over 1 year at a large academic center, the incidence of community-acquired AKI was 1.5%. This study also showed that only 19% of these episodes were recognized by the treating physician [76]. Each of these studies argues for improved recognition and surveillance in general pediatric populations.
Nephrotoxic Medication Exposure
Children exposed to nephrotoxic medications represent a patient population at particular risk for AKI irrespective of their location in the hospital. It is critical that providers understand this risk and identify those at risk, as nephrotoxic medication exposure may be the single most modifiable risk factor for the development of AKI in hospitalized patients. Epidemiologic studies clearly identify sub-populations at risk including, but not limited to, those exposed to aminoglycosides, non-steroidal anti-inflammatory drugs, vancomycin with piperacillin/tazobactam, or multiple nephrotoxins concurrently [77,78,79]. Recent work has suggested that AKI induced by nephrotoxic medications has long-standing consequences with evidence of residual kidney damage at 6-month follow-up in 70% of a cohort of 100 children with nephrotoxic medication-induced AKI [80].
The magnitude of this problem led to the development and implementation of electronic medical record (EMR) surveillance initiatives aimed at identifying and ultimately decreasing the rates of nephrotoxic medication-induced AKI. In 2013, Goldstein et al. first reported on a surveillance system called Nephrotoxic Injury Negated by Just-in-time Action (NINJA). This study utilized the EMR to identify patients at risk of AKI (intravenous aminoglycosides ≥ 3 days or ≥ 3 nephrotoxic medications) and subsequently trigger renal function monitoring with daily SCr. In the initial and follow-up studies, the authors showed that such a system could be deployed through a multidisciplinary effort on an institutional level and the quality improvement initiative could be sustained over time [81, 82••]. The sustained effort resulted in a 64% decrease in AKI rate over the 43-month study period [82••].
Early Recognition, Therapeutics, and Interventions and Advancements
Early Recognition
Despite significant advances in our understanding of the risk factors, epidemiology, and outcomes associated with AKI, there has been little progress in the development of new therapeutic options for neonates and children with AKI. Our current therapeutic repertoire is largely limited to patient optimization (nutrition, renal perfusion), prevention (decreased nephrotoxic medication exposure, improved surveillance), and management of sequelae (FO, etc.) The failure to develop and execute successful interventional trials stems at least in part from the utilization of SCr as a biomarker. SCr has a number of limitations including a delay in rise after insult, and, more importantly, it is solely a marker of kidney function instead of injury. Based on these characteristics, it is not surprising that studies utilizing rise in SCr as entry criteria, or even as endpoints, have been unsuccessful. As a result, there has been a significant amount of research to identify novel biomarkers to allow for the earlier recognition and diagnosis of AKI [83].
The identification and study of the “novel” AKI biomarkers largely began in patients undergoing CPB where insult timing is largely known. These biomarkers detect damage, rather than describe function, and include urine neutrophil gelatinase-associated lipocalin (NGAL), kidney injury molecule-1, interleukin 18, liver fatty acid binding protein, and others [84]. Each of these biomarkers has been shown to rise 2–12 h following an insult, and each was predictive of AKI at 48 h in several studies [84]. As with any biomarker in medicine, when these are used indiscriminately, they perform very poorly. However, when used in conjunction with risk factor assessments, these biomarkers provide significant promise to improve care and clinical trials in AKI [84].
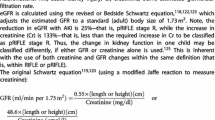
A critical step to improve the care of children with AKI is to shift the focus to earlier identification of AKI. While biomarkers undoubtedly play a role in this, it is critical to risk-stratify patients in order to optimally deploy biomarkers. The first effort to systematically risk-stratify critically ill pediatric patients has come in the form of the Renal Angina Index (RAI). The RAI is a scoring system derived from existing literature based on clinical risk factors for AKI (pediatric ICU admission, stem cell transplant, mechanical ventilation, ionotrope utilization) and signs of injury (FO, rise in SCR; Fig. 1) [85,86,87]. In 2014, Basu et al. described the derivation and validation of the RAI in four cohorts of critically ill children. In this study, the RAI performed very well with a negative predictive value of > 92% for severe day 3 AKI [86]. A follow-up single-center, prospective trial in 184 critically ill children further validated the RAI and, more importantly, showed that the addition of urinary NGAL significantly increased the ability of the RAI to predict severe day 3 AKI (AUC/ROC 0.80 to 0.97) [88]. The RAI has subsequently been studied and validated in a single-center study and in the multicenter AWARE study [89, 90••].
Another important component in the improved care of children with AKI is the development of a functional kidney test to identify the patients at highest risk for severe AKI. The “furosemide stress test” (FST) represents such a test and utilizes a single dose of furosemide followed by a 6-h period of monitored urine response to identify patients at risk for severe AKI. In a study of adults, urine output < 200 ml in the first 2 h had a sensitivity of 87.1% and specificity 84.1% to predict the development of stage 3 AKI [91]. A recent single-center study of 99 children undergoing cardiac surgery supports this concept. In this study, the furosemide response in the first 24 h following cardiac surgery predicted subsequent AKI and FO [92]. This is consistent with another recent study in children following cardiac surgery [93]. While the RAI, novel biomarkers, and FST all represent interesting tools, the answer for early AKI identification undoubtedly lies in a multi-faceted approach incorporating many, if not all, of these tools.
Therapeutics
While there remains a paucity of medical interventions for established AKI, in recent years, there have been several important studies that have evaluated the ability of medications to prevent the development and/or progression of AKI in high-risk populations. Here, we will review recent studies evaluating aminophylline/theophylline, caffeine, dexmedetomidine, and rasburicase.
Theophylline, caffeine, and aminophylline are adenosine receptor antagonists that have recently shown promise as agents that may prevent or ameliorate AKI in high-risk populations (congenital cardiac surgery, perinatal asphyxia, and premature neonates) [55, 64, 94,95,96,97,98,99]. These medications impact renal perfusion by inhibiting adenosine-induced vasoconstriction. There have now been four randomized controlled trials evaluating the impact of a single dose of theophylline given in the first hour of life on renal function in neonates suffering from perinatal asphyxia. The most recent of these trials was published in 2016 and included 159 neonates with perinatal asphyxia. This study showed that those that received theophylline had less AKI (15% vs 48%, p < 0.01), less oliguria, and better fluid balance at postnatal day 3 [99]. While these positive studies have clearly shown promise for the utilization of theophylline in this population, theophylline has to be studied in a population undergoing therapeutic hypothermia.
In premature neonates, caffeine is commonly utilized to prevent and/or treat apnea of prematurity and its impact on AKI has recently drawn interest. In a single-center retrospective study of 140 VLBW neonates, caffeine exposure was associated with less AKI (aOR 0.21) [64]. These findings were confirmed in a secondary analysis of 675 premature neonates in the AWAKEN study, where after multivariable adjustment, administration of caffeine reduced the odds of developing AKI (aOR, 0.20), indicating that for every 4.3 neonates exposed to caffeine, a case of AKI was prevented [55].
Children undergoing cardiac surgery represent a population where there have been a number of recent studies evaluating a variety of agents to prevent or ameliorate AKI. Aminophylline initially has shown promise in a single-center retrospective study of children with AKI following cardiac surgery, which demonstrated improved renal function and urine output in those treated with aminophylline. A well done follow-up single-center double-blinded, placebo-controlled, randomized clinical trial showed no impact on AKI or fluid balance in those treated for 72 h with aminophylline following CPB [98]. Dexmedetomidine is an α2-adrenergic receptor agonist that has been reported to be renal protective in adults after heart surgery [100]. A single-center study of 29 children undergoing atrial or ventricular septal defect repair suggested that dexmedetomidine may decrease the incidence of postoperative AKI. Each of these agents warrants further study.
Rasburicase is a recombinant urate oxidase that catalyzes the conversion of uric acid to allantoin and has been used extensively to treat hyperuricemia associated with tumor lysis syndrome. A number of case reports have shown successful use of rasburicase in the treatment of severe hyperuricemia associated with AKI in a variety of populations including neonates, rhabdomyolysis, and pediatric patients with hemolytic uremic syndrome [101,102,103,104]. Currently, firm recommendations about its use cannot be made, and additional studies investigating the role of hyperuricemia and its status as a modifiable risk factor in AKI and the use of rasburicase are needed.
Interventions and Advancements
The indications for renal replacement therapy (RRT) in children with AKI include uremia (typically blood urea nitrogen (BUN) > 100–120 mg/dl), electrolyte abnormalities, inability to provide adequate nutrition, and FO. CRRT has become one of the more commonly prescribed modalities for delivering RRT in critically ill children. This has been done utilizing devices designed for adults, creating significant challenges in providing CRRT to our smallest patients. The development of CRRT devices that are specifically designed for neonates and small infants (smaller extracorporeal volumes, improved precision, lower blood flows, smaller catheters) will revolutionize our ability to provide this therapy to our smallest patients. Two such machines include the CARPEDIEM® (Cardio-Renal Pediatric Dialysis Emergency Machine), which is currently in use outside of North America, and NIDUS® (Newcastle Infant Dialysis and Ultrafiltration System) [105, 106]. The timely mobilization of these devices is critical to improving outcomes for our smallest patients.
Over the last decade, pediatricians have been at the forefront of identifying the association of FO at CRRT initiation with increased mortality [24, 49•, 107,108,109]. These studies clearly suggest that FO of 10–20% represents a critical point when providers must consider intervention with RRT in critically ill infants and children. In those receiving ECMO, FO of 20–30% likely represents an important benchmark based on the current literature [49•]. The timing for the initiation of RRT remains a critical area for further study in children.
Long-Term Outcomes
In recent years, it has become clear that the implications of AKI extend beyond short-term morbidity and mortality to include an increased risk of subsequent chronic kidney disease (CKD). This association has been clearly shown in the adult literature, and an association is being shown in small pediatric studies with increasing frequency [80, 110,111,112,113]. The seminal pediatric publication on this topic was published in 2012 and evaluated renal outcomes at 1–3 years following an AKI episode during critical care in 126 patients. Ten percent of patients had evidence of chronic kidney disease (GFR < 60 ml/min/1.73 m2), and an additional 47% were at risk for CKD (GFR of 60–90 ml/min/1.73 m2, persistent hypertension, and/or hyperfiltration (≥ 150 ml/min/1.73 m2)) [111]. Subsequent small single-center studies have shown abnormal long-term renal function in those with AKI following nephrotoxic medication exposure, VLBW neonates, and CPB-associated AKI [80, 113, 114]. While there appears to be a signal present, confirmation with long-term follow-up studies of cohorts such as AWARE and AWAKEN are critical. Based upon expert opinion, the KDIGO guidelines currently recommend follow-up evaluation after an episode of AKI within 3 months of hospital discharge [10••].
Conclusion
In recent years, there have been many exciting advances in neonatal and pediatric AKI. Through the utilization of standardized definitions, there has been a revolution in understanding the epidemiology and impact of AKI across all populations in pediatrics. This has culminated in the recent publication of the AWARE and AWAKEN studies, which definitively describe the incidence and negative impact of AKI in pediatric and neonatal populations, respectively. Efforts now must turn to the prevention, early recognition, and therapies for AKI. The NINJA study clearly demonstrates the importance of standardized protocols to improve surveillance in patients receiving nephrotoxic medications. Translating these protocols to the ICUs, including increased monitoring of neonatal renal function, is a critical next step to improving short- and long-term outcomes. In addition, the further deployment and development of risk stratification strategies (RAI, FST), coupled with the utilization of novel biomarkers, have the opportunity to change the paradigm of AKI from one of the reactions to one of the early interventions.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Basu RK, Devarajan P, Wong H, Wheeler DS. An update and review of acute kidney injury in pediatrics. Pediatr Crit Care Med. 2011;12(3):339–47.
Devarajan P. Update on mechanisms of ischemic acute kidney injury. J Am Soc Nephrol. 2006;17(6):1503–20.
• Selewski DT, Charlton JR, Jetton JG, Guillet R, Mhanna MJ, Askenazi DJ, et al. Neonatal acute kidney injury. Pediatrics. 2015;136(2):e463–73 This state of the art review is leading publication on neonatal acute kidney injury. This artile was written by members of the Neonatal Kidney Collaborative .
Jose PA, Fildes RD, Gomez RA, Chevalier RL, Robillard JE. Neonatal renal function and physiology. Curr Opin Pediatr. 1994;6(2):172–7.
Su SW, Stonestreet BS. Core Concepts: Neonatal Glomerular Filtration Rate. NeoReviews. 2010;11(12):e714–21.
Lameire N, Van Biesen W, Vanholder R. Acute renal failure. Lancet. 2005;365(9457):417–30.
Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P. Acute Dialysis quality initiative w. acute renal failure - definition, outcome measures, animal models, fluid therapy and information technology needs: the second international consensus conference of the acute Dialysis quality initiative (ADQI) group. Crit Care. 2004;8(4):R204–12.
Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, et al. Acute kidney injury network: report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007;11(2):R31.
Akcan-Arikan A, Zappitelli M, Loftis LL, Washburn KK, Jefferson LS, Goldstein SL. Modified RIFLE criteria in critically ill children with acute kidney injury. Kidney Int. 2007;71(10):1028–35.
•• Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO Clinical Practice Guideline for Acute Kidney Injury. Kidney inter. Suppl. 2012(2):1–138. This manuscipt outlines the consensus guidelines on the diagnosis and management of AKI put forth by the Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. This working group represents international experts in the field of adult, pediatric, and neonatal AKI.
Selewski DT, Cornell TT, Heung M, Troost JP, Ehrmann BJ, Lombel RM, et al. Validation of the KDIGO acute kidney injury criteria in a pediatric critical care population. Intensive Care Med. 2014;40(10):1481–8.
•• Kaddourah A, Basu RK, Bagshaw SM, Goldstein SL, Investigators A. Epidemiology of acute kidney injury in critically ill children and young adults. N Engl J Med. 2017;376(1):11–20 The assessment of worldwide acute kidney injury, Renal Angina and Epidemiology in critically ill children (AWARE) study is the seminal publication describing the incidence and implication of AKI in the largest multi-center cohort to date .
Fortenberry JD, Paden ML, Goldstein SL. Acute kidney injury in children: an update on diagnosis and treatment. Pediatr Clin N Am. 2013;60(3):669–88.
Jetton JG, Rhone ET, Harer MW, Charlton JR, Selewski DT. Diagnosis and treatment of acute kidney injury in pediatrics. Curr Treat Options Pediatr. 2016;2(2):56–68.
Jetton JG, Askenazi DJ. Update on acute kidney injury in the neonate. Curr Opin Pediatr. 2012;24(2):191–6.
Zappitelli M, Ambalavanan N, Askenazi DJ, Moxey-Mims MM, Kimmel PL, Star RA, et al. Developing a neonatal acute kidney injury research definition: a report from the NIDDK neonatal AKI workshop. Pediatr Res. 2017;82(4):569–73.
•• Jetton JG, Boohaker LJ, Sethi SK, Wazir S, Rohatgi S, Soranno DE, et al. Incidence and outcomes of neonatal acute kidney injury (AWAKEN): a multicentre, multinational, observational cohort study. Lancet Child Adolesc Health. 2017;1(3):184–94 The Assessment of Worldwide Acute Kidney injury Epidemiology in Neonates (AWARKEN) study is the seminal publication describing the incidence and implication of neonatal AKI in the largest multi-center cohort to date .
Blinder JJ, Asaro LA, Wypij D, Selewski DT, Agus MSD, Gaies M, et al. Acute kidney injury after pediatric cardiac surgery: a secondary analysis of the safe pediatric Euglycemia after cardiac surgery trial. Pediatr Crit Care Med. 2017;18(7):638–46.
Cornell TT, Selewski DT, Alten JA, Askenazi D, Fitzgerald JC, Topjian A, et al. Acute kidney injury after out of hospital pediatric cardiac arrest. Resuscitation. 2018;131:63–8.
Criss CN, Selewski DT, Sunkara B, Gish JS, Hsieh L, McLeod JS, et al. Acute kidney injury in necrotizing enterocolitis predicts mortality. Pediatr Nephrol. 2018;33(3):503–10.
Alkandari O, Eddington KA, Hyder A, Gauvin F, Ducruet T, Gottesman R, et al. Acute kidney injury is an independent risk factor for pediatric intensive care unit mortality, longer length of stay and prolonged mechanical ventilation in critically ill children: a two-center retrospective cohort study. Crit Care. 2011;15(3):R146.
Blinder JJ, Goldstein SL, Lee VV, Baycroft A, Fraser CD, Nelson D, et al. Congenital heart surgery in infants: effects of acute kidney injury on outcomes. J Thorac Cardiovasc Surg. 2012;143(2):368–74.
Schneider J, Khemani R, Grushkin C, Bart R. Serum creatinine as stratified in the RIFLE score for acute kidney injury is associated with mortality and length of stay for children in the pediatric intensive care unit. Crit Care Med. 2010;38(3):933–9.
Goldstein SL, Currier H, Graf C, Cosio CC, Brewer ED, Sachdeva R. Outcome in children receiving continuous venovenous hemofiltration. Pediatrics. 2001;107(6):1309–12.
Selewski DT, Cornell TT, Lombel RM, Blatt NB, Han YY, Mottes T, et al. Weight-based determination of fluid overload status and mortality in pediatric intensive care unit patients requiring continuous renal replacement therapy. Intensive Care Med. 2011;37(7):1166–73.
Askenazi DJ, Koralkar R, Hundley HE, Montesanti A, Patil N, Ambalavanan N. Fluid overload and mortality are associated with acute kidney injury in sick near-term/term neonate. Pediatr Nephrol. 2013;28(4):661–6.
Lane PH, Mauer SM, Blazar BR, Ramsay NK, Kashtan CE. Outcome of dialysis for acute renal failure in pediatric bone marrow transplant patients. Bone Marrow Transplant. 1994;13(5):613–7.
Hazle MA, Gajarski RJ, Yu S, Donohue J, Blatt NB. Fluid overload in infants following congenital heart surgery. Pediatr Crit Care Med. 2013;14(1):44–9.
Bontant T, Matrot B, Abdoul H, Aizenfisz S, Naudin J, Jones P, et al. Assessing fluid balance in critically ill pediatric patients. Eur J Pediatr. 2015;174(1):133–7.
van Asperen Y, Brand PL, Bekhof J. Reliability of the fluid balance in neonates. Acta Paediatr. 2012;101(5):479–83.
Selewski DT, Goldstein SL. The role of fluid overload in the prediction of outcome in acute kidney injury. Pediatr Nephrol. 2018;33(1):13–24.
Mehta RL, Cerda J, Burdmann EA, Tonelli M, Garcia-Garcia G, Jha V, et al. International Society of Nephrology's 0by25 initiative for acute kidney injury (zero preventable deaths by 2025): a human rights case for nephrology. Lancet. 2015;385(9987):2616–43.
Villacrés SM, Medar SS, Aydin SI. Acute Kidney Injury in Children With Acute Respiratory Failure. Clin Pediatr. 2018;57(11):1340–48. https://doi.org/10.1177/0009922818779222.
Deep A, Sagar H, Goonasekera C, Karthikeyan P, Brierley J, Douiri A. Evolution of acute kidney injury and its association with systemic hemodynamics in children with fluid-refractory septic shock. Crit Care Med. 2018;46(7):e677–e83.
Fitzgerald JC, Ross ME, Thomas NJ, Weiss SL, Balamuth F, Anderson AH. Risk factors and inpatient outcomes associated with acute kidney injury at pediatric severe sepsis presentation. Pediatr Nephrol. 2018.
Fitzgerald JC, Basu RK, Akcan-Arikan A, Izquierdo LM, Pineres Olave BE, Hassinger AB, et al. Acute kidney injury in pediatric severe Sepsis: an independent risk factor for death and new disability. Crit Care Med. 2016;44(12):2241–50.
Palmieri T, Lavrentieva A, Greenhalgh D. An assessment of acute kidney injury with modified RIFLE criteria in pediatric patients with severe burns. Intensive Care Med. 2009;35(12):2125–9.
Aydin SI, Seiden HS, Blaufox AD, Parnell VA, Choudhury T, Punnoose A, et al. Acute kidney injury after surgery for congenital heart disease. Ann Thorac Surg. 2012;94(5):1589–95.
Taylor ML, Carmona F, Thiagarajan RR, Westgate L, Ferguson MA, del Nido PJ, et al. Mild postoperative acute kidney injury and outcomes after surgery for congenital heart disease. J Thorac Cardiovasc Surg. 2013;146(1):146–52.
Ueno K, Seki S, Shiokawa N, Matsuba T, Miyazono A, Hazeki D, et al. Validation of acute kidney injury according to the modified KDIGO criteria in infants after cardiac surgery for congenital heart disease. Nephrology. 2018;1–29. https://doi.org/10.1111/nep.13240.
Zappitelli M, Bernier PL, Saczkowski RS, Tchervenkov CI, Gottesman R, Dancea A, et al. A small post-operative rise in serum creatinine predicts acute kidney injury in children undergoing cardiac surgery. Kidney Int. 2009;76(8):885–92.
Basu RK, Wong HR, Krawczeski CD, Wheeler DS, Manning PB, Chawla LS, et al. Combining functional and tubular damage biomarkers improves diagnostic precision for acute kidney injury after cardiac surgery. J Am Coll Cardiol. 2014;64(25):2753–62.
Lex DJ, Toth R, Cserep Z, Alexander SI, Breuer T, Sapi E, et al. A comparison of the systems for the identification of postoperative acute kidney injury in pediatric cardiac patients. Ann Thorac Surg. 2014;97(1):202–10.
Askenazi DJ, Selewski DT, Paden ML, Cooper DS, Bridges BC, Zappitelli M, et al. Renal replacement therapy in critically ill patients receiving extracorporeal membrane oxygenation. Clin J Am Soc Nephrol. 2012;7(8):1328–36.
Smith AH, Hardison DC, Worden CR, Fleming GM, Taylor MB. Acute renal failure during extracorporeal support in the pediatric cardiac patient. ASAIO J. 2009;55(4):412–6.
Gadepalli SK, Selewski DT, Drongowski RA, Mychaliska GB. Acute kidney injury in congenital diaphragmatic hernia requiring extracorporeal life support: an insidious problem. J Pediatr Surg. 2011;46(4):630–5.
Zwiers AJ, de Wildt SN, Hop WC, Dorresteijn EM, Gischler SJ, Tibboel D, et al. Acute kidney injury is a frequent complication in critically ill neonates receiving extracorporeal membrane oxygenation: a 14-year cohort study. Crit Care. 2013;17(4):R151.
•• Fleming GM, Sahay R, Zappitelli M, King E, Askenazi DJ, Bridges BC, et al. The Incidence of Acute Kidney Injury and Its Effect on Neonatal and Pediatric Extracorporeal Membrane Oxygenation Outcomes: A Multicenter Report From the Kidney Intervention During Extracorporeal Membrane Oxygenation Study Group. Pediatr Crit Care Med. 2016;17(12):1157–69 This manuscript put forth by the the Kidney Interventions During Extracorporeal Membrane Oxygenation (KIDMO) study group is the first multicenter study describing the incidence and impact of AKI in pediatric ECMO .
• Selewski DT, Askenazi DJ, Bridges BC, Cooper DS, Fleming GM, Paden ML, et al. The impact of fluid overload on outcomes in children treated with extracorporeal membrane oxygenation: a multicenter retrospective cohort study. Pediatr Crit Care Med. 2017;18(12):1126–35 This manuscript put forth by the the Kidney Interventions During Extracorporeal Membrane Oxygenation (KIDMO) study group is the first multicenter study describing the incidence and impact of fluid overload in pediatric ECMO.
Murphy HJ, Cahill JB, Twombley KE, Annibale DJ, Kiger JR. Implementing a practice change: early initiation of continuous renal replacement therapy during neonatal extracorporeal life support standardizes care and improves short-term outcomes. J Artif Organs. 2018;21(1):76–85.
Hoover NG, Heard M, Reid C, Wagoner S, Rogers K, Foland J, et al. Enhanced fluid management with continuous venovenous hemofiltration in pediatric respiratory failure patients receiving extracorporeal membrane oxygenation support. Intensive Care Med. 2008;34(12):2241–7.
Chowdhary V, Vajpeyajula R, Jain M, Maqsood S, Raina R, Kumar D, et al. Comparison of different definitions of acute kidney injury in extremely low birth weight infants. Clin Exp Nephrol. 2018;22(1):117–25.
Velazquez DM, Reidy KJ, Sharma M, Kim M, Vega M, Havranek T. The effect of hemodynamically significant patent ductus arteriosus on acute kidney injury and systemic hypertension in extremely low gestational age newborns. The Journal of Maternal-Fetal & Neonatal Medicine. 2018:0(0);1–6. https://doi.org/10.1080/14767058.2018.1460349.
Bakhoum CY, Basalely A, Koppel RI, Sethna CB. Acute kidney injury in preterm infants with necrotizing enterocolitis. The Journal of Maternal-Fetal & Neonatal Medicine 2018:0(0);1–6. https://doi.org/10.1080/14767058.2018.1459553.
Harer MW, Askenazi DJ, Boohaker LJ, Carmody JB, Griffin RL, Guillet R, et al. Association between early caffeine citrate administration and risk of acute kidney injury in preterm neonates: results from the AWAKEN study. JAMA Pediatr. 2018;172(6):e180322.
SooHoo MM, Patel SS, Jaggers J, Faubel S, Gist KM. Acute kidney injury defined by fluid corrected creatinine in neonates after the Norwood procedure. World J Pediatr Congenit Heart Surg. 2018;9(5):513–21.
Garcia RU, Natarajan G, Walters HL, Delius RE, Aggarwal S. Acute kidney injury following first-stage palliation in hypoplastic left heart syndrome: hybrid versus Norwood palliation. Cardiol Young. 2018;28(2):261–8.
Srinivasan N, Schwartz A, John E, Price R, Amin S. Acute kidney injury impairs postnatal renal adaptation and increases morbidity and mortality in very low-birth-weight infants. Am J Perinatol. 2018;35(1):39–47.
Chock VY, Frymoyer A, Yeh CG, Van Meurs KP. Renal saturation and acute kidney injury in neonates with hypoxic ischemic encephalopathy undergoing therapeutic hypothermia. J Pediatr. 2018;200:232–9 e1.
Carlo WF, Clark ST, Borasino S, Alten JA. Impact of contrast exposure from computed tomography angiography on acute kidney injury after neonatal cardiopulmonary bypass surgery. Congenit Heart Dis. 2017;12(4):540–5.
Maqsood S, Fung N, Chowdhary V, Raina R, Mhanna MJ. Outcome of extremely low birth weight infants with a history of neonatal acute kidney injury. Pediatr Nephrol. 2017;32(6):1035–43.
Constance JE, Reith D, Ward RM, Balch A, Stockmann C, Korgenski EK, et al. Risk of nonsteroidal anti-inflammatory drug-associated renal dysfunction among neonates diagnosed with patent ductus arteriosus and treated with gentamicin. J Perinatol. 2017;37(10):1093–102.
Stoops C, Sims B, Griffin R, Askenazi DJ. Neonatal acute kidney injury and the risk of intraventricular hemorrhage in the very low birth weight infant. Neonatology. 2016;110(4):307–12.
Carmody JB, Harer MW, Denotti AR, Swanson JR, Charlton JR. Caffeine exposure and risk of acute kidney injury in a retrospective cohort of very low birth weight neonates. J Pediatr. 2016;172:63–8 e1.
Weintraub AS, Connors J, Carey A, Blanco V, Green RS. The spectrum of onset of acute kidney injury in premature infants less than 30 weeks gestation. J Perinatol. 2016;36(6):474–80.
Wong JH, Selewski DT, Yu S, Leopold KE, Roberts KH, Donohue JE, et al. Severe acute kidney injury following stage 1 Norwood palliation: effect on outcomes and risk of severe acute kidney injury at subsequent surgical stages. Pediatr Crit Care Med. 2016;17(7):615–23.
Kumar TK, Allen Ccp J, Spentzas Md T, Berrios Ccp L, Shah Md S, Joshi Md VM, et al. Acute kidney injury following cardiac surgery in neonates and young infants: experience of a single center using novel perioperative strategies. World J Pediatr Congenit Heart Surg. 2016;7(4):460–6.
Askenazi D, Patil NR, Ambalavanan N, Balena-Borneman J, Lozano DJ, Ramani M, et al. Acute kidney injury is associated with bronchopulmonary dysplasia/mortality in premature infants. Pediatr Nephrol. 2015;30(9):1511–8.
Piggott KD, Soni M, Decampli WM, Ramirez JA, Holbein D, Fakioglu H, et al. Acute kidney injury and fluid overload in neonates following surgery for congenital heart disease. World J Pediatr Congenit Heart Surg. 2015;6(3):401–6.
Sarkar S, Askenazi DJ, Jordan BK, Bhagat I, Bapuraj JR, Dechert RE, et al. Relationship between acute kidney injury and brain MRI findings in asphyxiated newborns after therapeutic hypothermia. Pediatr Res. 2014;75(3):431–5.
Carmody JB, Swanson JR, Rhone ET, Charlton JR. Recognition and Reporting of AKI in Very Low Birth Weight Infants. Clin J Am Soc Nephrol. 2014;9(12):2036–43.
Rhone ET, Carmody JB, Swanson JR, Charlton JR. Nephrotoxic medication exposure in very low birth weight infants. J Matern Fetal Neonatal Med. 2014;27(14):1485–90.
Selewski DT, Jordan BK, Askenazi DJ, Dechert RE, Sarkar S. Acute kidney injury in asphyxiated newborns treated with therapeutic hypothermia. J Pediatr. 2013;162(4):725–9 e1.
Alabbas A, Campbell A, Skippen P, Human D, Matsell D, Mammen C. Epidemiology of cardiac surgery-associated acute kidney injury in neonates: a retrospective study. Pediatr Nephrol. 2013;28(7):1127–34.
McGregor TL, Jones DP, Wang L, Danciu I, Bridges BC, Fleming GM, et al. Acute kidney injury incidence in noncritically ill hospitalized children, adolescents, and young adults: a retrospective observational study. Am J Kidney Dis. 2016;67(3):384–90.
Bernardo EO, Cruz AT, Buffone GJ, Devaraj S, Loftis LL, Arikan AA. Community-acquired acute kidney injury among children seen in the pediatric emergency department. Acad Emerg Med. 2018;25(7):758–68.
Zappitelli M, Moffett BS, Hyder A, Goldstein SL. Acute kidney injury in non-critically ill children treated with aminoglycoside antibiotics in a tertiary healthcare Centre: a retrospective cohort study. Nephrol Dial Transplant. 2011;26(1):144–50.
Misurac JM, Knoderer CA, Leiser JD, Nailescu C, Wilson AC, Andreoli SP. Nonsteroidal anti-inflammatory drugs are an important cause of acute kidney injury in children. J Pediatr. 2013;162(6):1153–9 9 e1.
Moffett BS, Goldstein SL. Acute kidney injury and increasing nephrotoxic-medication exposure in noncritically-ill children. Clin J Am Soc Nephrol. 2011;6(4):856–63.
Menon S, Kirkendall ES, Nguyen H, Goldstein SL. Acute kidney injury associated with high nephrotoxic medication exposure leads to chronic kidney disease after 6 months. J Pediatr. 2014;165(3):522–7 e2.
Goldstein SL, Kirkendall E, Nguyen H, Schaffzin JK, Bucuvalas J, Bracke T, et al. Electronic health record identification of nephrotoxin exposure and associated acute kidney injury. Pediatrics. 2013;132(3):e756–67.
•• Goldstein SL, Mottes T, Simpson K, Barclay C, Muething S, Haslam DB, et al. A sustained quality improvement program reduces nephrotoxic medication-associated acute kidney injury. Kidney Int. 2016;90(1):212–21 This manuscript describes the sustained success of utilizing the electronic medical rcord to idetify patients at risk for nephrotoxic medeictaion induced AKI. This is the follow-up manuscript to the 2013 Pediatrics manuscript describing the Nephrotoxic Injury Negated by Just-in-time Action (NINJA) study.
Coca SG, Yalavarthy R, Concato J, Parikh CR. Biomarkers for the diagnosis and risk stratification of acute kidney injury: a systematic review. Kidney Int. 2008;73(9):1008–16.
Goldstein SL. Acute kidney injury biomarkers: renal angina and the need for a renal troponin I. BMC Med. 2011;9:135.
Basu RK, Chawla LS, Wheeler DS, Goldstein SL. Renal angina: an emerging paradigm to identify children at risk for acute kidney injury. Pediatr Nephrol. 2012;27(7):1067–78.
Basu RK, Zappitelli M, Brunner L, Wang Y, Wong HR, Chawla LS, et al. Derivation and validation of the renal angina index to improve the prediction of acute kidney injury in critically ill children. Kidney Int. 2014;85(3):659–67.
Goldstein SL, Chawla LS. Renal angina. Clin J Am Soc Nephrol. 2010;5(5):943–9.
Menon S, Goldstein SL, Mottes T, Fei L, Kaddourah A, Terrell T, et al. Urinary biomarker incorporation into the renal angina index early in intensive care unit admission optimizes acute kidney injury prediction in critically ill children: a prospective cohort study. Nephrol Dial Transplant. 2016;31(4):586–94.
Kaur R, Dhooria GS, Pooni PA, Bhat D, Bhargava S, Kakkar S, et al. Utilization of the renal angina index in PICU of a developing country for prediction of subsequent severe acute kidney injury. Pediatr Nephrol. 2018.
•• Basu RK, Kaddourah A, Goldstein SL, Akcan-Arikan A, Arnold M, Cruz C, et al. Assessment of a renal angina index for prediction of severe acute kidney injury in critically ill children: a multicentre, multinational, prospective observational study. The Lancet Child & Adolescent Health. 2018;2(2):112–20 This publication showed that the renal angina index improved accuracy for prediction of severe acute kidney injury in critically ill children and young people utilizing the AWARE study cohort .
Chawla LS, Davison DL, Brasha-Mitchell E, Koyner JL, Arthur JM, Shaw AD, et al. Development and standardization of a furosemide stress test to predict the severity of acute kidney injury. Crit Care. 2013;17(5):R207.
Borasino S, Wall KM, Crawford JH, Hock KM, Cleveland DC, Rahman F, et al. Furosemide response predicts acute kidney injury after cardiac surgery in infants and neonates. Pediatr Crit Care Med. 2018;19(4):310–7.
Kakajiwala A, Kim JY, Hughes JZ, Costarino A, Ferguson J, Gaynor JW, et al. Lack of furosemide responsiveness predicts acute kidney injury in infants after cardiac surgery. Ann Thorac Surg. 2017;104(4):1388–94.
Jenik AG, Ceriani Cernadas JM, Gorenstein A, Ramirez JA, Vain N, Armadans M, et al. A randomized, double-blind, placebo-controlled trial of the effects of prophylactic theophylline on renal function in term neonates with perinatal asphyxia. Pediatrics. 2000;105(4):E45.
Bakr AF. Prophylactic theophylline to prevent renal dysfunction in newborns exposed to perinatal asphyxia--a study in a developing country. Pediatr Nephrol. 2005;20(9):1249–52.
Eslami Z, Shajari A, Kheirandish M, Heidary A. Theophylline for prevention of kidney dysfunction in neonates with severe asphyxia. Iran J Kidney Dis. 2009;3(4):222–6.
Axelrod DM, Anglemyer AT, Sherman-Levine SF, Zhu A, Grimm PC, Roth SJ, et al. Initial experience using aminophylline to improve renal dysfunction in the pediatric cardiovascular ICU. Pediatr Crit Care Med. 2014;15(1):21–7.
Axelrod DM, Sutherland SM, Anglemyer A, Grimm PC, Roth SJ. A double-blinded, randomized, placebo-controlled clinical trial of aminophylline to prevent acute kidney injury in children following congenital heart surgery with cardiopulmonary bypass. Pediatr Crit Care Med. 2016;17(2):135–43.
Raina A, Pandita A, Harish R, Yachha M, Jamwal A. Treating perinatal asphyxia with theophylline at birth helps to reduce the severity of renal dysfunction in term neonates. Acta Paediatr. 2016;105(10):e448–51.
Liu Y, Sheng B, Wang S, Lu F, Zhen J, Chen W. Dexmedetomidine prevents acute kidney injury after adult cardiac surgery: a meta-analysis of randomized controlled trials. BMC Anesthesiol. 2018;18(1):7.
Hobbs DJ, Steinke JM, Chung JY, Barletta GM, Bunchman TE. Rasburicase improves hyperuricemia in infants with acute kidney injury. Pediatr Nephrol. 2010;25(2):305–9.
Lin PY, Lin CC, Liu HC, Lee MD, Lee HC, Ho CS, et al. Rasburicase improves hyperuricemia in patients with acute kidney injury secondary to rhabdomyolysis caused by ecstasy intoxication and exertional heat stroke. Pediatr Crit Care Med. 2011;12(6):e424–7.
Acosta AA, Hogg RJ. Rasburicase for hyperuricemia in hemolytic uremic syndrome. Pediatr Nephrol. 2012;27(2):325–9.
Canpolat FE, Cekmez F. Rasburicase for hyperuricemia in an extremely low birth weight infant. Indian Pediatr. 2011;48(7):573–4.
Coulthard MG, Crosier J, Griffiths C, Smith J, Drinnan M, Whitaker M, et al. Haemodialysing babies weighing <8 kg with the Newcastle infant dialysis and ultrafiltration system (Nidus): comparison with peritoneal and conventional haemodialysis. Pediatr Nephrol. 2014;29(10):1873–81.
Ronco C, Garzotto F, Brendolan A, Zanella M, Bellettato M, Vedovato S, et al. Continuous renal replacement therapy in neonates and small infants: development and first-in-human use of a miniaturised machine (CARPEDIEM). Lancet. 2014;383(9931):1807–13.
Goldstein SL, Somers MJ, Baum MA, Symons JM, Brophy PD, Blowey D, et al. Pediatric patients with multi-organ dysfunction syndrome receiving continuous renal replacement therapy. Kidney Int. 2005;67(2):653–8.
Hayes LW, Oster RA, Tofil NM, Tolwani AJ. Outcomes of critically ill children requiring continuous renal replacement therapy. J Crit Care. 2009;24(3):394–400.
Sutherland SM, Zappitelli M, Alexander SR, Chua AN, Brophy PD, Bunchman TE, et al. Fluid overload and mortality in children receiving continuous renal replacement therapy: the prospective pediatric continuous renal replacement therapy registry. Am J Kidney Dis. 2010;55(2):316–25.
Coca SG, Singanamala S, Parikh CR. Chronic kidney disease after acute kidney injury: a systematic review and meta-analysis. Kidney Int. 2012;81(5):442–8.
Mammen C, Al Abbas A, Skippen P, Nadel H, Levine D, Collet JP, et al. Long-term risk of CKD in children surviving episodes of acute kidney injury in the intensive care unit: a prospective cohort study. Am J Kidney Dis. 2012;59(4):523–30.
Greenberg JH, Coca S, Parikh CR. Long-term risk of chronic kidney disease and mortality in children after acute kidney injury: a systematic review. BMC Nephrol. 2014;15:184.
Harer MW, Pope CF, Conaway MR, Charlton JR. Follow-up of acute kidney injury in neonates during childhood years (FANCY): a prospective cohort study. Pediatr Nephrol. 2017;32(6):1067–76.
Cooper DS, Claes D, Goldstein SL, Bennett MR, Ma Q, Devarajan P, et al. Follow-up renal assessment of injury long-term after acute kidney injury (FRAIL-AKI). Clin J Am Soc Nephrol. 2016;11(1):21–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Stephen M. Gorga and Heidi J. Murphy should receive credit as co-first authors
This article is part of the Topical Collection on Renal
Rights and permissions
About this article
Cite this article
Gorga, S.M., Murphy, H.J. & Selewski, D.T. An Update on Neonatal and Pediatric Acute Kidney Injury. Curr Pediatr Rep 6, 278–290 (2018). https://doi.org/10.1007/s40124-018-0184-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40124-018-0184-5