Abstract
Hidradenitis suppurativa (HS) is a relatively common chronic inflammatory disease with immune dysregulation. While eye manifestations of HS are rare, a dilemma arises when these patients seek treatment for refractive errors. Although excimer laser surgery can be safely performed in patients with autoimmune and immune-mediated inflammatory disease, there are caveats. Aside from the routine laser-assisted in situ keratomileusis (LASIK) screening tests, in some instances, we recommend additional screening tests in patients with HS, such as dry eye tests, consultation with specialists regarding HS diagnosis and treatment, careful assessment of the eyelids and periorbital structures, and thorough history of past and current lesions and treatments. After these patients undergo LASIK, careful, frequent, and long-term follow-up is necessary. Any adverse event or complication should be managed immediately.
Funding
Research to Prevent Blindness funded the study. Hoopes Vision funded the Rapid Service Fees.
Similar content being viewed by others
Hidradenitis suppurativa (HS) is an inflammatory skin condition most often affecting the groin and underarms. It is relatively common, with a prevalence of 0.05–4.10% [1]. It is characterized by cystic lesions that develop in the deep dermis, which often rupture, producing suppurative material [2, 3]. While there are classic areas of distribution for HS, it can affect many parts of the body, including the eye [4]. Cases with ocular involvement are rare. In a study looking at inflammatory eye disease (IED) in patients with HS, only 1% of IED could be attributed to HS alone, while 4% had another comorbid autoimmune disorder that could have produced ocular findings [4]. This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors. The purpose of this article is to lay a foundation for understanding HS and to provide guidelines on the appropriateness of laser-assisted in situ keratomileusis (LASIK) in this patient population.
The histopathology of HS commonly includes follicular hyperkeratosis, interfollicular inflammation, and perifolliculitis with predominantly lymphocytic infiltrates [5] at sites that tend to have apocrine gland predominance [3]. Biopsy of lesions shows increased levels of CD3+, CD4+, and CD8+ T cells [6] along with increased levels of innate immune system cells such as neutrophils, dendritic cells, and histiocytes [7]. Chronic lesions also have increased levels of B cells and plasma cells [7]. In addition to apocrine gland dysfunction, there appears to be a component of immune dysregulation in HS [8]. It has been proposed that an initial anatomical obstruction of the glandular unit leads to bacterial colonization, which then produces an innate immune response [3, 9]. The innate immune response produces various interleukins and cytokines, including tumor necrosis factor-α, IL-1β, and IL-10 [10], which then stimulates a systemic immune response [3, 8]. Although complex and not completely understood, this is a cyclic process that can lead to dysregulation of the systemic immune response [8].
Most patients report multiple lesions per month, with the average lesion lasting about 1 week [2]. There may be a genetic component to the disease [11], and there is also a female predominance [2, 12]. HS most commonly presents in the third decade of life and is chronic in nature [2]. HS is also associated with various comorbidities [13]. There is a significant association with HS and inflammatory bowel disease (IBD), with one study reporting HS in 23% of patients with IBD [14]. There are similarities in skin lesions from Crohn’s disease and HS, and it is appropriate to establish a proper diagnosis in cases of atypical presentations that may have predominant skin findings [13, 15]. HS is also associated with arthropathies [16] and malignancy (skin and solid organ) [17].
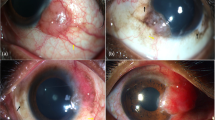
While the primary inciting events for HS occur in regions of high apocrine gland density, the subsequent systemic inflammation can have far-reaching effects, with multiple cases of HS associated with IED [4]. HS-associated IED includes bilateral interstitial keratitis [18], uveitis [4], Mooren-type ulcerations [19, 20], scleritis [4], glands of Moll involvement with mucopurulent discharge [21] (which are apocrine glands [22]), lacrimal sacs (including fistula formation) [23], and peripheral ulcerative keratitis (PUK) [4]. While there is no published information on patients with HS who have undergone LASIK, studies on LASIK in patients with well-controlled autoimmune or immune-mediated inflammatory diseases have shown that LASIK can be safely performed [24].
Although not characteristic, HS lesions can appear on the face and periorbital region [23, 25,26,27]. Because of this, a thorough exam should be done to look for any lesions that are on the eyelids, along the lid line [28], affecting the meibomian glands, or encroaching on the periorbital area. If any such lesions are noted, LASIK should be delayed. The patient should be screened for symptoms of dry eye secondary to glandular dysfunction. Obtaining a history regarding any past lesions involving the face or eyes is equally essential as lesions tend to be recurrent in nature [29]. If suspicious lesions are noted on exam, a referral to a dermatologist for appropriate diagnosis is recommended. In addition, consultation with a dermatologist to discuss the use of prophylactic doxycycline or anti-inflammatory therapy post-LASIK in patients with a history of facial manifestations of HS should be performed.
A thorough ophthalmic history should be taken. The presence or history of Mooren ulcers, interstitial keratitis, or PUK should raise serious concern when evaluating eligibility for LASIK. Interstitial keratitis is an absolute contraindication to LASIK [30]. While good outcomes have been reported from LASIK following the resolution of corneal ulceration [31], more attention should be given to patients with HS who have a history of corneal ulceration. There is an increased risk of keratitis and corneal ulceration following LASIK [32]. While it is not clear if this risk is compounded in patients who had keratitis or ulceration prior to LASIK, the risk of future disease warrants caution. Although LASIK is safe in patients with well-controlled autoimmune conditions [33, 34] and other immune-mediated inflammatory diseases, there have been reported cases of necrotizing keratitis post-LASIK in patients with well-controlled IBD [35].
A complete therapeutic history is critical. Even in cases where there are no visible ocular manifestations of HS that would preclude a patient from undergoing LASIK, it is essential to discuss any current medical treatments the patient may be undergoing. For example, isotretinoin (Accutane) therapy is a relatively common therapy for patients with HS [36]. The adverse ocular effects of isotretinoin are well categorized and include degenerative effects on epithelial cells as well as a negative influence on tear production and quality [37]. As such, isotretinoin use is a contraindication to undergoing LASIK [30, 38]. There is some evidence that healthy patients may return to pre-isotretinoin function as soon as 1 month after cessation of treatment [37, 39]. Despite this, patients with HS are at increased risk for ocular involvement due to the disease process and there is a lack of HS-specific data with regards return to baseline tear and epithelial cell function. As such, we advocate a more conservative approach in patients with HS and recommend that a patient have a 12-month period of isotretinoin cessation before being considered a candidate for LASIK. In addition, we recommend evaluation of tear production via the Schirmer tear test [40], assessing tear film breakup time, and a determination that tear osmolarity has returned to normal [41]. A survey of the meibomian glands to assess for adequate function can also be done. If meibomian gland dysfunction is found, various treatments are effective in alleviating symptoms [42, 43], although outcomes in patients with HS have not expressly been studied. Low-dose systemic anti-androgen therapy (spironolactone) may also be used for HS treatment [44]. Androgen deficiency may be associated with meibomian gland dysfunction and dry eye [45]. However, it is unclear how significant this effect is with low-dose systemic spironolactone. If a patient is taking spironolactone, we recommend screening for dry eye symptoms and proceeding with caution, but anti-androgen therapy is not an absolute contraindication to LASIK.
There is an increasing trend of using biologic agents to treat HS [46, 47]. Adalimumab, in particular, is effective in a significant proportion of patients with HS [1]. There is no published data on the direct effects of biologic drugs on outcomes in LASIK. However, there is an increased risk of infection when taking certain biologic drugs, including adalimumab [48]. This includes an increased risk for herpes simplex keratitis [49]. While prophylactic acyclovir could be considered in some instances, the duration of prophylactic treatment should be closely monitored, as prolonged prophylactic use can lead to resistant viral strains [50]. Patients taking biologics are also at increased risk of herpes zoster flares [51]. Mycobacterial infection is another concern in patients taking biologic agents [52], since keratitis post-LASIK is associated with this infection [53]. If a patient is undergoing treatment with a biologic agent, close follow-up is recommended.
After a careful screening process, if the patient is deemed a candidate for LASIK surgery, it is essential to pay particular attention to epithelial trauma during the procedure. If there is any flap trauma, a bandage contact lens with close follow-up is recommended. Close monitoring should be done for abrasions, ulcerations, or epitheliopathy as well. Punctal plugs should be placed if there is any concern that the patient is at high risk for inadequate tear production or glandular dysfunction. The continuing risk of developing future eye manifestations in patients with HS requires frequent and careful follow-up with immediate management of any adverse event.
In summary, HS is a complex inflammatory disease process with immune dysregulation. The decision to perform LASIK in a patient with HS should involve a multidisciplinary approach with guidance from the patient’s dermatologist and/or rheumatologist to assess the course and severity of their disease. The continuing risk of developing future eye manifestations in patients with HS, whether they undergo LASIK or not, should be made clear to the patient. Patients should be warned that LASIK may limit their future treatment options for controlling skin manifestations of their HS (such as isotretinoin). Prophylactic antibiotics or antivirals should be considered in high-risk cases (such as patients on immunomodulating therapy that have a history of infectious keratitis). If the disease is well controlled, there are no current precluding ocular findings, there is a unanimous agreement with other specialists, and the patient understands the nature of their systemic disease, it is reasonable to perform LASIK in patients with HS. Table 1 summarizes pre- and postoperative considerations for patients undergoing LASIK. These patients require clinical vigilance and there should be a low threshold to treat if there are signs of ocular complications. These same principles of careful screening, long-term follow-up, and immediate management of complications will apply to patients with HS who are being considered for alternative cornea refractive procedures such as small incision lenticule extraction (SMILE) and photorefractive keratotomy (PRK).
References
Saunte DML, Jemec GBE. Hidradenitis suppurativa: advances in diagnosis and treatment. JAMA. 2017;318(20):2019–32. https://doi.org/10.1001/jama.2017.16691.
von der Werth J, Williams H. The natural history of hidradenitis suppurativa. J Eur Acad Dermatol Venereol. 2000;14(5):389–92. https://doi.org/10.1046/j.1468-3083.2000.00087.x.
Hoffman L, Ghias M, Lowes M. Pathophysiology of hidradenitis suppurativa. Semin Cutan Med Surg. 2017;36(2):47–54. https://doi.org/10.12788/j.sder.2017.017.
Saygın D, Syed AU, Lowder CY, Srivastava S, Maya JJ, Hajj-Ali RA. Characteristics of inflammatory eye disease associated with hidradenitis suppurativa. Eur J Rheumatol. 2018;5(3):165–8. https://doi.org/10.5152/eurjrheum.2018.17163.
von Laffert M, Helmbold P, Wohlrab J, Fiedler E, Stadie V, Marsch WC. Hidradenitis suppurativa (acne inversa): early inflammatory events at terminal follicles and at interfollicular epidermis. Exp Dermatol. 2009;19(6):533–7. https://doi.org/10.1111/j.1600-0625.2009.00915.x.
van der Zee HH, Laman JD, de Ruiter L, Dik WA, Prens EP. Adalimumab (antitumour necrosis factor-α) treatment of hidradenitis suppurativa ameliorates skin inflammation: an in situ and ex vivo study. Br J Dermatol. 2012;166(2):298–305. https://doi.org/10.1111/j.1365-2133.2011.10698.x.
van der Zee HH, de Ruiter L, Boer J, et al. Alterations in leucocyte subsets and histomorphology in normal-appearing perilesional skin and early and chronic hidradenitis suppurativa lesions. Br J Dermatol. 2012;166(1):98–106. https://doi.org/10.1111/j.1365-2133.2011.10643.x.
Kelly G, Sweeney CM, Tobin A-M, Kirby B. Hidradenitis suppurativa: the role of immune dysregulation. Int J Dermatol. 2014;53(10):1186–96. https://doi.org/10.1111/ijd.12550.
van der Zee HH, Laman JD, Boer J, Prens EP. Hidradenitis suppurativa: viewpoint on clinical phenotyping, pathogenesis and novel treatments. Exp Dermatol. 2012;21(10):735–9. https://doi.org/10.1111/j.1600-0625.2012.01552.x.
van der Zee HH, de Ruiter L, van den Broecke DG, Dik WA, Laman JD, Prens EP. Elevated levels of tumour necrosis factor (TNF)-α, interleukin (IL)-1β and IL-10 in hidradenitis suppurativa skin: a rationale for targeting TNF-α and IL-1β. Br J Dermatol. 2011;164(6):1292–8. https://doi.org/10.1111/j.1365-2133.2011.10254.x.
Fitzsimmons JS, Guilbert PR, Fitzsimmons EM. Evidence of genetic factors in hidradenitis suppurativa. Br J Dermatol. 1985;113(1):1–8. http://www.ncbi.nlm.nih.gov/pubmed/4015966. Accessed 15 May 2019.
Giamarellos-Bourboulis EJ, Platzer M, Karagiannidis I, et al. High copy numbers of β-defensin cluster on 8p23.1, confer genetic susceptibility, and modulate the physical course of hidradenitis suppurativa/acne inversa. J Invest Dermatol. 2016;136(8):1592–8. https://doi.org/10.1016/j.jid.2016.04.021.
Miller IM, McAndrew RJ, Hamzavi I. Prevalence, risk factors, and comorbidities of hidradenitis suppurativa. Dermatol Clin. 2016;34(1):7–16. https://doi.org/10.1016/j.det.2015.08.002.
van der Zee HH, de Winter K, van der Woude CJ, Prens EP. The prevalence of hidradenitis suppurativa in 1093 patients with inflammatory bowel disease. Br J Dermatol. 2014;171(3):673–5. https://doi.org/10.1111/bjd.13002.
Church JM, Fazio VW, Lavery IC, Oakley JR, Milsom JW. The differential diagnosis and comorbidity of hidradenitis suppurativa and perianal Crohn’s disease. Int J Colorectal Dis. 1993;8(3):117–119. http://www.ncbi.nlm.nih.gov/pubmed/8245664. Accessed 15 May 2019.
Bruzzese V. Pyoderma gangrenosum, acne conglobata, suppurative hidradenitis, and axial spondyloarthritis. J Clin Rheumatol. 2012;18(8):413–5. https://doi.org/10.1097/RHU.0b013e318278b84c.
Lapins J, Ye W, Nyrén O, Emtestam L. Incidence of cancer among patients with hidradenitis suppurativa. Arch Dermatol. 2001;137(6):730–734. http://www.ncbi.nlm.nih.gov/pubmed/11405761. Accessed 15 May 2019.
Alzaga Fernandez AG, Demirci H, Darnley-Fisch DA, Steen DW. Interstitial keratitis secondary to severe hidradenitis suppurativa: a case report and literature review. Cornea. 2010;29(10):1189–91. https://doi.org/10.1097/ICO.0b013e3181d4fd5c.
Meskin SW, Carlson EM. Mooren’s-type ulceration associated with severe hidradenitis suppurativa: a case report and literature review. Ocul Immunol Inflamm. 2011;19(5):340–2. https://doi.org/10.3109/09273948.2011.584653.
Wilson SE, Lee WM, Murakami C, Weng J, Moninger GA. Mooren-type hepatitis C virus-associated corneal ulceration. Ophthalmology. 1994;101(4):736–45. https://doi.org/10.1016/S0161-6420(94)31291-7.
Sachs DD, Gordon AT. Hidradenitis suppurativa of glands of Moll. Arch Ophthalmol. 1967;77(5):635–6. https://doi.org/10.1001/archopht.1967.00980020637012.
Stoeckelhuber BM, Welsch U, Stoeckelhuber M. Human glands of Moll: histochemical and ultrastructural characterization of the glands of Moll in the human eyelid. J Invest Dermatol. 2003;121(1):28–36. https://doi.org/10.1046/J.1523-1747.2003.12328.X.
Hassan AS, Saldana M, Wearne M. Hidradenitis suppurativa of the periorbital skin with lacrimal sac and ethmoidal involvement. Orbit. 2014;33(5):382–4. https://doi.org/10.3109/01676830.2014.894542.
Schallhorn JM, Schallhorn SC, Hettinger KA, et al. Outcomes and complications of excimer laser surgery in patients with collagen vascular and other immune-mediated inflammatory diseases. J Cataract Refract Surg. 2016;42(12):1742–52. https://doi.org/10.1016/j.jcrs.2016.09.018.
Greer KE. Facial involvement with hidradenitis suppurativa. Arch Dermatol. 1974;109(3):408. https://doi.org/10.1001/archderm.1974.01630030062019.
Poli F, Wolkenstein P, Revuz J. Back and face involvement in hidradenitis suppurativa. Dermatology. 2010;221(2):137–41. https://doi.org/10.1159/000315508.
Bardenstein DS, Haluschak J, Gerson S, Zaim MT. Neutrophilic eccrine hidradenitis simulating orbital cellulitis. Arch Ophthalmol. 1994;112(11):1460. https://doi.org/10.1001/archopht.1994.01090230074023.
Mastrota KM. Hidradenitis suppurativa masquerades as blepharitis. 2018. https://www.optometrytimes.com/blepharitis/hidradenitis-suppurativa-masquerades-blepharitis. Accessed 16 May 2019.
Jemec GBE. Hidradenitis suppurativa. N Engl J Med. 2012;366(2):158–64. https://doi.org/10.1056/NEJMcp1014163.
Bower KS, Woreta F. Update on contraindications for laser-assisted in situ keratomileusis and photorefractive keratectomy. Curr Opin Ophthalmol. 2014;25(4):251–7. https://doi.org/10.1097/ICU.0000000000000055.
Procházková S, Netuková M, Klecka D, Novák P. Lasik after corneal ulcer. Cesk Slov Oftalmol. 2011;67(3):86–89. http://www.ncbi.nlm.nih.gov/pubmed/22132646. Accessed 14 May 2019.
Randleman JB, Shah RD. LASIK interface complications: etiology, management, and outcomes. J Refract Surg. 2012;28(8):575–86. https://doi.org/10.3928/1081597X-20120722-01.
Smith RJ, Maloney RK. Laser in situ keratomileusis in patients with autoimmune diseases. J Cataract Refract Surg. 2006;32(8):1292–5. https://doi.org/10.1016/J.JCRS.2006.02.059.
AlKharashi M, Bower KS, Stark WJ, Daoud YJ. Refractive surgery in systemic and autoimmune disease. Middle East Afr J Ophthalmol. 2014;21(1):18–24. https://doi.org/10.4103/0974-9233.124082.
Aman-Ullah M, Gimbel HV, Purba MK, van Westenbrugge JA. Necrotizing keratitis after laser refractive surgery in patients with inactive inflammatory bowel disease. Case Rep Ophthalmol. 2012;3(1):54–60. https://doi.org/10.1159/000336567.
Huang CM, Kirchhof MG. A new perspective on isotretinoin treatment of hidradenitis suppurativa: a retrospective chart review of patient outcomes. Dermatology. 2017;233(2–3):120–5. https://doi.org/10.1159/000477207.
Karalezli A, Borazan M, Altinors DD, Dursun R, Kiyici H, Akova YA. Conjunctival impression cytology, ocular surface, and tear-film changes in patients treated with systemic isotretinoin. Cornea. 2009;28(1):46–50. https://doi.org/10.1097/ICO.0b013e318183a396.
Malik M, Simpson RC, Varma S. Isotretinoin as contraindication. BMJ. 2011;342:d3353. https://doi.org/10.1136/bmj.d3353.
Bozkurt B, Irkeç MT, Atakan N, Orhan M, Geyik PO. Lacrimal function and ocular complications in patients treated with systemic isotretinoin. Eur J Ophthalmol. 12(3):173–176. http://www.ncbi.nlm.nih.gov/pubmed/12113560. Accessed 05 July 2019.
Li S, Kim YH, Li W, Lin MC, Radke CJ. Human lacrimal production rates from modified Schirmer-tear test. Optom Vis Sci. 2018;95(4):343–8. https://doi.org/10.1097/OPX.0000000000001196.
Mathers WD, Shields WJ, Sachdev MS, Petroll WM, Jester JV. Meibomian gland morphology and tear osmolarity: changes with accutane therapy. Cornea. 1991;10(4):286–290. http://www.ncbi.nlm.nih.gov/pubmed/1832371. Accessed 16 May 2019.
Maskin SL, Testa WR. Growth of meibomian gland tissue after intraductal meibomian gland probing in patients with obstructive meibomian gland dysfunction. Br J Ophthalmol. 2018;102(1):59–68. https://doi.org/10.1136/bjophthalmol-2016-310097.
Finis D, König C, Hayajneh J, Borrelli M, Schrader S, Geerling G. Six-month effects of a thermodynamic treatment for MGD and implications of meibomian gland atrophy. Cornea. 2014;33(12):1265–70. https://doi.org/10.1097/ICO.0000000000000273.
Golbari NM, Porter ML, Kimball AB. Antiandrogen therapy with spironolactone for the treatment of hidradenitis suppurativa. J Am Acad Dermatol. 2019;80(1):114–9. https://doi.org/10.1016/j.jaad.2018.06.063.
Sullivan DA, Sullivan BD, Evans JE, et al. Androgen deficiency, meibomian gland dysfunction, and evaporative dry eye. Ann N Y Acad Sci. 2002;966:211–222. http://www.ncbi.nlm.nih.gov/pubmed/12114274. Accessed 21 May 2019.
Blok JL, Li K, Brodmerkel C, Horvátovich P, Jonkman MF, Horváth B. Ustekinumab in hidradenitis suppurativa: clinical results and a search for potential biomarkers in serum. Br J Dermatol. 2016;174(4):839–46. https://doi.org/10.1111/bjd.14338.
Kimball AB, Okun MM, Williams DA, et al. Two phase 3 trials of adalimumab for hidradenitis suppurativa. N Engl J Med. 2016;375(5):422–34. https://doi.org/10.1056/NEJMoa1504370.
Safety Information for HUMIRA (adalimumab) | rheumatology. https://www.humirapro.com/rheumatology/safety-data. Accessed 21 May 2019.
Bernauer W, Schuler S, Borradori L. Rituximab and bilateral HSV epithelial keratitis in a patient with mucous membrane pemphigoid. J Ophthalmic Inflamm Infect. 2018;8(1):12. https://doi.org/10.1186/s12348-018-0153-8.
van Velzen M, van de Vijver DAMC, van Loenen FB, Osterhaus ADME, Remeijer L, Verjans GMGM. Acyclovir prophylaxis predisposes to antiviral-resistant recurrent herpetic keratitis. J Infect Dis. 2013;208(9):1359–65. https://doi.org/10.1093/infdis/jit350.
Marra F, Lo E, Kalashnikov V, Richardson K. Risk of herpes zoster in individuals on biologics, disease-modifying antirheumatic drugs, and/or corticosteroids for autoimmune diseases: a systematic review and meta-analysis. Open forum Infect Dis. 2016;3(4):205. https://doi.org/10.1093/ofid/ofw205.
Tsuyuguchi K, Matsumoto T. [Biologics and mycobacterial diseases]. Kekkaku. 2013;88(3):337–353. http://www.ncbi.nlm.nih.gov/pubmed/23672175. Accessed 17 May 2019.
Ko J, Kim SK, Yong DE, Kim T, Kim EK. Delayed onset Mycobacterium intracellulare keratitis after laser in situ keratomileusis. Medicine (Baltimore). 2017;96(51):e9356. https://doi.org/10.1097/MD.0000000000009356.
Acknowledgements
Funding
Research to Prevent Blindness provided funding for the study, and Hoopes Vision provided funding for the Rapid Service Fees. All authors had full access to the articles reviewed in this manuscript and take complete responsibility for the integrity and accuracy of this manuscript.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
David B. Rosen, Majid Moshirfar, Madeline B. Heiland, Yasmyne C. Ronquillo, and Phillip C. Hoopes have nothing to disclose.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced digital features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.8832542.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License ( http://creativecommons.org/licenses/by-nc/4.0/ ), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Rosen, D.B., Moshirfar, M., Heiland, M.B. et al. Should Patients with Hidradenitis Suppurativa Undergo LASIK?. Ophthalmol Ther 8, 353–359 (2019). https://doi.org/10.1007/s40123-019-0201-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-019-0201-y