Abstract
Introduction
Few studies have investigated the effect of increased creatinine clearance (CrCl) on linezolid (LZD) concentration. Herein, we report the pharmacokinetic/pharmacodynamic (PK/PD) profile of LZD used in the management of methicillin-resistant Staphylococcus aureus (MRSA) pneumonia with concomitant bacteremia in a patient with high CrCl caused by diabetes insipidus (DI).
Case Report
A 19-year-old man was admitted to the intensive care unit following a traumatic brain injury. After admission, he underwent a craniotomy for the severe brain injury. However, he developed DI after the operation. Despite treatment with vasopressin, his urine output reached 5–6 L/day as a result of the DI, and his CrCl increased to 180–278 mL/min. We were required to administer 6–7 L of fluid a day to compensate for the high urinary fluid output. On day 55, MRSA pneumonia with sepsis was suspected and, consequently, LZD was administrated intravenously (600 mg every 12 h). He was treated with LZD for 14 days. The patient has since successfully recovered from MRSA pneumonia with concomitant bacteremia, and was transferred to the general ward on day 82. Blood LZD levels from days 60–68, which were measured after the patient’s transfer to the general ward, showed that the trough levels were lower than the threshold level of detection. The blood 24-h area under the plasma LZD concentration–time curve (AUC)24/minimum inhibitory concentration (MIC) was 69.3.
Conclusion
In spite of the low level of LZD AUC24/MIC caused by the high CrCl with DI, MRSA pneumonia with concomitant bacteremia was successfully treated with LZD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Linezolid (LZD) is an oxazolidinone antibiotic characterized by a wide spectrum of activity against Gram-positive pathogens resistant to β-lactams and glycopeptides, and its use has progressively increased in recent years [1, 2]. LZD clearance is mainly non-renal (approximately 65%) through the formation of two major inactive metabolites, the hydroxyethyl glycine metabolite (PNU-142586) and the aminoethoxyacetic acid metabolite (PNU-142300), which account for 40–50% and 9–10% of the total dose, respectively. Renal clearance of the unchanged parent drug accounts for the remaining 30–40% [3]. More recent reports have suggested that the influence of renal dysfunction on high LZD blood concentration may lead to hematological side effects such as thrombocytopenia [8, 9].
However, the influence of low LZD blood concentration in conjunction with high creatinine clearance (CrCl) still remains unknown. Additionally, the pharmacokinetic/pharmacodynamic (PK/PD) index for the efficacy of LZD was previously shown to be a 24-h area under the plasma LZD concentration–time curve/minimum inhibitory concentration (AUC24/MIC) ratio of ≥100 [4–6]. Herein, we report the PK/PD profile of a patient with methicillin-resistant Staphylococcus aureus (MRSA) pneumonia and bacteremia who developed diabetes insipidus (DI) with a high level of CrCl. Despite the low AUC24/MIC of LZD in comparison with the efficacy level of AUC24/MIC (≥100) [4–6], the patient was successfully treated for the MRSA infection.
Case Report
Sampling and Drug Administration
Blood samples for the quantification of LZD in plasma were collected through an indwelling arterial catheter both before and after the morning dosing, which was administered through an intermittent intravenous infusion of 600 mg over the course of 1 h. LZD was administrated twice a day (morning and night). Blood samples were taken in the morning before dosing (trough) and after the morning’s 1-h-long LZD administration. After centrifugation, plasma samples were separated and stored at −80 °C until assayed. Blood LZD concentration was measured after the patient’s transfer to the general ward.
Creatinine Clearance
To assess renal function, creatinine concentrations in both the serum and 24-h urine samples were determined. CrCl (mL/min) was calculated using the formula:
where C urine (mg/dL) is the creatinine concentration in urine, V urine (mL/min) is the urine volume, C serum (mg/dL) is the serum creatinine concentration, and BSA (m2) is the body surface area.
LZD Assay
LZD blood concentration was measured through high-performance liquid chromatography [7]. The lower limit of the quantification was 0.5 mg/L.
Pharmacokinetic Assessment
A PK analysis of LZD was performed using the nonlinear least squares program MULTI [8]. The drug concentration data were fit to a standard one-compartment model with zero-order input (1-h-long drug infusion) and first-order elimination. The PK parameters used were total clearance (L/h) and volume of distribution (L). The LZD AUC24 was estimated using PK parameters for daily dose/total clearance.
Case
A 19-year-old male was admitted to Fukuoka University Hospital after being involved in a traffic accident. A neurological assessment revealed a Glasgow Coma Scale (GCS) score of 3/15. Computed tomography (CT) of the head showed a subcutaneous and extradural hematoma. A craniotomy was immediately performed to remove the hematoma and to attain cerebral decompression and, as a result, the GCS score recovered to 10/15. On day 13, he developed polyuria. His 24-h urine volume reached 5–6 L/day with a urine osmolality of 159 mOsm/L and a plasma osmolality of 340 mOsm/L. Thus, he was diagnosed with cerebral DI. As a basal skull fracture was present, an intravenous vasopressin infusion was administered to treat the DI. However, it showed a poor therapeutic effect, polyuria continued, and CrCl was revealed to be 180–278 mL/min as a result of the DI. We were required to administer approximately 6–7 L/day of fluid to compensate for the high urinary fluid output. On day 50, MRSA was detected in surveillance cultures of sputum and urine samples (MIC for LZD was 1 mg/L).
On day 55, he developed systemic inflammatory response syndrome (SIRS) [9], and pneumonia and/or a urinary tract infection was suspected based upon the results of preceding surveillance cultures. Consequently, LZD was administrated intravenously (600 mg every 12 h) for 14 days. On day 57, a chest X-ray and CT scan showed a consolidation in the right lung (Fig. 1a, b). It was found that blood cultures that had been drawn before the administration of LZD developed MRSA (MIC for LZD was 1 mg/L) while the cerebrospinal fluid culture was negative. In transthoracic echocardiography, there was no evidence of infectious endocarditis at day 56. Based upon these findings, we diagnosed MRSA pneumonia with secondary bacteremia due to pneumonia or a urinary tract infection. Blood, urine, and sputum cultures were negative on days 61, 64, and 68, respectively. A chest X-ray on day 68 and CT scan on day 70 showed improvement in the consolidation (Fig. 1c, d). The patient was successfully transferred to the general ward on day 82. Concomitant antibiotics were not administered because the results of the cultures showed the development of MRSA only (Fig. 2).
Chest imaging before and after treatment with LZD. a (Chest X-ray) and b (chest CT scan; day 57) show consolidation in right lower lung before treatment (b, arrow). c The chest X-ray (day 68) and d shows the chest CT scan (day 70) images after treatment, and show the improvement in the consolidation
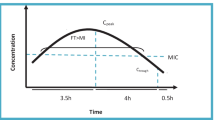
Clinical course and LZD blood concentration. Asterisk A ‘+’ indicates at least two SIRS criteria [9]. Plus A ‘+’ indicates that MRSA developed in the culture; a ‘−’ shows that nothing grew in the culture. LZD (600 mg) was administrated twice a day for 1 h. The concentration of LZD was shown before the day’s first administration (trough) and after the first 1-h LZD administration for the day. CrCL (mL/min) was calculated using the formula: CrCl = (C urine × V urine)/(C serum) × (1.73/BSA); where C urine (mg/dL) is the creatinine concentration in urine, V urine (mL/min) is the urine volume, C serum (mg/dL) is the serum creatinine concentration, and BSA (m2) is the body surface area. AUC 24 /MIC 24-h area under the plasma linezolid concentration–time curve/minimum inhibitory concentration, CrCl creatinine clearance, CRP C-reactive protein, LZD linezolid, MRSA methicillin-resistant Staphylococcus aureus, ND not detected, NE not examined, SIRS systemic inflammatory syndrome
Blood concentrations of LZD from days 60–68 were measured after the patient’s transfer to the general ward. The AUC24/MIC values over the observation period were found to be 69.3 2 days after LZD administration, and the trough levels were too low to be detected (Fig. 2).
Informed consent was obtained from the patient’s family in relation to his being included in the study.
Discussion
To the best of our knowledge, this is the first case to report a PK profile of LZD in a patient with DI with high CrCl. In this case, CrCl was 180–278 mL/min as a result of DI. In regard to patients with a high level of CrCl in the intensive care unit, it was reported that blood LZD concentrations were variable, showing trough concentrations from 0.13 to 14.49 mg/L (median 2.06 mg/L) [10]. In the current case, blood LZD trough levels were lower than the detection limit (<0.5 mg/L) and the AUC24/MIC (69.3) was also remarkably low compared with those provided in previous reports concerning 20 critically ill patients (median 248 mg/L, interquartile range 144–347 mg/L) [11]. Since the LZD trough levels were lower than the detection limit (0.5 mg/L), the actual AUC24/MIC may have been lower than that in our calculated AUC24/MIC levels. The precise mechanism of the decreased LZD AUC24/MIC and blood trough levels in this case is unknown; however, LZD PK might be altered by high CrCl and a large volume of fluid administration.
In the current case, we diagnosed MRSA pneumonia for the following reasons. First, the precedent surveillance culture of sputum only developed MRSA and no other significant microorganisms; second, the chest CT scan showed a consolidation in the right lower lung, which suggested a transbronchial route of infection; and third, the pneumonia was successfully treated with LZD only, not with any other antimicrobials. An American consensus review [12] recommended vancomycin for the treatment of MRSA infections; however, in a randomized-controlled study for MRSA nosocomial pneumonia, LZD showed better clinical efficacy and microbiological responses than vancomycin [13]. Rayner et al. [5] reported that higher success rates for LZD may occur at AUC24/MIC values of 80–120 for bacteremia, skin and skin structure infections, and lower respiratory tract infections. In this case, on day 50, the urine culture developed MRSA ≥106/colony-forming units/mL. It is unclear whether the patient had a urinary tract infection or if the observed MRSA in the urine had simply passed into the urine from the blood. Additionally, on day 64, MRSA was not detected in the urine culture. To the best of our knowledge, little investigation has been conducted into the usefulness of LZD for the treatment of urinary tract infections [14]. Approximately 35% of LZD is excreted in urine [14]. In this case, a high level of urine output was observed because of DI and, consequently, the high doses of LZD may be passed though the urinary tract. Therefore, despite low plasma LZD AUC, the urine culture may become negative. Interestingly, in spite of the remarkably low level of the AUC24/MIC in this case, MRSA pneumonia bacteremia was treated successfully after LZD administration. In LZD, the level of plasma protein binding is 31% and the volume of distribution approximates the total water content of the body (40–50 L) [15, 16]. In lung tissues, it was reported that LZD concentrations in the epithelial lining fluid (64.3 ± 33.1 µg/mL) were much higher than those in the blood (7.3 ± 4.9 µg/mL) and alveolar cells (2.2 ± 0.6 µg/mL) [17]. These findings suggest that LZD is excluded or rapidly removed from the blood to the lung compartment. As this was a retrospective study, we could not examine the concentration of LZD in the epithelial lining fluid. For this reason we could not take cultures and blood samples every day.
To our knowledge, this is the first report showing the successful treatment of MRSA pneumonia with bacteremia despite very low LZD AUC24/MIC. Localized higher concentrations of LZD in the lung might have been sufficiently effective in treating the pneumonia and the secondary bacteremia as a result of the sites of these infections; however, the precise mechanism of low LZD AUC24/MIC and successful treatment of MRSA infection in these cases remains generally unknown.
Conclusions
In conclusion, sub-therapeutic levels of LZD blood concentrations may be caused by uncontrolled DI with high CrCl and a high level of fluid administration. In spite of the low level of AUC24/MIC, MRSA pneumonia and bacteremia were successfully treated with LZD. As this was a retrospective study, we were unable to evaluate the concentration of LZD on days 60–68 after the 1-h LZD administration for the PK assessment. We must further study the actual PK assessment of LZD in patients with high CrCl caused by DI. Further investigation is required into the mechanisms of low LZD AUC24/MIC and the successful treatment of these MRSA infections.
References
Cox H, Ford N. Linezolid for the treatment of complicated drug-resistant tuberculosis: a systematic review and meta-analysis. Int J Tuberc Lung Dis. 2012;16(4):447–54.
Ager S, Gould K. Clinical update on linezolid in the treatment of gram-positive bacterial infections. Infect Drug Resist. 2012;5:87–102.
Stalker DJ, Jungbluth GL. Clinical pharmacokinetics of linezolid, a novel oxazolidinone antibacterial. Clin Pharmacokinet. 2003;42(13):1129–40.
Andes D, van Ogtrop ML, Peng J, Craig WA. In vivo pharmacodynamics of a new oxazolidinone (linezolid). Antimicrob Agents Chemother. 2002;46(11):3484–9.
Rayner CR, Forrest A, Meagher AK, Birmingham MC, Schentag JJ. Clinical pharmacodynamics of linezolid in seriously ill patients treated in a compassionate use programme. Clin Pharmacokinet. 2003;42(15):1411–23.
MacGowan AP. Pharmacokinetic and pharmacodynamic profile of linezolid in healthy volunteers and patients with gram-positive infections. J Antimicrob Chemother. 2003;51(Suppl 2):17ii–25.
Hara S, Uchiyama M, Yoshinari M, et al. A simple high-performance liquid chromatography for the determination of linezolid in human plasma and saliva. Biomed Chromatogr. 2015;29(9):1428–31. doi:10.1002/bmc.3441.
Yamaoka K, Tanigawara Y, Nakagawa T, Uno T. A pharmacokinetic analysis program (multi) for microcomputer. J Pharmacobiodyn. 1981;4(11):879–85.
Bone RC, Balk RA, Cerra FB, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The accp/sccm consensus conference committee. American college of chest physicians/society of critical care medicine. Chest. 1992;101(6):1644–55.
Zoller M, Maier B, Hornuss C, et al. Variability of linezolid concentrations after standard dosing in critically ill patients: a prospective observational study. Crit Care. 2014;18(4):R148.
Yagi T, Naito T, Doi M, et al. Plasma exposure of free linezolid and its ratio to minimum inhibitory concentration varies in critically ill patients. Int J Antimicrob Agents. 2013;42(4):329–34.
Rybak M, Lomaestro B, Rotschafer JC, et al. Therapeutic monitoring of vancomycin in adult patients: a consensus review of the American society of health-system pharmacists, the infectious diseases society of America, and the society of infectious diseases pharmacists. Am J Health Syst Pharm. 2009;66(1):82–98.
Wunderink RG, Niederman MS, Kollef MH, et al. Linezolid in methicillin-resistant Staphylococcus aureus nosocomial pneumonia: a randomized, controlled study. Clin Infect Dis. 2012;54(5):621–9.
Onda H, Wagenlehner FM, Lehn N, Naber KG. In vitro activity of linezolid against gram-positive uropathogens of hospitalized patients with complicated urinary tract infections. Int J Antimicrob Agents. 2001;18(3):263–6.
Slatter JG, Stalker DJ, Feenstra KL, et al. Pharmacokinetics, metabolism, and excretion of linezolid following an oral dose of [(14)c]linezolid to healthy human subjects. Drug Metab Dispos. 2001;29(8):1136–45.
Sisson TL, Jungbluth GL, Hopkins NK. Age and sex effects on the pharmacokinetics of linezolid. Eur J Clin Pharmacol. 2002;57(11):793–7.
Conte JE Jr, Golden JA, Kipps J, Zurlinden E. Intrapulmonary pharmacokinetics of linezolid. Antimicrob Agents Chemother. 2002;46(5):1475–80.
Acknowledgments
No funding or sponsorship was received for this study or publication of this article. The article processing charges for this publication were funded by the authors. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for this version to be published.
Disclosures
Yoshihiko Nakamura, Masanobu Uchiyama, Shuuji Hara, Mariko Mizunuma, Takafumi Nakano, Hiroyasu Ishikura, Kota Hoshino, Yasumasa Kawano, and Tohru Takata have nothing to disclose.
Compliance with ethics guidelines
Informed consent was obtained from the patient’s family in relation to his being included in the study.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Nakamura, Y., Uchiyama, M., Hara, S. et al. Therapeutic Dose Monitoring for Linezolid in a Patient with MRSA Pneumonia with Bacteremia in Diabetes Insipidus. Infect Dis Ther 5, 81–87 (2016). https://doi.org/10.1007/s40121-015-0100-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-015-0100-z