Abstract
Purpose of Review
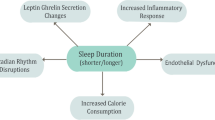
Poor sleep is a risk factor for cardiometabolic morbidity. The relationship of sleep and cardiometabolic health could be confounded, mediated, or modified by diet, yet the incorporation of diet in sleep-cardiometabolic health studies is inconsistent. This rapid systematic literature review evaluates the conceptualization of diet as a confounder, mediator, or effect modifier within sleep-cardiometabolic health investigations, and the statistical approaches utilized.
Recent Findings
Of 4692 studies identified, 60 were retained (28 adult, 32 pediatric). Most studies included diet patterns, quality, or energy intake as confounders, while a few examined these dietary variables as mediators or effect modifiers. There was some evidence, mostly in pediatric studies, that inclusion of diet altered sleep-cardiometabolic health associations.
Summary
Diet plays a diverse role within sleep-cardiometabolic health associations. Investigators should carefully consider the conceptualization of diet variables in these relationships and utilize contemporary statistical approaches when applicable.


Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major Importance
Huang PL. A comprehensive definition for metabolic syndrome. Dis Model Mech. 2009;2:231–7. https://doi.org/10.1242/dmm.001180.
Mccullough AJ. Epidemiology of the metabolic syndrome in the USA. J Dig Dis. 12:333–340.
Ranasinghe P, Mathangasinghe Y, Jayawardena R, Hills AP, Misra A. Prevalence and trends of metabolic syndrome among adults in the Asia-Pacific region: a systematic review. BMC Public Health. 2017;17:101. https://doi.org/10.1186/s12889-017-4041-1.
Shin D, Kongpakpaisarn K, Bohra C. Trends in the prevalence of metabolic syndrome and its components in the United States 2007–2014. Int J Cardiol. 2018;259:216–9. https://doi.org/10.1016/j.ijcard.2018.01.139.
Rimm EB, Appel LJ, Chiuve SE, et al. Seafood long-chain n-3 polyunsaturated fatty acids and cardiovascular disease: a science advisory from the American Heart Association. Circulation. 2018; https://doi.org/10.1161/CIR.0000000000000574.
Shen J, Wilmot KA, Ghasemzadeh N, et al. Mediterranean dietary patterns and cardiovascular health. Annu Rev Nutr. 35:425–449.
World Health Organization (WHO) & Food and Agriculture Organization of the United nations (FAO). Diet, nutrition and the prevention of chronic diseases.
Shukla C, Basheer R. Metabolic signals in sleep regulation: recent insights. Nat Sci Sleep. 8:9–20.
Xi B, He D, Zhang M, Xue J, Zhou D. Short sleep duration predicts risk of metabolic syndrome: a systematic review and meta-analysis. Sleep Med Rev. 2014;18:293–7. https://doi.org/10.1016/j.smrv.2013.06.001.
Knutson KL, Spiegel K, Penev P, Van Cauter E. The metabolic consequences of sleep deprivation. Sleep Med Rev. 11:163–178.
Hart CN, Carskadon MA, Considine RV, Fava JL, Lawton J, Raynor HA, et al. Changes in children’s sleep duration on food intake, weight, and leptin. Pediatrics. 2013;132:e1473–80. https://doi.org/10.1542/peds.2013-1274.
Mullins EN, Miller AL, Cherian SS, Lumeng JC, Wright KP Jr, Kurth S, et al. Acute sleep restriction increases dietary intake in preschool-age children. J Sleep Res. 2017;26:48–54. https://doi.org/10.1111/jsr.12450.
Howatson G, Bell PG, Tallent J, Middleton B, McHugh MP, Ellis J. Effect of tart cherry juice (Prunus cerasus) on melatonin levels and enhanced sleep quality. Eur J Nutr. 2012;51:909–16. https://doi.org/10.1007/s00394-011-0263-7.
Peuhkuri K, Sihvola N, Korpela R. Dietary factors and fluctuating levels of melatonin. Food Nutr Res. 2012;56:1–9. https://doi.org/10.3402/fnr.v56i0.17252.
Spiegel K, Tasali E, Penev P, Van Cauter E. Brief communication: sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med. 2004;141:846–50. https://doi.org/10.7326/0003-4819-141-11-200412070-00008.
Afaghi A, O’Connor H, Chow CM. High-glycemic-index carbohydrate meals shorten sleep onset. Am J Clin Nutr. 2007;85:426–30. https://doi.org/10.1093/ajcn/85.2.426.
• Cespedes EM, Hu FB, Redline S, et al. Chronic insufficient sleep and diet quality: contributors to childhood obesity. Obesity (Silver Spring). 2016;24:184–90. https://doi.org/10.1002/oby.21196. This was a longitudinal study of US children with parent-reported sleep measures from age 6 months through 7 years. Investigators found that chronic insufficient sleep was associated with higher BMI z scores during mid-childhood, and they evaluated diet quality as a potential mediator and potential effect modifier, with partial evidence for both.
Schisterman EF, Cole SR, Platf RW. Overadjustment bias and unnecessary adjustment in epidemiologic studies. Epidemiology. 2009;20:488–95. https://doi.org/10.1097/EDE.0b013e3181a819a1.
Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Inf Libr J. 26:91–108.
Baird J, Hill CM, Harvey NC, Crozier S, Robinson SM, Godfrey KM, et al. Duration of sleep at 3 years of age is associated with fat and fat-free mass at 4 years of age: the Southampton Women’s Survey. J Sleep Res. 2016;25:412–8. https://doi.org/10.1111/jsr.12389.
•• de Souza MC, Eisenmann JC, e Santos DV, et al. Modeling the dynamics of BMI changes during adolescence. The Oporto Growth, Health and Performance Study. Int J Obes. 2015;39:1063–9. https://doi.org/10.1038/ijo.2015.60. Adolescents age 10–18 from the longitudinal Portuguese study Oporto Growth, Health and Performance Study were assessed over 3 years to determine changes in BMI during puberty. Weeknight sleep duration was not associated with BMI trajectories in fully adjusted models that included daily fruit and vegetable intake as dietary measures.
Fairley L, Santorelli G, Lawlor DA, Bryant M, Bhopal R, Petherick ES, et al. The relationship between early life modifiable risk factors for childhood obesity, ethnicity and body mass index at age 3 years: findings from the born in Bradford birth cohort study. BMC Obes. 2015;2:9. https://doi.org/10.1186/s40608-015-0037-5.
Shang L, O’Loughlin J, Tremblay A, Gray-Donald K. The association between food patterns and adiposity among Canadian children at risk of overweight. Appl Physiol Nutr Metab. 2014;39:195–201. https://doi.org/10.1139/apnm-2012-0392.
Lytle LA, Murray DM, Laska MN, Pasch KE, Anderson SE, Farbakhsh K. Examining the longitudinal relationship between change in sleep and obesity risk in adolescents. Health Educ Behav. 2013;40:362–70. https://doi.org/10.1177/1090198112451446.
• Byrne DW, Rolando LA, Aliyu MH, et al. Modifiable healthy lifestyle behaviors: 10-year health outcomes from a health promotion program. Am J Prev Med. 2016;51:1027–37. https://doi.org/10.1016/j.amepre.2016.09.012. Frequency of sleeping 7–8 hours per night and dietary intake was assessed over time via self-report among university employees. Always sleeping 7–8 hours per night was associated with lower risk of cardiometabolic outcomes than never sleeping 7–8 hours per night after accounting for poor diet and additional covariates.
Hoevenaar-Blom MP, Spijkerman AM, Kromhout D, Verschuren WM. Sufficient sleep duration contributes to lower cardiovascular disease risk in addition to four traditional lifestyle factors: the MORGEN study. Eur J Prev Cardiol. 2014;21:1367–75. https://doi.org/10.1177/2047487313493057.
Li Y, Sato Y, Yamaguchi N. Lifestyle factors as predictors of general cardiovascular disease: use for early self-screening. Asia Pac J Public Health. 2014;26:414–24. https://doi.org/10.1177/1010539511423067.
Restall A, Taylor RS, Thompson JM, et al. Risk factors for excessive gestational weight gain in a healthy, nulliparous cohort. J Obes. 2014;2014:148391–9. https://doi.org/10.1155/2014/148391.
Sayon-Orea C, Bes-Rastrollo M, Carlos S, et al. Association between sleeping hours and siesta and the risk of obesity: the SUN Mediterranean Cohort. Obes Facts. 2013;6:337–47. https://doi.org/10.1159/000354746.
Kelishadi R, Heidari Z, Kazemi I, Jafari-Koshki T, Mansourian M, Motlagh ME, et al. A hierarchical Bayesian tri-variate analysis on factors associated with anthropometric measures in a large sample of children and adolescents: the CASPIAN-IV study. J Pediatr Endocrinol Metab. 2018;31:443–9. https://doi.org/10.1515/jpem-2017-0213.
Magriplis E, Farajian P, Panagiotakos DB, et al. The relationship between behavioral factors, weight status and a dietary pattern in primary school aged children: the GRECO study. Clin Nutr. 2018; https://doi.org/10.1016/j.clnu.2018.01.015.
MacWana JI, Mehta KG, Baxi RK. Predictors of overweight and obesity among school going adolescents of Vadodara City in western India. Int J Adolesc Med Health. 2017;29. doi: https://doi.org/10.1515/ijamh-2015-0078.
Roman-Vinas B, Chaput JP, Katzmarzyk PT, et al. Proportion of children meeting recommendations for 24-hour movement guidelines and associations with adiposity in a 12-country study. Int J Behav Nutr Phys Act. 2016;13:123. https://doi.org/10.1186/s12966-016-0449-8.
Wilkie HJ, Standage M, Gillison FB, Cumming SP, Katzmarzyk PT. Multiple lifestyle behaviours and overweight and obesity among children aged 9–11 years: results from the UK site of the International Study of Childhood Obesity, Lifestyle and the Environment. BMJ Open. 2016;6:e010677. https://doi.org/10.1136/bmjopen-2015-010677.
Zhang T, Cai L, Ma L, Jing J, Chen Y, Ma J. The prevalence of obesity and influence of early life and behavioral factors on obesity in Chinese children in Guangzhou. BMC Public Health. 2016;16:954. https://doi.org/10.1186/s12889-016-3599-3.
Arora T, Taheri S. Associations among late chronotype, body mass index and dietary behaviors in young adolescents. Int J Obes. 2015;39:39–44. https://doi.org/10.1038/ijo.2014.157.
Cao M, Zhu Y, He B, Yang W, Chen Y, Ma J, et al. Association between sleep duration and obesity is age- and gender-dependent in Chinese urban children aged 6-18 years: a cross-sectional study. BMC Public Health. 2015;15:1029. https://doi.org/10.1186/s12889-015-2359-0.
D’Aniello R, Troisi J, D’Amico O, Sangermano M, Massa G, Moccaldo A, et al. Emerging pathomechanisms involved in obesity. J Pediatr Gastroenterol Nutr. 2015;60:113–9. https://doi.org/10.1097/mpg.0000000000000559.
Hunsberger M, Mehlig K, Bornhorst C, et al. Dietary carbohydrate and nocturnal sleep duration in relation to children’s BMI: findings from the IDEFICS study in eight European countries. Nutrients. 2015;7:10223–36. https://doi.org/10.3390/nu7125529.
Katzmarzyk PT, Barreira TV, Broyles ST, Champagne CM, Chaput JP, Fogelholm M, et al. Relationship between lifestyle behaviors and obesity in children ages 9-11: results from a 12-country study. Obesity (Silver Spring). 2015;23:1696–702. https://doi.org/10.1002/oby.21152.
Labree W, van de Mheen D, Rutten F, Rodenburg G, Koopmans G, Foets M. Differences in overweight and obesity among children from migrant and native origin: the role of physical activity, dietary intake, and sleep duration. PLoS One. 2015;10:e0123672. https://doi.org/10.1371/journal.pone.0123672.
• Peach H, Gaultney JF, Reeve CL. Sleep characteristics, body mass index, and risk for hypertension in young adolescents. J Youth Adolesc. 2015;44:271–84. https://doi.org/10.1007/s10964-014-0149-0. Among US sixth-graders, parent-reported sleep duration and daytime sleepiness was associated with BMI among boys whereas only daytime sleepiness was associated with BMI among girls. Daytime sleepiness had a direct effect on hypertension in boys and an indirect effect (through BMI) on hypertension in girls. Associations were independent of self-reported consumption of unhealthy foods such as soda, hotdogs, French fries and cookies.
Wijnhoven TM, van Raaij JM, Yngve A, et al. WHO European childhood obesity surveillance initiative: health-risk behaviours on nutrition and physical activity in 6–9-year-old schoolchildren. Public Health Nutr. 2015;18:3108–24. https://doi.org/10.1017/s1368980015001937.
Carrillo-Larco RM, Bernabe-Ortiz A, Miranda JJ. Short sleep duration and childhood obesity: cross-sectional analysis in Peru and patterns in four developing countries. PLoS One. 2014;9:e112433. https://doi.org/10.1371/journal.pone.0112433.
Chaput JP, Leduc G, Boyer C, Bélanger P, LeBlanc AG, Borghese MM, et al. Objectively measured physical activity, sedentary time and sleep duration: independent and combined associations with adiposity in Canadian children. Nutr Diabetes. 2014;4:e117. https://doi.org/10.1038/nutd.2014.14.
Arora T, Hosseini-Araghi M, Bishop J, Yao GL, Thomas GN, Taheri S. The complexity of obesity in U.K. adolescents: relationships with quantity and type of technology, sleep duration and quality, academic performance and aspiration. Pediatr Obes. 2013;8:358–66. https://doi.org/10.1111/j.2047-6310.2012.00119.x.
Dev DA, McBride BA, Fiese BH, Jones BL, Cho H, Behalf Of The Strong Kids Research Team. Risk factors for overweight/obesity in preschool children: an ecological approach. Child Obes. 2013;9:399–408. https://doi.org/10.1089/chi.2012.0150.
Pileggi C, Lotito F, Bianco A, Nobile CGA, Pavia M. Relationship between chronic short sleep duration and childhood body mass index: a school-based cross-sectional study. PLoS One. 2013;8:e66680. https://doi.org/10.1371/journal.pone.0066680.
Santiago S, Zazpe I, Marti A, et al. Gender differences in lifestyle determinants of overweight prevalence in a sample of southern European children. Obes Res Clin Pract. 2013;7:e391–400. https://doi.org/10.1016/j.orcp.2012.07.001.
Skidmore PM, Howe AS, Polak MA, et al. Sleep duration and adiposity in older adolescents from Otago, New Zealand: relationships differ between boys and girls and are independent of food choice. Nutr J. 2013;12:128. https://doi.org/10.1186/1475-2891-12-128.
Kjartansdottir I, Arngrimsson SA, Bjarnason R, Olafsdottir AS. Cross-sectional study of randomly selected 18-year-old students showed that body mass index was only associated with sleep duration in girls. Acta Paediatr. 2018;107:1070–6. https://doi.org/10.1111/apa.14238.
Pengpid S, Peltzer K. Prevalence of overweight and underweight and its associated factors among male and female university students in Thailand. Homo. 2015;66:176–86. https://doi.org/10.1016/j.jchb.2014.11.002.
Jayawardana NW, Jayalath WA, Madhujith WM, et al. Lifestyle factors associated with obesity in a cohort of males in the central province of Sri Lanka: a cross-sectional descriptive study. BMC Public Health. 2017;17:27. https://doi.org/10.1186/s12889-016-3963-3.
Roos V, Elmstahl S, Ingelsson E, et al. Alterations in multiple lifestyle factors in subjects with the metabolic syndrome independently of obesity. Metab Syndr Relat Disord. 2017;15:118–23. https://doi.org/10.1089/met.2016.0120.
Yan LX, Chen XR, Chen B, et al. Gender-specific association of sleep duration with body mass index, waist circumference, and body fat in Chinese adults. Biomed Environ Sci. 2017;30:157–69. https://doi.org/10.3967/bes2017.023.
Min H, Um YJ, Jang BS, Shin D, Choi EJ, Park SM, et al. Association between sleep duration and measurable cardiometabolic risk factors in healthy Korean women: the Fourth and Fifth Korean National Health and Nutrition Examination Surveys (KNHANES IV and V). Int J Endocrinol. 2016;2016:1–10. https://doi.org/10.1155/2016/3784210.
Brocato J, Wu F, Chen Y, Shamy M, Alghamdi MA, Khoder MI, et al. Association between sleeping hours and cardiometabolic risk factors for metabolic syndrome in a Saudi Arabian population. BMJ Open. 2015;5:e008590. https://doi.org/10.1136/bmjopen-2015-008590.
Grandner MA, Schopfer EA, Sands-Lincoln M, Jackson N, Malhotra A. Relationship between sleep duration and body mass index depends on age. Obesity (Silver Spring). 2015;23:2491–8. https://doi.org/10.1002/oby.21247.
Buman MP, Winkler EA, Kurka JM, et al. Reallocating time to sleep, sedentary behaviors, or active behaviors: associations with cardiovascular disease risk biomarkers, NHANES 2005–2006. Am J Epidemiol. 2014;179:323–34. https://doi.org/10.1093/aje/kwt292.
Japas C, Knutsen S, Dehom S, Dos Santos H, Tonstad S. Body mass index gain between ages 20 and 40 years and lifestyle characteristics of men at ages 40-60 years: the Adventist Health Study-2. Obes Res Clin Pract. 2014;8:e549–57. https://doi.org/10.1016/j.orcp.2013.11.007.
Parvaneh K, Poh BK, Hajifaraji M, Ismail MN. Sleep deprivation is related to obesity and low intake of energy and carbohydrates among working Iranian adults: a cross sectional study. Asia Pac J Clin Nutr. 2014;23:84–90. https://doi.org/10.6133/apjcn.2014.23.1.02.
Yu S, Guo X, Yang H, Zheng L, Sun Y. An update on the prevalence of metabolic syndrome and its associated factors in rural northeast China. BMC Public Health. 2014;14:877. https://doi.org/10.1186/1471-2458-14-877.
Georgousopoulou EN, D’Cunha NM, Mellor DD, et al. The association between sleeping time and metabolic syndrome features, among older adults living in Mediterranean Region: the MEDIS study. Metab Syndr Relat Disord. 2018;16:20–8. https://doi.org/10.1089/met.2017.0113.
Georgousopoulou EN, Naumovski N, Mellor DD, et al. Association between siesta (daytime sleep), dietary patterns and the presence of metabolic syndrome in elderly living in Mediterranean area (MEDIS study): the moderating effect of gender. J Nutr Health Aging. 2017;21:1118–24. https://doi.org/10.1007/s12603-016-0865-0.
Rangan A, Zheng M, Olsen NJ, et al. Shorter sleep duration is associated with higher energy intake and an increase in BMI z-score in young children predisposed to overweight. Int J Obes. 2017; https://doi.org/10.1038/ijo.2017.216.
Asarnow LD, McGlinchey E, Harvey AG. Evidence for a possible link between bedtime and change in body mass index. Sleep. 2015;38:1523–7. https://doi.org/10.5665/sleep.5038.
•• He F, Bixler EO, Liao J, et al. Habitual sleep variability, mediated by nutrition intake, is associated with abdominal obesity in adolescents. Sleep Med. 2015;16:1489–94. https://doi.org/10.1016/j.sleep.2015.07.028. This study of US adolescents found that actigraphy-assessed sleep duration variability was associated with higher abdominal fat measured by dual X-ray absorptiometry (DXA). Further, they found evidence of partial mediation by total energy intake, measured by a food frequency questionnaire.
McDonald L, Wardle J, Llewellyn CH, Fisher A. Nighttime sleep duration and hedonic eating in childhood. Int J Obes. 2015;39:1463–6. https://doi.org/10.1038/ijo.2015.132.
Cespedes EM, Rifas-Shiman SL, Redline S, Gillman MW, Peña MM, Taveras EM. Longitudinal associations of sleep curtailment with metabolic risk in mid-childhood. Obesity (Silver Spring). 2014;22:2586–92. https://doi.org/10.1002/oby.20894.
• Timmermans M, Mackenbach JD, Charreire H, et al. Exploring the mediating role of energy balance-related behaviours in the association between sleep duration and obesity in European adults. The SPOTLIGHT project. Prev Med. 2017;100:25–32. https://doi.org/10.1016/j.ypmed.2017.03.021. Mediation of the association between longer sleeping (≥ 9 hours) and obesity by dietary intake behaviors was assessed in urban-dwelling European adults. Longer sleep duration was associated with a lower likelihood of obesity than short sleep duration (< 7 hours), but there was no evidence of mediation by diet.
• Kanagasabai T, Ardern CI. Contribution of inflammation, oxidative stress, and antioxidants to the relationship between sleep duration and cardiometabolic health. Sleep. 2015;38:1905–12. https://doi.org/10.5665/sleep.5238. The association between vitamins and carotenoids and metabolic syndrome was assessed in a nationally-representative study of US adults. Carotenoids, vitamins C and D were modest mediators of the relationship between sleep duration and the metabolic syndrome among women.
Wirth MD, Hébert JR, Hand GA, Youngstedt SD, Hurley TG, Shook RP, et al. Association between actigraphic sleep metrics and body composition. Ann Epidemiol. 2015;25:773–8. https://doi.org/10.1016/j.annepidem.2015.05.001.
Chaput JP, Bouchard C, Tremblay A. Change in sleep duration and visceral fat accumulation over 6 years in adults. Obesity (Silver Spring). 2014;22:E9–12. https://doi.org/10.1002/oby.20701.
Mesas AE, Guallar-Castillon P, Lopez-Garcia E, et al. Sleep quality and the metabolic syndrome: the role of sleep duration and lifestyle. Diabetes Metab Res Rev. 2014;30:222–31. https://doi.org/10.1002/dmrr.2480.
Yeh SS, Brown RF. Disordered eating partly mediates the relationship between poor sleep quality and high body mass index. Eat Behav. 2014;15:291–7. https://doi.org/10.1016/j.eatbeh.2014.03.014.
National Cholesterol Education Program Expert Panel, National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–421. https://doi.org/10.1161/01.CIR.0000048067.86569.
•• Hjorth MF, Sjodin A, Dalskov SM, et al. Sleep duration modifies effects of free ad libitum school meals on adiposity and blood pressure. Appl Physiol Nutr Metab. 2016;41:33–40. https://doi.org/10.1139/apnm-2015-0319. Children from Denmark were enrolled in a crossover trial, in which they were fed a New Nordic Diet (NND) lunch for 1 month and had usual packed lunches for 1 month. Among children with habitual short sleep (assessed with actigraphy), the NND resulted in fat mass gain compared usual lunch consumption.
Doo H, Chun H, Doo M. Associations of daily sleep duration and dietary macronutrient consumption with obesity and dyslipidemia in Koreans: a cross-sectional study. Med. 2016;95:e5360. https://doi.org/10.1097/md.0000000000005360.
Doo M, Kim Y. The consumption of dietary antioxidant vitamins modifies the risk of obesity among Korean men with short sleep duration. Nutrients. 2017;9:E780.
Kim NH, Shin DH, Kim HT, Jeong SM, Kim SY, Son KY. Associations between metabolic syndrome and inadequate sleep duration and skipping breakfast. Korean J Fam Med. 2015;36:273–7. https://doi.org/10.4082/kjfm.2015.36.6.273.
Chaput J-P. Sleep patterns, diet quality and energy balance. Physiol Behav. 2014;134:86–91. https://doi.org/10.1016/j.physbeh.2013.09.006.
Reutrakul S, Van Cauter E. Sleep influences on obesity, insulin resistance, and risk of type 2 diabetes. Metabolism.
Espitia-Bautista E, Velasco-Ramos M, Osnaya-Ramírez I, et al. Social jet-lag potentiates obesity and metabolic syndrome when combined with cafeteria diet in rats. Metabolism. 2017; https://doi.org/10.1016/j.metabol.2017.04.006.
Acknowledgements
Dr. Jansen was supported by the National Institutes of Health/National Heart, Lung, and Blood Institute grant 5T32HL110952-05. Dr. Dunietz was supported by the National Institutes of Health/Eunice Kennedy Shriver National Institute of Child Health and Development grant F32 HD091938. Dr. Tsimpanouli was supported by the University of Michigan Postdoctoral Translational Scholars program (UL1TR002240).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Erica C. Jansen, Galit Levi Dunietz, Maria-Efstratia Tsimpanouli, Heidi M. Guyer, Carol Shannon, Shelley D. Hershner, Louise M. O’Brien, and Ana Baylin declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
This article is part of the Topical Collection on Diabetes and Obesity
Rights and permissions
About this article
Cite this article
Jansen, E.C., Dunietz, G.L., Tsimpanouli, ME. et al. Sleep, Diet, and Cardiometabolic Health Investigations: a Systematic Review of Analytic Strategies. Curr Nutr Rep 7, 235–258 (2018). https://doi.org/10.1007/s13668-018-0240-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13668-018-0240-3