Abstract
Introduction
The purpose of this study was to quantify United States (US) and United Kingdom (UK) physicians’ preferences for attributes of type 2 diabetes treatments.
Methods
Samples of general practitioners (GPs) and endocrinologists in the US (n = 204) and the UK (n = 200) completed a discrete-choice experiment in which respondents chose between pairs of hypothetical type 2 diabetes treatments in a series of trade-off questions. The questions described hypothetical injectable treatments with differing levels of attributes, such as glucose control and treatment side effects. Relative importance of attributes was estimated by a multivariate regression model for limited dependent variables. These results were used to calculate how the predicted probability of choosing hypothetical type 2 diabetes treatments varies with changes in given attributes.
Results
The most important attributes to physicians were glucose control, risk of a fatal myocardial infarction (MI), and weight change. For US physicians, glucose control was about twice as important as gastrointestinal side effects, 5 times more important than changes in depression symptoms, and 20 times more important than liver monitoring. For UK physicians, reduction in MI risk was about 1.5 times more important than glucose control, 2.5 times more important than gastrointestinal side effects, and 10 times more important than liver-monitoring requirements. Preferences were similar among physicians in the US and the UK and among GPs and endocrinologists.
Conclusions
Physicians valued type 2 diabetes treatments that go beyond glycemic control, although mitigating different complications and comorbidities was not equally as important.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes causes significant clinical and economic burden in the US and the UK [1–4]. Achieving effective glycemic control in patients with diabetes reduces microvascular complications, as well as long-term risks of macrovascular disease [5]. Even with glycemic control, complications and comorbidities, including cardiovascular disease, depression, and obesity, have significant effects on both the clinical and economic burden of type 2 diabetes. In particular, patients with type 2 diabetes have two to four times higher risk of cardiovascular disease than adults without diabetes, which constitutes the largest share of the cost of diabetes [1, 5, 6]. Depression is at least twice as prevalent among individuals with diabetes as it is among non-diabetics, increasing the risk of diabetic complications [7, 8]. Finally, obese adults are much more likely to have diabetes than adults who are not obese [3]. About 13% of the expenditures on metabolic conditions (including the estimated annual costs of $92.6 billion on obesity in the US) are attributable to diabetes [3, 9, 10]. In addition, liver abnormalities are more prevalent among individuals with diabetes; thus, managing diabetes could be complicated by liver-related alterations in drug metabolism, drug interactions, and risk of hepatotoxicity [11].
An additional challenge is that almost one-third of diabetic patients do not adhere to their treatment regimen, leading to poorer glycemic control and increased risk of complications, hospitalizations, and death [12–14]. A recent review identified more frequent or complex dosing, treatment-related weight gain, persistent gastrointestinal (GI) side effects, and depression to be among the factors that impair adherence [15].
Diabetes outcomes are improved when management goes beyond glycemic control to managing comorbidities and complications [5], and such therapies have been a focus of research and clinical practice [16]. However, little is known about how prescribing physicians weigh the relative importance of glucose control, managing comorbidities and complications, and other treatment attributes that could affect adherence. The objective of this study was to quantify US and UK physicians’ preferences for extra-glycemic benefits of type 2 diabetes relative to other attributes of type 2 diabetes treatments. There are no type 2 diabetes treatments with proven depression benefits, and most treatments (with the exception of thiazolidinediones) do not require liver monitoring. Thus, the latter two outcomes are novel with respect to existing treatments, and this study is exploratory in terms of understanding preferences for these outcomes.
A discrete-choice-experiment (DCE) survey provided data on physician respondents’ evaluations of pairs of hypothetical diabetes treatments. Treatment profiles described hypothetical injectable treatments with differing levels of treatment attributes. DCE is a valid and reliable survey technique for eliciting trade-offs to quantify the relative importance respondents assign to attributes and outcomes of health interventions [17, 18]. These methods increasingly are used to quantify preferences for treating diabetes and other health conditions [19–22].
Materials and Methods
A DCE is based on the principle that medical treatments are comprised of multiple characteristics. Physicians’ disposition to prescribe a treatment depends on the characteristics of both the treatment and the patient being treated. In a DCE, respondents make hypothetical prescribing decisions about constructed treatment alternatives. The researcher controls the features of the treatment alternatives and the patient characteristics; physicians’ patterns of choices are analyzed to estimate the implicit relative importance weights physicians use to identify preferred treatment alternatives [17, 23].
Survey Development, Pretests, and Administration
This study described hypothetical injectable type 2 diabetes treatments using seven treatment features (or attributes) based on published literature, consultation with clinical experts, and one-on-one interviews with physicians. The treatments of interest were non-insulin injectables used to treat patients who had failed to respond to two or three oral medications. The following criteria were used to identify attributes that: (a) were of potential therapeutic interest; (b) were clinically relevant; (c) reflected other, nonclinical features of concern to physicians; and/or (d) incorporated physicians’ assessments of patient concerns. The resulting attributes included: glucose control [treated hemoglobin A1c (HbA1c) levels], weight change, frequency of injection, GI side effects, requirement for liver monitoring, reduction in the 5-year risk of a fatal myocardial infarction (MI), and reduction in depression symptoms (Table 1).
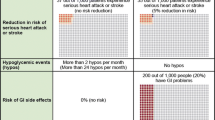
The first section of the survey instrument obtained information on physicians’ characteristics and experience in treating patients with type 2 diabetes, as well as their target level of glucose control for a type 2 diabetes patient with the following characteristics: aged 45–65 years, obese class II (body mass index 35–40 kg/m2), sedentary lifestyle, moderate depression (a score of 15–19 on the Patient Health Questionnaire or a score of 14–18 on the Hamilton Depression Rating Scale), failure to respond to two or three oral agents, and an HbA1c level of 9%. The second section provided physician respondents with definitions of the treatment attributes and levels. Levels are specific values for the treatment attributes. For example, weight change is an attribute, which may take on several possible levels such as 5% weight gain, 5% weight loss, or 10% weight loss. MI risks were presented as frequencies [24]. The third section included the trade-off questions that asked physicians to choose which of two hypothetical injectable treatment profiles they would recommend as the next line of treatment for the patient described (Fig. 1). All hypothetical treatments were injectables, because injectables often are the next line of treatment for patients with the target profile.
The draft survey instrument was pretested and refined based on in-depth, semistructured interviews conducted with 15 physicians in the US and 5 physicians in the UK. The objectives of the pretests were to test the understandability of the survey instrument, the appropriateness of descriptive information, and the cognitive burden of the trade-off questions. The US pretests were completed first. The final survey instrument for the US study was adapted for the UK, and the UK pretests were used to evaluate whether any cultural adaptations were necessary to facilitate comprehension of the survey concepts. As with the final sample, around half of the US pretest respondents were endocrinologists and the other half were primary care physicians, internists, or family practitioners. All UK pretest respondents were general practitioners (GPs). The sample in the UK had more experience, having been in practice at least 16 years, while the US sample had 1 to >25 years of experience. The UK sample treated fewer patients per week, on average, than the US sample. As described below, similar differences in experience and number of patients were observed in the full study sample.
As a result of the pretest findings, the survey instrument was adapted to improve the descriptive information, and to reduce the cognitive burden of the trade-off questions. Statements were added regarding what the hypothetical treatments would be in addition to oral treatments, and that the treatment outcomes already accounted for potential interactions between glucose control, weight loss, and MI risk. The question about target HbA1c was added as physicians in the pretests reported various HbA1c targets. In addition, the glucose control attribute was changed from describing changes in HbA1c (e.g., “0.7% reduction”) to describing the level to which HbA1c was reduced. The GI side effects attribute was refined to describe the severity of symptoms, and a number of revisions to the patient profile were made, including adding the baseline level of HbA1c, narrowing the BMI range from 35–45 kg/m2 to 40–45 kg/m2, and dropping a second patient profile in which the patient had no depression. A number of minor editorial changes were also made based on the pretests, and the final survey instrument was programed for online administration.
To create the stimuli used to construct the treatment profiles and pairs in the choice questions, we employed a D-efficient experimental design that resulted in 96 hypothetical treatment pairs [25–27]. Because the quality of responses to choice questions declines as the number of choice tasks increases, leading to fatigue or cognitive burden [28, 29], we divided the 96 paired comparisons in the experimental design into eight survey versions, each containing 12 choice questions. Each physician was randomly assigned to one of the eight versions of the experimental design, and the order of the choice questions was also randomized for each respondent.
Sample Recruitment
Physicians from an online opt-in physician panel were invited to complete the survey by e-mail. Physicians were recruited to the panel by phone, online, or face-to-face interviews with eligibility verified by a third party at their place of work. As an opt-in panel, some potential selection bias might exist, such as panel members being more interested in and/or more available for participation in survey research. Invitations to participate in the survey were sent to a random sample of panel members who met the sample inclusion criteria: (1) board-eligible or board-certified primary care physicians in the US or GPs in the UK or endocrinologists from either country, and (2) treat patients with type 2 diabetes regularly. The panel recruitment and study recruitment procedures were the same in the US and the UK.
There are no power calculations for DCEs [30]. Most published conjoint analysis studies have a sample size between 100 and 300 respondents [18]. However, minimum sample size depends on a number of criteria, including the question format, the complexity of the choice task, the desired precision of the results, and the need to conduct subgroup analyses [30]. Given the results of a recent meta-regression [30], the research team’s previous experience, previously published studies [18], and an interest in estimating separate results for the UK and US samples, the study aimed to interview 200 respondents in each country.
The Office of Research Protection and Ethics at Research Triangle Institute granted a consent exemption for this study, indicating that this research did not meet the definition of human (or animal) subjects research. US physicians received a $55 cash honorarium for participating in the survey. UK GPs received the equivalent of a $66 cash honorarium, while UK endocrinologists were given the equivalent of $75. The 25-minute online survey was administered in February 2012.
Statistical Analysis
The pattern of physicians’ responses to the choice questions was analyzed using a random-parameters logit (RPL) model. Results from the RPL model are log-odds estimates relative to the mean effect normalized at zero and represent the weighted effect of each treatment attribute level on respondents choosing a profile containing that attribute level. These estimates also can be interpreted as preference weights indicating the relative strength of preference for each attribute, and differences between preference weights indicate the relative strength of preference for changes among attribute levels in the study.
The parameter estimates were combined with the treatment profiles in the experimental design to obtain a conjoint-utility index that indicated the average value score that physicians would assign to prescribing the treatment of interest to the target patient. The conjoint-utility index was used to examine how predicted choice probabilities (the likelihood that one treatment would be chosen over another treatment) would change in response to changes in a single medication attribute, other factors held constant.
Results
Physician Sample Characteristics
E-mail invitations to participate in the survey were sent to 691 physicians in the US and 1,915 physicians in the UK. Of these, 264 US physicians (38.2%) and 306 UK physicians (15.9%) responded. Of the physicians who responded, 204 (77.3%) in the US and 200 (65.4%) in the UK met the inclusion criteria and completed the survey.
One respondent in each of the US and UK samples had no variation in their treatment-profile choices (always picked treatment A or treatment B). They were deleted from the sample as this lack of variation in response likely indicated that they did not pay attention to the choice questions. The final sample sizes used for analysis were therefore 203 physicians in the US and 199 in the UK.
The characteristics of the respondents the US and UK samples are shown in Table 2. The average UK physician was younger and had not been in practice as long as the average US physician (P < 0.05). UK physicians treated fewer patients than US physicians (P < 0.05), and a larger percentage of the UK physicians selected higher target HbA1c levels for the patient profile (P < 0.01).
Preferences for Treatment Attributes
Figure 2 presents the estimated log-odds preference estimates for US and UK physicians and the 95% confidence intervals (CI) for the seven treatment attributes. The estimated preference weights were generally consistent with the natural order of attribute levels (e.g., lower HbA1c levels were preferred to higher HbA1c levels). In three instances, the order of measured preference weights were inconsistent with the expected order of preference for the attribute levels: one injection per day was preferred to one injection every other day in the US sample; one injection per week was preferred to one injection every month in the US sample; and GI side effects that resolved after taking the medication for 2 weeks were preferred to no GI side effects in the UK sample. However, the differences between disordered preference weights were not statistically significant (P > 0.05).
The difference between the most-preferred and least-preferred level of an attribute indicates the overall relative importance of each attribute, conditional on the attributes and levels shown in the survey. The overall relative importance of all medication attributes except glucose control were similar across the US and UK samples (P > 0.05), indicating that physicians in the US and UK samples had similar preferences. However, glucose control was more important to US physicians than to UK physicians (P < 0.01).
Although glucose control was the most important attribute for US physicians, the relative importance of this attribute was not significantly different from the importance of reducing the 5-year risk of experiencing a fatal MI, and change in body weight, which were the second and third most important attributes. For UK physicians in the sample, a reduction in the 5-year risk of experiencing a fatal MI was the most important attribute, followed by change in body weight and glucose control. For physicians in both countries, liver monitoring and changes in depression symptoms were the least important attributes of the medication.
GPs and endocrinologists in both countries had similar preferences for treatment attributes. In the US, preference weights for treatment attributes were not significantly different between GPs and endocrinologists (P > 0.05). However, in the UK, GPs had significantly lower preference weights for liver monitoring requirements than for no liver monitoring requirements (P < 0.05), whereas endocrinologists did not distinguish between medications requiring liver monitoring and those that did not (P > 0.05). The overall relative importance of the remaining attributes was not significantly different between UK endocrinologists and GPs (P > 0.05).
Figure 3 summarizes selected marginal choice probabilities. All marginal choice probabilities for the study are reported in an online Appendix. For example, if a treatment further improves HbA1c to 7.0% compared with 8.3% from a baseline level of 9%, the predicted choice probability for that treatment increases by 46 and 41 percentage points in the US and UK samples, respectively. If depression benefits improve from having no effect on moderate depression symptoms to eliminating moderate depression symptoms, the predicted choice probability increases by 15 and 12 percentage points in the US and UK samples, respectively.
Selected estimates of marginal choice probabilities for given improvements in medication attributesa,b. HbA1c hemoglobin A1c, GI gastrointestinal, MI myocardial infarction. aThe estimates implicitly assume that all attributes other than that being valued remain unchanged. b Brackets indicate 95% CIs. cThe patient profile indicated that the patient had a baseline HbA1c level of 9%. dThe marginal choice probability was not calculated for this change, because the estimated preferences for this sample were not consistent with the natural ordering of the medication feature
The largest marginal choice probabilities in both the US and UK samples were associated with the largest changes in glucose control (from 8.3 to 7.0%), body weight (from 5% weight gain to 20% weight loss), and the 5-year risk of fatal MI (from 0 to 1.5%) (Fig. 3). In the US sample, the smallest positive marginal choice probability (4%) was associated with changes in liver monitoring requirements (from monitoring liver enzymes every month for the first 3 months, then quarterly as long as the patient takes the medicine, to no liver monitoring requirements). In the UK sample, the smallest positive marginal choice probability (2%) was associated with changes in depression symptoms.
Larger changes in GI side effects (from continuing as long as patient takes medicine, to either resolving after 2 weeks, or no GI side effects) were more important than relatively small changes in efficacy (from an HbA1c of 8.3 to 8.0%). Also, avoiding a 5% weight gain was two to three times as important to physicians as a 5% weight loss (Fig. 3). That is, avoiding a 5% weight gain was predicted to increase the choice probability by 18 or 21 percentage points, depending on the sample, while a 5% weight loss would increase the choice probability by only 5 or 11 percentage points, on average.
To assess whether preference differences were due to differences in age and experience between the US and UK physicians, interaction terms were added to the US and UK models. Respondents’ reported age and years of experience were interacted with each treatment-attribute variable. The significance of the all age interactions and all experience interactions were tested separately; neither set of interactions was found to be statistically significant. Given that the estimates for the age interaction terms and experience interaction terms represent adjustments to preference weights based on respondents’ age and years of experience, respectively, these results indicate that there was no statistically significant effect of age or experience on preferences for treatment attributes.
Discussion
US and UK physicians in our sample valued type 2 diabetes treatments that would go beyond glycemic control (i.e., HbA1c reduction) to help control diabetes complications and comorbidities. Physicians placed about as much overall importance on cardiovascular and weight benefits from diabetes treatments as they placed on glucose control. Physicians did not place much overall importance on depression benefits or on requirements for liver monitoring. We can only speculate about why physicians value some extra-glycemic benefits more than others. Physicians may place greater weight on familiar attributes than on attributes that are not present in currently marketed diabetes medications.
Our survey-development activities indicated that the links between diabetes and both weight and cardiovascular outcomes were well documented in the literature and well understood by the physicians who participated in the pretests. However, the links between type 2 diabetes and depression are not as well documented, and pretest physicians varied in the extent to which they considered diabetes and depression to be correlated. Some physicians in the pretest also noted that there are numerous effective and inexpensive depression medications currently available, and one physician was concerned that combining treatments would limit the extent to which depression medications could be titrated.
On average, physicians placed a low weight on liver monitoring requirements. Many of the pretest physicians noted that they test diabetes patients’ glucose levels frequently and can conduct a liver monitoring test using the blood drawn for that purpose without changing treatment practices.
To our knowledge, there has been only one previously published study of physicians’ preferences for type 2 diabetes treatments. Porzsolt and colleagues [31] examined German physicians’ relative preferences for glucose control, side effects, convenience, and weight change. Our findings are consistent with their results, that weight change was as important to German physicians as glucose control.
Larger changes in GI side effects were more important than relatively small (and less clinically meaningful) changes in efficacy, and about as important as changes in fatal MI risk and larger changes in weight loss. Many pretest physicians stated that GI side effects were key factors in treatment adherence and persistence.
Physicians had a strong aversion to weight gain. This has been observed in other studies [32] and suggests that avoiding even a relatively small weight gain among patients like the one described in the survey is more important than a similarly small weight loss.
The study was conducted in the US and the UK to explore physicians’ relative preferences for extra-glycemic control outcomes in two settings with different health care systems. Preferences for type 2 diabetes treatment outcomes generally were similar in the two samples. The three most important attributes in the US sample were glucose control, MI risk reduction, and weight change, though the importance differences were not statistically significant. The three most important attributes in the UK sample were the same, however, glucose control was less important than MI risk reduction (P < 0.05) while the importance differences for weight change and MI risk reduction were not statistically different. Glucose control was less important in the UK sample than in the US sample (P < 0.01). The reason for this is not clear from the study, though differences in experience and the health care systems could play a part. Physicians in the UK were younger, on average; had been practicing fewer years; and reported higher target HbA1c levels for the patient profiled in the survey than the US sample. However, regression analyses suggested that age and experience did not influence estimated preferences. It is possible that the differences are due to other differences in the study populations, perhaps related to different response rates in the US and the UK. The same processes and criteria were used to recruit physicians to the panel and to invite physicians to participate in the study, but there are potentially many other factors (e.g., holidays, professional conferences, other studies in same topic) that may have influenced enrollment differently between the two countries. However, we are not aware of any information indicating that other factors may have affected the response rates in this study.
Finally, at the time of the survey, the American Diabetes Association standards of care [33] indicated that lowering HbA1c to <7% was a reasonable goal for many non-pregnant adults and the National Institute for Health and Care Excellence’s (NICE) quality standard [34] defined clinical best practice as an HbA1c target between 6.5 and 7.5%. Further, the NICE quick reference guide for the management of type 2 diabetes suggests that target HbA1c levels be individualized, with less stringent targets (<7.5%) for patients on multiple therapies. The fact that guidelines in the UK permitted higher HbA1c targets could partially account for the fact that more UK physicians than US physicians selected higher HbA1c targets for the profiled patient.
Based on the pretests, discussions with clinical experts, and reviews of publicly available information about treatment and referral guidelines, we hypothesized that there would be differences in preferences between endocrinologists on the one hand and all other specialties that treat diabetes on the other. While all of these specialties treat patients with type 2 diabetes, it appears that endocrinologists tend to see more advanced or acute cases (though there may be exceptions). The results indicated that the preferences of GPs and endocrinologists were similar in both the US and the UK, with the exception of differences in preference for liver monitoring among GPs and endocrinologists in the UK.
Despite the increasing use of DCE in health applications to elicit preferences, this approach has several limitations. First, physician choices among hypothetical treatment profiles do not have the same clinical consequences as actual choices. We minimized the potential for hypothetical bias by offering treatments that mimic real-world trade-offs as closely as possible. Second, physicians’ actual medication choices may differ from predicted choices because actual choices depend on a number of clinical, institutional, and financial factors that were beyond the scope of this study. This study limited the characterization of hypothetical diabetes treatments to seven treatment attributes and excluded, for example, the risk of pancreatitis. The US Food and Drug Administration (FDA) [35] and recent literature [36, 37] have highlighted controversies about the possible risks of pancreatitis and pancreatic cancer associated with some diabetes treatments. Third, we cannot fully judge how representative our physician samples were or whether our results are generalizable to all physicians in the US and the UK. Fourth, the results we present relate to the patient profile that physicians were asked to consider. The sample was insufficient to explore physician preferences for different patient profiles. Finally, this study was not designed to support development of treatment guidelines or to provide clinical advice.
The study also has a number of strengths from using best practices [17]. In particular, the survey was carefully designed in collaboration with clinical experts, was pretested using in-depth interviews with physicians in the US and the UK, and employed a state-of-the-art experimental design. The choice data were analyzed using advanced RPL methods that avoid estimation bias from unobserved variation in preferences across the sample and within-sample correlation in the choice sequence for each respondent. We also tested for the effect of systematic preference differences by age, experience, and medical specialty.
Conclusion
This study provides evidence that physicians place about as much importance on a type 2 diabetes medication’s cardiovascular and weight outcomes as they place on glucose control. We found broad consensus about treatment priorities among physicians with different personal and professional characteristics who treat diabetic patients. These findings are consistent with the challenges in diabetes care, in which cardiovascular disease and obesity continue to be problems. However, physicians place relatively low importance on the attributes describing depression benefits and liver monitoring requirements in this study. As the literature regarding the links between diabetes and depression and liver abnormalities matures, physicians and stakeholders should become better informed about these links and physicians’ relative preferences for type 2 diabetes treatments may change.
References
Centers for Disease Control and Prevention. National Diabetes Fact Sheet: National estimates and general information on diabetes and prediabetes in the United States, 2011; 2011. http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf (Accessed Dec 13, 2012).
Diabetes UK. Diabetes in the UK 2012: key statistics on diabetes; 2012. http://www.diabetes.org.uk/Documents/Reports/Diabetes-in-the-UK-2012.pdf (Accessed Dec 13, 2012).
American Diabetes Association. Economic costs of diabetes in the U.S. in 2007. Diabetes Care. 2008;31:596–615.
Kanavos P, van den Aardweg S, Schurer W. Diabetes expenditure, burden of disease and management in 5 EU countries; 2012. http://www2.lse.ac.uk/LSEHealthAndSocialCare/research/LSEHealth/MTRG/LSEDiabetesReport26Jan2012.pdf (Accessed Dec 13, 2012).
American Diabetes Association. Standards of medical care in diabetes—2010. Diabetes Care. 2009;33(Suppl. 1):S11–61.
Franco OH, Steyerberg EW, Hu FB, Mackenbach J, Nusselder W. Associations of diabetes mellitus with total life expectancy and life expectancy with and without cardiovascular disease. Arch Intern Med. 2007;167:1145–51.
Lloyd C. The effects of diabetes on depression and depression on diabetes. Diabetes Voice. 2008;53:23–6.
Lustman PJ, Clouse RE. Depression in diabetic patients: the relationship between mood and glycemic control. J Diabetes Complicat. 2005;19:113–22.
Kopelman PG. Obesity as a medical problem. Nature. 2000;404:635–43.
Finkelstein EA, Fiebelkorn IC, Wang G. National medical spending attributable to overweight and obesity: how much, and who’s paying? Health Aff (Millwood). 2003;Suppl Web Exclusives:W3-219–26.
Tolman KG, Fonseca V, Dalpiaz A, Tan MH. Spectrum of liver disease in type 2 diabetes and management of patients with diabetes and liver disease. Diabetes Care. 2007;30:734–43.
DiMatteo MR. Variations in patients’ adherence to medical recommendations: a quantitative review of 50 years of research. Med Care. 2004;42:200–9.
Ho PM, Rumsfeld JS, Masoudi FA, et al. Effect of medication nonadherence on hospitalization and mortality among patients with diabetes mellitus. Arch Intern Med. 2006;166:1836–41.
Pladevall M, Williams LK, Potts LA, Divine G, Xi H, Lafata JE. Clinical outcomes and adherence to medications measured by claims data in patients with diabetes. Diabetes Care. 2004;27:2800–5.
Bailey CJ, Kodack M. Patient adherence to medication requirements for therapy of type 2 diabetes. Int J Clin Pract. 2011;65:314–22.
Nathan DM, Buse JB, Davidson MB, et al. Management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2006;29:1963–72.
Bridges JF, Hauber AB, Marshall D, et al. Conjoint analysis applications in health—a checklist: a report of the ISPOR Good Research Practices for Conjoint Analysis Task Force. Value Health. 2011;14:403–13.
Marshall D, Bridges JF, Hauber B, et al. Conjoint analysis applications in health—how are studies being designed and reported? An update on current practice in the published literature between 2005 and 2008. Patient. 2010;3:249–56.
Hauber AB, Johnson FR, Sauriol L, Lescrauwaet B. Risking health to avoid injections: preferences of Canadians with type 2 diabetes. Diabetes Care. 2005;28:2243–5.
Hauber AB, Mohamed AF, Johnson FR, Falvey H. Treatment preferences and medication adherence of people with Type 2 diabetes using oral glucose-lowering agents. Diabet Med. 2009;26:416–24.
Johnson FR, Hauber B, Özdemir S, Siegel CA, Hass S, Sands BE. Are gastroenterologists less tolerant of treatment risks than patients? Benefit-risk preferences in Crohn’s disease management. J Manag Care Pharm. 2010;16:616–28.
Poulos C, Yang JC, Levin C, Van Minh H, Giang K, Nguyen D. Mothers’ preferences and willingness to pay for HPV vaccines in Vinh Long Province, Vietnam. Soc Sci Med. 2011;73:226–34.
Louviere JJ, Hensher DA, Swait JD. Stated choice methods: analysis and applications. New York: Cambridge University Press; 2000.
Akl EA, Oxman AD, Herrin J, et al. Using alternative statistical formats for presenting risks and risk reductions. Cochrane Database Syst Rev. 2011;16:CD006776.
Dey A. Orthogonal fractional factorial designs. New York: Halstead Press; 1985.
Kanninen B. Optimal design for multinomial choice experiments. J Mark Res. 2002;39:214–27.
Reed Johnson F, Lancsar E, Marshall D, et al. Constructing experimental designs for discrete-choice experiments: report of the ISPOR Conjoint Analysis Experimental Design Good Research Practices Task Force. Value Health. 2013;16:3–13.
Bech M, Kjaer T, Lauridsen J. Does the number of choice sets matter? Results from a web survey applying a discrete choice experiment. Health Econ. 2011;20:273–86.
Swait J, Adamowicz W. The influence of task complexity on consumer choice: a latent class model of decision strategy switching. J Consum Res. 2001;28:135–48.
Johnson FR, Yang J-C, Mohamed AF. In defense of imperfect experimental designs: statistical efficiency and measurement error in choice-format conjoint analysis. Podium presentation at the 4th conjoint analysis in health conference, Orlando; 2012.
Porzsolt F, Clouth J, Deutschmann M, Hippler HJ. Preferences of diabetes patients and physicians: a feasibility study to identify the key indicators for appraisal of health care values. Health Qual Life Outcomes. 2010;8:125.
Matza LS, Yurgin N, Boye KS, Malley K, Shorr JM. Obese versus non-obese patients with type 2 diabetes: patient-reported outcomes and utility of weight change. Curr Med Res Opin. 2007;23:2051–62.
American Diabetes Association. Standards of medical care in diabetes—2012. Diabetes Care. 2012;35 Suppl. 1:S11–63.
National Institute for Health and Care Excellence (NICE). Diabetes in Adults. Quality Standards QS6. c2013. http://www.nice.org.uk/guidance/QS6 (Accessed 30 Aug, 2013).
U.S. Food and Drug Administration. FDA Drug Safety Communication: FDA investigating reports of possible increased risk of pancreatitis and pre-cancerous findings of the pancreas from incretin mimetic drugs for type 2 diabetes. http://www.fda.gov/drugs/drugsafety/ucm343187.htm (Accessed 30 Aug, 2013).
Nauck MA. A critical analysis of the clinical use of incretin-based therapies: the benefits by far outweigh the potential risks. Diabetes Care. 2013;36:2126–32.
Butler PC, Elashoff M, Elashoff R, Gale EA. A critical analysis of the clinical use of incretin-based therapies: are the GLP-1 therapies safe? Diabetes Care. 2013;36:2118–25.
Acknowledgments
The study which is the subject of this manuscript was conducted by RTI Health Solutions and funded by Eli Lilly and Company. The article processing charges were funded by Eli Lilly.
Dr. Poulos is the guarantor for this article, and takes responsibility for the integrity of the work as a whole.
Conflict of interest
Christine Poulos, Juan Marcos González and F. Reed Johnson declare no conflict of interest.
At the time of the study, Lauren J. Lee was a full time employee and stock owner of Eli Lilly and Company.
Kristin S. Boye is a full time employee and stock owner of Eli Lilly and Company.
Jay P. Bae is a full time employee and stock owner of Eli Lilly and Company.
Mark A. Deeg is a full time employee and stock owner of Eli Lilly and Company.
Compliance with ethical guidelines
The Office of Research Protection and Ethics at Research Triangle Institute granted a consent exemption for this study. This article does not contain any studies with human or animal subjects performed by any of the authors.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix
Appendix
See Table 3.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License (https://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Poulos, C., González, J.M., Lee, L.J. et al. Physician Preferences for Extra-Glycemic Effects of Type 2 Diabetes Treatments. Diabetes Ther 4, 443–459 (2013). https://doi.org/10.1007/s13300-013-0046-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-013-0046-7