Abstract
Purpose of Review
To review the data on the Aspergillus lateral flow assay for the diagnosis of invasive Aspergillosis.
Recent Findings
Aspergillus spp. cause a wide spectrum of disease with invasive aspergillosis (IA) as its most severe manifestation. Early and reliable diagnosis of disease is crucial to decrease associated morbidity and mortality, and enable prompt initiation of treatment for IA. Most recently, non-culture-based tests, such as Aspergillus galactomannan (GM), have been useful in early identification and treatment of patients with IA. However, cost, turnaround time, and variable performance indifferent populations at risk for IA remain significant drawbacks to the use of this test. Several diagnostic tests for IA have been developed, including the sōna Aspergillus GM Lateral flow assay (GM-LFA) rapid test.
Summary
The GM-LFA has shown excellent performance for the diagnosis of IA in patients with hematologic malignancy and may be a viable option for settings where ELISA GM testing is not feasible. Further evaluation of the GM-LFA in the non-hematology setting is ongoing, including in solid organ transplant recipients and patients in the intensive care unit.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Aspergillus spp. are environmental fungi that cause a wide spectrum of infections in humans [1], including invasive aspergillosis (IA), the most severe manifestation of disease. Globally, IA causes over 300,000 diagnosed infections annually, with a mortality rate ranging from 30 to 80% [2, 3]. Recently, IA also emerged as a complication in patients with severe Coronavirus Disease 2019, resulting in high mortality rates [4,5,6,7].
Diagnosis of IA remains difficult, particularly in patients receiving mold-active antifungals [8, 9]. Aspergillus galactomannan (GM) is an enzyme-linked immunosorbent assay (ELISA) which detects the GM polysaccharide that primarily exists in the cell wall of Aspergillus species [10]. ELISA GM is used as mycological criteria for the diagnosis of IA [11]. The ELISA GM is used on serum or bronchoalveolar fluid (BALF) specimens [12,13,14,15]. Across all patient populations, ELISA GM is more sensitive than culture, with a sensitivity and specificity from blood of 82% and 81%, respectively [15], while ELISA GM on BALF has shown better diagnostic performance than on blood, with a sensitivity and specificity of 88% and 81%, respectively [16]. The performance of GM BALF, compared to serum, is also superior in certain patient populations, such as those receiving anti-mold active agents, and those without neutropenia who usually develop invasive airway disease [17••]. Despite ELISA GM has been commercially available for more than two decades, many mycology laboratories around the Globe do not have access to ELISA GM testing, with only 23% of laboratories surveyed in Asia able to offer this test [18]. ELISA GM testing suffers from many limitations, including cost and turnaround time, particularly in settings where bulk testing is not commonly done or samples are sent to a central lab [14, 19,20,21,22]. Molecular tests such as polymerase chain reaction (PCR) are widely used to diagnose IA [19, 23, 24], although there is a lack of standardization among assays [25] and a large variation in diagnostic performance across studies and settings [21, 26]. Aspergillus PCR from blood shows particularly poor performance for the diagnosis of breakthrough infections [27] in settings that use mold-active prophylaxis [28, 29].
Diagnostic assays with improved performance, more rapid results, can be more easily performed in facilities with limited infrastructure to enable earlier, targeted treatment of invasive aspergillosis (IA). The following review provides an update on the performance of sōna Aspergillus Galactomannan lateral flow assay (LFA) (IMMY, Norman, Oklahoma, USA), a rapid test for the prompt diagnosis of IA.
Technical Aspects of GM-LFA
The GM-LFA is a self-contained sandwich immunochromatographic test for the qualitative and quantitative detection of Aspergillus GM from serum and BAL samples. It functions much like the widely used home pregnancy test, eliminating the need for advanced laboratory equipment. It is based on the principle of lateral flow: GM-specific antibodies conjugated to colloidal nano-gold bind to GM (the antigen), if it is present in the specimen sample, as it flows up the test strip through two testing zones. If binding occurs, the antibody-antigen complex will migrate up the strip by capillary flow until it is captured by the GM-specific antibodies in the test line, resulting in the formation of a visible test line. Concurrently, control antibodies conjugated to gold are present that wick along with the specimen and are captured by the control antibodies present on the control line, serving as a control.
The test requires a total of 300 μL of BALF or serum sample which is pretreated to allow adequate binding of the detecting antibodies, heated to 120 °C to denature the immunoglobulins and any other potentially interfering protein (thus freeing up the GM for detection), and centrifuged, before an aliquot is transferred to a second tube and mixed with a running buffer. Test strips are subsequently inserted into the sample running buffer aliquot and results read after 30 min [30,31,32,33]. Positive test results create two lines (test and control lines) and negative result forms only one line (the control line). If the control line fails to develop, the test is deemed invalid. Recently, an digital tube reader has been developed that provides a quantitative number which corresponds to the detected GM titer [30]. The GM-LFA test is CE-marked and currently in the process of being FDA approved.
As the LFA is designed to detect GM epitopes, some cross-reactivity with other galactofuranose-producing fungi can occur. Cross-reactivity with culture filtrate from Paracoccidiodes brasiliensis, Coccidioides spp., Histoplasma spp., and Candida spp. has been reported (IMMY, 2019). It is currently unknown if this in vitro cross-reactivity is also clinically relevant for patients infected with these fungi. In a retrospective study of sputum and BALF samples, cross-reactivity with Scedosporium spp., Fusarium spp., Saccharomyces cerevisiae, Candida parapsilosis, and Geotrichium spp. has been described [33]. Whether these findings constitute true cross-reactivity or rather undiagnosed co-infection with Aspergillus or another closely related fungus is unclear.
Performance of GM-LFA Using Visual Readout
Hematology Patients
In patients with hematological malignancy with suspected invasive pulmonary aspergillosis (IPA), ELISA-GM testing in serum and BALF is highly recommended by various guideline groups [34,35,36,37] and is the standard of care in many centers. ELISA GM is recommended particularly in highly vulnerable cohorts of patients such as those with hematological malignancy, as the early diagnosis of IPA and prompt treatment initiation is essential for successful management of the disease. In this setting, the GM-LFA with a visual readout is a promising alternative to ELISA-GM testing, as no specific technical equipment is required nor is specially-trained laboratory staff needed. Currently, clinical data evaluating the diagnostic performance of the GM-LFA with visual readout in hematological malignancy patients is limited, but results published up to date are encouraging.
A single-center retrospective trial found a sensitivity and specificity of the GM-LFA on BALF for proven or probable IPA 89% and 88%, respectively [32••]. Considering that the ELISA GM was included as a mycological criterion in this study and that the number of samples was low (N = 24), GM-LFA performed as good as the ELISA-GM and the Aspergillus-specific lateral flow device (LFD) in this study. A larger multicenter retrospective study of 235 patients with hematological malignancy found a sensitivity of 83% and specificity of 87% when comparing proven or probable IPA cases versus controls [38••]. When excluding ELISA-GM as a mycological criterion, which may be interpreted as a confounder overestimating the performance of ELISA-GM (inclusion bias), the sensitivity of GM-LFA even increased to 87%, whereas specificity remained unchanged. A potential drawback of GM-LFA with visual readout is that interpretation may be influenced by the individual interpreting the test lines, specifically for weak positive test results. This was also mentioned in the study above, where a mismatch (positive versus negative) of two independent investigators was observed in 11% of the samples [38••]. This mismatch may warrant investigation in future studies, as with other lateral-flow assays reproducibility overall was good [39], although an automated readout is now available which would circumvent this drawback. Data suggest that empiric antifungal treatment significantly reduced the sensitivity of the LFA in BALF [38••], which may potentially reflect the performance of the LFA in patients on mold-active prophylaxis. However, the performance of GM-LFA in the presence or absence of mold-active prophylaxis has not been studied.
Solid Organ Transplant Recipients
Similar to other non-culture-based test for IPA, initial reports suggest that the performance of GM- LFA testing of BALF in solid organ transplant (SOT) recipients is variable, with lower sensitivity and specificity compared with those of patients with hematological malignancy [40]. Data on the performance of GM-LFA for the diagnosis of IPA in SOT recipients is limited. One single-center study evaluated the performance of LFA in the BALF samples of 82 patients at risk for IPA but without hematological malignancy. Twenty-seven of these patients were SOT recipients, including 24/27 (89%) who were lung transplant recipients; of these patients, 5 were diagnosed with IPA (proven/probable 2, possible 3) and 19 without IPA. In this study, the sensitivity and specificity of the visual readout in SOT recipients was 50% and 48%, respectively [31••]. Further studies are currently under progress.
Intensive Care Unit/Other Patients
Only one study has evaluated the GM-LFA with visual readout assay in patients in the intensive care unit (ICU) or those with other non-hematologic diseases. In a single-center study, 82 BALF samples from 82 patients at risk for IPA were analyzed. IPA was classified according to the revised EORTC/MSG criteria [41] and a modified version of the Blot algorithm [31••]. The majority of patients were either in the ICU (15/82, 18%) or had other chronic underlying diseases such as cystic fibrosis, asthma, HIV, rheumatoid arthritis, interstitial lung disease, or liver cirrhosis (33/82, 40%). Based on EORTC/MSG criteria, 9/48 (19%) were classified as probable/proven IPA and 39/48 (81%) no IPA; according to BLOT criteria, 16/48 (33%) were classified as putative/proven IPA and 32/48 (67%) no IPA. In this study, the sensitivity and specificity of the GM-LFA was 11/18 (61%) and 28/35 (80%) in patients in the ICU or those with other diseases.
Performance of GM-LFA Using Cube Reader Readout
Hematology Patients
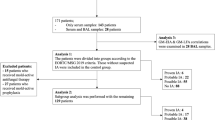
Multiple studies have evaluated the performance of GM LFA using automated reader on BALF and serum from patients with hematologic malignancies. A single center study evaluated the performance of GM LFA using automated readout on serum samples of 239 hematologic cancer patients, including 41 cases of proven/probable IPA and 188 controls. Serum GM-LFA had a sensitivity of 49% and a specificity of 95%, with a negative predictive value of 90% for probable/proven IPA vs controls. The performance of ELISA-GM was similar to that of GM-LFA, with a sensitivity of 44% and a specificity of 99%, with a negative predictive value of 89% [30]. In another study of the GM-LFA from BALF and sputum samples, a total of 398 respiratory samples from 390 patients were evaluated, of which 52 samples were positive for Aspergillus spp. by culture and microscopy, 254 were positive for either microscopy or culture, and 92 samples negatives by both culture and microscopy. The GM-LFA had a diagnostic accuracy of 92% for differentiating samples that were positive by culture and microscopy from those that were negative by both. For differentiating samples that were either positive by culture or microscopy versus negative samples, sensitivity was 90% and specificity 84% [33]. In a recent single-center retrospective case control study of 179 serum samples from 136 patients with invasive fungal disease, the GM- LFA with digital reader had a sensitivity of 96.9% (31/32) and a specificity of 98% (98/100) at a positive GM threshold of > 0.5. Furthermore, the agreement between the LFA and ELISA GM test was 89%, with the most common discordance due to false negative ELISA GM values that were positive with GM-LFA [42]. Finally, a recent multicenter study that included BALF samples from 63 patients with hematological malignancies, including 35 with probable or proven IPA, found a AUC of 0.917 (95% CI 0.847–0.988) for differentiating probable/proven versus no IPA, and a sensitivity of 80% and specificity of 89% when using a LFA cutoff of 1.0 ODI, while specificity increased to 96% (sensitivity 71%) when increasing the cutoff to 2.0 ODI [43••]. Of note, performance of GM-LFA in that study was not impacted by mold-active prophylaxis.
Solid Organ Transplant Recipients
To date only two studies have evaluated performance of GM-LFA with digital read out in SOT recipients. One multicenter study included BALF samples from 33 SOT recipients, of whom 9 had probable or proven IPA. In that study, the AUC for GM-LFA was 0.806 (95% CI 0.659–0.953), and therefore lower than for other patient groups. In terms of cut-off, a 1.0 ODI cutoff exhibited 100% sensitivity, but only 42% specificity. Specificity was 83% at a cut-off of 2.0 ODI (sensitivity 56%) [43••]. In another recent study on the performance of GM-LFA in BALF samples of a diverse population that included mostly SOT recipients, the use of a digital reader for the diagnosis of proven/probable IPA resulted in higher specificity when compared to visual read out (up to 94% vs. 84%), but did not affect the sensitivity of the test which was low (40%) [44]. Publication of those findings is currently in progress.
Intensive Care Unit/Other Patients
To date, only one study has evaluated the performance of the BALF GM-LFA assay using a digital reader for the diagnosis of IPA in ICU patients. This multicenter study included patients from Austria, Germany, and the USA, including 153 patients classified as ICU/other patient groups (i.e., without hematological malignancy and not SOT recipients). Of those, 44 had either putative or proven IPA, and GM LFA had an AUC of 0.867 (95% CI 0.797–0.937) for differentiating those with putative/proven IPA from those without IPA [43••]. In terms of cut-off, 1.0 ODI showed 80% sensitivity and 75% specificity, while 1.5 ODI showed 73% sensitivity, and therefore increased 83% specificity. Further studies in ICU patients, including studies focusing specifically on diagnosis of COVID-19-associated aspergillosis are currently in progress.
Conclusion/Future Steps
The CE-certified IMMY sōna Aspergillus Galactomannan LFA has advanced over recent years, with an automated cube reader now included in LFA kits, making the tests comparable across study sites and allow for more investigation of quantitative test performance. It is currently in the process of getting FDA approval. While this is not an assay that allows for testing directly at the bedside, it can be performed in rudimentary laboratories, requiring only pretreatment, heating, and centrifugation before testing. Most studies to date have published performance of the LFA in patients with hematological malignancies, where the assay showed very good to excellent discriminatory power for IA in serum and BALF samples, with performances similar to GM. Larger multicenter studies are needed to investigate performance of the LFA diagnosis of IA in other patient groups who are increasingly reported at risk for IA, such as SOT recipients or patients in the ICU. As an important next step, reliable definitions of IA are needed for the non-hematology settings as clinical presentation and radiologic findings differ.
In conclusion, the Aspergillus Galactomannan LFA shows promise as a new and reliable test for the diagnosis of IA and may serve a role as a rapid test that that may replace ELISA GM testing in settings where GM results are not rapidly available.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Salzer HJF, Prattes J, Hoenigl M. Editorial: diagnostic approaches for Aspergillus infections. Front Microbiol. 2019;10:446.
Bongomin F, Gago S, Oladele RO, Denning DW. Global and multi-national prevalence of fungal diseases-estimate precision. J Fungi (Basel). 2017;3(4).
Barton RC. Laboratory diagnosis of invasive aspergillosis: from diagnosis to prediction of outcome. Scientifica (Cairo). 2013;2013:459405.
Koehler P, Cornely OA, Böttiger BW, Dusse F, Eichenauer DA, Fuchs F, et al. COVID-19 associated pulmonary Aspergillosis. Mycoses. 2020;63:528–34.
Verweij PE, Gangneux J-P, Bassetti M, Brüggemann RJM, Cornely OA, Koehler P, et al. Diagnosing COVID-19-associated pulmonary aspergillosis. Lancet Microbe.
Arastehfar A, Carvalho A, van de Veerdonk FL, Jenks JD, Koehler P, Krause R, et al. COVID-19 associated pulmonary aspergillosis (CAPA)-from immunology to treatment. J Fungi (Basel). 2020;6(2).
Thompson GR III, Cornely OA, Pappas PG, Patterson TF, Hoenigl M, Jenks JD, et al. Invasive Aspergillosis as an underrecognized superinfection in COVID-19. Open Forum Infect Dis. 2020;7.
Jenks JD, Salzer HJF, Hoenigl M. Improving the rates of Aspergillus detection: an update on current diagnostic strategies. Expert Rev Anti-Infect Ther. 2019;17(1):39–50.
Jenks JD, Cornely OA, Chen SC, Thompson GR, 3rd, Hoenigl M. Breakthrough invasive fungal infections: who is at risk? Mycoses. 2020.
Zhou W, Li H, Zhang Y, Huang M, He Q, Li P, et al. Diagnostic value of galactomannan antigen test in serum and bronchoalveolar lavage fluid samples from patients with nonneutropenic invasive pulmonary Aspergillosis. J Clin Microbiol. 2017;55(7):2153–61.
Donnelly JP, Chen SC, Kauffman CA, Steinbach WJ, Baddley JW, Verweij PE, et al. Revision and update of the consensus definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer and the mycoses study group education and research consortium. Clin Infect Dis. 2020;71(6):1367–76.
Hoenigl M, Salzer HJ, Raggam RB, Valentin T, Rohn A, Woelfler A, et al. Impact of galactomannan testing on the prevalence of invasive aspergillosis in patients with hematological malignancies. Med Mycol. 2012;50(3):266–9.
Hoenigl M, Seeber K, Koidl C, Buzina W, Wolfler A, Duettmann W, et al. Sensitivity of galactomannan enzyme immunoassay for diagnosing breakthrough invasive aspergillosis under antifungal prophylaxis and empirical therapy. Mycoses. 2013;56(4):471–6.
•• Eigl S, Hoenigl M, Spiess B, Heldt S, Prattes J, Neumeister P, et al. Galactomannan testing and Aspergillus PCR in same-day bronchoalveolar lavage and blood samples for diagnosis of invasive aspergillosis. Med Mycol. 2017;55(5):528–34 Multicenter study outlining the importance of combining biomarkers with molecular tests, both preferably from BALF, to diagnose IA in patients on mold-active prophylaxis.
Rawlings SA, Heldt S, Prattes J, Eigl S, Jenks JD, Flick H, et al. Using interleukin 6 and 8 in blood and bronchoalveolar lavage fluid to predict survival in hematological malignancy patients with suspected pulmonary mold infection. Front Immunol. 2019;10:1798.
de Heer K, Gerritsen MG, Visser CE, Leeflang MM. Galactomannan detection in broncho-alveolar lavage fluid for invasive aspergillosis in immunocompromised patients. Cochrane Database Syst Rev. 2019;5:Cd012399.
•• Heldt S, Prattes J, Eigl S, Spiess B, Flick H, Rabensteiner J, et al. Diagnosis of invasive aspergillosis in hematological malignancy patients: Performance of cytokines, Asp LFD, and Aspergillus PCR in same day blood and bronchoalveolar lavage samples. J Infect. 2018;77(3):235–41 Study showing the potential of serum cytokine measurements, in particular of IL-8 for diagnosis of IA in patients on mold-active prophylaxis.
Chindamporn A, Chakrabarti A, Li R, Sun P-L, Tan B-H, Chua M, et al. Survey of laboratory practices for diagnosis of fungal infection in seven Asian countries: an Asia fungal working group (AFWG) initiative. Med Mycol. 2018;56(4):416–25.
Buchheidt D, Reinwald M, Hoenigl M, Hofmann WK, Spiess B, Boch T. The evolving landscape of new diagnostic tests for invasive aspergillosis in hematology patients: strengths and weaknesses. Curr Opin Infect Dis. 2017;30(6):539–44.
Hoenigl M, Prattes J, Neumeister P, Wolfler A, Krause R. Real-world challenges and unmet needs in the diagnosis and treatment of suspected invasive pulmonary aspergillosis in patients with haematological diseases: an illustrative case study. Mycoses. 2018;61(3):201–5.
Springer J, Lackner M, Nachbaur D, Girschikofsky M, Risslegger B, Mutschlechner W, et al. Prospective multicentre PCR-based Aspergillus DNA screening in high-risk patients with and without primary antifungal mould prophylaxis. Clin Microbiol Infect. 2016;22(1):80–6.
Reinwald M, Hummel M, Kovalevskaya E, Spiess B, Heinz WJ, Vehreschild JJ, et al. Therapy with antifungals decreases the diagnostic performance of PCR for diagnosing invasive aspergillosis in bronchoalveolar lavage samples of patients with haematological malignancies. J Antimicrob Chemother. 2012;67(9):2260–7.
Guenter S, Gorkiewicz G, Halwachs B, Kashofer K, Thueringer A, Wurm P, et al. Impact of ITS-Based Sequencing on Antifungal Treatment of Patients with Suspected Invasive Fungal Infections. J Fungi (Basel). 2020;6(2).
Jenks JD, Spiess B, Buchheidt D, Hoenigl M. (new) methods for detection of Aspergillus fumigatus resistance in clinical samples. Curr Fungal Infect Rep. 2019;13(3):129–36.
White PL, Bretagne S, Klingspor L, Melchers WJ, McCulloch E, Schulz B, et al. Aspergillus PCR: one step closer to standardization. J Clin Microbiol. 2010;48(4):1231–40.
White PL, Wingard JR, Bretagne S, Loffler J, Patterson TF, Slavin MA, et al. Aspergillus polymerase chain reaction: systematic review of evidence for clinical use in comparison with antigen testing. Clin Infect Dis. 2015;61(8):1293–303.
Cornely OA, Hoenigl M, Lass-Florl C, Chen SC, Kontoyiannis DP, Morrissey CO, et al. Defining breakthrough invasive fungal infection-position paper of the mycoses study group education and research consortium and the European Confederation of Medical Mycology. Mycoses. 2019;62(9):716–29.
Egger M, Jenks JD, Hoenigl M, Prattes J. Blood Aspergillus PCR: The Good, the Bad, and the Ugly. J Fungi (Basel, Switzerland). 2020;6(1):E18.
Arvanitis M, Ziakas PD, Zacharioudakis IM, Zervou FN, Caliendo AM, Mylonakis E. PCR in diagnosis of invasive aspergillosis: a meta-analysis of diagnostic performance. J Clin Microbiol. 2014;52(10):3731–42.
Mercier T, Guldentops E, Lagrou K, Maertens J. Prospective evaluation of the turbidimetric β-D-glucan assay and two lateral flow assays on serum in invasive aspergillosis. Clin Infect Dis. 2020.
•• Jenks JD, Mehta SR, Taplitz R, Aslam S, Reed SL, Hoenigl M. Point-of-care diagnosis of invasive aspergillosis in non-neutropenic patients: Aspergillus Galactomannan Lateral Flow Assay versus Aspergillus-specific Lateral Flow Device test in bronchoalveolar lavage. Mycoses. 2019;62(3):230–6 First study to compare the performance of the two commercially available lateral flow device tets in non-hematological patients.
•• Jenks JD, Mehta SR, Taplitz R, Law N, Reed SL, Hoenigl M. Bronchoalveolar lavage Aspergillus Galactomannan lateral flow assay versus Aspergillus-specific lateral flow device test for diagnosis of invasive pulmonary Aspergillosis in patients with hematological malignancies. J Infect. 2019;78(3):249–59 First study to compare the performance of the two commercially available lateral flow device tests.
Lass-Flörl C, Lo Cascio G, Nucci M, Camargo Dos Santos M, Colombo AL, Vossen M, et al. Respiratory specimens and the diagnostic accuracy of Aspergillus lateral flow assays (LFA-IMMY™): real-life data from a multicentre study. Clin Microbiol Infect. 2019;25(12):1563.e1-.e3.
•• Ullmann AJ, Aguado JM, Arikan-Akdagli S, Denning DW, Groll AH, Lagrou K, et al. Diagnosis and management of Aspergillus diseases: executive summary of the 2017 ESCMID-ECMM-ERS guideline. Clin Microbiol Infect. 2018;24(Suppl 1):e1–e38 ESCMID ECMM guidelines for the diagnosis and treatment of IA.
Marchetti O, Lamoth F, Mikulska M, Viscoli C, Verweij P, Bretagne S, et al. ECIL recommendations for the use of biological markers for the diagnosis of invasive fungal diseases in leukemic patients and hematopoietic SCT recipients. Bone Marrow Transplant. 2012;47(6):846–54.
Schelenz S, Barnes RA, Barton RC, Cleverley JR, Lucas SB, Kibbler CC, et al. British Society for Medical Mycology best practice recommendations for the diagnosis of serious fungal diseases. Lancet Infect Dis. 2015;15(4):461–74.
Patterson TF, Thompson GR 3rd, Denning DW, Fishman JA, Hadley S, Herbrecht R, et al. Practice guidelines for the diagnosis and Management of Aspergillosis: 2016 update by the Infectious Diseases Society of America. Clin Infect Dis. 2016;63(4):e1–e60.
•• Mercier T, Dunbar A, de Kort E, Schauwvlieghe A, Reynders M, Guldentops E, et al. Lateral flow assays for diagnosing invasive pulmonary aspergillosis in adult hematology patients: A comparative multicenter study. Med Mycol. 2020;58(4):444–52 Important paper investigating the performance of the LFA in BALF from patients with hematological malignancies and comparing visual with automated read-out.
Wiederhold NP, Najvar LK, Bocanegra R, Kirkpatrick WR, Patterson TF, Thornton CR. Interlaboratory and interstudy reproducibility of a novel lateral-flow device and influence of antifungal therapy on detection of invasive pulmonary aspergillosis. J Clin Microbiol. 2013;51(2):459–65.
Miceli MH, Maertens J. Role of non-culture-based tests, with an emphasis on galactomannan testing for the diagnosis of invasive Aspergillosis. Semin Respir Crit Care Med. 2015;36(5):650–61.
De Pauw B, Walsh TJ, Donnelly JP, Stevens DA, Edwards JE, Calandra T, et al. Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/invasive fungal infections cooperative group and the National Institute of Allergy and Infectious Diseases mycoses study group (EORTC/MSG) consensus group. Clin Infect Dis. 2008;46(12):1813–21.
White PL, Price JS, Posso R, Cutlan-Vaughan M, Vale L, Backx M. Evaluation of the performance of the IMMY sona Aspergillus galactomannan lateral flow assay when testing serum to aid in diagnosis of invasive Aspergillosis. J Clin Microbiol. 2020;58(6).
•• Jenks JD, Prattes J, Frank J, Spiess B, Mehta SR, Boch T, et al. Performance of the bronchoalveolar lavage fluid Aspergillus galactomannan lateral flow assay with cube reader for diagnosis of invasive pulmonary aspergillosis: a multicenter cohort study. Clin Infect Dis. 2020. A large multicenter study evaluating the LFA with automated read-out in a mixed cohort.
Miceli MH, et al. Publication currently in progress. 2020.
Funding
This work was partially funded by NIH UL1TR001442.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
MH received research funding from Gilead and Pfizer. The other authors declare no conflicts of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Advances in Diagnosis of Invasive Fungal Infections
Rights and permissions
About this article
Cite this article
Jenks, J.D., Miceli, M.H., Prattes, J. et al. The Aspergillus Lateral Flow Assay for the Diagnosis of Invasive Aspergillosis: an Update. Curr Fungal Infect Rep 14, 378–383 (2020). https://doi.org/10.1007/s12281-020-00409-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12281-020-00409-z